Abstract
Do different operationalizations of family structure offer different understandings of the links between family structure and older adult mortality? Using the Health and Retirement Study (N=29,665), we examine mortality risks by three measures of family structure: whether respondents have different family statuses (e.g., being married vs. unmarried), the volume of family members available (e.g., having one vs. two living immediate family members), and family embeddedness (e.g., has neither spouse nor child vs. has spouse but no child). We focus on three kin types: partner/spouse, children, and siblings. We find that differences in empirical estimates across measures of family structure are not dramatic, but that family embeddedness can show some additional heterogeneity in mortality patterns over family status variables or the volume of ties. This article tests different ways of operationalising family structure to study mortality outcomes and advances our understanding of how family functions as a key social determinant of health.
Keywords: Family, Kinless, Mortality, Health, Kinship, Social Networks
Family structure is a key social determinant of health (Russell et al. 2018) and mortality (Kravdal et al. 2012). Dozens if not hundreds of studies examine associations between older adult mortality and different measures of family structure, such as being married or the number of living family members available to older adults. For instance, prior research indicates that being married (Waite 1995; Rendall et al. 2011; Franke and Kulu 2018), having children (Keizer et al. 2012; Högnäs et al. 2017; Reyes et al. 2018), and having siblings alive (Perls et al. 2002; Bobak et al. 2003) are each associated with reduced mortality hazards. Other studies capture the volume of ties or network size and associations with health and mortality (e.g. Eng et al. 2002; Mair 2010). However, to date, only a few studies have considered how different measures of family structure might yield different understandings of the links between older adult mortality and family structure (Kalmijn 2017; Kravdal et al. 2012; O’Flaherty et al. 2016). For instance, most quantitative studies tend to treat measures of family structure as individual variables and do not examine more nuanced operationalizations such as whether older adults with a spouse and no children have different mortality patterns than older adults with a spouse and at least one child. Likewise, research on such associations using the number of family members available or size of network tends to ignore the types of ties. This neglect is unfortunate because specific types of family structures might constrain how older adults access their family networks for help and support. As such, the most common measurement strategies may be unable to capture the trade-offs and substitutions that different family structures can necessitate for older adults, such as how the childless and widowed draw extensively on siblings for instrumental support during illness (Connidis 1994).
Do different operationalizations of family structure offer different understandings of the links between family structure and older adult mortality? We answer this question by investigating three different operationalizations. First, we consider a family status operationalization, where family statuses are defined as having or not having members of different relationship types (e.g., one lacks a spouse but may or may not have living children). Second, we examine a volume of ties operationalization, where the volume of ties is defined by the number of available immediate family members (e.g., one has one immediate family member but this person may be either a spouse or a child). Third, we move the literature forward by also examining a family embeddedness operationalization, which we define as the cross-classification of members available in different statuses (e.g., differentiating between, for instance, those who lack a spouse and have no living children and those who lack a spouse and have living children).
A critical observation in research about social influences on health behaviors highlights that “… the constellation of social ties, not any single social tie, matters most for health habits…” (Umberson et al. 2010, p. 142). However, to date, few studies have tested whether this insight applies to the associations between older adult mortality and family, and this paper provides the first comparison of different operationalizations of family structure, mapping theory to variable construction. There are also practical reasons to consider these distinctions. Among contemporary older adults, it may become increasingly important to study more nuanced measures of family structure – such as family embeddedness – because of the thinning of kin networks and the rapid growth of novel family forms in older adulthood. Reductions in mortality have led to longer shared lives with family members (Bengtson 2001), but fertility declines in the last half-century mean that new cohorts of older adults have fewer siblings and fewer children, on average, than prior cohorts (Morgan and Taylor 2006; Verdery 2015). Childlessness is also on the rise (Morgan and Taylor 2006), as is “gray divorce,” or divorce over the age of 50 (Brown and Lin 2012). All of these changes are contributing to the ongoing rise in “kinless” older adults who do not have any family members, including living partners, children, or siblings (Margolis and Verdery 2017; Verdery and Margolis 2017; Verdery et al. 2019). At the same time, the effects of these changes may be blunted by increases in older adult non-marital cohabitation (Hemez and Brown 2016), repartnering (Brown et al. 2018, Brown et al. 2019), partners who “live apart together” (Benson and Coleman 2016), and the increasing importance of step-families (Wachter 1997; Lin et al. 2018). It may be difficult to measure family embeddedness due to data limitations (e.g., not all data sets ask about non-coresidential children) or the rarity of the some family forms (e.g., not all surveys are large enough to observe a sufficient number of older adults lacking multiple types of kin for statistical analysis). Without knowing whether these operationalizations offer different understandings of older adult mortality risks, researchers are not able to weigh what is being overlooked.
It is also important to consider whether the relationships between older adult mortality and different operationalizations of family structure vary when accounting for other factors. We explore three sets of explanatory factors that may either confound or mediate the relationship between mortality risks and family structure. First, economic security is likely to be associated with both older adult mortality and family structure. For instance, adults with fewer resources are less likely to partner (Smock et al. 2005), which may influence their wealth creation over the life course, and these economic circumstances could contribute to their survivorship (Sorlie et al. 1992). A second factor is health. For example, adults with chronic conditions may be at higher risk of both partnership dissolution and mortality (Elwert and Christakis 2008), while partnership itself may influence health behaviors (August and Sorkin 2010), which help lower mortality risk. Last, social connectedness beyond the family also matters, as studies repeatedly find that loneliness and social isolation are highly predictive risk factors for mortality (Luo et al. 2012). Aside from these three factors, higher mortality risks and family structure may also vary by other characteristics, including easily measured characteristics like race and gender, and factors that are more challenging to measure in survey data, such as the types of social support that families can provide through help managing chronic illness, providing care, or providing a sense of “meaning” (Margolis 2013a; Taylor et al. 2018).
In this article, we test whether and how older adult mortality hazards are associated with different operationalizations of family structure using 20 years of prospective data on U.S. older adults from the Health and Retirement Study. First, we test whether a family embeddedness approach offers a deeper understanding of the associations between mortality and family structure in older adulthood than measuring family with singular family statuses like partnership or parenthood or by focusing on the volume of family ties available by considering the diversity of family roles. Next, we examine whether three explanatory factors account for the relationships between mortality hazards and family structure: economic security, health, and social connectedness. Finally, given established findings in the literature regarding stratification in the social challenges of aging in the U.S. (Klinenberg 2002; Margolis and Verdery 2017), we test for variation by race and gender in the associations between mortality risks and family embeddedness.
Background
Families and older adult mortality
Prior scholarship clearly demonstrates numerous links between family structure and older adult mortality (or a key determinant of mortality, health). For instance, a meta-analysis of the literature on mortality and partnership finds that never married adults have 24% higher mortality hazards than their currently married counterparts (Roelfs et al. 2011). The literature indicates that partnership, rather than marriage per se, is the defining distinction. Although married and cohabiting older adults historically had different mortality risks, recent research finds that the importance of this distinction is declining (Franke and Kulu 2018), or that the link between partnership and health outcomes is ambiguous (Kalmijn 2017). Likewise, contemporary studies suggest small differences in mortality risks among different types of single adults, including the never married, divorced, and widowed (Rendall et al. 2011). Other research describes the relationships between older adult mortality and having children. There is evidence of elevated mortality risks in both adults without children and adults with many children compared to those with a small number of children (Grundy and Kravdal 2010; Högnäs et al. 2017). Although it is rare that studies test relationships between older adult mortality and the presence or absence of other types of family members, a few studies offer mixed evidence about mortality risks and the availability of siblings (Perls et al. 2002; Bobak et al. 2003; Gakidou and King 2006).
A focus on singular family status variables or the volume of family ties dominates empirical research linking older adult mortality and families, despite theoretical motivations calling for more nuanced measurement (Umberson et al. 2010). This focus on family statuses and volume may be limited for several reasons. First, a focus on the relationships between mortality and single family statuses or the volume of ties ignores recent developments in both contemporary families and scholarship about them. Families are complex entities, and scholarship about them is increasingly attuned to the importance and diversity of different family compositions (Seltzer 2019). Part of the reason for this attention is that there is increasing diversity in family structure at all ages, even for older adults. For example, more older adults are “kinless,” without any living family (Margolis and Verdery 2017; Zhou et al. 2018). Focusing on individual family statuses would miss the increasing prevalence of this family form because it fails to differentiate the kinless from those who are, as an example, un-partnered but who have living children. We focus on the different combinations or constellations of kin.
Second, a focus on family statuses or the volume of family ties ignores how different kin become more or less important in the absence of other kin in the family, which are determined beyond the dyadic level (Bronfenbrenner 1986; Cox and Paley 2003). For instance, support to a parent may be less forthcoming when that parent is partnered, while the childless may be more likely to turn to siblings than those with children. However, studies of family statuses will miss these processes, unable to separate the cases of those without family from those who lack a particular type of family member. Likewise, simply considering the volume of ties available may provide insufficient understandings of the functional roles played by family members of different types. The prior example contemplating support to a parent is instructive when thinking about how considerations of family embeddedness might differ from considerations of the volume of ties: it seems likely that a child’s provision of support to a parent will hinge more strongly on whether that parent is partnered than the number of other children the parent has.
