Abstract
Objective
To compare computer-aided design and computer-aided manufacturing (CAD/CAM) customized nitinol retainers with standard stainless-steel fixed retainers over a 12-month study period.
Methods
This randomized controlled trial (RCT) was conducted on 62 patients randomly allocated to a control group that received stainless-steel retainers or a test group that received customized CAD/CAM nickel-titanium retainers. Four time points were defined retainer placement (T0) and 1-month (T1), 6-month (T2), and 12-month (T3) follow-up appointments. At each time point, Little’s irregularity index (LII) (primary endpoint) and dental stability measurements such as intercanine width were recorded in addition to assessment of periodontal parameters. Radiological measurements such as the incisor mandibular plane angle (IMPA) were recorded at T0 and T3. Failure events (wire integrity or debonding) were assessed at each time point.
Results
From T0 to T3, LII and other dental measurements showed no significant differences between the two groups. The data for periodontal parameters remained stable over the study period, except for the gingival index, which was slightly, but significantly, higher in the test group at T3 (p = 0.039). The IMPA angle showed no intergroup difference. The two groups showed no significant difference in debonding events.
Conclusions
This RCT conducted over a 12-month period demonstrated no significant difference between customized CAD/CAM nickel-titanium lingual retainers and standard stainless-steel lingual retainers in terms of dental anterior stability and retainer survival. Both retainers eventually appeared to be equally effective in maintaining periodontal health.
Keywords: Randomized clinical trial, Digital models, CAD/CAM, Retainer
INTRODUCTION
The stability of orthodontic treatment outcomes is the primary concern of orthodontists, as mentioned by Oppenheim in 1934. Indeed, Sadowsky and Sakols1 stated that 72% of patients show relapse approximately 20 years after orthodontic treatment. This was confirmed in 2013 by Yu et al.,2 who described stability values ranging between 30% and 50% that reduced to 10% 20 years after debonding. Therefore, the placement of an orthodontic retainer has been highly recommended.
Retainers have been described in the literature as removable or fixed systems that can be associated with a non-mechanical process such as surgery (e.g., fibrotomy). Over time, fixed retainers have progressively gained favor over removable retainers3 due to their durability, lack of compliance requirements,4 esthetic appearance, and growing patient demand.5 Currently, the gold standard remains the multi-stranded wire introduced by Björn Zachrisson. However, fixed retainers are associated with several limitations, notably a high percentage of related failures (debonding, fractures) mainly in the maxilla (23% to 58%) compared to the mandible (5% to 37%).6 Moreover, dental plaque control around fixed retainers appears to be difficult for patients, leading to periodontal problems.7,8 Finally, Renkema et al.7 reported “wire syndrome” episodes in 2.7% of the cases 5 years after post-orthodontic treatment.
Computer-aided design and computer-aided manufacturing (CAD/CAM) technology was recently introduced in the orthodontic field, especially for custom-made orthodontic appliances (clear aligners, customized labial or lingual systems) and has been extended to orthodontic fixed retainers. Knaup et al.8 conducted a clinical in vitro and in vivo study comparing conventional spiral twistflex wires and computer-fabricated lingual nitinol retainers in a retrospective controlled clinical trial assessing in vitro biofilm formation and biofilm formation after intraoral incubation. In these studies, nitinol retainers designed and manufactured by CAD/CAM technology demonstrated better results in terms of oral health indices and biofilm formation. Additionally, an in vitro study by Aycan and Goymen9 concluded that CAD/CAM-fabricated wires were a relevant alternative to stainless-steel wires since the CAD/CAM group showed no deformation due to the nickel-titanium content.
Considering the fact that fixed retainers are considered the gold standard in the post-orthodontic retention phase7 and that they have been in use for more than 40 years,10 randomized controlled trials (RCTs) assessing CAD/CAM lingual fixed retainers should be relevant. To the best of our knowledge, no clinical study has yet compared an innovative CAD/CAM fixed retainer with a standard stainless-steel fixed retainer with respect to lower anterior alignment stability, wire and bonding integrity, and patient opinions.
Therefore, the objective of this prospective RCT was to compare an innovative customized CAD/CAM nitinol lingual retainer to the standard multi-stranded stainless-steel lingual retainer over a 12-month period. The primary objective was to compare the alignment stability of six mandibular anterior teeth between the two groups by using Little’s irregularity index (LII). The secondary objectives were to evaluate mandibular dental arch parameters by dental cast and cephalometric measurements, failure events such as debondings or fractures related to retainers, periodontal health and patient-reported outcome measures (PROMs). The null hypothesis was that customized CAD/CAM nitinol lingual retainers and standard stainless-steel retainers provide equal results for the dental anterior stability parameters.
MATERIALS AND METHODS
Experimental design
Ethical approval
Ethical approval for this randomized control trial was obtained from the Ethics Committee of the University Hospital of Liège, Belgium (No. 2019/25). All patients were verbally informed of the purposes, risks, benefits, and monitoring of the study, and they all signed an informed consent form.
