Abstract
The upsurge in the number of people affected by the COVID-19 is likely to lead to increased rates of emotional trauma and mental illnesses. This article systematically reviewed the available data on the benefits of interventions to reduce adverse mental health sequelae of infectious disease outbreaks, and to offer guidance for mental health service responses to infectious disease pandemic. PubMed, Web of Science, Embase, PsycINFO, WHO Global Research Database on infectious disease, and the preprint server medRxiv were searched. Of 4278 reports identified, 32 were included in this review. Most articles of psychological interventions were implemented to address the impact of COVID-19 pandemic, followed by Ebola, SARS, and MERS for multiple vulnerable populations. Increasing mental health literacy of the public is vital to prevent the mental health crisis under the COVID-19 pandemic. Group-based cognitive behavioral therapy, psychological first aid, community-based psychosocial arts program, and other culturally adapted interventions were reported as being effective against the mental health impacts of COVID-19, Ebola, and SARS. Culturally-adapted, cost-effective, and accessible strategies integrated into the public health emergency response and established medical systems at the local and national levels are likely to be an effective option to enhance mental health response capacity for the current and for future infectious disease outbreaks. Tele-mental healthcare services were key central components of stepped care for both infectious disease outbreak management and routine support; however, the usefulness and limitations of remote health delivery should also be recognized.
Key words: COVID-19, infectious disease, mental health service, psychological intervention, tele-mental healthcare
Introduction
The coronavirus disease 2019 (COVID-19) pandemic is the largest threat to the world in this century (WHO, 2020). To limit transmission, business and school closures are implemented, mass quarantines (Brooks et al., 2020) are imposed and self-isolation and social distancing (Kaplan et al., 2020) are highly recommended, and such measures have been implemented in almost all countries to differing extents (Galea, Merchant, & Lurie, 2020; Ho, Chee, & Ho, 2020; Jung & Jun, 2020; Li et al., 2020a, 2020b). Millions of people in the world have been infected, with ever increasing numbers under quarantine or in isolation. Fear of illness, severe shortages of resources, social isolation, large and growing financial losses, and increased uncertainty will contribute to widespread psychological distress and increased risk for mental illness and behavioral disorders as a consequence of COVID-19 (Pfefferbaum & North, 2020).
The worldwide impact of the COVID-19 pandemic on mental health has already been identified as including insomnia, anxiety, and depression among healthcare workers and other vulnerable populations (Que et al., 2020; Tang et al., 2020; Brooks et al., 2020; Cao et al., 2020; Gao et al., 2020; Gonzalez-Sanguino et al., 2020; Holmes et al., 2020; King, Delfabbro, Billieux, & Potenza, 2020; Li et al., 2020a, 2020b; Shi et al., 2020; Wang et al., 2020a, 2020b, 2020c; Xiao, Zhang, Kong, Li, & Yang, 2020). Chinese healthcare workers exposed to the COVID-19 pandemic reported symptoms of depression (50.4%), anxiety (44.6%), insomnia (34.0%), and psychological distress (71.5%) (Lai et al., 2020). These symptoms also manifest in the general population, whose prevalence of depression, anxiety, insomnia, and acute stress was 27.9, 31.6, 29.2, and 24.4%, respectively (Shi et al., 2020). Similar types of symptoms have accompanied other infectious disease epidemics such as severe acute respiratory syndrome (SARS), middle east respiratory syndrome (MERS), and Ebola virus disease (EVD) (Ho et al., 2020; Jalloh et al., 2018; Pfefferbaum & North, 2020; Vyas, Delaney, Webb-Murphy, & Johnston, 2016; Wu et al., 2009). People discharged from hospital after recovering from COVID-19 have reported high rates of post-traumatic stress disorder (PTSD) (Bo et al., 2020). A systematic review showed that after severe coronavirus infection, the point prevalence of PTSD was 32.2% (95% CI 23.7–42.0), depression was 14.9% (12.1–18.2), and anxiety was 14.8% (11.1–19.4) (Rogers et al., 2020). Some mental health problems persisted for years with a quarter of SARS patients having PTSD, and 15.6% having depression 2 years after experiencing SARS (Mak, Chu, Pan, Yiu, & Chan, 2009).
Early detection and recognition of COVID-19-related psychiatric symptoms is pivotal for tailoring cost-effective accessible interventions. Mental health responses could enhance coping and lead to recovery from this massive worldwide psychological trauma of COVID-19 and the pandemic. Given the developing situation with coronavirus pandemic worldwide, policy makers urgently need an evidence synthesis to produce guidance for the development of psychological interventions and mental health response. The aim of this paper is to synthesize the data on mental health services and interventions for the infectious disease epidemics, and to enhance knowledge and improve the quality and effectiveness of the mental health response to COVID-19 and future infectious disease epidemics.
Methods
Search strategy and selection criteria
We sought to include any articles focusing on mental health interventions or services applied specifically for infectious disease outbreaks. We searched PubMed, Web of Science, Embase, PsycINFO on 5 May 2020, using a combination of text words and MeSH terms: (SARS OR severe acute respiratory syndrome OR Middle East Respiratory Syndrome Coronavirus OR middle east respiratory syndrome* OR MERS-CoV OR Mers OR Middle Eastern Respiratory Syndrome* OR MERSCoV* OR coronavirus OR coronavirus infections OR coronavirus* OR COVID-19 OR 2019-nCoV OR SARS-CoV-2 OR Ebola) AND (mental disorders OR mental health OR mental health programs OR mental health services OR public health services OR emergency services psychiatric OR emotional trauma OR psychosocial interventions OR psychiatric interventions OR psychological treatment OR psychotherapy). We also searched WHO Global Research Database on COVID-19 using the term ‘mental health’, and the preprint server medRxiv with search terms ‘SARS or MERS or Ebola or coronavirus or COVID-19’ and ‘mental health’ on 15 April 2020. Articles about mental health services (e.g. mental health system, mental health measures or strategies) and specific types of psychological interventions for infectious diseases such as SARS, MERS, EVD, and COVID-19 were included in the present review. We excluded articles on the epidemiology of psychological impacts, mental health responses to other types of diseases, and non-English publications.
All articles were independently screened for eligibility by two reviewers (SYK and YW) on title and abstract. All full-text articles identified were reviewed by YJL and BYP. For each retrieved full-text article, we hand searched the article's references and examined possible additional studies. Original intervention trials were independently critically appraised using the Cochrane Collaboration's quality assessment tool by two reviewers (SSZ and YK) (Higgins et al., 2011; Higgins & Green, 2009). Consensus was used to resolve any disagreements. Review authors’ judgments evaluated selection bias, performance bias, detection bias, attrition bias, reporting bias, and other bias. In all cases, an answer ‘L’ indicates a low risk of bias and an answer ‘H’ indicates high risk of bias. If insufficient detail was reported of what happened in the study, the judgment will usually be ‘Unclear’ risk of bias.
Results
Search retrieval and characteristics
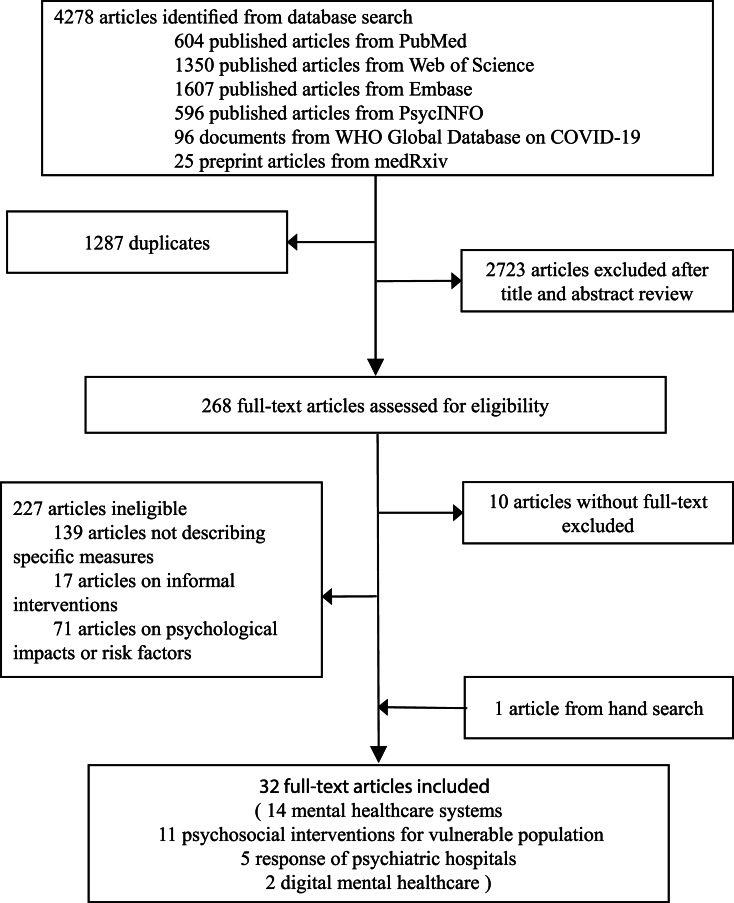
The PubMed, Web of Science, Embase, and PsycINFO search identified 604, 1350, 1607, and 596 articles, respectively. The WHO Global Research Database on COVID-19 identified 96 articles and medRxiv identified 25 articles. There were 2723 articles left after removing those articles which were duplicates from the six searches. Hand searching of full-text articles yielded one additional reference to include in this review. In total, 32 eligible articles were included in this review (see Fig. 1), most focusing on COVID-19, followed by EVD, SARS, and MERS. Of the 32 articles, one used a randomized controlled trial (RCT), seven used quasi-experimental methods or pre-post intervention or quantitative interview, 24 reported processes of the delivery of care but did not rigorously evaluate outcomes (8 reports, 14 commentaries, and 2 reviews) (see Table 1). Twenty-three articles described mental health practices and services for COVID-19 [China (9), South Korea (2), Singapore (2), Italy (2), and one each for Canada, Germany, USA, UK, Malaysia, Iran, Australia, and Spain], seven articles for EVD [Sierra Leone (5), Liberia (1), and USA (1)], one article for SARS (Hong Kong, China), and one article for MERS (South Korea).
Fig. 1.
