New York City was an epicenter of the coronavirus disease 2019 (COVID-19) pandemic, leading to an unprecedented burden on cardiac imaging.1 Cardiac sonographers bear increased infectious risk from close patient contact when performing transthoracic echocardiograms (TTEs). The American Society of Echocardiography (ASE) issued recommendations at the beginning of the pandemic to reduce viral transmission risk and provide guidance in the absence of disease-specific data.2 , 3 Echocardiography labs across the country adapted. The unique perspective of cardiac sonographers on such changes during the COVID-19 pandemic is unknown.
In this cross-sectional study, we surveyed cardiac sonographers in major academic centers in New York City to explore disinfection and scanning practice patterns during the surge of COVID-19 cases from March to May 2020. Invitations to participate in the anonymous online survey (via REDCap, Vanderbilt University) were sent to echocardiography lab directors at 15 institutions across all five boroughs for distribution to sonographers. We collected responses from August 12, 2020, to September 16, 2020. The study was exempt from complete IRB submission by the Mount Sinai Morningside Institutional Review Board, but was approved by an expedited exempt review.
A total of 78 cardiac sonographers responded. The majority practiced in Manhattan (71%) followed by the Bronx (18%). The highly affected boroughs of Queens and Brooklyn had only five (6%) and four (5%) respondents. Over half of those surveyed had ≥10 years of experience. The mean age was 41.6 ± 9 years, and 71% were women. The average number of TTEs performed daily per sonographer prior to March 2020 was seven to nine studies (59% of respondents) or ≥10 (29%), with a substantial drop to less than seven (95%) during the surge.
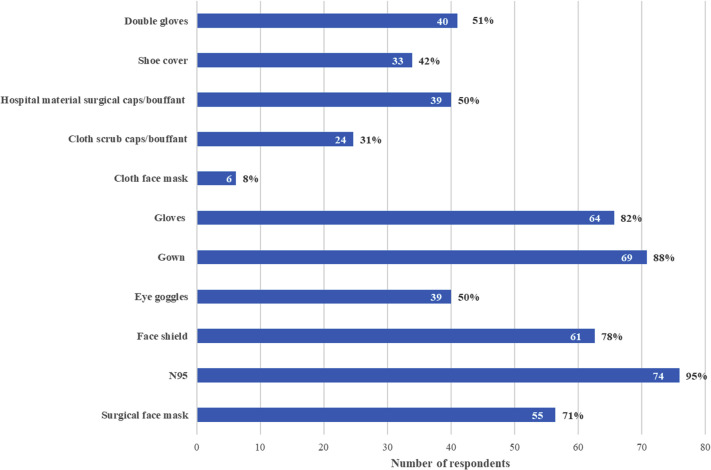
Over 80% of survey participants were aware of the patient's COVID-19 status prior to scanning. Following ASE suggestions for personal protective equipment (PPE), the majority of sonographers (95%) used N95 respirators, whereas Centers for Disease Control and Prevention (CDC) guidance during the surge stated surgical face masks were adequate for non-aerosol-generating procedures such as TTE (Figure 1 ).4 In fact, the overlapping responses of N95 and surgical face masks suggest double masking to conserve N95. As supply chains strengthened, CDC guidelines changed to prefer N95 respirators for all suspected-positive patient interactions. Few sonographers used homemade cloth masks (8%), suggesting an adequate supply of hospital-issued masks. Only half reported using dedicated eye goggles, as ASE guidelines did not specify this aspect of PPE and CDC guidelines delayed until June to include eye protection as standard precaution.
Figure 1.
Use of PPE by cardiac sonographers, with N95 respirators, gowns, and gloves being the most commonly used components of PPE. Overlapping answers for N95 and surgical face mask are likely due to double masking.
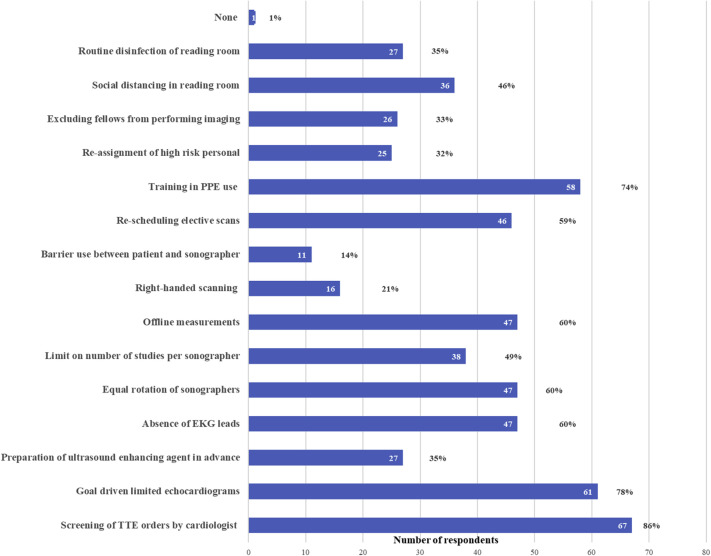
Sonographers reported infrequent use of plastic echocardiogram machine covers (9%), barriers between the patient and sonographer (11%), or probe covers (30%) (Figure 2). Further, approximately a quarter of respondents reported a lack of training in disinfection practices of ultrasound equipment. Offline measurements or omission of electrocardiogram leads was variable across institutions surveyed. However, the ASE suggested all such practices to protect sonographers and concurrently ease disinfection burden. Innovation such as tablet-based echocardiography can mitigate such issues.5 These gaps, as elucidated by sonographers, are significant and merit attention toward practice modifications to reduce infectious risk and increase uniformity across labs.