Trial design
This study was designed as a single-center RCT to compare two different fixed retainers placed on the mandible from canine to canine over a 12-month follow-up period (Figure 1) after retainer placement:
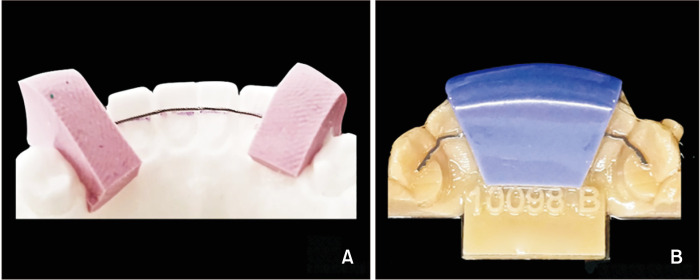
Figure 1.
Photograph of the retainers. A, Control group: Round 0.0175-inch (in) 6-strand twisted stainless-steel wire retainer. B, Test group: Rectangular 0.014 × 0.014-in memory shape customized computer-aided design and computer-aided manufacturing nitinol retainer.
Control group: Round 0.0175-inch (in) 6-strand twisted stainless-steel wire retainer (Supra-FlexTM; RMO Europe, Illkirch-Graffenstaden, France)
Test group: Rectangular 0.014 × 0.014-in memory shape customized CAD/CAM nitinol retainer (MemotainTM; CA Digital GmbH, Mettmann, Germany)
There were no changes to the protocol after trial commencement.
Participants, eligibility criteria, and settings
Sixty-two patients from the Department of Orthodontics and Dentofacial Orthopedics, University Hospital of Liège, were included in the RCT. They were randomly assigned to the control or test groups. The patient selection criteria were as follows: (1) patients undergoing fixed orthodontic appliance at the mandible; (2) end of treatment defined as Class I, i.e., complete correction of upper and lower maxillary and mandibular crowding, optimal overjet and overbite (from 1 to 2 mm), coincident upper and lower midlines, occlusion according to the six keys of Andrews11; (3) adequate oral hygiene; and (4) no missing teeth. The exclusion criteria were as follows: (1) craniofacial or severe asymmetry syndromes; (2) history of periodontal disease; (3) dental restorations or missing teeth on the anterior mandibular area; (4) previous anterior fixed retainer placement; and (5) nickel allergy.
Operators and investigator training
Two orthodontists were involved in the conception of the study, retainer placement, data acquisition, analysis, or interpretation. Additionally, two academic statistical experts performed the statistical analyses and contributed to the data analysis and interpretation. Two calibration meetings took place, in which the goals of the trial and the materials and methods to be used were reviewed and established in common.
Interventions
Dental impressions were taken using an intraoral scanner (TriosTM; 3Shape, Copenhagen, Denmark) for both groups. For the control group, based on a resin model printed from the digital impressions, an independent Belgian laboratory technician hand-bent the stainless-steel wire and supplied the silicone gutter to perform indirect wire bonding. For the test group, dental impressions (stereolithography [.stl] files) were sent to the company (CA Digital GmbH), which designed and manufactured the fixed lingual retainers using a CAD/CAM approach. All patients in both groups underwent the same bonding protocol (3M Primer Transbond XT and Transbond LR; 3M, Maplewood, MN, USA) in accordance with the manufacturer’s instructions, and fixed retainers were bonded by an indirect bonding technique from mandibular canine to canine. For cases involving retainer debonding, loss, or breakage, the patient was instructed to come back immediately to the orthodontic clinic.
Data collection
The following time points were defined over the study period of 12 months:
(1) T0: bonding of the lingual fixed retainer
(2) T1: 1 month after T0
(3) T2: 6 months after T0
(4) T3: 12 months after T0 (end of the study)
Dental stability parameters
Dental stability parameter measurements were performed using Ortho Analyzer 3-D software (3Shape) at T0, T1, T2, and T3. The LII12 value was assessed by adding the five distances obtained from the displacement of anatomic contact points on the lower anterior teeth from canine to canine. The following mandibular arch measurements were also recorded: intercanine width, interpremolar width, anterior arch length, and total arch length.
Periodontal data
The following periodontal parameters were scored at T0, T1, T2, and T3: gingival index (GI) as described by Loe and Silness,13 plaque index (PI) using the Silness-Loe index,14 recession level (RL) based on the Sullivan and Atkins index,15 and calculus index (CI) as defined by Greene and Vermillion.16
Radiographic data
Radiographic data were captured at T0 and T3. The degree of mandibular anterior tooth tipping based on American Board of Orthodontics (ABO) measurements was scored from 0 to 2 on panoramic radiographs. In addition, cephalometric measurements described by Steiner were measured as follows: inter-incisor angle and incisor mandibular plane angle (IMPA).
Retainer failures
Retainer and bonding integrity were recorded at T1, T2, and T3. Retainer integrity was categorized as follows: total integrity, partially damaged, fractured at one place, or fractured at several places. For assessment of bond integrity, the total number of debonded retainers in each group was recorded, and the average events/patient was calculated. Additionally, the type of debonding was recorded as adhesive-enamel interface debonding or wire-composite interface debonding.
Patient-reported outcome measures
Patient satisfaction was evaluated using a questionnaire with a 0–10 visual analogue scale (VAS) at T3 as follows: overall satisfaction and level of discomfort for the tongue.
