Abstract
Purpose:
To report on the development of the Schiøtz tonometer and to put its subsequent role into perspective with regard to the history of glaucoma, the career of Hjalmar Schiøtz (1850–1927), and the evolution of the tonometer leading up to the development of the Goldmann tonometer.
Introduction:
The story of physicians’ attempts to assess intraocular pressure goes back many centuries. Mechanical instruments designed for this purpose were first introduced in the latter part of the 19th century, but did not gain traction until the introduction of the Schiøtz tonometer in 1905. This report reviews details about this instrument, its inventor and its role in glaucoma treatment.
In the 5th century B.C., Hippocrates, the father of modern medicine, taught that experienced doctors were aware that the laying on of hands could relieve pain, induce healing, and be informative to the physician (Ref. 1, 2). In a similar manner, palpation of the eye appears to have been employed in cases of ocular disease. Palpation of the eye through the lids to determine the globe’s hardness or softness probably preceded any concept of glaucoma as a disease (Ref. 3).
In ancient Greece, glaucos was sometimes used to describe diseased eyes in which the pupil or iris appeared light blue, grey, or green (Ref. 3). Galen associated the glaucos with a hard crystalline lens and later authors such as Celsus and Avicenna advocated palpation of the eye to determine if the intraocular humors had hardened and to estimate maturity of the cataract prior to couching (Ref. 3). An English eye physician, Richard Banister, in his Breviary (1622) (Ref. 4) is generally credited as the first to appreciate that elevation of intraocular pressure (IOP) was recognizable by the globe’s resistance to palpation, and, if present, was a distinct sign of ocular disease (Ref. 5). Thirty-four years later, Felix Platter observed that the glaucomatous eye was hard (Ref. 6).