Among the studies that test associations between older adult mortality (or health) and broader operationalizations of family status and structure, a majority focus on marital and fertility histories and health rather than mortality (e.g. O’Flaherty et al. 2016; Kalmijn 2017). The few studies that examine family structure and mortality focus on European countries with rich data registries on families (Berntsen and Kravdal 2012; Kravdal et al. 2012), or only focus on subgroups like women (Henretta 2007; Reyes et al. 2018; Sabbath et al. 2015; Wolfe et al. 2018). These studies provide a critical base for understanding how family members can influence aspects of older adult health which then shape mortality. European research shows that the welfare state can shape the effect of different family statuses on health and mortality outcomes (Hank 2010). Therefore, our U.S.-based study focuses on a context with less generous social welfare and health care policies and different normative expectations that families bear the care burden for older family members (Carr 2019). In addition, there is great variation within the U.S. by race/ethnic group in family structure, living arrangements, and transfers.
There are many reasons to think that accounting for family embeddedness might improve understandings of the links between older adult mortality and family structure. As discussed, social support is conditional on family embeddedness, and support is strongly predictive of mortality (Shor et al. 2013). Second, a focus on family embeddedness can help to disentangle how different family statuses contribute to mortality. For example, it may be that associations between having no children and mortality are driven by those who are not partnered. Children may also explain part of the difference between the mortality of those with partners and those without, as Franke and Kulu (2018) find that the gap in mortality risks between partnered and un-partnered older adults is substantially lower after accounting for numbers of children. Although it is surely true that the volume of family ties available is important, there may also be differences between counts of available family members that do not distinguish those in different roles (e.g., someone has three living family members) and counts of the diversity of family roles with available family members (e.g., someone has a spouse, a child, and a sibling). A full consideration of family embeddedness would help to isolate these patterns. At the extreme, older adults without any family members may have the highest mortality risk. Recent research shows that kinless older adults are in worse health than their counterparts with family, and that kinlessness is expected to increase in the coming decades in the U.S. (Margolis and Verdery 2017; Verdery and Margolis 2017). Taking a family embeddedness perspective to understand the relationships between older adult mortality and family may allow researchers to better grasp how these ongoing changes in older adult family structures might influence current and future health trends.
Explanatory factors
Economic security, physical health, and social connectedness are three explanatory factors that may act as confounders or mediators of the relationship between older adult mortality and family structure. It is important to recognize that these factors may confound or mediate such relationships through multiple mechanisms: they likely act both through selection into various family statuses and as a consequence of family status. Although understanding whether these factors are producers or products of family structure is an important research area in its own right, it is not a central consideration when focusing on the relationship between family structure and mortality. Instead, when focusing on that relationship, the key question is the extent to which these factors might account for the association.
Components of economic security, including income and wealth, may be particularly important in explaining variation in both mortality and family structure through either selection or mediation mechanisms. For instance, those with few resources have a low likelihood of marriage and partnership (Smock et al. 2005) and older adults who have never been married have the highest rates of poverty (Tamborini 2007). Marriage also serves as a wealth-building institution since it involves sharing residences and economies of scale (Waite 1995), and wealth is independently associated with lower mortality risks (Wolfe et al. 2018). Other research also links economic security, family structure, and mortality through different mechanisms. For example, socioeconomic factors, including education, help to explain part of the association between mortality and birth parity (Barclay and Kolk 2018).
Health is another factor. Adults who are healthier are more likely to be married and have children (Franke and Kulu 2018), either because they are more likely to enter these relationships or, in the case of marriage, to preserve them (Waldron et al. 1996). The selection of healthier people into denser family networks seems to explain some of the association between marriage, number of children, and mortality (Waite 1995; Keizer et al. 2012). However, these associations do not seem to be entirely driven by selection, as married adults continue to have better health outcomes compared with single adults even after accounting for health status differentials at entry to marriage (Rogers et al. 2010). Similar findings exist for partnered adults compared to non-partnered adults (Rendall et al. 2011). There is less research on sibling relationships, health, and mortality. Having siblings alive at older ages may represent the robustness of the family genes (Perls et al. 2002) and affect mortality via selection, or it could represent the importance of social support provided by siblings in older adulthood (Connidis 1994; Connidis and Campbell 1995).
A third factor is social connectedness. More social connections are associated with reductions in mortality risks (Shye et al. 1995; Litwin 2007). Older adults without family members may be at higher risk of social isolation or loneliness (Klinenberg 2013), and this may explain elevated mortality. Trade-offs and substitutions occur among ties as well, as for example when unmarried older adults report larger reductions in loneliness than married older adults upon contact with children and siblings (Pinquart 2003). Non-family ties may also be important (Mair 2019), as well as ties to other institutions (Anxo et al. 2019). For instance, married older adults, compared to single older adults, are more likely to be in the labor market (Flippen and Tienda 2000), and labor force exit is associated with increased mortality risk (Fitzpatrick and Moore 2018). In addition to providing social connections, being in the labor market can also provide economic security. Alternatively, it may also function as a proxy for age or health status.
Race/ethnicity, gender, family, and mortality
Prior scholarship also points to the importance of considering differences between population subgroups and suggests that associations between older adult mortality and family structure are likely to vary by race and gender. Decades of research documents race differences in the functional roles played by family members of different types (Parsons 1943; Stack 1975; Cross 2019). Racial/ethnic and gender differences are also a core concern of the general literature on social connections and health behaviors (Umberson et al. 2010). Prior research suggests that the detrimental effects of aging alone are stronger for some racial and ethnic groups than others, and more for men than for women (Klinenberg 2002; Margolis and Verdery 2017). Physically, men benefit more from marriage compared to women (Rendall et al. 2011), though unemployed women see similar protective health effects from marriage compared to men (Waldron et al. 1996). Divorce and singledom are more strongly associated with higher mortality risk for men than women (Kaplan and Kronick 2006). Partnership is not the only family domain with race and gender differences in mortality risks. Among a sample of women, for instance, having children is associated with longevity for White women but not Black women (Reyes et al. 2018). Contact with family members is more protective for Black men’s mortality outcomes compared to Black women’s (Bryant and Rakowski 1992).
Factors that may explain the relationship between older adult mortality and family embeddedness may also have differential importance for different racial, ethnic, and gender groups. For instance, economic security may be a bigger confounder or mediator for some groups than others. There are substantial race differences in family formation (Raley and Sweeney 2007) and in income and wealth (Noël 2018). Having higher income is also associated with greater reductions in mortality risks for White than Black adults (Sorlie et al. 1992). Health selection and mediation are also likely to differ by race and gender. For instance, unhealthy men are more likely to re-partner than unhealthy women (Lillard and Panis 1996). Last, although social connections are important for both men and women’s mortality, men benefit more than women from small increases in network size (Shye et al. 1995). These patterns may influence mortality disparities.
Data
To study the links between older adult mortality and family structure, we use data from the Health and Retirement Study (HRS), a biennial, longitudinal study of aging that is nationally representative of older adults in the United States. It comprises multiple cohorts of older adults including the Lost Generation born 1890-1923, the Silent Generation born 1924-1930, the original HRS cohort born 1931-41, War Babies born 1942-47, early Baby Boomers born 1948-1953, and mid Baby Boomers born 1954-1959. The HRS is ideally suited to answer questions about mortality and family structure because its sample is large enough to examine complex older adult family structures, and it carefully measures mortality timing and a host of potential explanatory factors that could confound or mediate the relationship between family structure and mortality including health, economic circumstances, and social support. Unlike many other aging surveys, HRS follows respondents if they enter nursing facilities (since 2000), which offers a chance to examine a wider range of mortality events. The HRS is a high-quality survey with low attrition and a response rate above 80% for each wave (Health and Retirement Survey 2017).
We compile an analytic sample covering the period 1992 to 2012 (Waves 1 to 11) from the RAND HRS main and family files and 2014 Tracker file (RAND Center for the Study of Aging 2016; University of Michigan 2018). We use event history analysis (see Methods, below) which examines deaths occurring in time intervals and thus necessitates at least two observations per person. Of the 37,796 individuals the HRS attempted to reach, 35,779 of them responded by self or proxy to at least two of these waves. The HRS also included spouses of respondents, some of whom may be younger than the target ages of eligibility; we exclude such people from our analysis (3,300 people), leaving 32,479 respondents that were ages 50 and older upon entry into the survey.
In general, the HRS has low item non-response, but it is a complex data set. First, it “preloads” certain responses from prior waves in each subsequent wave. Second, the RAND files impute missing data on some variables. Third, not all questions are asked of every person in every wave; for instance, proxy respondents do not answer questions about loneliness, and Instrumental Activities of Daily Living (IADL) and Activities of Daily Living (ADL) items are not available in the first wave. To deal with these complexities and fill in remaining missing data for non-kin related items, we carry forward respondents’ responses to prior waves when data are missing in a wave, or if no prior wave information is available, we carry information backward from the subsequent wave. For our kin measures, we only carry data backward for children and siblings (e.g., if a sibling is alive in Wave 11 but missing in Wave 10, we marked them alive in Wave 10). After these procedures, missing data are uncommon: we use listwise deletion to exclude an additional 2,811 individuals who have missing data on at least one measure of interest. Our final analytic sample includes 29,665 respondents who contribute a total of 159,667 time intervals (an average of 5.4 intervals between observations per person).
Methods
We first describe the prevalence of different types of family embeddedness among older adults in the United States (Table 1). We then describe the relationship between mortality and family embeddedness using a Kaplan-Meier survival curve (Figure 1). Next, we statistically test the relationships between older adult mortality and the three different operationalisations of family structure (family status variables, the volume of ties, and family embeddedness) using Cox Proportional Hazard models (Table 2–4). From the Cox models, Table 2 presents survival probabilities at years 5, 10, and 20, and Tables 3 and 4 present hazard ratios (HRs). Next, we examine whether these relationships vary by population subgroup by estimating models that interact family embeddedness with race and gender (Table 5).
Table 1.