Sample size calculation, randomization, and statistical analysis
The primary endpoint was the LII value for the mandible assessed at each of the four time points (0, 1 month, 6 months, and 12 months). Thus, assuming a power of 80% (1-β = 0.80), a significance level (α) of 0.0125 to account for multiple comparisons, the standard deviation (SD) of LII distribution as 0.15 mm in the two groups, and the use of two-sided t-tests at each time point, the power calculation showed that with at least 24 patients in each group (total n = 48 patients), a mean difference (Δ) of at least 0.15 mm in LII could be evidenced between the two groups over the entire study period. The sample size was increased to 31 patients in each group (total n = 62 patients) to compensate for potential dropouts during the study and to enable descriptive assessment of secondary endpoints. Patients were randomized sequentially by blocks of 10 (5 in each group) until completion of the required sample size.
Results are presented as mean and SD or median and interquartile range (IQR) for continuous variables and as frequencies (number, %) for categorical variables. The two-sided unpaired Student’s t-test was used to compare the means of the control or test groups. For proportions, the chi-squared test was applied. Additionally, generalized linear mixed effects models (GLMMs) were fitted to the data in order to assess the effect of time and group on the variables recorded longitudinally. The results were considered significant at the 5% uncertainty level (p < 0.05). All statistical analyses were performed using SAS software version 9.4 (SAS Institute, Cary, NC, USA) and the graphics were obtained using the software R version 3.6.1.
RESULTS
Participant flow
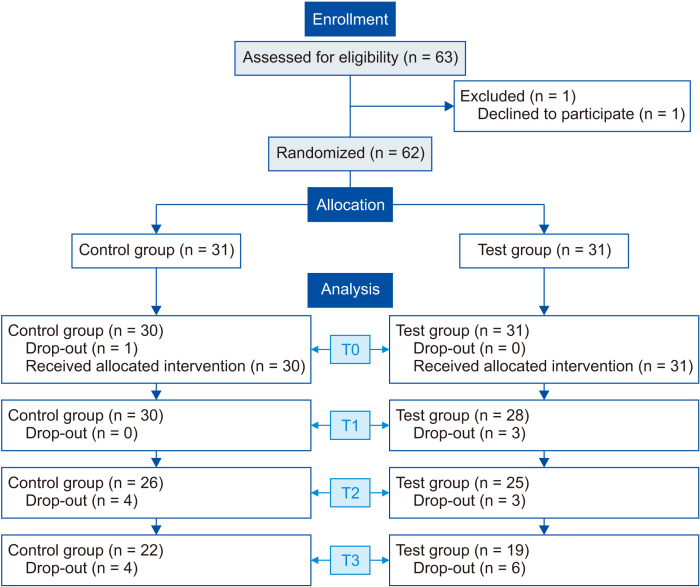
Figure 2 illustrates the patient flow through the trial. Sixty-three patients were eligible, but one patient declined to participate. Thus, 62 patients consented to participate and were randomized (31 each in the control and test groups). One randomized patient in the control group did not start the trial and was eliminated. During the study, 3, 7, and 10 patients discontinued their participation at T1, T2, and T3 respectively, and were treated as dropouts.
Figure 2.
Consolidated Standards of Reporting Trials flow diagram.
T0, Baseline; T1, 1 month; T2, 6 months; T3, 12 months.
Baseline characteristics
Patient demographics are presented in Table 1. Globally, the mean age of the patients was 17 ± 4.4 years, and there were 18 males and 43 females. The LII value before the orthodontic treatment was 4.09 ± 2.32 mm. At bonding of lingual fixed retainer (T0), the two groups were homogeneous for all the parameters, except for a small difference in the CI (control group: 0.47 ± 0.51; test group: 0.77 ± 0.43; p = 0.017).
Table 1.
Baseline characteristics of study patients in the control and test groups (n = 61)
| Variable | Control group (n = 30) |
Test group (n = 31) |
p-value |
|---|---|---|---|
| Sex | 0.30 | ||
| Female | 23 (76.7) | 20 (64.5) | |
| Male | 7 (23.3) | 11 (35.5) | |
| Age (yr) | 16.0 ± 3.18 | 18.0 ± 5.14 | 0.074 |
| Little’s irregularity index (LII) before orthodontic treatment (mm) | 4.20 ± 2.15 | 3.98 ± 2.51 | 0.72 |
Values are presented as mean ± standard deviation for continuous variables and as frequencies (number, %) for categorical variables.
Chi-square test for the comparison of the sex proportion between groups.
Two-sided unpaired Student’s t-test for the comparison of the age and LII means between groups.