It was, however, almost 200 years later that Sir William Bowman suggested to physicians at the meeting of the British Medical Association in 1826 to employ digital tonometry in the diagnosis of ocular disease (Ref. 7). And 26 years after that Bowman noted: “I have long paid special attention to the subject of the tension of the globe…and have found it possible and practically useful to distinguish nine degrees of tension” (Ref. 7).
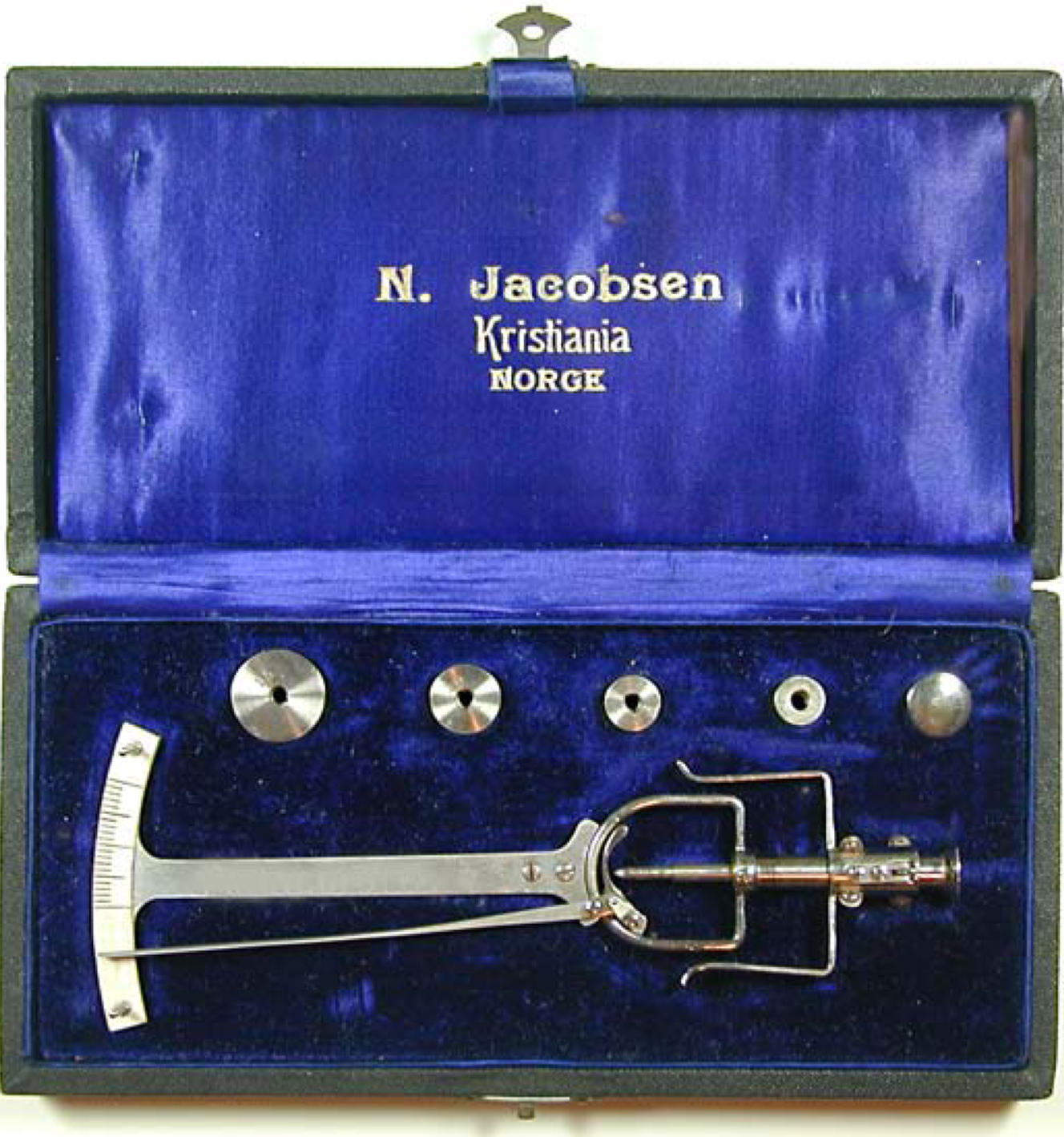
The first attempts at developing tonometry using a mechanical instrument were apparently made by Albrecht von Graefe. Graefe (Fig. 1) mentioned his initial trials with instrumental tonometry (Fig. 2) in a letter to Frans Cornelis Donders in 1862, but apparently his instruments advanced only to the prototype stage (Ref 8). The earliest impression tonometers that were actually built and found their way into clinical use were developed in Donders’ clinic in Utrecht between 1863 and 1868 (Ref. 9, 10, 11, 12). The foot plate was applied to the sclera following determination of the scleral curvature, and the IOP estimated according to the depth of the indentation. More refined variations of the Donders’ tonometer followed from Priestley Smith (Ref. 13), (1879 and 1887) and F. Layerat (1885) (Ref. 14).
Figure 1.
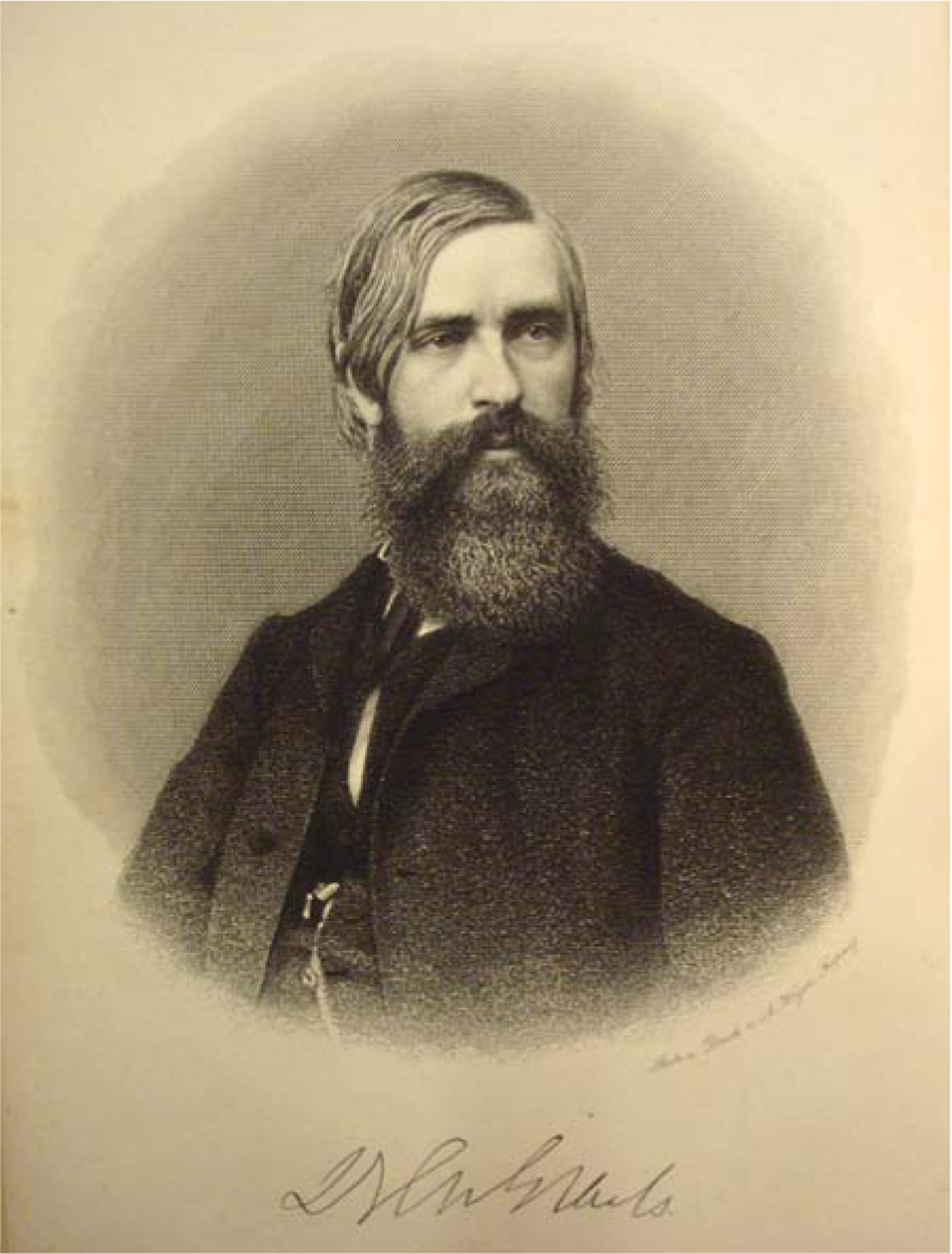
Albrecht von Graefe. Courtesy of Richard Keeler, FRCOphth (Hon), Honorary Curator, The Royal College of Ophthalmologists. Open source.
Figure 2.

von Graefe Tonometer. Courtesy Tonkelaar, I den et al. Eye and Instruments.