Selection of included studies.
Table 1.
Characteristics and main results of articles included in the systematic review
| Author, year | Country | Infectious disease | Study design | Target population (sample size) | Mental healthcare/outcome |
|---|---|---|---|---|---|
| Mental health systems | |||||
| Agyapong et al. (2020) | Canada | COVID-19 | Commentary | The general public (-) | Alberta Health Services launched a supportive text message (Text4Mood) program. Residents of Alberta can subscribe to the program by texting ‘COVID19HOPE’ to a sort code number and receive free daily supportive text messages for 3 months, crafted by a team of clinical psychologists, psychiatrists, mental health therapist, and mental health service users. Within 1 week of the launch of Text4Hope, 32805 subscribers had signed up to the program, and there were expressions of interests from other jurisdictions to implement a similar program to those in quarantine, isolation, or lockdown. |
| Bauerle et al. (2020) | Germany | COVID-19 | Commentary | Psychiatric patients (-) | ‘Coping with Corona: Extended Psychosomatic care in Essen’ (CoPE includes four structured modules: psychoeducation, mindfulness, and cognitive behavioral skills training), comprises telephone and videoconferencing calls with experts, as well as web contents and online interventions. An integrated part of the community emergency action plan includes a stepped procedure of assessment, indication, counseling and intervention. |
| Ho et al. (2020) | Singapore | COVID-19 | Commentary | Psychiatric patients, the general public (-) | Online psychotherapy to psychiatric patients through Zoom. Community psychiatric partners and psychologists also provided online emotional counseling for COVID-related issues. |
| Jung et al. (2020) | South Korea | COVID-19 | Commentary | Individuals in quarantine, the general public (-) | Psychological counseling for quarantined people was offered and guidelines were released for people with symptoms of COVID-19. Hotlines for the current mental health crisis were provided. Leaflets warning about possible mental health problems and guidelines to cope were distributed. |
| Li et al. (2020a, 2020b) | China | COVID-19 | Review | Psychiatric patients, the general public, vulnerable individuals such as frontline healthcare workers, confirmed COVID-19 patients, suspected COVID-19 cases, and their families (-) | The NHC issued guidelines and workplans on ‘emergency psychological crisis intervention’, ‘online mental health services’, ‘management of patients with severe mental disorders’, ‘strengthening psychological support and social work services’, ‘psychological counseling and therapies’. Psychological assistance expert groups were dispatched to Hubei province including psychologists and psychiatrists to provide individual counseling on e-Platforms. Psychiatric hospitals reduced outpatient visits, tightened admission criteria, and shortened the length of hospitalization. For newly admitted psychiatric patients, isolation wards were set up and visiting was suspended. Psychiatric hospitals provided telemedicine to patients with serious mental illness living in the community. |
| Park et al. (2020) | South Korea | COVID-19 | Commentary | Individuals in quarantine, the general public (-) | The mental health professionals provided psychological counseling to individuals in quarantine. National hospitals and community mental health centers also provided mental health care services. Leaflets promoting mental health care for the distress caused by infectious disease outbreaks were distributed. |
| Percudani et al. (2020) | Italy | COVID-19 | Report | (-) | Regional Health Authorities authorized the continuation of mental health services for the general population. Safety guidelines for both medical staff and patients were implemented, including remote psychosocial interventions and telemedicine. Hospital admissions for acute psychiatric disorders in patients positive for COVID-19 need a dedicated area in the psychiatric ward or alternatively, a medical ward supported by psychiatric staff. |
| Qiu et al. (2020) | China | COVID-19 | Report | The general public, isolated patients, frontline medical workers (-) | A comprehensive system including population-level monitoring of mental states, online emergency psychological intervention based on artificial intelligence, community-based scientific dissemination and social bond enhancement, virtual reality and neuromodulation-based intervention, and human resources training for emergency psychological interventions set up. |
| Wang et al. (2020a, 2020b, 2020c) | China | COVID-19 | Report | (-) | Policies, proposals, and guides for psychological assistance, and practical progress of psychological assistance. |
| Wang et al. (2020a, 2020b, 2020c) | China | COVID-19 | Commentary | Old adults (-) | The Chinese Society of Geriatric Psychiatry, in collaboration with the Chinese Society of Psychiatry, the Chinese Psychiatrist Association, and the Chinese Association for Mental Health, responded to the crisis promptly with an interdisciplinary solution. Mental health professionals, social workers, nursing home administrators, and volunteers delivered MHPSS for older adults collaboratively, especially for community-dwelling residents and nursing-home residents. Within a team, geriatric mental health professionals took the lead and supported the team members coming from other disciplines. |
| Yao et al. (2020) | China | COVID-19 | Commentary | (-) | A mental health triage strategy to provide four levels of psychological crisis interventions developed by NHC, a nation-wide system of online mental health services, including mental health education, psychological support, and medical consultation and treatment established, and various kinds of mental health interventions including cognitive therapies, expressive therapies, Tai Chi, and dance-based exercises implemented. |
| Zhou (2020) | China | COVID-19 | Commentary | (-) | Psychological intervention and self-help manual of COVID-19 published, 24 h psychological assistance hotlines, online psychological consultation opened and online survey about mental health conducted in Sichuan province. |
| Schreiber et al. (2019) | USA | EVD | Report | Healthcare workers, their families (-) | The ‘Anticipate, Plan and Deter Responder Risk and Resilience Model’ was used to assess and manage healthcare workers’ psychological risk and resilience. |
| Yoon et al. (2016) | South Korea | MERS | Quasi-experimental intervention | Individuals in quarantine (6231), their families (1221) | The community-based mental health system of detection, brief intervention, and refer to treatment was established for the quarantined MERS patients and their families. Service utilization rate, 71.3% receive one consultation, 28.7% required continuing services, 35.4% received continuing services. |
| Psychosocial interventions | |||||
| Albott et al. (2020) | USA | COVID-19 | Commentary | Healthcare workers (-) | A rapidly deployable Psychological Resilience Intervention founded on a peer support model (Battle Buddies) protects the well-being of medical workforce during the pandemic. Developing key cognitive, emotional, and interpersonal skills for adaptive responses. The Buddy provided peer support, and a mental health consultant assigned to their unit who gets to know their activities and concerns and was available to facilitate the peer support process at the unit level. |
| Blake et al. (2020) | UK | COVID-19 | Intervention development | Healthcare students, registered nurses, healthcare workers from nursing, and the allied health professions (55) | This e-package includes evidence-based guidance, support, and signposting relating to psychological wellbeing for all UK healthcare employees. A three-step rapid development process included public involvement activities (STEP 1), content and technical development with iterative peer review (STEP 2), and delivery and evaluation (STEP 3). The package was accessed 17633 times and had >50 000 exposures via social media within 7 days of release. 82% of healthcare participants reported having used the information in their work or home lives, and 100% anticipated they would use it in the future. |
| Cole et al. (2020) | Sierra Leone | EVD | Pre-post intervention | ETC staff (253) | Small group CBT developed to treat anxiety, depression, and functional impairment, eight sessions over 6 weeks. At post-intervention, anxiety, depression, and functional impairment significantly reduced, helping 60.8% of the participants to their personal goals or recovery. Overall, the intervention was given a mean rating of 4.44 out of 5 by the participants. |
| Ping et al. (2020) | Malaysia | COVID-19 | Report | Nurses on the COVID-19 frontline (25) | Ultra-brief psychological interventions for 1 month including group problem-solving techniques, mindfulness skills and so on. The informal qualitative feedback has suggested that it has helped respond effectively to individuals with anger or frustration, anxiety secondary to the uncertainty of the daily fluctuations of COVID-19, panic and tension in committee meetings, and the general psychological wellness of hospital staff. |
| Rastegar Kazerooni et al. (2020) | Iran | COVID-19 | Report | Medical junior students (371) | Near peer mentoring via the social media platform. 10 senior students under the supervision of expert faculty offered psychological supports for junior students such as stress relaxation techniques, time management, etc. 71% of junior medical students believed the platform had a significant impact on helping them adjust faster to these emergency conditions. |
| Decosimo et al. (2019) | Sierra Leone | EVD | Pre-post intervention | Children who were Ebola-survivors; living in Ebola-infected homes or community (870) | A community-based psychosocial arts program (Playing to Live). Activities included storytelling, musical freeze dance, art drawing, yoga, and dancing. Contrasted a 5-month to a 3-month treatment. Significant decrease in reported symptoms in both treatment groups pre- to post-intervention and a significant difference in total symptoms over time. |
| Waterman et al. (2019) | Sierra Leone | EVD | Quantitative interview | ex-ETC staff (253) | 6-week group CBT program for depression and anxiety modeled on evidence-based low-intensity interventions. Barriers (lack of motivation to attend, low literacy) and enablers (novelty of CBT, social network). |
| Waterman et al. (2018) | Sierra Leone | EVD | Pre-post intervention | ex-ETC staff (75) | Three-phased CBT-based intervention. Improvement of PTSD, sleep, depression, anxiety, and alcohol usage. |
| Kamara et al. (2017) | Sierra Leone | EVD | Report | The general public, inpatients (143) | General nurses were trained in PFA, case identification and referral pathways and provided basic counseling and problem-solving therapy for individuals in the need of mental healthcare. |
| Kohrt et al. (2015) | Liberia | EVD | Pre-post intervention | MHCs (16);law enforcement officers (14) | Adapting the CIT Model implemented a national community-based anti-stigma program, family support and advocacy activities, and facilitated partnerships to advance mental health policy, legislation, and funding. The anti-stigma and advocacy activities involved work with journalists, pharmacists, religious leaders, and other stakeholders. There is a need to develop formal collaborations with law enforcement for stigma reduction, service provision, and human rights protection. There was a significant increase in knowledge (78–88% of items answered correctly), a significant increase in positive attitudes, and a significant decrease in social distance. |
| Ng et al. (2006) | Hong Kong, China | SARS | Randomized controlled trial-intervention | The general public (25 vs. 26) | The ‘Strength-Focused and Meaning-Oriented Approach to Resilience and Transformation’ intervention using a cognitive redefinition was applied. After the 1-day group debriefing, participants showed significant decrease in depression level and changes in cognitive appraisal toward SARS. Such changes were sustained in a 1-month follow-up. |
| Psychiatric hospitals’ responses | |||||
| Garriga et al. (2020) | Spain | COVID-19 | Commentary | Psychiatric patients (-) | For community care centers and out-patient clinics, in-person visits were recommended for patients with a psychiatric emergency, risk of psychiatric relapse or new emergent cases of psychiatric patients, incorporating phone call follow-ups and telepsychiatry consultations. As per in-patients, early discharges of the psychiatry emergency rooms and acute wards were moved forward and the suspension of family visits was implemented. A novel mental health home hospitalization care was recommended. |
| Poremski et al. (2020) | Singapore | COVID-19 | Commentary | (-) | Prevention and control strategies implemented in Singapore's IMH at three levels of hospital, ward, and individual, for example, restricted access into IMH, restrictions on the number of visitors, isolation ward for potential infectious cases, electronic tracking of staff movement to facilitate contact tracing, and so on. |
| Shao et al. (2020) | China | COVID-19 | Commentary | Medical staff, psychiatric patients (-) | For outpatients, body temperature monitored and traveling history identified; for inpatients, face-to-face visitation suspended and temporary isolation ward employed; for medical staff, 14 days observation before start working, and body temperature and health status reported daily, online mental health services and relaxing courses. |
| Starace et al. (2020) | Italy | COVID-19 | Report | Psychiatric patients (-) | The Society of Epidemiological Psychiatry issued operational instructions for mental health departments for the COVID-19 pandemic. For example, psychiatric departments should postpone scheduled outpatient visits or replace them by phone check-ins, suspend group activities, take preventive measures with staff, and triage outpatients and new admissions for minimal face to face visits. |
| Xiang et al. (2020) | China | COVID-19 | Review | Psychiatric patients (-) | A 30-bed ward in an infectious disease hospital in Wuhan was established. Isolation wards were also established in psychiatric hospitals. Gyms, exhibition centers, and sports centers have been converted into ‘Fang Cang’ hospitals for infected patients with mild symptoms. |
| Digital mental healthcare | |||||
| Liu et al. (2020) | China | COVID-19 | Commentary | Medical staff, the general public (-) | Online mental health psychoeducation on WeChat, Weibo, TikTok, e-books, online psychological counseling services on WeChat by mental health professionals, online psychological self-help like CBT for depression, anxiety, and insomnia, suicide identification via AI program (Tree Holes Rescue). |
| Zhou et al. (2020) | Australia | COVID-19 | Commentary | Healthcare workers (general practitioners and specialists) (-) | Telehealth consultations. |
AI, artificial intelligence; CBT, cognitive behavioral therapy; CBT-I, cognitive behavioral therapy of insomnia; CIT, crisis intervention team; COVID-19, coronavirus disease 2019; ETC, Ebola treatment center; EVD, Ebola virus disease; IMH, Institute of Mental Health; MERS, middle east respiratory syndrome; MHCs, mental health clinicians; MHPSS, mental health and psychosocial support; NHC, National Health Center; PFA, psychological first aid; SARS, severe acute respiratory syndrome.