Dental cast outcomes
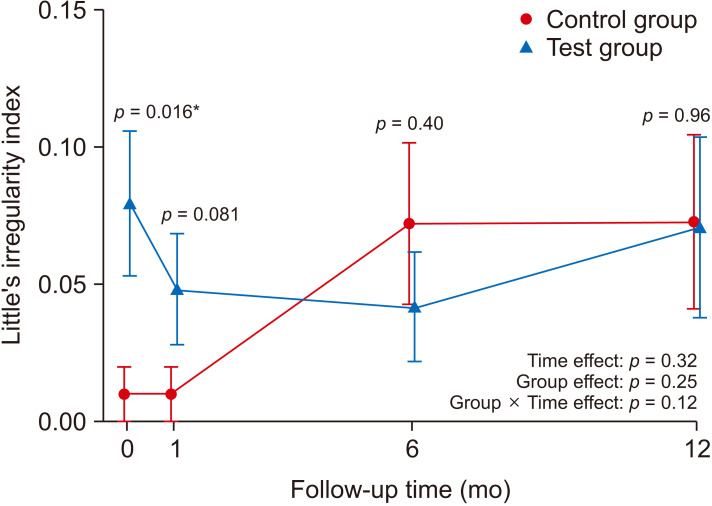
Over the study period (Figure 3), the primary endpoint (LII) did not significantly differ between the two groups. Although the mean LII at T0 was slightly higher in the test group (0.08 ± 0.14 mm) than in the control group (0.01 ± 0.06 mm), the difference (p = 0.016) did not reach the statistical significance level of 1.25% set in the power calculation. These findings were confirmed by applying a GLMM analysis to the data with no group effect (p = 0.25), no time effect (p = 0.32), and no interaction effect (p = 0.12). For the other dental cast parameters, including intercanine width, no significant differences within and between groups were demonstrated (Table 2).
Figure 3.
Evolution of Little’s irregularity index in the control and test groups. Group mean values and standard error bars displayed at each time point with p-values obtained by two-sided unpaired t-test. p-values of time effect, group effect and interaction effect on “Little Irregularity Index” measures over time obtained by Generalized Linear Mixed effects Models (GLMM).
*p < 0.05.
Table 2.
Dental stability parameter measurements in the control and test groups
| Variable | Control group | Test group | p-value |
|---|---|---|---|
| Intercanine width (mm) | |||
| T0 | 27.0 ± 1.43 | 26.6 ± 1.58 | 0.37 |
| T1 | 27.1 ± 1.48 | 27.0 ± 1.16 | 0.83 |
| T2 | 26.9 ± 1.49 | 27.0 ± 1.28 | 0.84 |
| T3 | 26.6 ± 1.38 | 26.9 ± 1.25 | 0.51 |
| Interpremolar width (mm) | |||
| T0 | 34.5 ± 2.78 | 34.7 ± 2.25 | 0.76 |
| T1 | 34.5 ± 2.82 | 35.0 ± 2.04 | 0.46 |
| T2 | 34.6 ± 2.74 | 35.4 ± 2.69 | 0.31 |
| T3 | 34.9 ± 2.13 | 34.6 ± 1.56 | 0.70 |
| Anterior arch length (mm) | |||
| T0 | 3.88 ± 0.47 | 3.67 ± 0.50 | 0.10 |
| T1 | 4.03 ± 0.48 | 3.84 ± 0.55 | 0.18 |
| T2 | 3.82 ± 0.53 | 3.69 ± 0.55 | 0.40 |
| T3 | 3.70 ± 0.45 | 3.75 ± 0.53 | 0.76 |
| Total arch length (mm) | |||
| T0 | 22.9 ± 2.18 | 22.8 ± 1.82 | 0.93 |
| T1 | 23.0 ± 2.16 | 23.0 ± 2.03 | 0.94 |
| T2 | 23.1 ± 2.00 | 23.1 ± 1.78 | 0.99 |
| T3 | 23.4 ± 1.77 | 23.7 ± 1.25 | 0.59 |
Values are presented as mean ± standard deviation.
Two-sided unpaired Student’s t-test for the comparison between groups at each time point.
T0, Baseline; T1, 1 month; T2, 6 months; T3, 12 months.
Radiographic variables
On the panoramic radiographs, the degree of mandibular anterior tooth tipping did not show any intergroup difference at each time point. From T0 and T3, the IMPA and inter-incisor angles remained stable between the two groups (Table 3).
Table 3.
Evolution of cephalometric measurements in the control and test groups during the study period
| Variable | Control group |
Test group |
p-value |
|---|---|---|---|
| Inter-incisor angle (°) | |||
| T0 | 123.0 ± 9.54 | 123.0 ± 8.32 | 0.91 |
| T3 | 121.0 ± 9.00 | 121.0 ± 8.77 | 0.95 |
| IMPA (°) | |||
| T0 | 102.0 ± 9.82 | 98.4 ± 5.74 | 0.13 |
| T3 | 99.7 ± 8.51 | 97.3 ± 7.26 | 0.37 |
Values are presented as mean ± standard deviation.
Two-sided unpaired Student’s t-test for the comparison between groups at each time point.
T0, Baseline; T3, 12 months; IMPA, incisor mandibular plane angle.
Periodontal parameters
The overall periodontal parameters also remained unchanged from baseline until the end of the study in each group, except for the GI which was slightly, but significantly, higher in the test group than in the control group at T3 (control group: 0.23 ± 0.43; test group: 0.63 ± 0.76; p = 0.039) (Table 4).
Table 4.