The introduction of cocaine corneal anesthesia by Karl Koller in 1884 (Ref. 15, 16) allowed tonometers to be applied directly to the cornea. Using this better defined and anatomically more uniform site led to more consistent measurements. A fundamental source of error in all these early tonometers was noted by Adolf Weber in 1867: The indention of the sclera and cornea displaced a sufficient quantity of intraocular fluid to alter the pressure it was intended to measure (Ref. 16). To address this problem, Weber designed the first applanation tonometer, designed to measure the IOP with only minimal fluid displacement. The leaders in the glaucoma field at this time failed to appreciate the concept of a perfect applanation point without fluid displacement and Weber’s tonometer did not gain wide acceptance. A few years later, in 1885, C. L. Maklakoff (Ref. 17), who was unaware of Weber’s work, introduced a more advanced tonometer (Fig. 3) designed on the applanation concept. It is generally considered to be the first reasonably accurate instrument produced before 1900.
Figure 3.

Maklakoff tonometer circa 1885. Courtesy of Richard Keeler, FRCOphth (Hon), Honorary Curator, The Royal College of Ophthalmologists.
Armand Imbert in France (Ref. 18), and Adolf Eugen Fick (Ref. 19), in Germany, each independently provided critical research results regarding the design of an improved applanation tonometer. They showed that when the application of the tonometer produces a flat surface, forces cancel each other and the reading of the tonometer equals the IOP. This proved critical in Hans Goldmann’s development of the Goldmann tonometer and he termed this the “Imbert-Fick Law (Ref. 20). Fick himself designed a tonometer but it did not gain popularity.