Four different mental health practices were reported in this systematic review, including mental healthcare systems, psychosocial interventions, specific responses of psychiatric hospitals and digital mental healthcare (see Fig. 2). Fourteen articles described mental healthcare systems, six in China (all for COVID-19), three in South Korea (2 for COVID-19 and 1 for MERS), one each for COVID-19 in Canada, Germany, Singapore, Italy, and one for EVD in the USA. Eleven articles evaluated psychosocial interventions (5 for EVD in Sierra Leone, 1 for EVD in Liberia, 1 for SARS in Hong Kong China and 1 each for COVID-19 in the USA, UK, Malaysia, and Iran). Five articles described the response of psychiatric hospitals during the COVID-19 pandemic [China (2), Spain (1), Singapore (1), and Italy (1)]. Two articles reported the digital mental healthcare for the COVID-19 outbreak [China (1) and Australia (1)]. Multiple vulnerable populations were the main target subjects including healthcare workers, psychiatric patients, quarantined individuals, family members, older adults, and children (see Table 1).
Fig. 2.
Summary of mental health interventions during infectious disease outbreaks.
Quality appraisal
Table 2 summarizes the assessment of risk of bias for five controlled trials. The majority of the intervention trials showed a low risk of bias, or we were unable to determine the risk. One trial had low risk of performance bias and detection bias, one trial had high risk of selection bias, and we were unable to determine the risk for other trials. All five trials had low risk of attrition bias, reporting bias, and other biases. As the other 27 records included in this review were not controlled trials or were commentaries, we did not conduct quality assessments for them.
Table 2.
Risk of bias summary showing review authors’ judgments about each risk of bias domain
| Domain | Cole et al. (2020) | Decosimo et al. (2019) | Waterman et al. (2018) | Kohrt et al. (2015) | Ng et al. (2006) | |
|---|---|---|---|---|---|---|
| Selection bias | Random sequence generation | U | L | U | H | L |
| Allocation concealment | U | U | U | U | L | |
| Performance bias | Blinding of participants and personnel | U | L | U | U | U |
| Detection bias | Blinding of outcome assessment | U | L | U | U | U |
| Attrition bias | Incomplete outcome data | L | L | L | L | L |
| Reporting bias | Selective reporting | L | L | L | L | L |
| Other bias | Other sources of bias | L | L | L | L | L |
L, low risk; H, high risk; U, unable to determine.
Mental health intervention systems for infectious disease outbreaks
Governments have variously developed interventions and response systems to deal with the mental health problems caused by emergency infectious disease epidemic. Countries including China, South Korea, Singapore, and Canada had experienced SARS and MERS outbreaks, which brought them evidence-based experience to better cope with the mental health crisis related to the COVID-19 pandemic. Following the MERS outbreak, the South Korean government established a community-based mental health system for detection, brief intervention, and referral of treatment for the MERS patients and their families quarantined in Gyeonggi province (Yoon, Kim, Ko, & Lee, 2016). Various mental health centers such as public health centers, community mental health centers cooperatively delivered services for MERS patients and the National Center for Crisis Mental Health Management evaluated people using these services and subsequently transferred them to local community mental health centers for continuing case management and follow-up. The service utilization rate was high, but they also found that the referral system from the national level to regional or local levels did not work well (Yoon et al., 2016). While active detection of subjects with emotional difficulties and interventions following the COVID-19 outbreak was a potential option, they needed a more efficient process for an open entry system at the local level rather than a triage system starting nationally from the top.
A series of mental health-related actions were taken at the initial stage of the COVID-19 outbreak in China (Li et al., 2020a, 2020b; Qiu, Zhou, Liu, & Yuan, 2020; Wang et al., 2020a, 2020b, 2020c; Yao, Chen, Zhao et al., 2020; Zhou, 2020), Singapore (Ho et al., 2020), South Korea (Jung & Jun, 2020; Park & Park, 2020; Yoon et al., 2016), Canada (Agyapong, 2020), Germany (Bauerle, Skoda, Dorrie, Bottcher, & Teufel, 2020), Italy (Percudani, Corradin, Moreno, Indelicato, & Vita, 2020), and the USA (Schreiber, Cates, Formanski, & King, 2019). Specifically, mental health professionals including psychiatrists, psychiatric nurses, and psychologists were deployed to provide psychological counseling and support for vulnerable populations (e.g. frontline healthcare workers, confirmed COVID-19 patients, suspected COVID-19 cases and their families) in China and for people in quarantine in South Korea. The National Health Center of China (NHC) issued several guidelines and plans (NHC-China, 2020b, 2020c, 2020d, 2020e, 2020g). Several national associations related to mental health and academic societies cooperated to establish expert groups on psychological interventions to older adults (Wang et al., 2020a, 2020b, 2020c). Psychoeducational books, articles, and videos were made available for the public through e-platforms and mobile apps (e.g. WeChat) at the early stage of the COVID-19 outbreak in China (Bao, Sun, Meng, Shi, & Lu, 2020; Li et al., 2020a, 2020b; Pfefferbaum et al., 2012).
Several hospitals, individual psychiatric departments, community psychiatric partners, and psychologists all provided online psychotherapy and counseling to psychiatric patients and the general public with COVID-related psychological distress through videoconferencing platforms (e.g. Zoom) in Singapore (Ho et al., 2020). Leaflets for the general public provided guidelines for coping with the COVID-19 distress and hotlines provided information for COVID-19 mental health crisis that might occur in South Korea (Park & Park, 2020). Canada launched a support text message (Text4Mood) program to respond to the psychological impact of COVID-19. This program provided free psychological supportive text messages daily for 3 months (Agyapong, 2020). Germany's ‘Coping with Corona: Extended Psychosomatic care in Essen’ (CoPE) offered psychological support for distressed individuals, which included four steps: initial contact, triage and diagnosis, support via tele- or video-conference, and aftercare. This program offered psycho-educational information materials about resources, relaxation techniques, and mental health (Bauerle et al., 2020).
Increasing public mental health literacy is vital to prevent and overcome the mental health crisis during the COVID-19 pandemic. Education and support from the voluntary and professional mental health sectors should be a part of mental health prevention under large infectious disease outbreaks.
Psychosocial interventions for specific populations during infectious disease outbreaks
Psychological and physical supports tended to be specifically matched to different vulnerable populations, such as children, older adults, and health care workers.
For individuals with mental health needs
A national community-based anti-stigma and advocacy activity, which is a curriculum based upon the Crisis Intervention Team (CIT) model was launched in Liberia during the EVD outbreak, could significantly decrease mental health and public health problems including violence, self-harm and suicide (Kohrt et al., 2015). A mental health unit was created at Connaught hospital in Sierra Leone during EVD outbreak (Kamara et al., 2017). General nurses were trained in psychological first aid (PFA), case identification, and referral pathways, and provided basic counseling and problem-solving therapy for individuals with mental healthcare needs. A nurse-led approach within a non-specialist setting appears to have been successful for delivering mental health and psychosocial support (MHPSS) services during the EVD outbreak. Peer support programs or services led by non-professional mental health workers are potential ways to deliver care in areas with limited human resources and weak social welfare systems.