Periodontal parameters in the control and test groups at each time point
| Variable | Control group | Test group | p-value |
|---|---|---|---|
| Gingival index | |||
| T0 | 0.97 ± 0.72 | 1.07 ± 0.91 | 0.64 |
| T1 | 0.80 ± 0.71 | 0.69 ± 0.79 | 0.59 |
| T2 | 1.04 ± 0.79 | 0.88 ± 0.90 | 0.50 |
| T3 | 0.23 ± 0.43 | 0.63 ± 0.76 | 0.039* |
| Plaque index | |||
| T0 | 1.17 ± 0.65 | 1.07 ± 0.74 | 0.58 |
| T1 | 0.77 ± 0.57 | 0.73 ± 0.67 | 0.83 |
| T2 | 1.16 ± 0.62 | 0.92 ± 0.65 | 0.19 |
| T3 | 0.95 ± 0.49 | 1.05 ± 0.62 | 0.57 |
| Recession index | |||
| T0 | 0.00 ± 0.00 | 0.00 ± 0.00 | 0.99 |
| T1 | 0.00 ± 0.00 | 0.00 ± 0.00 | 0.99 |
| T2 | 0.00 ± 0.00 | 0.00 ± 0.00 | 0.99 |
| T3 | 0.00 ± 0.00 | 0.00 ± 0.00 | 0.99 |
| Calculus index | |||
| T0 | 0.47 ± 0.51 | 0.77 ± 0.43 | 0.017* |
| T1 | 0.30 ± 0.47 | 0.27 ± 0.45 | 0.80 |
| T2 | 0.44 ± 0.58 | 0.42 ± 0 .50 | 0.88 |
| T3 | 0.23 ± 0.43 | 0.42 ± 0.51 | 0.19 |
Values are presented as mean ± standard deviation.
Two-sided unpaired Student’s t-test for the comparison between groups at each time point.
T0, Baseline; T1, 1 month; T2, 6 months; T3, 12 months.
*p < 0.05.
Retainer failures
Retainer integrity was categorized as total integrity in both groups at each time point. In assessments of retainer debonding over the study period, nine events were recorded in the control group and 10 events in the test group. The average number of debondings per patient showed no significant difference from T1 to T3 between the two groups. However, a significant increase in the quantity of debondings was noted over time in the two groups (time effect p = 0.022). Finally, the type of debonding (adhesive-enamel interface or wire-composite interface) did not show any difference between the two groups (Tables 5 and 6).
Table 5.
Number of retainer debonding events categorized by debonding at the adhesive-enamel interface or the wire-composite interface
| Variable | Control group | Test group | p-value |
|---|---|---|---|
| Type of debonding | |||
| T1 | 2 | 0 | NA |
| Adhesive-enamel interface | 2 | 0 | |
| Wire-composite interface | 0 | 0 | |
| T2 | 4 | 8 | 0.091 |
| Adhesive-enamel interface | 2 | 2 | |
| Wire-composite interface | 2 | 6 | |
| T3 | 3 | 2 | 0.40 |
| Adhesive-enamel interface | 1 | 2 | |
| Wire-composite interface | 2 | 0 |
Values are presented frequencies (number) and proportions were compared between groups with the Fisher exact test.
T1, 1 month; T2, 6 months; T3, 12 months.
Table 6.
Total number of debondings per patient from T1 to T3 in the control and test groups
| Variable | Control group | Test group |
p-value |
|---|---|---|---|
| Total debonding | |||
| T1 | 0.07 ± 0.25 | 0.00 ± 0.00 | 0.19 |
| T2 | 0.16 ± 0.37 | 0.33 ± 0.70 | 0.28 |
| T3 | 0.14 ± 0.35 | 0.11 ± 0.32 | 0.77 |
Values are presented as mean ± standard deviation.
Two-sided unpaired Student’s t-test for the comparison between groups at each time point.
Patient-reported outcome measures
At the end of study, the level of satisfaction in terms of the final result was the same in the two groups (9.9 vs. 9.6, p = 0.23), similar to the level of discomfort for the tongue (0.3 vs. 0.6, p = 0.26).
DISCUSSION
The aim of this RCT was to compare, for the first time, an innovative nitinol CAD/CAM retainer (test group) with a standard multi-stranded stainless-steel wire retainer (control group) on the basis of several parameters, including anterior mandibular dental stability and retainer survival, over a 12-month study period. Since the null hypothesis of the study was not rejected, we concluded that no statistically significant difference could be demonstrated between the two retainers.
Anterior dental stability
After retainer bonding, the LII value remained stable over the study period in each group and between groups. Additionally, no difference was found for the anterior transversal and sagittal arch dimensions between the two groups, and the IMPA angle, whose average values correspond to an effective anterior guide, did not show any differences either. Therefore, while the stability of the six mandibular anterior teeth was ensured over time in both groups, the new CAD/CAD nitinol retainer did not demonstrate a better efficacy than the standard retainer.