Approximately 15 tonometers were described in the literature before the beginning of the 20th century. The Maklakoff improved model of 1892 (Fig. 3), although complicated and difficult to use continued to be employed in Russia and Eastern Europe until the end of the 20th century (Ref. 21). Apart from that instrument, none of the others met the requirements of a reliable and clinically useful instrument and none found its way into the practice of ophthalmology. As the 20th century dawned, digital tonometry, as propounded by Bowman, remained as the unrivaled standard method of determining IOP.
In 1905, Hjalmar Schiøtz (1850–1927) (Fig. 4), a Norwegian ophthalmologist, inventor, and innovator, introduced his indentation tonometer (Fig. 5) (Ref. 22). A half century later, in an article published posthumously in 1957, Jonas S. Friedenwald (Fig. 6) wrote: “It is difficult after the lapse of so many years to gain a clear idea of the magnitude and solidity of Hjalmar Schiøtz’s contribution. During these years, the Schiøtz tonometer became the ‘gold standard’ for the measurement of intraocular pressure (Ref. 23).” It was simple, rugged, and for an indentation tonometer, remarkably precise and rapidly gained epithet of “the first clinically useful tonometer.” The instrument has a relatively flat foot plate of 15mm radius curved to match the average human corneal curvature. It deforms most corneas to a uniform, somewhat flattened state which becomes the plane of reference for the indentation.
Figure 4.

Portrait of Hjalmar Schiøtz (1850–1927). Courtesy Otto Johansen, Hjalmar Schiøtz (1850–1927), 1999/2000.
Figure 5.
Schiøtz tonometer. Courtesy of Richard Keeler, FRCOphth (Hon), Honorary Curator, The Royal College of Ophthalmologists.
Figure 6.

Dr. Jonas S. Friedenwald. Courtesy of Peter J. McDonnell, M.D., Chairman of the Wilmer Eye Institute, Johns Hopkins Medicine.
The Schiøtz tonometer functions in the following manner: “Gravity provides a known force on a weighted metal plunger. The plunger rides inside a metal cylinder attached to a foot plate. The top of the plunger rides along a curved lever that attaches to a pointer, which in turn rides along a scale. For each 0.05 mm that the plunger sinks below the level of the footplate, the pointer moves up 1 scale unit. Thus the lower the IOP, the farther into the cornea the plunger sinks and the higher the scale reading….” (Ref. 8). “….The scale measuring the amount of indentation is linear. The relation between the amount of indentation and intraocular pressure is… logarithmic, so that the higher IOP values are compressed toward the lower end of the scale.” (Ref. 8, 23). The original calibrations between the scale readings and the IOP were done in conjunction with manometry readings in artificial eyes and cadavers. Schiøtz’s brother, a physicist, helped him convert the tonometer readings into millimeters of mercury of IOP (Ref. 24).
Hjalmar August Schiøtz, was a major figure in late 19th and early 20th century ophthalmology in his native Norway and on the European continent. He was less well recognized in England and the United States since he published almost exclusively in Norwegian and German. He attended medical school in Oslo and trained in ophthalmology with Karl Ferdinand von Arlt and Ernst Fuchs in Vienna. He spent the subsequent two years working with Louis Emile Javal at the Sorbonne ophthalmologic laboratory where they constructed an early keratometer known as the “Javal Schiøtz ophthalmometer.”
Schiøtz (Ref. 24) returned to Norway and in 1881 introduced the concept of asepsis to Norway at the Rikshospitalet in Oslo which included disinfection of instruments by boiling in water and the use of white coats when performing surgery. In 1882, Schiøtz presented an ophthalmoscope (Fig. 7) of his own design which featured two moveable mirrors allowing the instrument to be used for either direct or indirect ophthalmology without requiring removal and replacement of either mirror as was previously the case. Also in 1882, he invented an instrument to measure colored halos in narrow angle glaucoma. Three years later, in 1885, he presented his new self-monitoring perimeter and in 1888 he demonstrated a prism apparatus to investigate and measure muscle balance between the two eyes and in 1916, a “blink lantern” to diagnose color vision abnormalities in seamen and train personnel. His medical thesis in 1883 was “On Some Optical Corneal Characteristics” and he was later one of the earliest performers of refractive corneal surgery.