Percent distribution and sample size of family embeddedness at baseline disaggregated in three ways.
| Weighted prevalence | Sample size | |||||
|---|---|---|---|---|---|---|
| Disaggregated by: | Disaggregated by: | |||||
| Partnership only | Partner & children | Partner, children, & siblings | Partnership only | Partner & children | Partner, children, & siblings | |
| Partner | 67.7% | 20,696 | ||||
| & child | 64.5% | 19,755 | ||||
| & sibling | 57.7% | 17,372 | ||||
| & no Sibling | 6.8% | 2,383 | ||||
| & no child | 3.2% | 941 | ||||
| & sibling | 2.8% | 797 | ||||
| & no sibling | 0.4% | 144 | ||||
| No partner | 32.3% | 8,969 | ||||
| & child | 25.4% | 7,351 | ||||
| & sibling | 22.1% | 6,291 | ||||
| & no sibling | 3.3% | 1,060 | ||||
| & no child | 6.8% | 1,618 | ||||
| & sibling | 5.9% | 1,346 | ||||
| & no sibling | 1.0% | 272 | ||||
| Total | 100.0% | 100.0% | 100.0% | 29,665 | 29,665 | 29,665 |
Note: Partner = partner or spouse; Child = any children; Sibling = any siblings.
Figure 1.
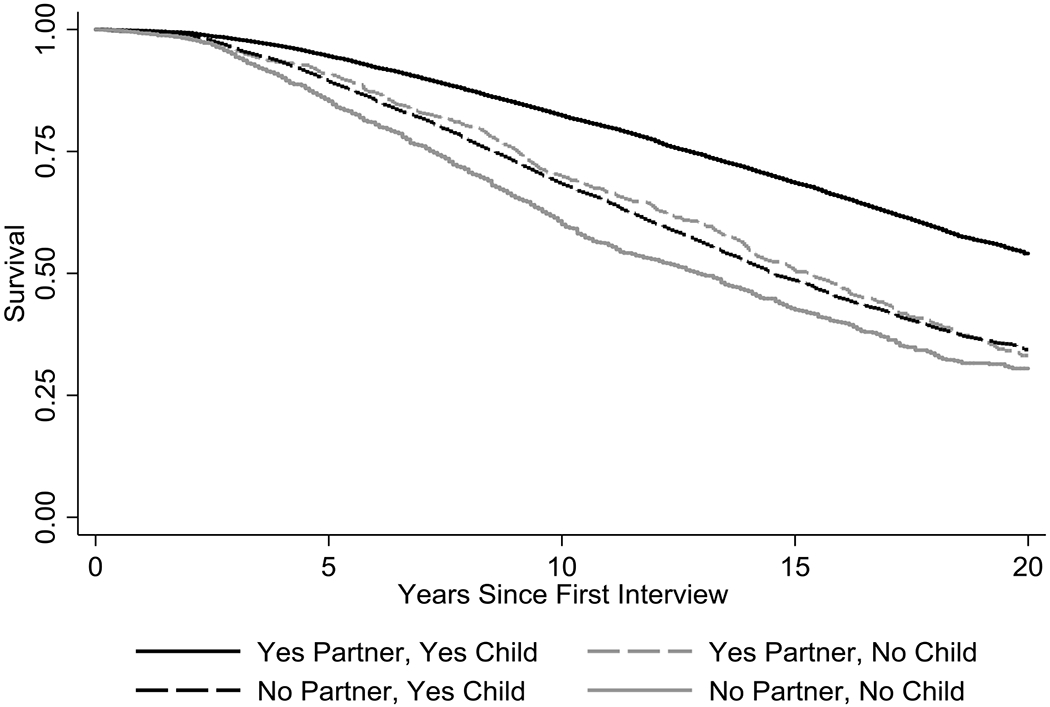
Kaplan-Meier survival curves by family embeddedness (including partner/spouse and children) at baseline.
Table 2.
Descriptive probabilities from Kaplan Meier curves and adjusted predicted probabilities of survival from survival curves at 5, 10, and 20 years for three measures of family structure.
| Survival probability | ||||||
|---|---|---|---|---|---|---|
| Descriptive |
Adjusted |
|||||
| 5 years | 10 years | 20 years | 5 years | 10 years | 20 years | |
| Family status | ||||||
| No partner | 88.6% (87.8, 89.3) | 67.1% (65.9, 68.2) | 33.8% (32.4, 35.1) | 90.6% (90.2, 91.0) | 79.2% (78.6, 79.8) | 64.7% (63.8, 65.6) |
| Partner | 94.3% (94.0, 94.6) | 81.9% (81.3, 82.5) | 53.2% (52.3, 54.2) | 91.5% (91.1, 91.8) | 80.9% (80.4, 81.3) | 67.1% (66.5, 67.7) |
| No child | 87.4% (85.9, 88.8) | 63.9% (61.6, 66.1) | 31.5% (28.9, 34.1) | 90.1% (89.5, 90.7) | 78.3% (77.3, 79.3) | 63.4% (62.0, 64.8) |
| Child | 93.1% (92.7, 93.4) | 78.7% (78.1, 79.2) | 48.8% (48.0, 49.6) | 91.3% (90.9, 91.6) | 80.5% (80.1, 80.9) | 66.6% (66.1, 67.2) |
| Volume of ties | ||||||
| Zero | 85.3% (83.2, 87.2) | 60.3% (57.4, 63.2) | 30.5% (27.3, 33.7) | 89.7% (89.0, 90.4) | 77.6% (76.4, 78.8) | 62.6% (60.9, 64.3) |
| One | 87.3% (85.6, 88.7) | 64.1% (61.7, 66.4) | 28.5% (25.8, 31.3) | 89.7% (89.1, 90.4) | 77.6% (76.6, 76.8) | 62.6% (61.2, 64.1) |
| Two+ | 93.5% (93.1, 93.8) | 79.5% (79.0, 80.1) | 49.9% (49.1, 50.7) | 91.4% (91.0, 91.7) | 80.7% (80.3, 81.1) | 66.9% (66.3, 67.4) |
| Family embeddedness | ||||||
| Yes partner, yes child | 94.5% (94.1, 94.8) | 82.4% (81.8, 83.0) | 54.1% (53.1, 55.0) | 91.6% (91.3, 92.0) | 81.1% (80.6, 81.6) | 67.4% (66.8, 68.0) |
| No partner, yes child | 89.2% (88.4, 90.0) | 68.4% (67.2, 69.6) | 34.4% (32.9, 35.9) | 90.6% (90.2, 91.1) | 79.3% (78.6, 79.9) | 65.7% (63.8, 65.7) |
| Yes partner, no child | 90.9% (88.6, 92.7) | 69.8% (66.1, 73.2) | 33.2% (28.8, 37.6) | 90.0% (89.1, 90.9) | 78.0% (76.4, 79.6) | 63.0% (60.8, 65.3) |
| No partner, no child | 85.3% (83.2, 86.2) | 60.3% (57.4, 63.2) | 30.5% (27.3, 33.7) | 89.6% (88.9, 90.4) | 77.4% (76.2, 78.6) | 62.2% (60.5, 63.9) |
Notes: Descriptive survival probabilities are unadjusted; the adjusted models include all controls used in Table 3 Model 6.
Table 4.
Hazard ratios from Cox proportional hazard models by three measures of family structure (including partner/spouse, children, and siblings).
| Model 1 (family status & controls) | Model 2 (volume of ties & controls) | Model 3 (family embeddedness & controls) | Model 4 (M1 & explanatory factors) | Model 5 (M2 & explanatory factors) | Model 6 (M3 & explanatory factors) | |
|---|---|---|---|---|---|---|
| Family status | ||||||
| No partner (yes partner) | 1.306*** | 1.131*** | ||||
| No child (yes child) | 1.173*** | 1.168*** | ||||
| No sibling (yes sibling) | 1.224*** | 1.118*** | ||||
| Volume of ties (0) | ||||||
| 1 | 0.928 | 1.024 | ||||
| 2+ | 0.686*** | 0.782*** | ||||
| Family embeddedness (yes partner, yes child, yes sibling) | ||||||
| No partner, yes child, yes sibling | 1.337*** | 1.148*** | ||||
| Yes partner, no child, yes sibling | 1.279** | 1.189* | ||||
| Yes partner, yes child, no sibling | 1.235*** | 1.119** | ||||
| No partner, no child, yes sibling | 1.477*** | 1.296*** | ||||
| Yes partner, no child, no sibling | 1.665*** | 1.624*** | ||||
| No partner, yes child, no sibling | 1.604*** | 1.262*** | ||||
| No partner, no child, no sibling | 1.794*** | 1.420*** | ||||
| Control variables | ||||||
| Female (male) | 0.649*** | 0.699*** | 0.649*** | 0.627*** | 0.645*** | 0.626*** |
| Race (White, non-Hispanic) | ||||||
| Black, non-Hispanic | 1.087* | 1.143*** | 1.084* | 0.904*** | 0.918** | 0.902*** |
| Hispanic | 0.811*** | 0.816 | 0.810*** | 0.678*** | 0.675*** | 0.678*** |
| Other, non-Hispanic | 0.935 | 0.958 | 0.934 | 0.789* | 0.797* | 0.790* |
| Education (less than high school) | ||||||
| High school degree | 0.775*** | 0.772*** | 0.775*** | 1.005 | 1.007 | 1.004 |
| Some college | 0.667*** | 0.678*** | 0.669*** | 0.951 | 0.968 | 0.951 |
| College degree or more | 0.582*** | 0.583*** | 0.582*** | 0.969 | 0.977 | 0.968 |
| Age | 1.086*** | 1.090*** | 1.086*** | 1.063*** | 1.065*** | 1.063*** |
| Economic security | ||||||
| Logged wealth | 0.987*** | 0.984*** | 0.987*** | |||
| Logged individual income | 0.984** | 0.984** | 0.984** | |||
| Physical health | ||||||
| Good/excellent health (fair/poor health) | 0.567*** | 0.567*** | 0.568*** | |||
| Number of chronic conditions | 1.097*** | 1.097*** | 1.096*** | |||
| Smoking (never smoker) | ||||||
| Former smoker | 1.278*** | 1.280*** | 1.278*** | |||
| Current smoker | 1.824*** | 1.849*** | 1.823*** | |||
| Number of ADLs | 1.147*** | 1.148*** | 1.147*** | |||
| Number of IADLs | 1.197*** | 1.197*** | 1.197*** | |||
| Participate in vigorous activity (does not participate) | 0.671*** | 0.670*** | 0.671*** | |||
| Social connectedness | ||||||
| Lonely (not lonely) | 0.986 | 0.996 | 0.986 | |||
| Labor force participation (not working) | ||||||
| Part-time | 0.647*** | 0.647*** | 0.647*** | |||
| Full-time | 0.583*** | 0.585*** | 0.583*** | |||
Note: N=159,667. Partner = partner or spouse; Child = any children; Sibling = any siblings.
p<0.01
p<0.01
p<0.05.