Several explanations can be proposed to explain these findings. First, the positive effect of fixed retainers on the alignment stability of mandibular anterior teeth is well-known,17 although the measures for prevention of some undesirable occlusal changes remain unclear.17 Second, indirect bonding (applied in patients of both groups) is considered to be an accurate method of maintaining tooth alignment.18 Furthermore, the efficacy of the stainless-steel wire retention has already been demonstrated in several studies18 and a systematic review and meta-analysis.19 In an RCT, Gunay and Oz20 compared the clinical success of 0.0175-in 6-strand stainless-steel wire with a 0.0195-in dead-soft coaxial wire (created directly on the patient’s mandibular arch without a dental cast) and considered the stainless-steel wire as being more efficient in tooth alignment retention. Moreover, a retrospective study by Renkema et al.7 demonstrated the stability of the LII in 90.5% of 200 patients over 5 years after active orthodontic treatment with stainless-steel flexible spiral wire.
Nevertheless, CAD/CAM retainers have some interesting characteristics; Schumacher10 and Kravitz et al.6 highlighted the wire shape manufacturing precision, and Möhlhenrich et al.21 showed in an in vitro study that CAD/CAM nitinol retainers had better mechanical properties in terms of permanent deformation resistance than twisted stainless-steel wires. Additionally, as investigated by Wolf et al.,3 CAD/CAM technology seems to provide a high level of correlation between the intraoral position of the retainer and the virtual setup position, which therefore induces a high level of predictability even in anatomically demanding regions. Nevertheless, to the best of our knowledge, no RCTs have already investigated tooth stability with CAD/CAM retainers. All things considered, according to our results and the literature cited above, hand-bent multi-stranded wires are comparable to CAD/CAM-designed and produced retainers in terms of anterior tooth stability, when using an indirect bonding for both wires.
Retainer failures
No occurrence of retainer fracture was observed in either of the study groups. Indeed, Zinelis et al.22 have demonstrated that multi-stranded stainless-steel wires could maintain their elemental integrity throughout a 14-year intraoral exposure period. With respect to the CAD/CAM retainer, its properties, which include resistance to deformation and corrosion as well as flexibility,6 may explain the absence of fractures. Moreover, the fact that CAD/CAM wires are directly manufactured in the desired shape by laser cutting without wire bending could also reduce the risk of deformations or micro fractures.6 However, bonding failures were reported in both groups, with a higher occurrence in the first 6 months but similar rates of occurrence in the control and test groups. In fact, the occurrence of bond failure of lingual retainers is generally higher during the first 6 months, according to some authors.23 The early failure peak can be explained by the fact that tooth mobility is higher just after the completion of orthodontic treatment than it is later in the retention period.24 Interestingly, in an in vitro study, Aycan and Goymen9 investigated the type of debonding that occurred in a multi-stranded stainless-steel wire group when compared to a CAD/CAM nitinol wire group. They demonstrated, in contrast to our findings, that the higher flexibility of the CAD/CAM nitinol wire leads to more occurrences of enamel-adhesive interface debondings than wire-adhesive interface debondings.
Periodontal health
Although fixed retainers are likely to increase gingival recession, plaque retention, and bleeding on probing,8 the results in the present study demonstrated that both retainers are equally compatible with good periodontal health. Whereas the CAD/CAM nitinol group showed a significant and slightly higher GI at T3 than the control group, the Silness and Löe scores remained, on average, inferior to 1 over the study period in both groups. In a recent systematic review, Arn et al.25 confirmed that fixed retainers represent a good retention method in terms of respecting periodontal health. Moreover, patients were recalled at 1 month, 6 months, and 1 year, and toothbrushing recommendations were reiterated at each time point, since regular checkups are recommended in order to detect post-treatment complications at an early stage.7 Furthermore, in the present study, the inclusion criteria ensured that the patients had good oral brushing habits, since fixed retainers are restricted to patients who pay attention to their oral hygiene.26 According to the literature, CAD/CAM retainer characteristics contribute to the decrease in periodontal events.8,27 Firstly, CAD/CAM nitinol wires exhibit higher flexibility, which allows physiological dental mobility and also reduces the risk of further periodontal problems.10 Moreover, the CAD/CAM nitinol manufacturing procedure permits thinner manufactured retainers and integrates an electro-polishing step for the wire, both of which contribute to reducing plaque retention.27 Finally, in the in vitro study by Knaup et al.,8 who analyzed biofilm formation on conventional lingual twistflex wires and computer-fabricated lingual nitinol retainers over 6 months, the CAD/CAM group demonstrated better results. Nevertheless, due to regular retainer checkups and patients who took care of their oral hygiene, CAD/CAM retainers did not clinically improve the overall periodontal health parameters compared to standard stainless-steel retainers in the present study.
Patient-reported outcome measures
The overall patient satisfaction rate was significantly high in both groups, and no difference in terms of tongue discomfort was noted between groups. Therefore, the CAD/CAM nitinol electro-polished surface seems to have no influence on patient comfort.