An alternate strategy which was employed during the SARS outbreak in Hong Kong (Ng et al., 2006) was the Strength-Focused and Meaning-Oriented Approach to Resilience and Transformation (SMART). This intervention employed a body-mind-spirit framework with a strong emphasis on cognitive redefinition of the stressful situation and the individual's response. Results of the RCT (n = 51) suggested that participants’ depression levels and adaptive changes in cognitive appraisal of SARS decreased significantly after the single-day group debriefing. As this intervention trial included only a small sample, its efficacy needs to be replicated in a larger sample, and should include a follow-up study.
For children and adolescents
A community-based psychosocial arts program created by Playing to Live (PTL) was established for children who were Ebola-survivors or living in Ebola-affected homes or communities (Decosimo, Hanson, Quinn, Badu, & Smith, 2019). The PTL group hired and trained 40 Ebola-survivors to run the PTL activities two to three times a week in their communities. They also hired 40 psychosocial workers to provide weekly supportive talks to families, and information about childcare and child rights. The PTL activities included storytelling, musical freeze dance, art drawings, yoga, and dancing. Results of the pre-post-evaluation (n = 870) suggested that the 3-month program was associated with a 15% reduction in symptoms including social withdrawal, extreme anger, bedwetting, worry/anxiety, poor eating habits, violence, and continued sadness, whereas the 5-month intervention group showed a 38% reduction of such symptoms.
For older adults
For mental disorders of old age, particularly dementia, there have been limited reports of the effects of the COVID-19 pandemic. We found only one report on mental health care for older adults among our included papers. Given the high death rate among older adults infected with COVID-19 and the added strain on families with older relatives and on the institutions caring for them, the Chinese Society of Geriatric Psychiatry in collaboration with the Chinese Society of Psychiatry responded with an interdisciplinary solution. Mental health professionals, social workers, nursing home administrators, and volunteers collaboratively delivered MHPSS for older adults, especially for community-dwelling residents and nursing-home residents (Wang et al., 2020a, 2020b, 2020c). Mental health care for older adults during this epidemic was not given enough attention in the early stage of outbreak. More specific age-appropriate interventions may need to be developed for older adults for effective intervention during pandemic in the future.
For healthcare workers
Frontline health care workers are also shouldering a greater mental health burden, and thus need support in strengthening their resilience through peer support and other interventions (Que et al., 2020). First, proper protection against their own infection is critical. For example, masks, personal protective equipment, and other essential medical equipment (e.g. ventilators) will help relieve the stress of having to treat people with infections, and improve their mental wellbeing. During this COVID-19 crisis, various interventions were offered to healthcare workers, such as a peer-supported resilience intervention in the USA (Albott et al., 2020), e-package with Agile methodology in the UK (Blake, Bermingham, Johnson, & Tabner, 2020), and the ultra-brief psychological intervention in Malaysia (Ping et al., 2020). The e-package in the UK included evidence-based guidance, support, and signposting relating to psychological wellbeing, and results of this pre-post intervention (n = 55) revealed that 82% of healthcare participants used the information in their work or home lives (Blake et al., 2020). Feedback from healthcare workers suggests that qualitative wellness is improved by providing a free online resource manual targeting psychological skills and interventions to reduce the distress caused by uncertainty during the pandemic (Ping et al., 2020). Many countries have developed dedicated teams to provide mental health support for healthcare workers; however, the type of support needed depends on the stage of the pandemic, and can benefit from peer and professional counseling (Isaksson Rø, Veggeland, & Aasland, 2016).
The Anticipate, Plan, and Deter responder risk and resilience model was used to assess and manage healthcare workers’ psychological risk and resilience during the EVD outbreak (Schreiber et al., 2019). The Anticipate, Plan, and Deter model contains three components. First, pre-deployment training about the stressors that healthcare workers may face during deployment (‘Anticipate’). Second, development of a personal resilience plan (‘Plan’) and monitoring stress exposure during deployment using the web-based system. Third, invoking the personal resilience plan when risk is elevated (‘Deter’), addressing responder risk early before the onset of impairment. Psychological support was offered to junior medical students in Iran via a novel social media platform during the COVID-19 (Rastegar Kazerooni, Amini, Tabari, & Moosavi, 2020). In total, 71% of participants (n = 371) believed the platform had a significant impact on helping them adjust faster to these emergency conditions.
Following the EVD outbreak in Sierra Leone, cognitive behavioral therapy (CBT) was widely used among Ebola treatment center (ETC) staff (Cole et al., 2020; Waterman et al., 2018; Waterman, Cole, Greenberg, Rubin, & Beck, 2019). Results of the pre-post intervention (n = 253) showed that small group CBT could significantly reduce anxiety, depression, and functional impairment of ETC staff after eight sessions over 6 weeks (Cole et al., 2020). Workshops with different themes such as PFA, stress, sleep, depression, anxiety, relationships, and behavior were developed in phase 1 and 2. Participants still displaying high anxiety and depression levels after phase 1 and 2 were enrolled in phase 3 with low-intensity CBT strategies. Significant improvements in the stress, anxiety, depression, and anger domains were reported, but no improvement in sleep (Waterman et al., 2018). CBT is an evidence-based intervention delivered through various means besides face-to-face interactions. For example, delivery over the Internet or smartphone apps can be efficient for broad outreach to the populations at risk for mental health complications. The feasibility and effectiveness of training a national team to deliver a three-phase CBT-based group intervention to ex-ETC staff suggested that this model protected healthcare workers from negative psychological consequences of potentially traumatic stressors (Waterman et al., 2018; Waterman et al., 2019). However, the effectiveness of this model and its components needs more rigorous evaluation, because it relied on a single small sample during a unique epidemic (Schreiber et al., 2019). Furthermore, most of the reviewed studies were pre-post measurements with substantial heterogeneity in the included participants, methods, study designs, and outcomes. Standardized evaluations in randomized clinical trials were difficult to implement due to the urgent nature of the pandemics. Evidence-based interventions that have shown efficacy in conditions differing from epidemics also might be effective approaches to combat COVID-19, but their effectiveness needs to be tested in controlled trials during the COVID-19 pandemic.
Psychiatric hospitals’ response for infectious disease outbreaks: focus on COVID-19
Psychiatric hospitals in China prepared to cope with the COVID-19 outbreak by establishing crisis psychological intervention teams across many psychiatric hospitals, including psychiatrists, clinical psychologists, and psychiatric nurses (Li et al., 2020a, 2020b; Shao, Shao, & Fei, 2020; Xiang et al., 2020). A specialized psychiatric ward was established in an infectious disease hospital in Wuhan on 3 February 2020, and in turn isolation wards were established in psychiatric hospitals for mentally ill patients with suspected or confirmed COVID-19 (Xiang et al., 2020). NHC issued a set of guidelines in February 2020 to standardize the management of patients with severe mental disorders during the COVID-19 outbreak (NHC-China, 2020f). Subsequently, the Chinese Society of Psychiatry published guidelines to the hospital administration applicable to both psychiatric hospitals and psychiatric units in general hospitals during the outbreak (Chinese Society of Psychiatry, 2020). Psychiatric hospitals reduced outpatient visits, tightened admission criteria, and shortened the length of inpatient hospitalizations. For newly admitted psychiatric patients, isolation wards were set up and visiting was suspended to minimize the potential risk of nosocomial infection. Additionally, the majority of psychiatric hospitals used telemedicine to provide psychiatric consultations for infected patients and medical treatments for patients with preexisting mental disorders, and antipsychotic drugs were often delivered to patients’ homes following the COVID-19 outbreak in China.
The Italian Society of Epidemiological Psychiatry also issued operational instructions for the management of mental health departments and similar measures were employed in Italy (Starace & Ferrara, 2020). The Institute of Mental Health (IMH) in Singapore implemented a series of prevention and control strategies at the levels of hospital, ward, and individual (Poremski et al., 2020). Except for restrictions on patients and visitors, medical staff were managed effectively, for example, electronic tracking of staff movement to facilitate contact tracing in Singapore (Poremski et al., 2020) and China (Shao et al., 2020). For community care centers and out-patient clinics, in-person visits were recommended for patients with a psychiatric emergency, risk of psychiatric relapse or new emergent cases with mental disorders, incorporating phone call follow-ups and telepsychiatry consultations in Spain (Garriga et al., 2020). As per in-patients, early discharges of the psychiatry emergency rooms and acute wards were moved forward and the suspension of family visits was implemented. A novel mental health home hospitalization care was recommended (Garriga et al., 2020).
The infection control measures needed to limit potential exposure to SARS-CoV-2 led to inaccessibility of some mental health interventions such as injectable medications and electroconvulsive therapy, and the relative risks and benefits of these treatment losses need to be evaluated (Moreno et al., 2020). These losses should be assessed in the balance with many novel strategies involving digital telemedicine, mental health home hospitalization, commercial drug delivery, and electronic tracking. Moreover, follow-up studies are needed on how effective these interventions were in mitigating the mental health impacts of other losses to mental services and patients.
Digital mental healthcare for infectious disease outbreaks, particularly for COVID-19
Tele-mental health services were prioritized for individuals at higher risk of exposure to COVID-19 infection such as frontline clinicians, infected patients, suspected cases of infection, their families, and policemen. There are well-documented reports of China proactively providing various tele-mental health services during the COVID-19 outbreak (Liu et al., 2020; Zhou et al., 2020). The NHC and the Chinese Psychological Society provided guidelines on conducting online mental health services (Li et al., 2020a, 2020b; NHC-China, 2020a, 2020e). These services were provided by the government, academic agencies (e.g. hospitals, universities, institutes), associations of mental health professionals, and non-government organizations. The services included counseling, supervision, training, as well as psychoeducation through e-platforms (e.g. hotline, WeChat, Weibo, Tencent QQ, Alihealth, and HaoDaiFu) (MOE-China, 2020). Additionally, online self-help psychological interventions such as CBT for depression, anxiety, and insomnia were also developed (Liu et al., 2020). Early reports indicated high interest and acceptance of these services by the target population. The ‘National Crisis Intervention Platform for COVID-19’ was created with mental health professionals. Several hospitals set up their own crisis counseling system for staff and patients using telehealth in many provinces of China (Chen et al., 2020; Kang et al., 2020). The Australian government had delivered a wide range of telehealth services including telehealth consultations to general practitioners and specialists (Zhou et al., 2020). However, to date, the Australian government has focused on managing the physical health needs of the population during the epidemic, with less focus on mental health (Zhou et al., 2020). Access to other existing tele-mental health support services such as self-help platforms, videoconferencing, or mobile apps for depression, anxiety, and emotional problems should be made available for the general population (Zhou et al., 2020).