Table 3.
Hazard ratios from Cox proportional hazard models by three measures of family structure (including partner/spouse and children).
| Model 1 (family status & controls) | Model 2 (volume of ties & controls) | Model 3 (family embeddedness & controls) | Model 4 (M1 & explanatory factors) | Model 5 (M2 & explanatory factors) | Model 6 (M3 & explanatory factors) | |
|---|---|---|---|---|---|---|
| Family status | ||||||
| No partner (yes partner) | 1.307*** | 1.131*** | ||||
| No child (yes child) | 1.176*** | 1.169*** | ||||
| Volume of ties (0) | ||||||
| 1 | 0.967 | 0.996 | ||||
| 2+ | 0.751*** | 0.809*** | ||||
| Family embeddedness (yes partner, yes child) | ||||||
| No partner, yes child | 1.330*** | 1.143*** | ||||
| Yes partner, no child | 1.297*** | 1.239*** | ||||
| No partner, no child | 1.479*** | 1.292*** | ||||
| Control variables | ||||||
| Female (male) | 0.651*** | 0.693*** | 0.651*** | 0.628*** | 0.642*** | 0.627*** |
| Race (White, non-Hispanic) | ||||||
| Black, non-Hispanic | 1.093** | 1.131*** | 1.090* | 0.907*** | 0.912** | 0.905*** |
| Hispanic | 0.805*** | 0.817*** | 0.804*** | 0.675*** | 0.676*** | 0.674*** |
| Other, non-Hispanic | 0.929 | 0.944 | 0.928 | 0.788* | 0.792* | 0.788* |
| Education (less than high school) | ||||||
| High school degree | 0.786*** | 0.775*** | 0.786*** | 1.012 | 1.009 | 1.012 |
| Some college | 0.679*** | 0.681*** | 0.681*** | 0.963 | 0.973 | 0.964 |
| College degree or more | 0.594*** | 0.584*** | 0.595*** | 0.979 | 0.979 | 0.979 |
| Age | 1.088*** | 1.090*** | 1.088*** | 1.064*** | 1.065*** | 1.064*** |
| Economic security | ||||||
| Logged wealth | 0.987*** | 0.985*** | 0.987*** | |||
| Logged individual income | 0.984** | 0.984*** | 0.984** | |||
| Physical health | ||||||
| Good/excellent health (fair/poor) | 0.568*** | 0.568*** | 0.568*** | |||
| Number of chronic conditions | 1.097*** | 1.098*** | 1.097*** | |||
| Smoking (never smoker) | ||||||
| Former smoker | 1.282*** | 1.282*** | 1.282*** | |||
| Current smoker | 1.831*** | 1.845*** | 1.830*** | |||
| Number of ADLs | 1.148*** | 1.148*** | 1.148*** | |||
| Number of IADLs | 1.198*** | 1.197*** | 1.198*** | |||
| Participates in vigorous activity (does not participate) | 0.670*** | 0.671*** | 0.671*** | |||
| Social connectedness | ||||||
| Lonely (not lonely) | 0.987 | 0.994 | 0.987 | |||
| Labor force participation (not in labor force) | ||||||
| Part-time | 0.648*** | 0.650*** | 0.648*** | |||
| Full-time | 0.583*** | 0.585*** | 0.583*** | |||
Notes: N=159,667. Partner = partner or spouse; Child = any children.
p<0.01
p<0.01
p<0.05.
Table 5.
Hazard ratios from Cox proportional hazard models with gender and race interactions by family embeddedness (including partner/spouse and children).
| Model 1 (gender interaction) | Model 2 (race interaction) | |
|---|---|---|
| Family embeddedness (yes partner, yes child) | ||
| No partner, yes child | 1.191*** | 1.177*** |
| Yes partner, no child | 1.194* | 1.325*** |
| No partner, no child | 1.259* | 1.340*** |
| Family*gender interaction | ||
| Female | 0.633*** | |
| No partner, yes child × female | 0.942 | |
| Yes partner, no child × female | 1.084 | |
| No partner, no child × female | 1.034 | |
| Family*race interaction | ||
| White, non-Hispanic (omitted) | ||
| Black, non-Hispanic | 0.975 | |
| Hispanic | 0.711*** | |
| Other, non-Hispanic | 0.876 | |
| No partner, yes child × Black, non-Hispanic | 0.890* | |
| Yes partner, no child × Black, non-Hispanic | 0.717* | |
| No partner, no child × Black, non-Hispanic | 0.871 | |
| No partner, yes child × Hispanic | 0.872 | |
| Yes partner, no child × Hispanic | 1.033 | |
| No partner, no child × Hispanic | 0.845 | |
| No partner, yes child × other, non-Hispanic | 0.810 | |
| Yes partner, no child × other, non-Hispanic | 0.794 | |
| No partner, no child × other, non-Hispanic | 0.762 |
Note: N=159,667. Partner = partner or spouse; Child = any children. This table interacts gender (model 1) and race (model 2) with the family embeddedness measures; compare to results in Table 2, Model 4. Wald tests for interactions not significant. Includes all controls from Table 2, Model 4.
p<0.01
p<0.01
p<0.05.
We also examine a series of sensitivity tests and supplemental models that are summarized below and included in the supplemental digital content, including: models that use time-varying measures of family embeddedness, different definitions of family embeddedness, survival analysis modeled on age instead of time in the survey, and an alternative modeling approach to illustrate survival curves.
Measures
Outcome variable: time to mortality
For the event history analysis, we examine time from survey entry to mortality as the focal outcome variable. The analysis begins with the interview date when the respondent enters the survey, and ends at the time of death, with censoring of individuals who are still alive at the end of the survey. Deaths are coded on the month and year of death according to the National Death Index, but if not available then we use the death date from the exit interview, and if neither is available, then the date of last interview. About one-third (34.0%; n=10,074) of the sample dies during their time in the survey.
Key explanatory variables: three operationalizations of family structure
Our key explanatory measures reflect the presence or absence of three types of family ties at the time of entry into the survey: partners (whether or not the respondent reports being married, married but spouse absent, or partnered), children (whether or not the respondent reports any children including biological, step-, or other children), and siblings (whether or not the respondent reports any living siblings; HRS does not distinguish sibling types). We examine these measures in three ways, individually, summatively, and as interactions that cross-classify the full range of available family members. When we look at family ties individually, such as being a parent or a partner, they are disembedded measures of family status. When we look at family ties summatively, such as how many family members of these types someone has without considering what types they are, they reflect the volume of family ties available. When we look at family ties as interactions, such as when we contrast those who are both a parent and partnered to those who are a parent but not partnered, they are measures of family embeddedness. For simplicity, we present the family embeddedness measures in categorical terms at first interview (e.g., whether or not someone has a partner but no child, or no partner and no child). In the supplementary analyses, we consider some alternative specifications, including time-varying measures of family embeddedness and ones where we distinguish married and partnered individuals and conduct separate analyses by child type (e.g., biological vs. other types of children).
Control Variables
We control for additional attributes associated with mortality and family structure. We control for age as a continuous variable, gender, and race/ethnicity (Non-Hispanic White, Non-Hispanic Black, Hispanic, or Non-Hispanic Other Race). We measure educational attainment at first interview (less than a high school degree, a high school degree/GED, some college, or a college degree).
Explanatory factors
We examine three explanatory factors that scholarship suggests may account for the association between older adult mortality and family structure through confounding or mediation mechanisms. The first is economic security, which we measure with total personal wealth excluding secondary residences. We chose this measure because it is asked at every interview. We also look at individual income in the last year. We log both measures of wealth and income to normalize the distributions. Health is the second explanatory factor we test to understand the relationships between mortality and family structure. We measure health with a series of variables. We include self-rated health, which we dichotomize into good health or better compared to fair/poor health. We also include the number of chronic conditions that respondents report in response to questions about hypertension, diabetes, cancer, chronic lung disease, heart attack/angina/congestive heart failure, stroke, emotional/nervous/psychiatric problems, and arthritis/rheumatism. The next health measures we examine are health behaviors: smoking (never, former, or current smoker), and whether the respondent engaged in multiple bouts of vigorous physical activity during the week. We use “at least once per week” to harmonize across waves. The last health measures we include are the number of IADL and ADLs with which the respondent reported needing help. We base each of these on responses to five questions: for IADLs, these include help using a telephone, taking medication, handling money, shopping, or preparing meals; for ADLS, they include help bathing, eating, dressing, walking across a room, and getting in or out of bed. The last explanatory factor is social connectedness, which we measure with loneliness and labor force participation. In all waves, the HRS collects a loneliness measure as part of the CES-D scale, which asks respondents whether or not they felt lonely much of the time over the week prior to the interview; in Wave 1, wording referred to most of the time or more. We also tested the full CES-D scale but found that it was less strongly associated with mortality than just the loneliness measure and had more missing data (not shown). Our second measure of social connectedness, labor force participation, categorizes respondents as either working full time, part-time, or not in the labor force. Note that labor force participation can also provide economic security, so it can be interpreted as contributing to both economic security and social connectedness. Alternatively, it may also function as a proxy for age or health status.