Figure 7.
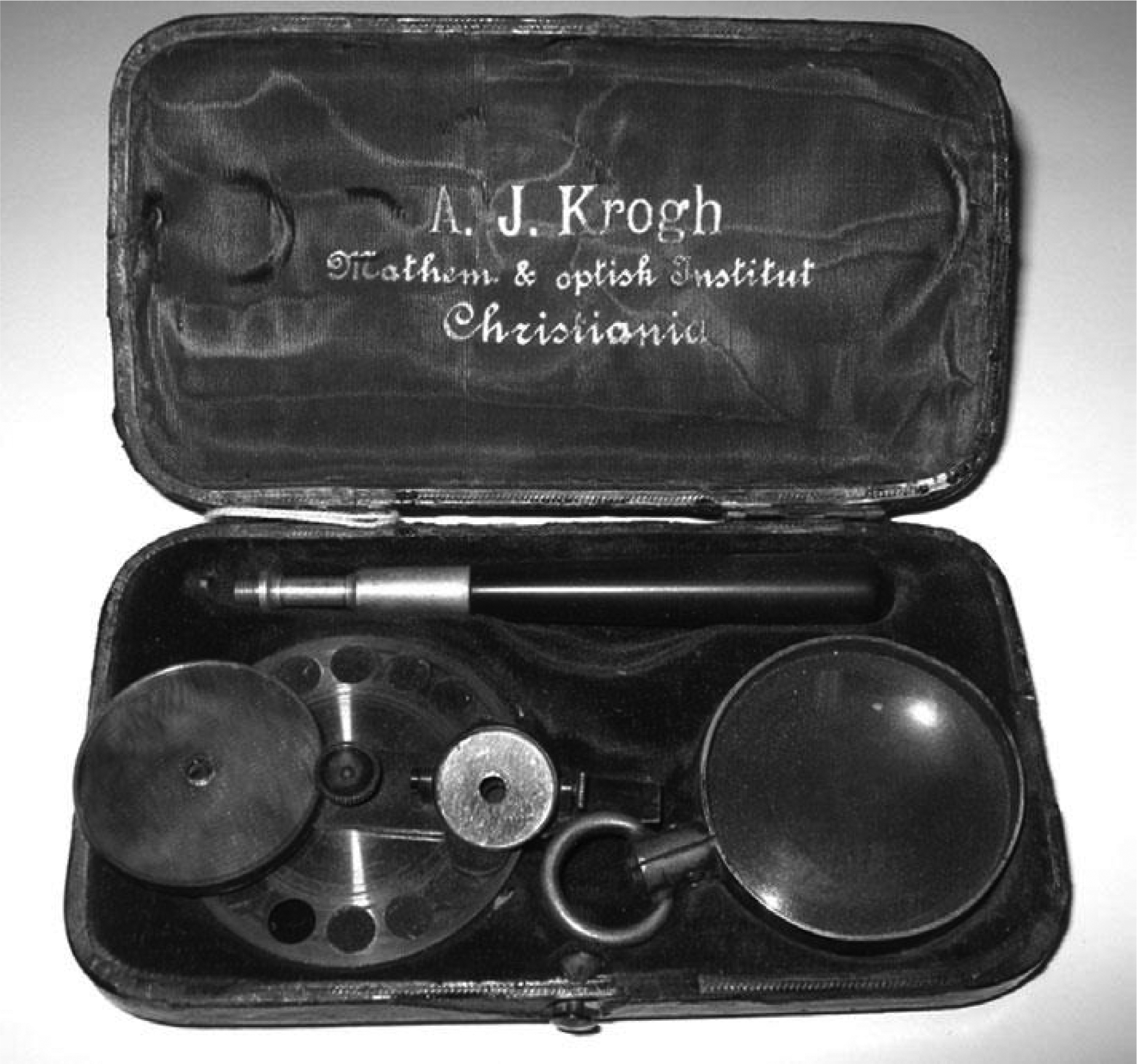
The Schiøtz ophthalmoscope manufactured by Andreas Jensen Krogh. Courtesy of Richard Keeler, FRCOphth (Hon), Honorary Curator, The Royal College of Ophthalmologists.