Telehealth has become a cost-effective alternative for delivering mental health care during the COVID-19 global pandemic when in person and face-to-face visits are not possible. Solid evidence supports the effectiveness of telephone and web-based interventions, especially for alleviating symptoms of depression, anxiety, and PTSD (Kerst, Zielasek, & Gaebel, 2020; Turgoose, Ashwick, & Murphy, 2018). Videoconferencing, online programs, smartphone apps, text-messaging, and e-mails have been useful communication methods for the delivery of mental health services (Torniainen-Holm et al., 2016; Zhou et al., 2020). National and provincial digital mental health services (e.g. hotlines, websites, WeChat, Weibo) have been established as essential measures to address mental health needs of key target populations such as healthcare providers during the COVID-19 outbreak. However, digital therapies might not be appropriate for older or demented people, people with reading difficulties, poor people, or people who are not technologically adept. The combination of online and offline psychological counseling is a key strategy for mental health services and intervention systems during the COVID-19 pandemic.
Discussion
This paper provides a rapid review of the published literature on mental health practices and services during recent infectious disease epidemics. Except for publications on some mental health intervention systems and psychosocial interventions, most other reports were not specifically designed to evaluate the feasibility and effectiveness of mental health interventions. More evidence-based psychosocial interventions with telehealth services and considering contextual adaptation, complexity, and resources requirements are needed during the COVID-19 pandemic and future outbreaks of infectious diseases.
During infectious disease outbreaks such as COVID-19, measures implemented for their prevention (e.g. quarantine and isolation, business or school closures) as well as the losses induced by them (e.g. finance, food, personal freedom, social connection, and relationships) contributed to significant emotional distress, reduced mental well-being, and may lead to psychiatric or behavioral disorders in both the short and long term. These consequences are of sufficient magnitude, requiring immediate efforts and direct interventions to reduce the impact of the outbreaks at both individual and population levels (Galea et al., 2020). Psychoeducation and emotional support in particular help to normalize crisis reaction, mobilize resources, and increase adaptive coping strategies for progression to serious mental illness such as major depression or PTSD (North & Pfefferbaum, 2002; North, Hong, & Pfefferbaum, 2008; Reyes, 2004). However, many countries have tended to focus on the physical health needs of COVID-19, often neglecting mental health needs with few designated organizations offering specific mental health services with easy access to those in need. The integration of mental health provisions into the COVID-19 (and other infectious disease emergencies) response should be best addressed at the national, state, and local planning levels (Pfefferbaum & North, 2020).
Call for evidence-based psychosocial interventions to cope with the COVID-19 pandemic
Prevention efforts in mental health were implemented primarily for people who were at risk or had greater vulnerability, such as frontline workers, confirmed COVID-19 patients, infected family members, and those affected by the loss of loved ones (Holmes et al., 2020). MHPSS programs through international organizations were used effectively in several low- and middle-income countries during infectious disease outbreaks (Cenat et al., 2020). For example, group-based CBT (Waterman et al., 2018; Waterman et al., 2019), PFA, PTL (Decosimo et al., 2019), culturally adapted interventions such as SMART (Ng et al., 2006), ultra-brief psychological interventions (Ping et al., 2020) and peer supports (Rastegar Kazerooni et al., 2020) have been reported to effectively mitigate the emotional impacts of COVID-19, EVD, and SARS outbreaks. However, the quality of evidence was still restricted because limited studies have provided quantitative data, and most intervention studies included small numbers of participants.
During the COVID-19 pandemic, other evidence-based interventions can be applied, and their feasibility and effectiveness should be evaluated. For example, mindfulness-based interventions (Hofmann & Gomez, 2017) or CBT for insomnia (Koffel, Bramoweth, & Ulmer, 2018; Riemann et al., 2017; Trauer, Qian, Doyle, Rajaratnam, & Cunnington, 2015) can be assessed for their effectiveness in the provision for individuals suffering from severe sleep problems or chronic anxiety symptoms. Psychosocial interventions can provide support for individuals in the wake of a crisis and can increase the perceived safety of individuals, further ameliorating maladaptive stress reactions and reducing emotional distress (Slavich, 2020). People with major losses or those with more severe illnesses are more vulnerable to experience depression, suicidal ideation, or PTSD in the initial phase of the pandemic or even after it ends (North, Suris, Davis, & Smith, 2009). Evidence-based trauma-focused psychotherapies and pharmacotherapy are appropriate. For specific subgroups, family intervention may be recommended (Dawson et al., 2015; Forbes et al., 2010; North & Pfefferbaum, 2013). Facing the pandemic, measures for identifying, triaging, referring, and treating severe psychosocial consequences, death notification, and bereavement care should be established (North & Pfefferbaum, 2013; Pfefferbaum & North, 2020; Sun, Bao, & Lu, 2020). Moreover, for the lower income countries, with greater scarcity of mental health resources, implementation or modification of evidence-based psychological treatments, such as psychological treatments to be delivered by non-specialist providers including through task sharing, is urgently needed (Barbui et al., 2020; Singla et al., 2017).
Evaluating the effectiveness of interventions to mitigate COVID-19's mental health consequences on patients
The degree of risk for infection with COVID-19 for individuals with severe mental illnesses has not been clearly established; however, it is reasonable to presume such risk to be higher than that of the general population, because of disordered mental state, possible poor self-care, inadequate insight, or side effects of psychotropic medications (Starace & Ferrara, 2020; Xiang et al., 2020). Furthermore, adverse social determinants brought about by the COVID-19 pandemic, including poverty, food insecurity, and stigma, can be contributory (Lund et al., 2018). People with severe mental health problems commonly live in poverty which impacts their ability to socially distance themselves from neighbors or the local community and increases transmission risk. Psychiatric inpatients confirmed or suspected COVID-19 could be treated in specialized wards in infectious disease hospitals or in isolated wards in psychiatric hospitals or shelter hospitals equipped with psychiatric consultations. As for psychiatric hospitals, measures including strict triaging/precautionary procedures and admission criteria, and shorter hospitalization length of stay should be taken to prevent the clustering of COVID-19 cases (Chinese Society of Psychiatry, 2020; Shao et al., 2020; Starace & Ferrara, 2020). Additionally, mental health home hospitalization care was recommended (Garriga et al., 2020), and medical staff management in psychiatric hospitals such as electronic tracking of staff movement might facilitate contact tracing (Poremski et al., 2020). However, follow-up studies on how effective these interventions were in mitigating COVID-19's mental health impacts on mentally ill patients are needed. These studies should balance the risks and benefits of these alternative interventions on mental health services among patients and providers.
Opportunity to develop evidence-based digital mental health
The potential of digital therapy programs which can offer cost-effective evidence-based therapies has not been fully realized. However, awareness of the disparities in access to the technology of poorer populations and cultural and linguistically diverse communities in low- and middle-income countries may have an impact on their implementation (Naslund et al., 2017). The effectiveness of digital mental health interventions in such countries has not been rigorously evaluated. Online mental health services’ utilization is still low in China and Australia (Yao, Chen, & Xu, 2020). However, telehealth remains a valuable way of reducing psychosocial distress without increasing the risk of infection. During infectious disease outbreaks, tele-mental health services can enable remote triaging of care, offer cognitive and/or relaxation skills to deal with stress symptoms, encourage access to online self-help programs, and deliver professional psychological interventions if necessary. Simple communication methods such as e-mail and text messaging can and should be used more extensively in low-income countries. However, many of these interventions require more rigorous assessments to determine their efficacy, effectiveness, treatment retention, and outcomes. Investing in the collection of evidence on the outcomes, workforce requirements, patient engagement, and ethical uses of tele-mental health services will allow them to truly deliver their full potential (Smith et al., 2020). Telehealth and digital services should not completely replace face-to-face treatment for patients in need, particularly those requiring intensive mental health treatment and support including wider deployment of injectable long-acting medications and hands-on interventions such as electroconvulsive and transcranial magnetic stimulation therapies, when in-person contact is once again safe.
Limitations
Several limitations of this systematic review need to be considered. First, few RCTs on the effectiveness of mental healthcare interventions on mitigating mental problems during any of these infectious disease outbreaks were identified, and more high-quality RCT studies are needed. Second, due to the limited number of studies on psychological interventions during infectious disease outbreaks, and the heterogeneity of evaluation methods, we only could provide a systematic review without a formal meta-analysis. Third, relatively few countries have reported mental health services and treatments during infectious disease outbreaks, more high-quality studies are in need to form culture-adapted efficient and nationally unique mental health responses for infectious disease outbreaks.
Conclusion
The pandemic of COVID-19 brings huge challenges for mental health systems worldwide which have to rapidly change, but also can offer an opportunity for improvement of mental health responses, and lead to long-term development of sustainable mental health care systems. Despite differences in political, social, and health systems, mental health services worldwide have implemented acute responses that focus on care for mental health service users, and have facilitated access to mental health assessment and care for new-onset or high-risk patients. More evidence-based interventions should be implemented during epidemics especially for vulnerable populations such as children, older adults, and healthcare workers. The effectiveness of alternative digital interventions in mitigating the mental health consequences on mental services and patients should be assessed in follow-up studies.
Tele-mental health strategies and global cooperation are sound approaches to develop and implement mental health systems to cope with the current COVID-19 pandemic and to improve mental health response capacity for future comparable infectious disease outbreaks. During infectious disease outbreaks, expanded access to cost-effective approaches for delivering effective mental health services should be a priority and retain effective existing services and promote new practices. Effective existing practices should be refined and scaled up, and the usefulness and limitations of remote health delivery should be recognized. Culturally-adapted and cost-effective mental health emergency systems based on evidence-based intervention methods integrated into public health emergency responses at the national and global levels are recommended to reduce the psychological impacts of infectious disease outbreaks, especially for COVID-19.
Acknowledgements
We appreciate An-Yi Zhang, Yi-Jie Wang, Xiao-Xing Liu, Xi-Mei Zhu, Ze Yuan, Chen-Wei Yuan and Meng-Ni Jing for their help with the data search.