Results
Table 1 presents a classification of our sample by family embeddedness upon entry into the survey. It shows estimates of the weighted prevalence and sample size of U.S. adults age 50 and older with different combinations of kin. The descriptive statistics are nested so that interested readers can understand how the presence and absence of different family members contributes to the distribution. Considering family statuses, our weighted estimates suggest that 67.7% of U.S. older adults have a partner, 89.9% have at least one living child (64.5%+25.4%), and 88.5% have a living sibling (57.7%+2.8%+22.1%+5.9%). Thinking in terms of family embeddedness, the estimates also show the cross-classified estimates of whether people have or do not have partners, living children, and siblings. Counting family embeddedness as the cross-classification of partners and children, an estimated 64.5% of older adults have a living partner and at least one child and an estimated 3.2% have a partner and no children. We compared our estimate to the National Health and Aging Trends Study (NHATS), a nationally representative U.S. study of adults 65+ and find the weighted estimate for this group to be almost the same in 2015 (3.2%). These estimates suggest that 25.4% of older adults have no partner and at least one child, while 6.8% have no partner and no children. Last, the table presents an even more refined estimate of family embeddedness that accounts for whether or not people have living siblings, although the sample size becomes small in some cases. Only 0.4% (N=144 respondents) of U.S. older adults have a partner, no children, and no siblings, and 1.0% (N=272 respondents) of U.S. older adults have no partner, no children, and no siblings.
Figure 1 presents Kaplan Meier survivorship curves by family embeddedness defined as whether respondents had a partner and/or at least one living child at first interview. Respondents with both a partner and at least one child have the highest survival, followed by those with a partner but no children, then those with a child but no partner. Those with neither a partner nor child had the lowest survival. The differences in survival are large in magnitude. For instance, ten years after the first interview, older adults with a partner and at least one child had an 82.4% survival probability, compared with 69.8% for those with a partner but no child, 68.4% for those with a child but no partner, and 60.3% for those with neither type of kin. Both the logrank and Wilcoxon tests indicate significant differences in survival probabilities between these groups (p<.001).
Table 2 presents estimated survival probabilities to five, ten and twenty years for respondents with three different measures of family structure: family status, volume of family ties, and family embeddedness. The left side of Table 2 shows unadjusted, descriptive survival probabilities. There is a large degree of variation in unadjusted mortality across the three operationalisations, and the three measures show some key differences. For instance, by family status, 48.8% of older adults who have at least one child and may or may not have a spouse survive 20 years, compared to only 34.4% of older adults who have at least one child but no partner via the family embeddedness measure. Similarly, although the 20-year survival probability of older adults without any measured immediate kin is the same by family count and family embeddedness operationalizations, we see that 49.9% of those who have two or more family ties survive, but taking into account the type of kin – like having both a partner and a child – yields a 54.1% survival probability.
Adjusted survival probabilities on the right side of Table 2 show much less variation in mortality, but they still highlight some interesting distinctions across the three measures of family structure. For instance, an older adult with a “no partner” family status (i.e., someone who may or may not have a child) has a 64.7% probability of survival 20 years after entering the survey, but someone with no partner and no children has a 65.7% probability. Just as in the descriptive models on the left hand side, although our family embeddedness measure of having no kin mirrors a family count of zero, we see that even having two or more family ties has a 66.9% survival probability, but accounting for the types of ties – both a partner and a child, in our family embeddedness measures – yields a 67.4% 20 year survival probability.
Table 3 presents hazard ratios from multivariate survival models by family structure. Model 1 shows the results of a family status approach, indicating that respondents without a partner, and respondents without a child have elevated mortality risk, net of demographic control variables. The hazard ratio for lacking a partner is 1.31 (p<0.001), and it is 1.18 (p<0.001) for lacking a child. Model 2 measures the volume of family ties and finds no differences between those with one versus no ties, but that those with two or more family ties have a 24.9 percent reduction in the hazard ratio of mortality risk (HR 0.75, p<.001) compared to those with none, net of controls. Model 3 uses a family embeddedness approach and finds that compared to respondents with both a partner and child, older adults with no partner who have a child have a higher mortality risk (HR 1.33, p<0.001), followed by older adults who do have a partner but no child (HR1.30, p<0.001). Respondents with neither have the highest mortality risk (HR 1.48, p<0.001).
Models 4-6 in Table 3 examine how much of the associations between mortality and family structure are accounted for by the three sets of explanatory factors (economic security, health, and social connectedness). We find that the explanatory factors account for little of the mortality risk by family statuses for older adults with no children but some of the association for older adults with only a partner. Similarly, these factors account for some, but not all of the mortality risk associated with the volume of family ties. The results from Model 6 examining family embeddedness show that although economic security, physical health, and social connectedness are all important, mortality disadvantages persist for older adults lacking each type of kin compared to those with both a partner and child.
Table 4 examines mortality by family structure accounting for the presence/absence of siblings in addition to a partner and children. Similar to Table 3, when we compare Models 1, 2, and 3, we see greater variation in mortality risk captured by family embeddedness that we cannot see with singular family status variables in Model 1 or the volume of ties in Model 2. In Model 3, those without any kin have a 79 percent increase in their hazard ratio of mortality compared to older adults with all three kin types (HR 1.79 p<.001). Other family embeddedness groups also exhibit a wide range of mortality risk. Models 4, 5, and 6 show explanatory factors account for large portions of the elevated mortality risks in groups lacking different types of kin. However, just as in Table 3, these explanatory factors do not account for all the mortality differences that we observe. The multivariate models also show greater variation in mortality risk with the detailed measure of family embeddedness than with the other two simpler specifications.
We also test whether the associations between older adult mortality and family structure vary by gender and race. Because measures of family embeddedness captured greater variation in mortality than family status or volume of tie operationalisations, we show interactions only for this measure. Table 5 shows only coefficients from the main interactions, and the full results are shown in the supplemental digital content. Model 1 shows that the relationship between family embeddedness and mortality does not vary significantly by gender. Model 2 shows that most of the race/ethnicity interaction terms show no differences. The only one where we find differences between family embeddedness and mortality is for those with a partner but no child, and a child but no partner; These groups have a significantly lower association with mortality for non-Hispanic Black older adults than for non-Hispanic Whites. Many of the other coefficients in this model are negative, which offers some suggestive but not statistically significant evidence that the associations between mortality and different family embeddedness types may be less strong for racial minorities than for non-Hispanic White older adults.
Sensitivity analyses
Our supplemental digital content provides supplemental figures that extend the main analyses. Figure A shows the Kaplan Meier survivorship curves by family embeddedness by the availability of a partner, children, and siblings. Figure B presents adjusted survivorship curves from Table 3 Model 6. Figures C and D present adjusted survivorship curves by gender and race/ethnicity estimated from Table 5 Models 1 and 2.
The supplementary tables show results from several alternative specifications and descriptive statistics. Table A presents the descriptive statistics for our sample, broken down by family embeddedness. For alternative specifications, Table B tests whether measuring kin availability as time-varying shows different results from our main results which measure family structure at first interview. Our results show the same patterns as those in the main text but highlight that losing a sibling during the study is associated with a 13% increase in the risk of mortality. Table C tests whether distinguishing between partnered and married older adults, and between biological and non-biological children yields different results. The results are overall similar but shows that biological children are more protective than non-biological children for mortality. Tables D and E show the full models from Table 5 in the main text.
In addition to the results shown in the supplemental digital content, we also tested the robustness of the results to missing data: removing all missing data (i.e., excluding those with pre-filled and carried-over values) and estimating models with relevant flags for missing data in order to retain the original sample size both yielded similar patterns of results. Next, we re-estimated the survival analysis models using age instead of time in the survey and the results were similar (available upon request). We also tested a squared age term in our main models, finding that the results are similar (available upon request). Last, we used an alternative user-written package in Stata, -stmp2- to estimate parametric models that plot counterfactual survivals whereby each observation retains its values but the explicitly contrasted variables are changed and that also provide confidence intervals on figures (Lambert and Royston 2009; Lambert 2017). We re-estimate the models using this package and found similar results to those presented in the main text. All results from these supplementary analyses are available upon request.
Discussion
Demographic changes in fertility, mortality, and partnership are shifting family structures in the United States, and these changes may shape health and mortality in new ways. For older adults, changes in family structure might have particularly important consequences because older adults routinely turn to family members for social support (Verdery and Campbell 2019), companionship (Bookwala 2017), and help with disabilities and managing chronic conditions (August and Sorkin 2010; Margolis 2013b; Margolis and Wright 2017). Many studies consider associations between older adult mortality and different family structure variables, such as being partnered or having children, partnership history, or the volume of family ties available. Drawing on important theoretical distinctions, we examine various operationalizations of family structure and show the different patterns that can be seen from the empirical data. Our analysis examines three different operationalizations of family structure, including partners, children, and siblings. Although various recent studies in Europe and the U.S. have examined novel operationalizations of family structure (Kravdal et al. 2012; O’Flaherty et al. 2016; Kalmijn 2017; Franke and Kulu 2018), research has not explicitly compared across measures of family structure and their relationship with mortality.