Schiøtz was a gifted craftsman who built prototype models of his inventions in his home workshop. In 1915, he became the first Norwegian professor of ophthalmology and was a founder and first president of the Norwegian Ophthalmological Association.
Schiøtz was an austere, sensitive individual, haunted by depression who despised showmanship and publicity. Although he was an admired public figure in Norway and was warmly regarded by students and patients, he had little interaction with his international colleagues. His many inventions were well received during his lifetime, but since his death in 1928, only his tonometer has endured and although now beyond its zenith, remains widely used throughout the world. Starting in 1910, clinical studies with titles such as “Glaucoma Therapy Under the Guidance of the Schiøtz Tonometer” began to appear with increasing frequency (Ref. 15). Much of our present basic knowledge of IOP in the normal eye and in the glaucoma eye was gained using the Schiøtz tonometer (Ref. 22).
Until his death in 1928, Schiøtz continued to refine both the tonometer calibration process and the mechanism of the tonometer itself (Ref. 24) (Fig. 8). The Schiøtz tonometer was manufactured by Andreas Jensen Krogh (1849–1938), owner of a firm that produced mathematical and surgical instruments in Norway (Ref. 24) (Fig. 5). The moderate price of the tonometer no doubt contributed to its popularity.
Figure 8.
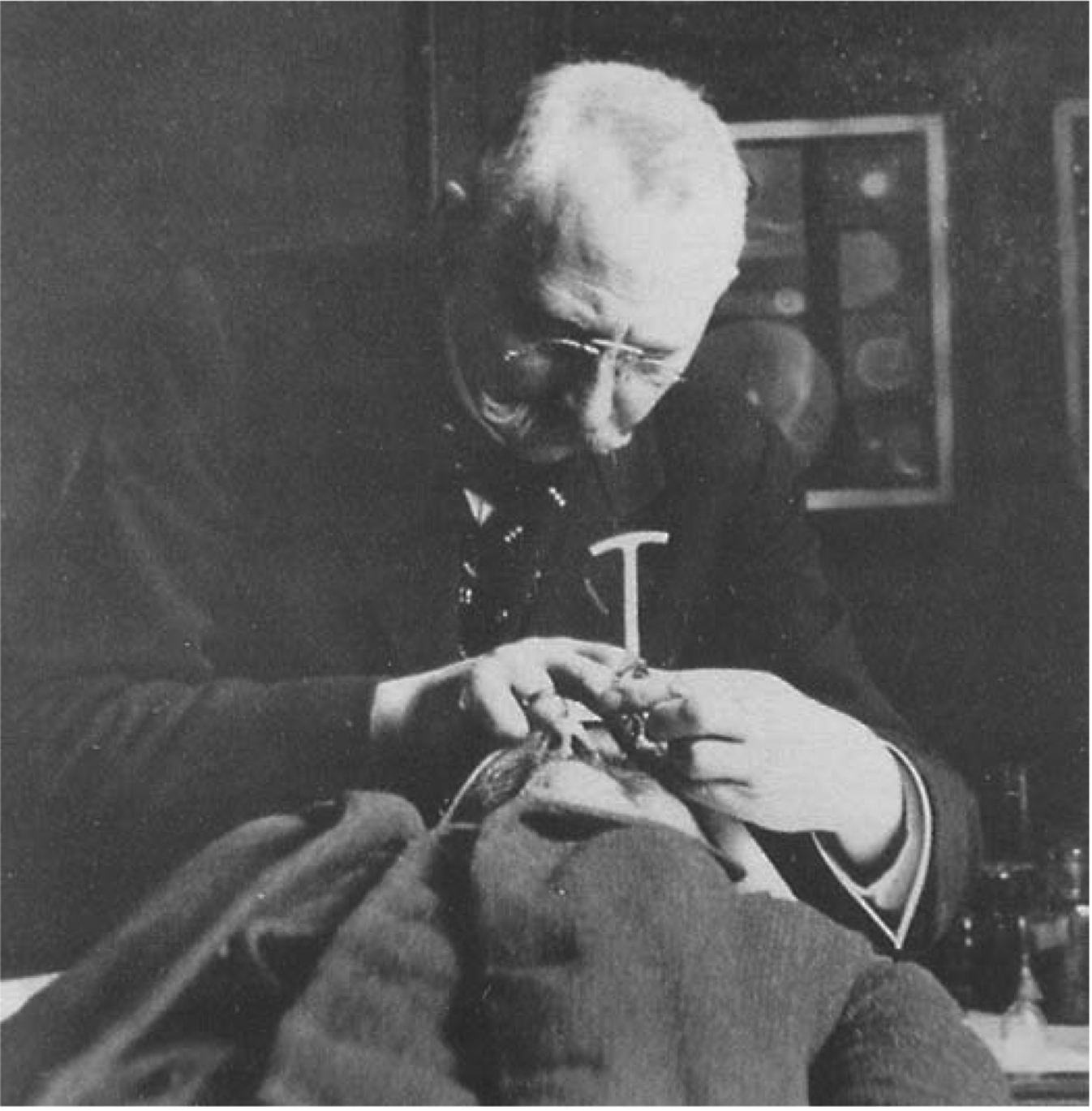
Schiøtz in old age using his tonometer. Courtesy Otto Johansen, Hjalmar Schiøtz (1850–1927), 1999/2000.
Starting about 1937, Jonas S. Friedenwald (Fig. 6), Johns Hopkins’ great ophthalmologist and visual scientist with wide-ranging interests, at the request of the American Academy of Ophthalmology and Otolaryngology, began making contributions to the theory and practice of tonometry (Ref. 25). In particular he improved the accuracy of the calibration scale for the Schiøtz tonometer (Ref. 26). Working with Robert A. Moses and others, he offered improved conversion tables in 1954 and again, posthumously in 1957- (Ref. 23), that prolonged the time during which the Schiøtz tonometer was the unrivalled standard for diagnosing and treating glaucoma patients. Friedenwald also designed electronic versions of the Schiøtz tonometer. But, although the problems inherent in impression tonometry were minimized and compensated for by these efforts, the basic flaws of impression tonometers could not be eliminated: the displacement of aqueous elevating the IOP; the variability of the cornea’s thickness, rigidity, curvature, and elastic properties, as well as the increased pressure, introduced by squeezing the lids (Ref. 8).
In 1955, Hans Goldmann, a Swiss ophthalmologist from the University of Bern, published his concept for an applanation tonometer and developed the Goldmann tonometer that replaced the Schiøtz as the gold standard against which all other are judged to the present day (Ref. 27). Its limitations are that it’s not portable, requires anesthesia and sterilization, needs to be calibrated and the apparent pressure can vary according to the corneal thickness. Despite being eclipsed by the Goldmann and other more recent tonometers, the Schiøtz tonometer nonetheless remains in wide use today and is manufactured in China, Pakistan, and India.
d). Financial Support:
An Unrestricted Grant from Research to Prevent Blindness, New York, New York and P30EY010572, Ophthalmology Core Facility
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Meeting Presentation: N/A
Conflict of Interest: “No conflicting relationship exists for the authors”
4. References
- 1.Jayne WA. The healing gods of ancient civilizations. New Haven, Yale University Press, 1925. [Google Scholar]
- 2.The International Center for Reiki Training, Reiki News Articles. Hippocrates and the laying on of hands. https://www.reiki.org/reikinews/hippocratesB.htm.