Financial support
This work was partially supported by grants from the National Natural Science Foundation of China (no. 81761128036, 81821092 and 31900805), the Special Research Fund of PKUHSC for Prevention and Control of COVID-19 (no. BMU2020HKYZX008) and the National Key Research and Development Program of China (no. 2019YFA0706200). GT is supported by the National Institute for Health Research (NIHR) Applied Research Collaboration South London at King's College London NHS Foundation Trust, and by the NIHR Asset Global Health Unit award. The views expressed are those of the authors and not necessarily those of the NHS, the NIHR or the Department of Health and Social Care. GT also receives support from the National Institute of Mental Health of the National Institutes of Health under award number R01MH100470 (Cobalt study). GT is supported by the UK Medical Research Council in relation the Emilia (MR/S001255/1) and Indigo Partnership (MR/R023697/1) awards.
Conflict of interest
None.
References
- Agyapong, V. I. O. (2020). Coronavirus disease 2019 pandemic: Health system and community response to a text message (Text4Hope) program supporting mental health in Alberta. Disaster Medicine and Public Health Preparedness, Apr 22, 1–2. doi: 10.1017/dmp.2020.114 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Albott, C. S., Wozniak, J. R., McGlinch, B. P., Wall, M. H., Gold, B. S., & Vinogradov, S. (2020). Battle buddies: Rapid deployment of a psychological resilience intervention for healthcare workers during the COVID-19 pandemic. Anesthesia and Analgesia, 131(1), 43–54. doi: 10.1213/ane.0000000000004912 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bao, Y., Sun, Y., Meng, S., Shi, J., & Lu, L. (2020). 2019-nCoV Epidemic: Address mental health care to empower society. Lancet (London. England), 395(10224), e37–e38. doi: 10.1016/s0140-6736(20)30309-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barbui, C., Purgato, M., Abdulmalik, J., Acarturk, C., Eaton, J., Gastaldon, C., … Thornicroft, G. (2020). Efficacy of psychosocial interventions for mental health outcomes in low-income and middle-income countries: An umbrella review. The Lancet Psychiatry, 7(2), 162–172. doi: 10.1016/S2215-0366(19)30511-5 [DOI] [PubMed] [Google Scholar]
- Bauerle, A., Skoda, E. M., Dorrie, N., Bottcher, J., & Teufel, M. (2020). Psychological support in times of COVID-19: The Essen community-based CoPE concept. Journal of Public Health (Oxford. England), 42(3), 649–650. doi: 10.1093/pubmed/fdaa053 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blake, H., Bermingham, F., Johnson, G., & Tabner, A. (2020). Mitigating the psychological impact of covid-19 on healthcare workers: A digital learning package. International Journal of Environmental Research and Public Health, 17(9), 2997. doi: 10.3390/ijerph17092997 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bo, H. X., Li, W., Yang, Y., Wang, Y., Zhang, Q., Cheung, T., … Xiang, Y. T. (2020). Posttraumatic stress symptoms and attitude toward crisis mental health services among clinically stable patients with COVID-19 in China. Psychological Medicine, Mar 27, 1–2. doi: 10.1017/s0033291720000999 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brooks, S. K., Webster, R. K., Smith, L. E., Woodland, L., Wessely, S., Greenberg, N., & Rubin, G. J. (2020). The psychological impact of quarantine and how to reduce it: Rapid review of the evidence. Lancet (London, England), 395(10227), 912–920. doi: 10.1016/s0140-6736(20)30460-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cao, W., Fang, Z., Hou, G., Han, M., Xu, X., Dong, J., & Zheng, J. (2020). The psychological impact of the COVID-19 epidemic on college students in China. Psychiatry Research, 287, 112934. doi: 10.1016/j.psychres.2020.112934 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cenat, J. M., Mukunzi, J. N., Noorishad, P. G., Rousseau, C., Derivois, D., & Bukaka, J. (2020). A systematic review of mental health programs among populations affected by the Ebola virus disease. Journal of Psychosomatic Research, 131, 109966. doi: 10.1016/j.jpsychores.2020.109966 [DOI] [PubMed] [Google Scholar]
- Chen, Q., Liang, M., Li, Y., Guo, J., Fei, D., Wang, L., … Zhang, Z. (2020). Mental health care for medical staff in China during the COVID-19 outbreak. The Lancet Psychiatry, 7(4), e15–e16. doi: 10.1016/s2215-0366(20)30078-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chinese Society of Psychiatry (2020). Expert consensus on managing pathway and coping strategies for patients with mental disorders during prevention and control of infectious disease outbreak (novel coronavirus pneumonia) (in Chinese). Chinese Journal of Psychiatry, 53(2), 78–83. doi: 10.3760/cma.j.cn113661-20200219-00039 [DOI] [Google Scholar]
- Cole, C. L., Waterman, S., Hunter, E. C. M., Bell, V., Greenberg, N., Rubin, G. J., … Beck, A. (2020). Effectiveness of small group cognitive behavioural therapy for anxiety and depression in Ebola treatment centre staff in Sierra Leone. International Review of Psychiatry (Abingdon, England), Apr 17, 1–9. doi: 10.1080/09540261.2020.1750800 [DOI] [PubMed] [Google Scholar]
- Dawson, K. S., Bryant, R. A., Harper, M., Kuowei Tay, A., Rahman, A., Schafer, A., & van Ommeren, M. (2015). Problem Management Plus (PM + ): A WHO transdiagnostic psychological intervention for common mental health problems. World Psychiatry, 14(3), 354–357. doi: 10.1002/wps.20255 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Decosimo, C. A., Hanson, J., Quinn, M., Badu, P., & Smith, E. G. (2019). Playing to live: Outcome evaluation of a community-based psychosocial expressive arts program for children during the Liberian Ebola epidemic. Global Mental Health (Cambridge, England), 6, e3. doi: 10.1017/gmh.2019.1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Forbes, D., Creamer, M., Bisson, J. I., Cohen, J. A., Crow, B. E., Foa, E. B., … Ursano, R. J. (2010). A guide to guidelines for the treatment of PTSD and related conditions. Journal of Traumatic Stress, 23(5), 537–552. doi: 10.1002/jts.20565 [DOI] [PubMed] [Google Scholar]
- Galea, S., Merchant, R. M., & Lurie, N. (2020). The mental health consequences of COVID-19 and physical distancing: The need for prevention and early intervention. JAMA Internal Medicine, 180(6), 817–818. doi: 10.1001/jamainternmed.2020.1562. [DOI] [PubMed] [Google Scholar]
- Gao, J., Zheng, P., Jia, Y., Chen, H., Mao, Y., Chen, S., … Dai, J. (2020). Mental health problems and social media exposure during COVID-19 outbreak. PLoS ONE, 15(4), e0231924. doi: 10.1371/journal.pone.0231924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garriga, M., Agasi, I., Fedida, E., Pinzón-Espinosa, J., Vazquez, M., Pacchiarotti, I., & Vieta, E. (2020). The role of mental health home hospitalization care during the COVID-19 pandemic. Acta Psychiatrica Scandinavica, 141(5), 479–480. doi: 10.1111/acps.13173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gonzalez-Sanguino, C., Ausin, B., Castellanos, M. A., Saiz, J., Lopez-Gomez, A., Ugidos, C., & Munoz, M. (2020). Mental health consequences during the initial stage of the 2020 Coronavirus pandemic (COVID-19) in Spain. Brain, Behavior, and Immunity, 87, 172–176. doi: 10.1016/j.bbi.2020.05.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Higgins, J. P., Altman, D. G., Gøtzsche, P. C., Jüni, P., Moher, D., Oxman, A. D., … Sterne, J. A. (2011). The Cochrane Collaboration's tool for assessing risk of bias in randomised trials. BMJ-British Medical Journal, 343, d5928. doi: 10.1136/bmj.d5928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Higgins, J. P., & Green, S. (2009). Cochrane handbook for systematic reviews of interventions. Version 5.1.0. Cochrane Collaboration.