Limitations
The study was designed as a single-center RCT, but it would be worthwhile to extend it to multiple centers in the future to take into account the wider experience of other sites. Secondly, while patients were blinded for the type of retainer, this was not possible for the orthodontist operator. Regarding patient characteristics, more female than male subjects were enrolled in the study due to the fact that more female undergo orthodontic treatment that is likely to improve their dental appearance. As for LII, limitations of the measurement technique have been reported.28 The LII does not consider dental modifications such as interdental spaces or rotations when the contact point is intact; additionally, it does not differentiate several minor tooth displacements from a single high contact point displacement.29 Nevertheless, the LII is considered to be a rapid and simple technique widely used in the literature, hence allowing comparisons with other publications.29 The benefit-cost ratio between the two groups has not been evaluated. However, without any further investigations, the cost of the CAD/CAM nitinol retainer used here was three times greater than that of the standard retainer. Interestingly, in their prospective study, Hu et al.,30 who compared titanium alloy retainers designed by the 3Shape software and manufactured by CAD/CAM with hand-bent conventional lingual retainers, found that the manufacturing of the conventional method retainers was twice as time-consuming. Moreover, the 12-month follow-up period is relatively limited in order to comprehensively explore the mechanical properties of CAD/CAM retainers over a much longer timeframe (e.g., the flexibility may become an advantage as the material ages) and in order to evaluate their lifespan. Finally, the trial was not registered and this could be defined as a limitation.
CONCLUSION
Under the restrictions of the present RCT conducted over 12 months, innovative customized CAD/CAM nitinol retainers and standard multi-stranded stainless-steel retainers were comparable in terms of dental anterior stability parameters. Both retainers were also equally compatible with maintaining periodontal health and comparable in terms of failure occurrence and patient’s opinion of the treatment.
Footnotes
CONFLICTS OF INTEREST
No potential conflict of interest relevant to this article was reported.
REFERENCES
- 1.Sadowsky C, Sakols EI. Long-term assessment of orthodontic relapse. Am J Orthod. 1982;82:456–63. doi: 10.1016/0002-9416(82)90312-8. [DOI] [PubMed] [Google Scholar]
- 2.Yu Y, Sun J, Lai W, Wu T, Koshy S, Shi Z. Interventions for managing relapse of the lower front teeth after orthodontic treatment. Cochrane Database Syst Rev. 2013;(9):CD008734. doi: 10.1002/14651858.CD008734.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wolf M, Schumacher P, Jäger F, Wego J, Fritz U, Korbmacher-Steiner H, et al. Novel lingual retainer created using CAD/CAM technology: evaluation of its positioning accuracy. J Orofac Orthop. 2015;76:164–74. doi: 10.1007/s00056-014-0279-8. [DOI] [PubMed] [Google Scholar]
- 4.Kartal Y, Kaya B. Fixed orthodontic retainers: a review. Turk J Orthod. 2019;32:110–4. doi: 10.5152/TurkJOrthod.2019.18080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kravitz ND, Shirck JM. Bonded lingual retainers [Internet] Orthodontic Products; 2015. Nov, [cited 2020 Jul]. Available from: http://www.kravitzorthodontics.com/assets/pdfs/bonded-lingual-retainers.pdf . [Google Scholar]
- 6.Kravitz ND, Grauer D, Schumacher P, Jo YM. Memotain: a CAD/CAM nickel-titanium lingual retainer. Am J Orthod Dentofacial Orthop. 2017;151:812–5. doi: 10.1016/j.ajodo.2016.11.021. [DOI] [PubMed] [Google Scholar]
- 7.Renkema AM, Renkema A, Bronkhorst E, Katsaros C. Long-term effectiveness of canine-to-canine bonded flexible spiral wire lingual retainers. Am J Orthod Dentofacial Orthop. 2011;139:614–21. doi: 10.1016/j.ajodo.2009.06.041. [DOI] [PubMed] [Google Scholar]
- 8.Knaup I, Wagner Y, Wego J, Fritz U, Jäger A, Wolf M. Potential impact of lingual retainers on oral health: comparison between conventional twistflex retainers and CAD/CAM fabricated nitinol retainers: a clinical in vitro and in vivo investigation. J Orofac Orthop. 2019;80:88–96. doi: 10.1007/s00056-019-00169-7. [DOI] [PubMed] [Google Scholar]
- 9.Aycan M, Goymen M. Comparison of the different retention appliances produced using CAD/CAM and conventional methods and different surface roughening methods. Lasers Med Sci. 2019;34:287–96. doi: 10.1007/s10103-018-2585-7. [DOI] [PubMed] [Google Scholar]
- 10.Schumacher P. [cited 2020 Jul 26];CAD/CAM-fabricated lingual retainers made of nitinol. Dental Tribune [Internet] 2015 Jun 11; Available from: https://www.dental-tribune.com/clinical/cadcam-fabricated-lingual-retainers-made-of-nitinol/