- 3.Leffler CT, Schwartz SG, Tamer MH, Salman A, Vasuki V. The early history of glaucoma: the glaucous eye (800 B.C. to 1050 A.D.). Clin Ophthalmol 9: 207–215, 2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Banister R. Banister’s Breviary, A treatise of one hundred and thirteene diseases of the eyes and eye liddes The second time published with some profitable additions of certain… London: Felix Kingstone for Thomas Man, 1622. [Google Scholar]
- 5.Kronfeld PC. Glaucoma, Chapter 11 in The History of Ophthalmology by Albert Daniel M. and Edwards Diane D.; Cambridge, MA; Blackwell Science; 203–223, 1996. [Google Scholar]
- 6.Platter F (1536–1614). Praxeos medicae opus, Basilea: Emmanuelis König, 1656. [Google Scholar]
- 7.Bowman W. The collected papers of Sir William Bowman, Bart F.R.S. Vol. 2: London, Harrison and sons, 1892. [Google Scholar]
- 8.Kniestadt C, Punjabi O, Lin S, Stamper RL. Tonometry through the ages. Survey of Ophthalmology, 53(6)568–590, 2008. [DOI] [PubMed] [Google Scholar]
- 9.Monnik AJW. Tonometres en tonometrie Academisch Proefschrift, Hoogeschool te Utrecht, 1868. [Google Scholar]
- 10.Donders FC. Vorzeigung neuer ophthalmometrischer instrumente. Zehnders Mbl Augenheilkd, 1863. [Google Scholar]
- 11.Dor H. Über Ophthalmotonometrie. Archiv für Ophthalmologie 14:13–46, 1868. [Google Scholar]
- 12.Snellen H. Über tonometer. Klin Monatsbl Augenheilkd 6:363–5, 1868. [Google Scholar]
- 13.Smith P. A new tonometer. Ophth Rev 6:33–42, 1887. [Google Scholar]
- 14.Layerat F. D’un nouveau tonometre oculaire. Recuieil Ophthal 20:614–24, 1885. [Google Scholar]
- 15.Altman AJ, Albert DM, Fournier G. Cocaine’s use in ophthalmology: our 100-year heritage. Surv Ophthalmol 29(4) 300–306, 1985. [DOI] [PubMed] [Google Scholar]
- 16.Weber A. Einige Worte Über Tonometrie: Neues tonometer. Graefes Arch Ophthalmol 13:201–209, 1867. [Google Scholar]
- 17.Maklakoff C. L’ophtalmotonométrie. Arch d’ophthalmologie (Paris) 5:159–165, 1885. [Google Scholar]
- 18.Imbert A. Théorie des ophthalmotonomѐtres. Arch Ophthalmol 5:358–363, 1885. [Google Scholar]
- 19.Fick A. Über Messung des Druckes im Auge Archiv für die gesamte Physiologie des Menschen und der Tiere. 42: Issue 1, 86–90, 1888. [Google Scholar]
- 20.Goldmann H. Un nouveau tonometre d’applanation. Bull Soc Ophtalmol Fr 67:474–8, 1955. [PubMed] [Google Scholar]
- 21.Kishimoto M, Hirose I, Kakimoto S et al. Experience in the clinical use of the Maklakov tonometers. Rinsho Ganka Jap J Clin Ophthal 18:525–33, 1964. [PubMed] [Google Scholar]
- 22.Schiøtz H. Ein neues tonometer. Arch f Augenh 52:401, 1905. [Google Scholar]
- 23.Friedenwald JS. Tonometer calibration; an attempt to remove discrepancies found in the 1954 calibration scale for Schiøtz tonometers. Trans Am Cad of Ophth Otolaryngol 61:108–22, 1957. [PubMed] [Google Scholar]
- 24.Keeler CR, Helland M, Albert DM. Hjalmar Schiøtz, the great Norwegian innovator and his ophthalmoscope. Acta Ophthalmologica 92:588–592, 2014. [DOI] [PubMed] [Google Scholar]
- 25.Friedenwald JS. Some problems in the calibration of tonometers. Am J Ophthalm 31:935–944, 1948. [DOI] [PubMed] [Google Scholar]
- 26.Friedenwald JS. Contribution to the theory and practice of tonometry. Am J Ophthalmol 20:985–1024, 1937. [Google Scholar]
- 27.Goldmann H. “Applanation Tonometry”. In: Newell Frank W (Ed) Transactions Second Glaucoma Conference. New York, Josiah Macy, Jr Foundation, 1957. [Google Scholar]