To better understand family as a social determinant of health (Russell et al. 2018) and specifically mortality, theoretical models suggest that family embeddedness is particularly important in offering a nuanced understanding of older adult mortality patterns compared to a focus on family status variables or a focus only on the volume of ties available. Using measures of family embeddedness, we find substantial heterogeneity within mortality patterns that would otherwise be obscured when looking only at individual family status variables or the volume of ties. This may be because of the tendency for resources and obligations to be allocated in broader family systems, and that accounting the set of available family members best captures variation in older adult mortality. For instance, considering just partners and children, we consistently find that those with neither of these types of family members have the highest mortality hazards. Those with both a partner and child have the lowest mortality risks, and those with just a partner (and no child) or just a child (and no partner) are in between. Additionally, only accounting for the number of family ties available masks the unique mortality risks associated with more nuanced measures of family embeddedness. For instance, although having more family ties is associated with a reduction in mortality risk, our family embeddedness measures show that having some ties (e.g. a partner) but not others (e.g. a child) is actually associated with an increased mortality risk – so the simple count of family ties does not matter as much as the type of constellations available to older adults. These findings are robust to numerous controls and key explanatory factors. Considering siblings, we find that those with no family or just one of the family member types (only a partner, only a child, or only a sibling) have high mortality risks, while those with two types (a partner and child but no sibling, a partner and sibling but no child, or a child and sibling but no partner) have intermediate mortality risks. Again, the lowest risks are among those with all three types of family members available. Similar to our findings on just partners and children, accounting for the different constellations of family members available to older adults shows more nuanced patterns of mortality risk compared to measuring individual family statuses or the simple count of family ties available.
This article offers one way that family embeddedness can be operationalised to study mortality outcomes and to advance our understanding of how family functions as a key social determinant of health in the U.S. Breaking down the conjoint availability of different types of family members highlights the interactive character of family availability and the potentially layered nature of family-related disadvantage in older adulthood, similar to how research on intersectionality examines matrices of disadvantage (Crenshaw 1991). However, there are many other ways that a family embeddedness perspective could be put into practice. Our sensitivity analyses in the supplemental digital content examining non-marital partners and non-biological children is one, for instance, but it is far from the only one. Embeddedness can also be extended beyond traditional notions of who is family, as other types of social support may increase in importance as traditional family networks shrink.
We examined the extent to which different explanatory factors contribute to the associations between mortality hazards and family structure: economic security, health, and social connectedness. Together they explain a substantial portion of the associations between mortality and family, but persistent associations remain even after accounting for these explanatory factors. The persistence of these associations suggests family structure plays an important role in older adult mortality, a role that likely goes beyond selection and mediation along these dimensions. For instance, family members may reduce the mortality risks of older adults by helping to manage chronic illnesses (Margolis and Wright 2017) or providing direct care when formal care is unavailable, especially for those who cannot afford paid care (Charles and Sevak 2005). Families may also provide a sense of “meaning” for older adults which may improve outcomes (Taylor et al. 2018), even net of reported loneliness and other forms of social connectedness. Other understudied family characteristics may also matter for explaining mortality patterns, for instance the educational attainment of key family members (Friedman and Mare 2014; Wolfe et al. 2018). Future work may attempt to account for the role of confounders and mediators with more complex modeling strategies, including marginal structural models.
Motivated by a literature that has come to emphasize group-level stratification in older adult family structure and health (Klinenberg 2002; Umberson 2017), we also tested whether the associations between mortality hazards and family embeddedness differ by race and gender subgroups in the population. We find few statistically significant interactions between family embeddedness and gender or race/ethnicity, but patterns suggesting that family embeddedness may differ by demographic group. However, sample sizes within different racial/ethnic groups are small, which increases the chances of obtaining such null results. Indeed, the direction of the coefficients in the models that interact the focal variables with race and gender offer some suggestive evidence that there may be group-level stratification in these relationships, specifically that the associations may be less strong for non-White than for White older adults and stronger for men than women. Such findings deserve further investigation.
Our analysis is constrained by available data. We cannot account for the full diversity of meaningful kin types present in the contemporary United States or all of the ways through which families can affect health and mortality. For example, the HRS does not distinguish between types of siblings (biological vs. step). In general, the role of siblings in the health and well-being of older adults is understudied. We find that sibling availability is important for older adults’ mortality risk. For instance, in our supplemental results, we find that the death of a sibling during participation in the survey is the only loss associated with higher mortality risk. This could be because siblings provide important resources and support (Voorpostel and Van Der Lippe 2007) especially at older ages (Connidis and Campbell 1995), or that they are particularly important when older adults do not have others to turn to (Pinquart 2003). We also do not examine interaction frequency, geographic proximity, or intergenerational transfers between family members. Instead, we concentrate on whether respondents have living kin, which is a necessary condition for any transfers or support; our estimates are likely to be conservative because they include all kin, rather than only considering those with whom respondents are close. We also cannot account for relationship quality, which might matter for the degree of social support and effects on one’s health.
Our supplemental analyses tested time-varying changes in available family members and found that most results were similar to those examining kin availability at first interview. This did not capture historical changes in partnership and fertility, nor the timing of, that occurred before the start of the survey, which have been shown to be important in shaping adults’ health and mortality (Doblhammer 2000; Berntsen and Kravdal 2012; Kravdal et al. 2012; O’Flaherty et al. 2016). Some of the groups we examine (either with certain family members available at baseline or those that lose family members over the course of the study) are small (e.g older adults with a partner but no children or siblings). Studying such quantitatively rare but theoretically important groups using a diversity of methods is an important direction to supplement knowledge about the outcomes for older adults in these unusual family forms.
Our main analysis focused on spouses, biological children, and siblings, and in the supplementary analysis, we also included non-marital partners and non-biological children. Future research could also consider additional family members such as parents, grandchildren, and extended kin like cousins. Ongoing changes in families have led some to speculate that others will fill some of the gaps. Step-relations, friends and other non-family ties are thought to be increasingly important (Latham-Mintus 2019; Mair 2019;) but unfortunately, few studies have substantial measurement of such ties. Other research finds that other forms of social engagement like volunteering (Okun, Yeung, and Brown 2013) and religious service attendance can be important for health and well-being (Litwin 2007), but we did not have consistent measures of these types of social activities in the majority of HRS waves. Further, the effect of certain family members and family embeddedness may change with age or across cohorts (Hurt, Ronsmans, Thomas 2006). For instance, families may be especially critical at the end of life, as major decisions and health tasks must be managed; more research is warranted. Future research should consider how families are one component of the broader health environments in which older adults are situated (Russell et al. 2018).
Studies have long examined the links between families and mortality. As the family structures of older adults have become more complex, and inequalities more layered upon each other than in the past (Carr 2019), it is important to examine how older adult mortality risks are distributed across contemporary family forms with a family embeddedness perspective. In this study, the most disadvantaged in terms of mortality are older adults who lack any measured family. Recent research shows that this group is not inconsequential in size, with 6.6% of adults 55 and above in the United States with no partner or children in 1998-2010 (Margolis and Verdery 2017); other work projects that the prevalence of this group will rise in the near future across a variety of contexts (Verdery and Margolis 2017; Verdery 2019). Policymakers of the future may face challenges posed by a growing population of older adults without close family members – a group with high mortality risk, poorer health, and lower economic security and social connections. To continue to improve the well-being of older adults, research must attend to the changing nature of families in contemporary society.