- Ho, C. S., Chee, C. Y., & Ho, R. C. (2020). Mental health strategies to combat the psychological impact of COVID-19 beyond paranoia and panic. Annals of the Academy of Medicine, Singapore, 49(1), 1–3. [PubMed] [Google Scholar]
- Hofmann, S. G., & Gomez, A. F. (2017). Mindfulness-based interventions for anxiety and depression. The Psychiatric Clinics of North America, 40(4), 739–749. doi: 10.1016/j.psc.2017.08.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holmes, E. A., O'Connor, R. C., Perry, V. H., Tracey, I., Wessely, S., Arseneault, L., … Bullmore, E. (2020). Multidisciplinary research priorities for the COVID-19 pandemic: A call for action for mental health science. The Lancet Psychiatry, 7(6), 547–560. doi: 10.1016/s2215-0366(20)30168-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Isaksson Rø, K., Veggeland, F., & & Aasland, O. G. (2016). Peer counselling for doctors in Norway: A qualitative study of the relationship between support and surveillance. Social Science & Medicine (1982), 162, 193–200. doi: 10.1016/j.socscimed.2016.06.037. [DOI] [PubMed] [Google Scholar]
- Jalloh, M. F., Li, W., Bunnell, R. E., Ethier, K. A., O'Leary, A., Hageman, K. M., … Redd, J. T. (2018). Impact of Ebola experiences and risk perceptions on mental health in Sierra Leone, July 2015. BMJ Global Health, 3(2), e000471. doi: 10.1136/bmjgh-2017-000471 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jung, S. J., & Jun, J. Y. (2020). Mental health and psychological intervention amid COVID-19 outbreak: Perspectives from South Korea. Yonsei Medical Journal, 61(4), 271–272. doi: 10.3349/ymj.2020.61.4.271 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kamara, S., Walder, A., Duncan, J., Kabbedijk, A., Hughes, P., & Muana, A. (2017). Mental health care during the Ebola virus disease outbreak in Sierra Leone. Bulletin of the World Health Organization, 95(12), 842–847. doi: 10.2471/blt.16.190470 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kang, L., Li, Y., Hu, S., Chen, M., Yang, C., Yang, B. X., … Liu, Z. (2020). The mental health of medical workers in Wuhan, China dealing with the 2019 novel coronavirus. The Lancet Psychiatry, 7(3), e14. doi: 10.1016/s2215-0366(20)30047-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaplan, H. S., Trumble, B. C., Stieglitz, J., Mamany, R. M., Cayuba, M. G., Moye, L. M., … Gurven, M. D. (2020). Voluntary collective isolation as a best response to COVID-19 for indigenous populations? A case study and protocol from the Bolivian Amazon. Lancet (London, England), 395(10238), 1727–1734. doi: 10.1016/s0140-6736(20)31104-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kerst, A., Zielasek, J., & Gaebel, W. (2020). Smartphone applications for depression: A systematic literature review and a survey of health care professionals’ attitudes towards their use in clinical practice. European Archives of Psychiatry and Clinical Neuroscience, 270(2), 139–152. doi: 10.1007/s00406-018-0974-3 [DOI] [PubMed] [Google Scholar]
- King, D. L., Delfabbro, P. H., Billieux, J., & Potenza, M. N. (2020). Problematic online gaming and the COVID-19 pandemic. Journal of Behavioral Addictions, 9(2), 184–186. doi: 10.1556/2006.2020.00016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koffel, E., Bramoweth, A. D., & Ulmer, C. S. (2018). Increasing access to and utilization of cognitive behavioral therapy for insomnia (CBT-I): A narrative review. Journal of General Internal Medicine, 33(6), 955–962. doi: 10.1007/s11606-018-4390-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kohrt, B. A., Blasingame, E., Compton, M. T., Dakana, S. F., Dossen, B., Lang, F., … Cooper, J. (2015). Adapting the Crisis Intervention Team (CIT) model of police-mental health collaboration in a low-income, post-conflict country: Curriculum development in Liberia, West Africa. American Journal of Public Health, 105(3), e73–80. doi: 10.2105/ajph.2014.302394 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lai, J., Ma, S., Wang, Y., Cai, Z., Hu, J., Wei, N., … Hu, S. (2020). Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019. JAMA Network Open, 3(3), e203976. doi: 10.1001/jamanetworkopen.2020.3976 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li, W., Yang, Y., Liu, Z. H., Zhao, Y. J., Zhang, Q., Zhang, L., … Xiang, Y. T. (2020a). Progression of mental health services during the COVID-19 outbreak in China. International Journal of Biological Sciences, 16(10), 1732–1738. doi: 10.7150/ijbs.45120 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li, J., Yang, Z., Qiu, H., Wang, Y., Jian, L., Ji, J., & Li, K. (2020b). Anxiety and depression among general population in China at the peak of the COVID-19 epidemic. World Psychiatry, 19(2), 249–250. doi: 10.1002/wps.20758 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu, S., Yang, L., Zhang, C., Xiang, Y. T., Liu, Z., Hu, S., & Zhang, B. (2020). Online mental health services in China during the COVID-19 outbreak. The Lancet Psychiatry, 7(4), e17–e18. doi: 10.1016/s2215-0366(20)30077-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lund, C., Brooke-Sumner, C., Baingana, F., Baron, E. C., Breuer, E., Chandra, P., … Saxena, S. (2018). Social determinants of mental disorders and the Sustainable Development Goals: A systematic review of reviews. The Lancet Psychiatry, 5(4), 357–369. doi: 10.1016/s2215-0366(18)30060-9 [DOI] [PubMed] [Google Scholar]
- Mak, I. W., Chu, C. M., Pan, P. C., Yiu, M. G., & Chan, V. L. (2009). Long-term psychiatric morbidities among SARS survivors. General Hospital Psychiatry, 31(4), 318–326. doi: 10.1016/j.genhosppsych.2009.03.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- MOE-China. (2020, March 20). In response to the epidemic, the Psychology Department of Beijing Normal University has opened a psychological support hotline and online counselling service (in Chinese). Retrieved from http://www.moe.gov.cn/jyb_xwfb/moe_1946/fj_2020/202001/t20200128_416724.html.
- Moreno, C., Wykes, T., Galderisi, S., Nordentoft, M., Crossley, N., Jones, N., … Arango, C. (2020). How mental health care should change as a consequence of the COVID-19 pandemic. The Lancet Psychiatry, 7(9), 813–824. doi: 10.1016/s2215-0366(20)30307-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Naslund, J. A., Aschbrenner, K. A., Araya, R., Marsch, L. A., Unutzer, J., Patel, V., & Bartels, S. J. (2017). Digital technology for treating and preventing mental disorders in low-income and middle-income countries: A narrative review of the literature. The Lancet Psychiatry, 4(6), 486–500. doi: 10.1016/s2215-0366(17)30096-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ng, S. M., Chan, T. H., Chan, C. L., Lee, A. M., Yau, J. K., Chan, C. H., & Lau, J. (2006). Group debriefing for people with chronic diseases during the SARS pandemic: Strength-Focused and Meaning-Oriented Approach for Resilience and Transformation (SMART). Community Mental Health Journal, 42(1), 53–63. doi: 10.1007/s10597-005-9002-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- NHC-China. (2020a, February 7). Guidelines for psychological assistance hotlines during 2019-nCoV pneumonia epidemic (in Chinese). Retrieved from http://www.nhc.gov.cn/jkj/s3577/202002/f389f20cc1174b21b981ea2919beb8b0.shtml.
- NHC-China. (2020b, January 26). Guidelines on psychological crisis intervention for COVID-19 emergency (in Chinese). Retrieved from http://www.nhc.gov.cn/xcs/zhengcwj/202001/6adc08b966594253b2b791be5c3b9467.shtml.
- NHC-China. (2020c, February 26). Notice on carrying out online services to further strengthen the epidemic prevention and control work in Hubei Province (in Chinese). Retrieved from http://www.nhc.gov.cn/xcs/zhengcwj/202002/91b668d87cd1443bbba1ee9c706be14b.shtml?from=timeline&isappinstalled=0.
- NHC-China. (2020d, February 18). Notice on management of severe psychiatric patients during COVID-19 epidemic (in Chinese). Retrieved from http://www.nhc.gov.cn/jkj/s3577/202002/f315a6bb2955474c8ca0b33b0c356a32.shtml.
- NHC-China. (2020e, February 2). Notice on psychological assistance hotlines during 2019-nCoV pneumonia epidemic (in Chinese). Retrieved from http://www.nhc.gov.cn/jkj/s3577/202002/8f832e99f446461a87fbdceece1fdb02.shtml.
- NHC-China. (2020f, February 18). Notice on strengthening the treatment and management of patients with severe mental disorders during the outbreak of the New Coronary Pneumonia (in Chinese). Retrieved from http://www.nhc.gov.cn/jkj/s3577/202002/f315a6bb2955474c8ca0b33b0c356a32shtml.
- NHC-China. (2020g, March 18). Workplan of psychological counseling and treatment for COVID-19 (in Chinese). Retrieved from http://www.nhc.gov.cn/jkj/s3577/202003/0beb22634f8a4a48aecf405c289fc25e.shtml.
- North, C. S., Hong, B. A., & Pfefferbaum, B. (2008). p-FLASH: Development of an empirically-based post-9/11 disaster mental health training program. Missouri Medicine, 105(1), 62–66. [PubMed] [Google Scholar]
- North, C. S., & Pfefferbaum, B. (2002). Research on the mental health effects of terrorism. JAMA, 288(5), 633–636. doi: 10.1001/jama.288.5.633 [DOI] [PubMed] [Google Scholar]
- North, C. S., & Pfefferbaum, B. (2013). Mental health response to community disasters: A systematic review. JAMA, 310(5), 507–518. doi: 10.1001/jama.2013.107799 [DOI] [PubMed] [Google Scholar]
- North, C. S., Suris, A. M., Davis, M., & Smith, R. P. (2009). Toward validation of the diagnosis of posttraumatic stress disorder. The American Journal of Psychiatry, 166(1), 34–41. doi: 10.1176/appi.ajp.2008.08050644 [DOI] [PubMed] [Google Scholar]
- Park, S. C., & Park, Y. C. (2020). Mental health care measures in response to the 2019 novel coronavirus outbreak in Korea. Psychiatry Investigation, 17(2), 85–86. doi: 10.30773/pi.2020.0058 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Percudani, M., Corradin, M., Moreno, M., Indelicato, A., & Vita, A. (2020). Mental health services in Lombardy during COVID-19 outbreak. Psychiatry Research, 288, 112980. doi: 10.1016/j.psychres.2020.112980 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pfefferbaum, B., Flynn, B. W., Schonfeld, D., Brown, L. M., Jacobs, G. A., Dodgen, D., … Lindley, D. (2012). The integration of mental and behavioral health into disaster preparedness, response, and recovery. Disaster Medicine and Public Health Preparedness, 6(1), 60–66. doi: 10.1001/dmp.2012.1 [DOI] [PubMed] [Google Scholar]
- Pfefferbaum, B., & North, C. S. (2020). Mental health and the Covid-19 pandemic. The New England Journal of Medicine, 383(6), 510–512. doi: 10.1056/NEJMp2008017 [DOI] [PubMed] [Google Scholar]