- 11.Andrews LF. The six keys to normal occlusion. Am J Orthod. 1972;62:296–309. doi: 10.1016/S0002-9416(72)90268-0. [DOI] [PubMed] [Google Scholar]
- 12.Little RM. The irregularity index: a quantitative score of mandibular anterior alignment. Am J Orthod. 1975;68:554–63. doi: 10.1016/0002-9416(75)90086-X. [DOI] [PubMed] [Google Scholar]
- 13.Loe H, Silness J. Periodontal disease in pregnancy. I. Prevalence and severity. Acta Odontol Scand. 1963;21:533–51. doi: 10.3109/00016356309011240. [DOI] [PubMed] [Google Scholar]
- 14.Silness J, Loe H. Periodontal disease in pregnancy. II. Correlation between oral hygiene and periodontal condtion. Acta Odontol Scand. 1964;22:121–35. doi: 10.3109/00016356408993968. [DOI] [PubMed] [Google Scholar]
- 15.Sullivan HC, Atkins JH. Freeutogenous gingival grafts. 1. Principles of successful grafting. Periodontics. 1968;6:5–13. [PubMed] [Google Scholar]
- 16.Greene JC, Vermillion JR. The oral hygiene index: a method for classifying oral hygiene status. J Am Dent Assoc. 1960;61:172–9. doi: 10.14219/jada.archive.1960.0177. [DOI] [Google Scholar]
- 17.Steinnes J, Johnsen G, Kerosuo H. Stability of orthodontic treatment outcome in relation to retention status: an 8-year follow-up. Am J Orthod Dentofacial Orthop. 2017;151:1027–33. doi: 10.1016/j.ajodo.2016.10.032. [DOI] [PubMed] [Google Scholar]
- 18.Egli F, Bovali E, Kiliaridis S, Cornelis MA. Indirect vs direct bonding of mandibular fixed retainers in orthodontic patients: comparison of retainer failures and posttreatment stability. follow-up A 2-year of a single-center randomized controlled trial. Am J Orthod Dentofacial Orthop. 2017;151:15–27. doi: 10.1016/j.ajodo.2016.09.009. [DOI] [PubMed] [Google Scholar]
- 19.Swidi AJ, Griffin AE, Buschang PH. Mandibular alignment changes after full-fixed orthodontic treatment: a systematic review and meta-analysis. Eur J Orthod. 2019;41:609–21. doi: 10.1093/ejo/cjz004. [DOI] [PubMed] [Google Scholar]
- 20.Gunay F, Oz AA. Clinical effectiveness of 2 orthodontic retainer wires on mandibular arch retention. Am J Orthod Dentofacial Orthop. 2018;153:232–8. doi: 10.1016/j.ajodo.2017.06.019. [DOI] [PubMed] [Google Scholar]
- 21.Möhlhenrich SC, Jäger F, Jäger A, Schumacher P, Wolf M, Fritz U, et al. Biomechanical properties of CAD/CAM-individualized nickel-titanium lingual retainers: an in vitro study. J Orofac Orthop. 2018;79:309–19. doi: 10.1007/s00056-018-0144-2. [DOI] [PubMed] [Google Scholar]
- 22.Zinelis S, Pandis N, Al Jabbari YS, Eliades G, Eliades T. Does long-term intraoral service affect the mechanical properties and elemental composition of multistranded wires of lingual fixed retainers? Eur J Orthod. 2018;40:126–31. doi: 10.1093/ejo/cjx045. [DOI] [PubMed] [Google Scholar]
- 23.Al-Nimri K, Al Habashneh R, Obeidat M. Gingival health and relapse tendency: a prospective study of two types of lower fixed retainers. Aust Orthod J. 2009;25:142–6. [PubMed] [Google Scholar]
- 24.Schneider E, Ruf S. Upper bonded retainers: survival and failure rates. Angle Orthod. 2011;81:1050–6. doi: 10.2319/022211-132.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Arn ML, Dritsas K, Pandis N, Kloukos D. The effects of fixed orthodontic retainers on periodontal health: a systematic review. Am J Orthod Dentofacial Orthop. 2020;157:156–64.e17. doi: 10.1016/j.ajodo.2019.10.010. [DOI] [PubMed] [Google Scholar]
- 26.Wouters C, Lamberts TA, Kuijpers-Jagtman AM, Renkema AM. Development of a clinical practice guideline for orthodontic retention. Orthod Craniofac Res. 2019;22:69–80. doi: 10.1111/ocr.12302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Doldo T, Di Vece L, Ferrari Cagidiaco E, Nuti N, Parrini S, Ferrari M, et al. A New Generation of Orthodontic retainer using 3d printing technology: clinical cases report. J Osseointegration. 2018;10:142–8. [Google Scholar]
- 28.Macauley D, Garvey TM, Dowling AH, Fleming GJ. Using Little's Irregularity Index in orthodontics: outdated and inaccurate? J Dent. 2012;40:1127–33. doi: 10.1016/j.jdent.2012.09.010. [DOI] [PubMed] [Google Scholar]
- 29.Forde K, Storey M, Littlewood SJ, Scott P, Luther F, Kang J. Bonded versus vacuum-formed retainers: a randomized controlled trial. Part 1: stability, retainer survival, and patient satisfaction outcomes after 12 months. Eur J Orthod. 2018;40:387–98. doi: 10.1093/ejo/cjx058. [DOI] [PubMed] [Google Scholar]
- 30.Hu X, Ling J, Wu X. The CAD/CAM method is more efficient and stable in fabricating of lingual retainer compared with the conventional method. Biomed J Sci Tech Res. 2019;18:13609–12. doi: 10.26717/BJSTR.2019.18.003157. [DOI] [Google Scholar]