Supplementary Material
Acknowledgements
This work was supported by the National Institute on Aging of the National Institutes of Health (T32AG000221), the Joint Programming Initiative, More Years Better Lives funding from the Canadian Institute of Health Research (MYB150262), and Social Sciences and Humanities Research Council (435-2017-0618; 890-2016-9000). Additionally, we acknowledge assistance provided by a National Institute of Aging Award (R01AG060949) and the Penn State Population Research Institute, which is supported by an infrastructure grant by the Eunice Kennedy Shriver National Institute of Child Health and Human Development (P2CHD041025). The HRS (Health and Retirement Study) is sponsored by the National Institute on Aging (U01AG009740) and is conducted by the University of Michigan. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
References
- Anxo Dominique, Ericson Thomas, and Miao Chizheng. 2019. Impact of late and Prolonged Working Life on Subjective Health: The Swedish Experience, European Journal of Health Economics 20(3): 389–405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- August Kristin J. and Sorkin Dara H.. 2010. Marital Status and Gender Differences in Managing a Chronic Illness: The Function of Health-Related Social Control, Social Science and Medicine 71(10): 1831–1838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barclay Kieron and Kolk Martin. 2018. Parity and Mortality: An Examination of Different Explanatory Mechanisms Using Data on Biological and Adoptive Parents, European Journal of Population 35: 63–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bengtson Vern L. 2001. Beyond the Nuclear Family: The Increasing Importance of Multigenerational Bonds, Journal of Marriage and Family 63(1): 1–16. [Google Scholar]
- Benson Jacquelyn J. and Coleman Marilyn. 2016. Older Adults Developing a Preference for Living Apart Together, Journal of Marriage and Family 78(3): 797–812. [Google Scholar]
- Berntsen Kjersti N. and Kravdal Øystein. 2012. The Relationship between Mortality and Time Since Divorce, Widowhood or Remarriage in Norway. Social Science and Medicine 75(12): 2267–2274. [DOI] [PubMed] [Google Scholar]
- Bobak Martin, Murphy Michael, Rose Richard, and Marmot Michael. 2003. Determinants of Adult Mortality in Russia: Estimates from Sibling Data, Epidemiology 14(5): 603–611. [DOI] [PubMed] [Google Scholar]
- Bookwala Jamila. 2017. Confidant Availability (In)Stability and Emotional Well-Being in Older Men and Women, Gerontologist 57(6): 1041–1050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bronfenbrenner Urie. 1986. Ecology of the Family as a Context for Human Development: Research Perspectives, Developmental Psychology 22(6): 723–742. [Google Scholar]
- Brown Susan L. and Lin I-Fen. 2012. The Gray Divorce Revolution: Rising Divorce Among Older Adults, Journals of Gerontology - Series B Social Sciences 67(6): 731–741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown Susan L., Lin I-Fen, Hammersmith Anna M., and Wright Matthew R.. 2018. Later Life Marital Dissolution and Repartnership Status: A National Portrait, Journals of Gerontology - Series B Social Sciences 73(6): 1032–1042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown Susan L., Lin I-Fen, Hammersmith Anna M., and Wright Matthew R.. 2019. Repartnering Following Gray Divorce: The Roles of Resources and Constraints for Women and Men, Demography 56(2): 503–523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bryant Sharon and Rakowski William. 1992. Predictors of Mortality Among Elderly African-Americans, Research on Aging 14(1): 50–67. [Google Scholar]
- Carr Deborah. 2019. Golden Years? Social Inequality in Later Life. Russell Sage Foundation. [Google Scholar]
- Charles Kerwin Kofi and Sevak Purvi. 2005. Can Family Caregiving Substitute for Nursing Home Care?, Journal of Health Economics 24(6): 1174–1190. [DOI] [PubMed] [Google Scholar]
- Connidis Ingrid A. 1994. Sibling Support in Older Age, Journal of Gerontology: Social Sciences 49(6): S309–18. [DOI] [PubMed] [Google Scholar]
- Connidis Ingrid Arnet and Campbell Lori D.. 1995. Closeness, Confiding, and Contact Among Siblings in Middle and Late Adulthood, Journal of Family Issues 16(6): 722–745. [Google Scholar]
- Cox Martha J. and Paley Blair. 2003. Understanding Families as Systems, Current Directions in Psychological Science 12(5): 193–196. [Google Scholar]
- Crenshaw Kimberle. 1991. Mapping the Margins: Intersectionality, Identity Politics, and Violence against Women of Color, Stanford Law Review 43(6): 1241–1299. [Google Scholar]
- Cross Christina J. 2019. Racial/Ethnic Differences in the Association Between Family Structure and Children’s Education, Journal of Marriage and Family 82(8): 691–712. [Google Scholar]
- Doblhammer Gabrielle. 2000. Reproductive History and Mortality Later in Life: A Comparative Study of England and Wales and Austria, Population Studies 54(2): 169–176. [DOI] [PubMed] [Google Scholar]
- Elwert Felix and Christakis Nicholas A.. 2008. Wives and Ex-Wives: A New Test for Homogamy Bias in the Widowhood Effect, Demography 45(4): 851–873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eng PM, Rimm EB, Fitzmaurice G, & Kawachi I 2002. Social Ties and Change in Social Ties in Relation to Subsequent Total and Cause-specific Mortality and Coronary Heart Disease Incidence in Men. American Journal of Epidemiology 155(8): 700–709. [DOI] [PubMed] [Google Scholar]
- Fingerman Karen L. and Bermann Eric. 2000. Applications of Family Systems Theory to the Study of Adulthood, International Journal of Aging & Human Development 51(1): 5–29. [DOI] [PubMed] [Google Scholar]
- Fitzpatrick Maria D. and Moore Timothy J.. 2018. The Mortality Effects of Retirement: Evidence from Social Security Eligibility at Age 62, Journal of Public Economics 157(January): 121–137. [Google Scholar]
- Flippen Chenoa and Tienda Marta. 2000. Pathways to Retirement: Patterns of Labor Force Participation and Labor Market Exit Among the Pre-Retirement Population by Race, Hispanic Origin, and Sex, Journal of Gerontology: Social Sciences 55(I): 14–27. [DOI] [PubMed] [Google Scholar]
- Franke Sebastian and Kulu Hill. 2018. Mortality Differences by Partnership Status in England and Wales: The Effect of Living Arrangements or Health Selection? European Journal of Population 34(1): 87–118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Friedman Esther M. and Mare Robert D.. 2014. The Schooling of Offspring and the Survival of Parents, Demography 51(4): 1271–1293. [DOI] [PubMed] [Google Scholar]
- Gakidou Emmanuela E. and King Gary. 2006. Death by Survey: Estimating Adult Mortality Without Selection Bias From Sibling Survival Data, Demography 43(3): 569–585. [DOI] [PubMed] [Google Scholar]
- Granovetter Mark. 1985. Economic Action and Social Structure: The Problem of Embeddedness, American Journal of Sociology 91(3): 481–510. [Google Scholar]
- Grundy Emily and Kravdal Øystein. 2010. Fertility History and Cause-Specific Mortality: A Register-Based Analysis of Complete Cohorts of Norwegian Women and Men, Social Science and Medicine, 70(11): 1847–1857. [DOI] [PubMed] [Google Scholar]
- Hank Karsten. 2010. Childbearing History, Later-Life Health, and Mortality in Germany, Population Studies 64(3): 275–291. [DOI] [PubMed] [Google Scholar]
- Health and Retirement Survey. 2017. Sample Sizes and Response Rates. Ann Arbor, MI: University of Michigan; Available: https://hrs.isr.umich.edu/sites/default/files/biblio/ResponseRates_2017.pdf (accessed: December 2019). [Google Scholar]
- Hemez Paul and Brown Susan L.. 2016. Cohabitation in Middle and Later Life. Bowing Green, OH: Family Profiles; Available: https://www.bgsu.edu/content/dam/BGSU/college-of-arts-and-sciences/NCFMR/documents/FP/fp-16-20-hemez-brown-cohab.pdf (accessed: December 2019). [Google Scholar]
- Henretta John C. 2007. Early Childbearing, Marital Status, and Women’s Health and Mortality after Age 50, Journal of Health and Social Behavior 48(3): 254–266. [DOI] [PubMed] [Google Scholar]
- Högnäs Robin S., Roelfs David J., Shor Eran, Moore Christa, and Reece Thomas. 2017. J-Curve? A Meta-Analysis and Meta-Regression of Parity and Parental Mortality, Population Research and Policy Review 36(2): 273–308. [Google Scholar]
- Hurt Lisa S., Ronsmans Carine, & Thomas Sara L. 2006. The Effect of Number of Births on Women’s Mortality: Systematic Review of the Evidence for Women Who Have Completed Their Childbearing, Population Studies 60(1): 55–71. [DOI] [PubMed] [Google Scholar]
- Kalmijn Matthijs, 2017. The Ambiguous Link between Marriage and Health: A Dynamic Reanalysis of Loss and Gain Effects, Social Forces 95(4): 1607–1636. [Google Scholar]
- Kaplan Robert M. and Kronick Richard G.. 2006. Marital Status and Longevity in the United States Population, Journal of Epidemiology and Community Health 60(9): 760–765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keizer Renske, Dykstra Pearl A., and Van Lenthe Frank J.. 2012. Parity and Men’s Mortality Risks, European Journal of Public Health 22(3): 343–347. [DOI] [PubMed] [Google Scholar]
- Klinenberg Eric. 2002. Heat Wave: A Social Autopsy of Disaster in Chicago. Chicago, IL: University of Chicago Press. [DOI] [PubMed] [Google Scholar]
- Klinenberg Eric. 2013. Going Solo: The Extraordinary Rise and Surprising Appeal of Living Alone. New York, NY: Penguin. [Google Scholar]
- Kravdal Øystein, Grundy Emily, Lyngstad Torkild H., & Wiik Kenneth A. 2012. Family Life History and Late Mid-life Mortality in Norway, Population and Development Review 38(2): 237–257. [Google Scholar]
- Lambert Paul C. 2017. Standardized Survival Functions. Available: https://pclambert.net/software/standsurv/standardized_survival/ (accessed: December 2019).