Figure 2.
Variations in the institutional policies for scanning during the COVID-19 pandemic implemented across programs, with the screening of echocardiogram requests by a cardiologist being the most common policy change.
The most common changes to institutional policies during the COVID-19 pandemic surge were (1) screening of TTE orders by a cardiologist (86%), (2) goal-driven echocardiograms via abbreviated protocols (78%), and (3) training in PPE use (74%). Most respondents agreed that these policy changes contributed to improving safety (strongly agree [23%], agree [58%]) and decreasing viral exposure time (strongly agree [35%], agree [44%]) during the pandemic surge.
Screening of orders by cardiologists allowed preemptive reduction in the inherent risks posed by COVID-19-positive patients to each sonographer with each scan. Previously, TTE requests for hospitalized patients with cardiac concerns were deemed appropriate, and thus rarely required filtering by a cardiologist.6 Screening of all orders, as such, was a new practice during the surge. Further, an emphasis on abbreviated scanning protocols is essential to limit sonographer exposure.7 Accordingly, in response to these temporary measures, over half of sonographers agreed that the TTE performed mostly yielded clinically significant information (always [19%], usually [41%]). Only 2% reported the information obtained was insignificant (rarely, never). The COVID-19 pandemic sheds light on elements of success as viewed by our sonographers and opportunities for future integration into practice.
The limitations of our study include a retrospective analysis of lab changes during the surge with limited data on continued postsurge modifications by institutions. We did not collect data on sonographer infection of COVID-19 due to an inability to discern transmission location (at-work versus outside the hospital).
In conclusion, our study is the first comprehensive assessment of cardiac sonographers’ perceptions during the pandemic. We identify specific areas—cardiologist review of TTE orders, abbreviated protocols, N95 respirators—in which sonographers agree that our labs in New York City have excelled. We also highlight safety protocols such as dedicated eye protection and disinfection practices as potentials for improvement in our practice of echocardiography as COVID-19 continues and future contagions emerge.
Acknowledgments
We thank the echocardiography laboratory directors who helped distribute the survey and especially all of the cardiac sonographers who not only took the time to complete the survey but also work each day as the pillars of our imaging labs.
Footnotes
Conflicts of Interest: None.
References
- 1.Argulian E., Weinsaft J.W., Hendel R.C., Garg V.P., Kim J., Phillips L.M. Life interrupted: on the front lines with COVID-19. JACC Cardiovasc Imaging. 2020;13:1834–1837. doi: 10.1016/j.jcmg.2020.05.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kirkpatrick J.N., Mitchell C., Taub C., Kort S., Hung J., Swaminathan M. ASE statement on protection of patients and echocardiography service providers during the 2019 novel coronavirus outbreak. J Am Soc Echocardiogr. 2020;33:648–653. doi: 10.1016/j.echo.2020.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mitchell C., Collins K., Hua L., McClanahan C., Shea E., Umland M. Specific considerations for sonographers when performing echocardiography during the 2019 novel coronavirus outbreak: supplement to the American Society of Echocardiography Statement. J Am Soc Echocardiogr. 2020;33:654–657. doi: 10.1016/j.echo.2020.04.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Centers for Disease Control and Prevention Interim infection prevention and control recommendations for patients with suspected or confirmed coronavirus disease 2019 (COVID-19) in healthcare settings. November 4, 2020. https://www.cdc.gov/coronavirus/2019-ncov/hcp/infection-control-recommendations.html?CDC_AA_refVal=https%3A%2F%2Fwww.cdc.gov%2Fcoronavirus%2F2019-ncov%2Finfection-control%2Fcontrol-recommendations.html
- 5.McMahon S.R., De Francis G., Schwartz S., Duvall W.L., Arora B., Silverman D.I. Tablet-based limited echocardiography to reduce sonographer scan and decontamination time during the covid-19 pandemic. J Am Soc Echocardiogr. 2020;33:895–899. doi: 10.1016/j.echo.2020.05.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Douglas P.S., Garcia M.J., Haines D.E., Lai W.W., Manning W.J., Patel A.R. ACCF/ASE/AHA/ASNC/HFSA/HRS/SCAI/SCCM/SCCT/SCMR 2011 Appropriate use criteria for echocardiography. J Am Coll Cardiol. 2011;57:1126–1166. [Google Scholar]
- 7.Kaminski A., Payne A., Roemer S., Ignatowski D., Khandheria B.K. Answering to the call of critically ill patients: limiting sonographer exposure to covid-19 with focused protocols. J Am Soc Echocardiogr. 2020;33:902–903. doi: 10.1016/j.echo.2020.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]