- Ping, N. P. T., Shoesmith, W. D., James, S., Nor Hadi, N. M., Yau, E. K. B., & Lin, L. J. (2020). Ultra brief psychological interventions for covid-19 pandemic: Introduction of a locally-adapted brief intervention for mental health and psychosocial support service. Malaysian Journal of Medical Sciences, 27(2), 51–56. doi: 10.21315/mjms2020.27.2.6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Poremski, D., Subner, S., Lam, G., Kin, F., Dev, R., Mok, Y. M., … Fung, D. S. (2020). Effective infection prevention and control strategies in a large accredited psychiatric facility in Singapore. Infection Control and Hospital Epidemiology, 41(10), 1–7. doi: 10.1017/ice.2020.163 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qiu, J. Y., Zhou, D. S., Liu, J., & Yuan, T. F. (2020). Mental wellness system for COVID-19. Brain, Behavior, and Immunity, 87, 51–52. doi: 10.1016/j.bbi.2020.04.032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Que, J., Shi, L., Deng, J., Liu, J., Zhang, L., Wu, S., … Lu, L. (2020). Psychological impact of the COVID-19 pandemic on healthcare workers: A cross-sectional study in China. General Psychiatry, 33(3), e100259. doi: 10.1136/gpsych-2020-100259 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rastegar Kazerooni, A., Amini, M., Tabari, P., & Moosavi, M. (2020). Peer mentoring for medical students during COVID-19 pandemic via a social media platform. Medical Education, 54(8), 762–763. doi: 10.1111/medu.14206 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reyes, G., & Elhai J. (2004). Psychosocial interventions in the early phases of disasters. Psychotherapy: Theory, Research, Practice, Training, 41(4), 399–411. doi: 10.1037/0033-3204.41.4.399 [DOI] [Google Scholar]
- Riemann, D., Baglioni, C., Bassetti, C., Bjorvatn, B., Dolenc Groselj, L., Ellis, J. G., … Spiegelhalder, K. (2017). European guideline for the diagnosis and treatment of insomnia. Journal of Sleep Research, 26(6), 675–700. doi: 10.1111/jsr.12594 [DOI] [PubMed] [Google Scholar]
- Rogers, J. P., Chesney, E., Oliver, D., Pollak, T. A., McGuire, P., Fusar-Poli, P., … David, A. S. (2020). Psychiatric and neuropsychiatric presentations associated with severe coronavirus infections: A systematic review and meta-analysis with comparison to the COVID-19 pandemic. The Lancet Psychiatry, 7(7), 611–627. doi: 10.1016/S2215-0366(20)30203-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schreiber, M., Cates, D. S., Formanski, S., & King, M. (2019). Maximizing the resilience of healthcare workers in multi-hazard events: Lessons from the 2014-2015 Ebola response in Africa. Military Medicine, 184(Suppl 1), 114–120. doi: 10.1093/milmed/usy400 [DOI] [PubMed] [Google Scholar]
- Shao, Y., Shao, Y., & Fei, J. M. (2020). Psychiatry hospital management facing COVID-19: From medical staff to patients. Brain, Behavior, and Immunity, 88, 947. doi: 10.1016/j.bbi.2020.04.018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shi, L., Lu, Z. A., Que, J. Y., Huang, X. L., Liu, L., Ran, M. S., … Lu, L. (2020). Prevalence of and risk factors associated with mental health symptoms among the general population in China during the Coronavirus disease 2019 pandemic. JAMA Network Open, 3(7), e2014053. doi: 10.1001/jamanetworkopen.2020.14053 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singla, D. R., Kohrt, B. A., Murray, L. K., Anand, A., Chorpita, B. F., & Patel, V. (2017). Psychological treatments for the world: Lessons from low- and middle-income countries. Annual Review of Clinical Psychology, 13, 149–181. doi: 10.1146/annurev-clinpsy-032816-045217 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Slavich, G. M. (2020). Social safety theory: A biologically based evolutionary perspective on life stress, health, and behavior. Annual Review of Clinical Psychology, 16, 265–295. doi: 10.1146/annurev-clinpsy-032816-045159 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith, A. C., Thomas, E., Snoswell, C. L., Haydon, H., Mehrotra, A., Clemensen, J., & Caffery, L. J. (2020). Telehealth for global emergencies: Implications for coronavirus disease 2019 (COVID-19). Journal of Telemedicine and Telecare, 26(5), 309–313. doi: 10.1177/1357633x20916567 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Starace, F., & Ferrara, M. (2020). COVID-19 disease emergency operational instructions for mental health departments issued by the Italian society of epidemiological psychiatry. Epidemiology and Psychiatric Sciences, 29, e116. doi: 10.1017/s2045796020000372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sun, Y., Bao, Y., & Lu, L. (2020). Addressing mental health care for the bereaved during the COVID-19 pandemic. Psychiatry and Clinical Neurosciences, 74(7), 406–407. doi: 10.1111/pcn.13008 [DOI] [PubMed] [Google Scholar]
- Sun, Y., Li, Y., Bao, Y., Meng, S., Sun, Y., Schumann, G., … Shi, J. (2020). Brief report: Increased addictive internet and substance use behavior during the COVID-19 pandemic in China. The American Journal on Addictions, 29(4), 268–270. doi: 10.1111/ajad.13066 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tang, W., Hu, T., Hu, B., Jin, C., Wang, G., Xie, C., … Xu, J. (2020). Prevalence and correlates of PTSD and depressive symptoms one month after the outbreak of the COVID-19 epidemic in a sample of home-quarantined Chinese university students. Journal of Affective Disorders, 274, 1–7. doi: 10.1016/j.jad.2020.05.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Torniainen-Holm, M., Pankakoski, M., Lehto, T., Saarelma, O., Mustonen, P., Joutsenniemi, K., & Suvisaari, J. (2016). The effectiveness of email-based exercises in promoting psychological wellbeing and healthy lifestyle: A two-year follow-up study. BMC Psychology, 4(1), 21. doi: 10.1186/s40359-016-0125-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trauer, J. M., Qian, M. Y., Doyle, J. S., Rajaratnam, S. M., & Cunnington, D. (2015). Cognitive behavioral therapy for chronic insomnia: A systematic review and meta-analysis. Annals of Internal Medicine, 163(3), 191–204. doi: 10.7326/M14-2841 [DOI] [PubMed] [Google Scholar]
- Turgoose, D., Ashwick, R., & Murphy, D. (2018). Systematic review of lessons learned from delivering tele-therapy to veterans with post-traumatic stress disorder. Journal of Telemedicine and Telecare, 24(9), 575–585. doi: 10.1177/1357633x17730443 [DOI] [PubMed] [Google Scholar]
- Vyas, K. J., Delaney, E. M., Webb-Murphy, J. A., & Johnston, S. L. (2016). Psychological impact of deploying in support of the U. S. response to Ebola: A systematic review and meta-analysis of past outbreaks. Military Medicine, 181(11), e1515–e1531. doi: 10.7205/milmed-d-15-00473 [DOI] [PubMed] [Google Scholar]
- Wang, H., Li, T., Gauthier, S., Yu, E., Tang, Y., Barbarino, P., … Yu, X. (2020a). Coronavirus epidemic and geriatric mental healthcare in China: How a coordinated response by professional organizations helped older adults during an unprecedented crisis. International Psychogeriatrics, Apr 9, 1–4. doi: 10.1017/S1041610220000551 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang, C., Pan, R., Wan, X., Tan, Y., Xu, L., Ho, C. S., & Ho, R. C. (2020b). Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in China. International Journal of Environmental Research and Public Health, 17(5), 1729. doi: 10.3390/ijerph17051729 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang, Y., Zhao, X., Feng, Q., Liu, L., Yao, Y., & Shi, J. (2020c). Psychological assistance during the coronavirus disease 2019 outbreak in China. Journal of Health Psychology, 25(6), 733–737. doi: 10.1177/1359105320919177 [DOI] [PubMed] [Google Scholar]
- Waterman, S., Cole, C. L., Greenberg, N., Rubin, G. J., & Beck, A. (2019). A qualitative study assessing the feasibility of implementing a group cognitive-behavioural therapy-based intervention in Sierra Leone. BJPsych International, 16(2), 31–34. doi: 10.1192/bji.2018.7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Waterman, S., Hunter, E. C. M., Cole, C. L., Evans, L. J., Greenberg, N., Rubin, G. J., & Beck, A. (2018). Training peers to treat Ebola centre workers with anxiety and depression in Sierra Leone. The International Journal of Social Psychiatry, 64(2), 156–165. doi: 10.1177/0020764017752021 [DOI] [PubMed] [Google Scholar]
- WHO. (2020, March 11). WHO characterizes COVID-19 as a pandemic. Retrieved from https://www.who.int/emergencies/diseases/novel-coronavirus-2019/events-as-they-happen.
- Wu, P., Fang, Y., Guan, Z., Fan, B., Kong, J., Yao, Z., … Hoven, C. W. (2009). The psychological impact of the SARS epidemic on hospital employees in China: Exposure, risk perception, and altruistic acceptance of risk. Canadian Journal of Psychiatry. Revue Canadienne de Psychiatrie, 54(5), 302–311. doi: 10.1177/070674370905400504 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xiang, Y. T., Zhao, Y. J., Liu, Z. H., Li, X. H., Zhao, N., Cheung, T., & Ng, C. H. (2020). The COVID-19 outbreak and psychiatric hospitals in China: Managing challenges through mental health service reform. International Journal of Biological Sciences, 16(10), 1741–1744. doi: 10.7150/ijbs.45072 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xiao, H., Zhang, Y., Kong, D., Li, S., & Yang, N. (2020). Social capital and sleep quality in individuals who self-isolated for 14 days during the coronavirus disease 2019 (COVID-19) outbreak in January 2020 in China. Medical Science Monitor, 26, e923921. doi: 10.12659/MSM.923921 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yao, H., Chen, J. H., & Xu, Y. F. (2020). Rethinking online mental health services in China during the COVID-19 epidemic. Asian Journal of Psychiatry, 50, 102015. doi: 10.1016/j.ajp.2020.102015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yao, H., Chen, J. H., Zhao, M., Qiu, J. Y., Koenen, K. C., Stewart, R., … Xu, Y. F. (2020). Mitigating mental health consequences during the COVID-19 outbreak: Lessons from China. Psychiatry and Clinical Neurosciences, 74(7), 407–408. doi: 10.1111/pcn.13018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yoon, M. K., Kim, S. Y., Ko, H. S., & Lee, M. S. (2016). System effectiveness of detection, brief intervention and refer to treatment for the people with post-traumatic emotional distress by MERS: A case report of community-based proactive intervention in South Korea. International Journal of Mental Health Systems, 10, 51. doi: 10.1186/s13033-016-0083-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhou, X. (2020). Psychological crisis interventions in Sichuan Province during the 2019 novel coronavirus outbreak. Psychiatry Research, 286, 112895. doi: 10.1016/j.psychres.2020.112895 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhou, X., Snoswell, C. L., Harding, L. E., Bambling, M., Edirippulige, S., Bai, X., & Smith, A. C. (2020). The role of telehealth in reducing the mental health burden from COVID-19. Telemedicine Journal and e-Health, 26(4), 377–379. doi: 10.1089/tmj.2020.0068 [DOI] [PubMed] [Google Scholar]