- Lambert Paul C. and Royston Patrick. 2009. Further Development of Flexible Parametric Models for Survival Analysis, Stata Journal 9(2): 265–290. [Google Scholar]
- Latham-Mintus Kenzie. 2019. A Friend in Need? Exploring the Influence of Disease and Disability Onset on the Number of Close Friends Among Older Adults, The Journals of Gerontology: Series B 74(8): e119–e124. [DOI] [PubMed] [Google Scholar]
- Lillard Lee A. and Panis Constantijn. 1996. Marital Status and Mortality: The Role of Health, Demography 33(3): 313–327. [PubMed] [Google Scholar]
- Lin I. Fen, Brown Susan L., and Jean Cupka Cassandra. 2018. A National Portrait of Stepfamilies in Later Life, Journals of Gerontology - Series B Social Sciences 73(6): 1043–1054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Litwin Howard. 2007. What Really Matters in the Social Network-Mortality Association? A Multivariate Examination among Older Jewish-Israelis, European Journal of Ageing 4(2): 71–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luo Ye, Hawkley Louise C., Waite Linda J., and Cacioppo John T.. 2012. Loneliness, Health, and Mortality in Old Age: A National Longitudinal Study, Social Science and Medicine 74(6): 907–914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mair Christine A. 2019. Alternatives to Aging Alone?: ‘Kinlessness’ and the Importance of Friends across European Contexts, The Journals of Gerontology: Series B 74(8): 1416–1428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mair CA 2010. Social Ties and Depression: An Intersectional Examination of Black and White Community-Dwelling Older Adults. Journal of Applied Gerontology 29(6): 667–696. 10.1177/0733464809350167 [DOI] [Google Scholar]
- Margolis Rachel. 2013a. Educational Differences in Healthy Behavior Changes and Adherence Among Middle-Aged Americans, Journal of Health and Social Behavior 54(3): 353–368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Margolis Rachel. 2013b. Health Shocks in the Family: Gender Differences in Smoking Changes, Journal of Aging and Health 25(5): 882–903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Margolis Rachel and Verdery Ashton M.. 2017. Older Adults Without Close Kin in the United States, Journals of Gerontology - Series B Social Sciences 72(4): 688–693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Margolis Rachel and Wright Laura. 2017. Older Adults With Three Generations of Kin: Prevalence, Correlates, and Transfers, The Journals of Gerontology Series B: Social Sciences 72(6): 1067–1072. [DOI] [PubMed] [Google Scholar]
- Morgan S. Philip and Taylor Miles G.. 2006. Low Fertility at the Turn of the Twenty-First Century, Annual Review of Sociology 32: 375–399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Noël Reginald A. 2018. Race, Economics, and Social Status. Washington, DC: Bureau of Labor Statistics; Available: https://www.bls.gov/spotlight/2018/race-economics-and-social-status/pdf/race-economics-and-social-status.pdf (accessed December 2019). [Google Scholar]
- O’Flaherty Martin, Baxter Janeen, Haynes Michele, & Turrell Gavin. 2016. The Family Life Course and Health: Partnership, Fertility Histories, and Later-life Physical Health Trajectories in Australia Demography 53(3): 777–804. [DOI] [PubMed] [Google Scholar]
- Okun Morris A., Heung Yeung Ellen Wan, and Brown Stephanie. 2013. Volunteering by Older Adults and Risk of Mortality: A Meta-Analysis, Psychology and Aging 28(2): 564–77. [DOI] [PubMed] [Google Scholar]
- Parsons Talcott. 1943. The Kinship System of the Contemporary United States, American Anthropologist 45(1): 22–38. [Google Scholar]
- Perls Thomas T., Wilmoth John, Levenson Robin, Drinkwater Maureen, Cohen Melissa, Bogan Hazel, Joyce Erin, Brewster Stephanie, Kunkel Louis, and Puca Annibale. 2002. Life-Long Sustained Mortality Advantage of Siblings of Centenarians, Proceedings of the National Academy of Sciences of the United States of America 99(12): 8442–8447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pinquart Martin. 2003. Loneliness in Married, Widowed, Divorced, and Never-Married Older Adults, Journal of Social & Personal Relationships 20(1): 31–53. [Google Scholar]
- Raley R. Kelly and Sweeney Megan M.. 2007. What Explains Race and Ethnic Variation in Cohabitation, Marriage, Divorce, and Nonmarital Fertility? Los Angeles, CA: UCLA California Center for Population Research; Available: https://escholarship.org/uc/item/82n1b82v (retrieved December 2019). [Google Scholar]
- RAND Center for the Study of Aging, with funding from the National Institute on Aging and the Social Security Administration. 2016. RAND HRS Data, Version P. [Google Scholar]
- Rendall Michael S., Weden Margaret M., Favreault Melissa M., and Waldron Hilary. 2011. The Protective Effect of Marriage for Survival: A Review and Update, Demography 48(2): 481–506. [DOI] [PubMed] [Google Scholar]
- Reyes Adriana M., Hardy Melissa, and Pavalko Eliza. 2018. Race Differences in Linking Family Formation Transitions to Women’s Mortality, Journal of Health and Social Behavior 59(2): 231–247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roelfs David J., Shor Eran, Kalish Rachel, and Yogev Tamar. 2011. The Rising Relative Risk of Mortality for Singles: Meta-Analysis and Meta-Regression, American Journal of Epidemiology 174(4): 379–389. [DOI] [PubMed] [Google Scholar]
- Rogers Richard G., Everett Bethany G., Saint Onge Jarron M., and Krueger Patrick M.. 2010. Social, Behavioral, and Biological Factors, and Sex Differences in Mortality, Demography 47(3): 555–578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Russell Luke T., Coleman Marilyn, and Ganong Lawrence. 2018. Conceptualizing Family Structure in a Social Determinants of Health Framework, Journal of Family Theory and Review 10(4): 735–748. [Google Scholar]
- Sabbath Erika L., Guevara Ivan M., Glymour M. Maria, & Berkman Lisa F. 2015. Use of Life Course Work–Family Profiles to Predict Mortality Risk among US Women. American Journal of Public Health, 105(4), e96–e102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seltzer Judith A. 2019. Family Change and Changing Family Demography, Demography 56(2): 405–426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shor Eran, Roelfs David J., and Yogev Tamar. 2013. The Strength of Family Ties: A Meta-Analysis and Meta-Regression of Self-Reported Social Support and Mortality, Social Networks 35(4): 626–638. [Google Scholar]
- Shye Diana, Mullooly John P., Freeborn Donald K., and Pope Clyde R.. 1995. Gender Differences in the Relationship between Social Network Support and Mortality, Social Science & Medicine 41(7): 935–947. [DOI] [PubMed] [Google Scholar]
- Smock Pamela J., Manning Wendy D., and Porter Meredith. 2005. ‘Everything’s There except Money’: How Money Shapes Decisions to Marry among Cohabitors, Journal of Marriage and Family 67(3): 680–696. [Google Scholar]
- Sonnega A, Faul JD, Ofstedal MB, Langa KM, Phillips JW, & Weir DR 2014. Cohort profile: the health and retirement study (HRS). International journal of epidemiology, 43(2), 576–585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sorlie P, Rogot E, Anderson R, Johnson NJ, and Backlund E. 1992. Black-White Mortality Differences by Family Income, The Lancet 340(8815): 346–350. [DOI] [PubMed] [Google Scholar]
- Stack Carol B. 1975. All Our Kin: Strategies for Survival in a Black Community. Basic Books. [Google Scholar]
- Tamborini Christopher R. 2007. The Never-Married in Old Age: Projections and Concerns for the near Future, Social Security Bulletin 67(2): 25–40. [PubMed] [Google Scholar]
- Taylor John, McFarland Michael J., and Carr Dawn C.. 2018. Age, Perceptions of Mattering, and Allostatic Load, Journal of Aging and Health 31(10): 1830–1849. [DOI] [PubMed] [Google Scholar]
- Umberson Debra. 2017. Black Deaths Matter: Race, Relationship Loss, and Effects on Survivors, Journal of Health and Social Behavior 58(4): 405–420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Umberson Debra, Crosnoe Robert, and Reczek Corinne. 2010. Social Relationships and Health Behavior Across the Life Course, Annual Review of Sociology 36: 139–157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- University of Michigan. 2018. Health and Retirement, Public Use Dataset. [Google Scholar]
- Verdery Ashton M. 2019. Modeling the Future of China’s Changing Family Structure to 2100, Eberstadt N (ed), China’s Changing Family Structure: Dimensions and Implications. Washington, DC: AEI Press, pp. 23–78. [Google Scholar]
- Verdery Ashton M. 2015. Links Between Demographic and Kinship Transitions, Population and Development Review 41(3): 465–484. [Google Scholar]
- Verdery Ashton and Campbell Colin. 2019. Social Support in America: Stratification and Trends in Access over Two Decades, Social Forces 98(2): 725–752. [Google Scholar]
- Verdery Ashton M. and Margolis Rachel. 2017. Projections of White and Black Older Adults without Living Kin in the United States, 2015 to 2060, Proceedings of the National Academy of Sciences 114(21): 11109–11114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Verdery Ashton M., Margolis Rachel, Zhou Zhangjun, Chai Xiangnan, and Rittirong Jongjit. 2019. Kinlessness Around the World, The Journals of Gerontology: Series B 74(8): 1394–1405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Voorpostel Marieke and Tanja Van Der Lippe. 2007. Support between Siblings and between Friends: Two Worlds Apart? Journal of Marriage and Family 69(5): 1271–1282. [Google Scholar]
- Wachter Kenneth W. 1997. Kinship Resources for the Elderly, Philosophical Transactions of the Royal Society B: Biological Sciences 352(1363): 1811–1817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Waite Linda J. 1995. Does Marriage Matter? Demography 32(4): 483–507. [PubMed] [Google Scholar]
- Waldron Ingrid, Hughes Mary Elizabeth, and Brooks Tracy L.. 1996. Marriage Protection and Marriage Selection - Prospective Evidence for Reciprocal Effects of Marital Status and Health, Social Science and Medicine 43(1): 113–123. [DOI] [PubMed] [Google Scholar]
- Weir David R. 2016. Validating Mortality Ascertainment in the Health and Retirement Study. Available: https://hrs.isr.umich.edu/sites/default/files/biblio/Weir_mortality_ascertainment.pdf (retrieved December 2019).
- Wolfe Joseph, Bauldry Shawn, Hardy Melissa A., and Pavalko Eliza K.. 2018. Multigenerational Attainments, Race, and Mortality Risk among Silent Generation Women, Journal of Health and Social Behavior 59(3): 335–51. [DOI] [PubMed] [Google Scholar]
- Zhou Zhangjun, Verdery Ashton M., and Margolis Rachel. 2018. No Spouse, No Son, No Daughter, No Kin in Contemporary China: Prevalence, Correlates, and Differences in Economic Support, The Journals of Gerontology: Series B 74(8): 1453–1462. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


