Abstract
Background
Natural disasters can affect mental health and result in symptoms of depression, anxiety, and post-traumatic stress disorder (PTSD). Playback Theatre (PT) is a form of improvisation where actors play-back personal stories told by audience members. Whether PT can be therapeutic in post-disaster settings is not known.
Method
We used a series of PT performances and studied levels of depression, anxiety, and PTSD symptoms in a sample of 13 people affected by Hurricane Harvey that happened in Houston, TX, August 2017. Brain imaging, specifically resting state functional connectivity of the amygdala was also studied before and after the PT performances.
Results
Both anxiety (p = .001, Cohen’s d = –1.25) and PTSD (p = .002, Cohen’s d = –1.0) symptoms significantly decreased after a series of 4 PT performances from January 2019 – February 2019. Depression reduction was not significant. We performed resting state functional connectivity (RSFC) MRI before and after the series of performances. We used the right and left amygdala as seeds for RSFC analysis and found that the connectivity between the left amygdala and the bilateral supramarginal gyri was increased after PT. The bilateral supramarginal connectivity with the default mode and the saliency networks increased too, which correlated with reduction in anxiety scores.
Conclusions
PT may offer a form of intervention for anxiety caused by disasters. An increase in left amygdala/supramarginal gyri connectivity may be the underlying mechanism.
Keywords: amygdala, art therapy, supramarginal gyrus, default mode network, Hurricane Harvey, natural disasters, PTSD, Resting state functional connectivity
Introduction
Disasters and Mental Health
About 13–19% of adults in the USA experience a disaster in their lifetime.1,2 Several negative mental health consequences are associated with disaster exposure,3 and techniques such as psychological debriefing and psychological first-aid can help with coping in the aftermath of disasters.4 Negative mental health outcomes include increased symptoms of depression, post-traumatic stress, and anxiety.5
Prevalence of PTSD has been estimated at 30–40% among direct disaster victims, 10–20% among rescue workers, and 5–10% in the general population,3,6,7 and generalized anxiety disorder (GAD) is also increased among those affected by disasters.8,9 Major Depression Disorder (MDD) has also repeatedly been shown to be increased after disasters. For example, 5% of the population affected by Hurricane Ike in Texas met criteria for MDD in the following month,10 and almost 10% of adult New Yorkers showed MDD symptoms the month following the 9/11 attacks.11 People exposed to disasters often report poor sleep quality, possibly due to grief over loss and anxiety about disaster reoccurrence.12 Poor sleep quality has been associated with multiple psychiatric symptoms.13
After disasters, many of those affected show subclinical symptoms and do not seek mental health help. These widespread subclinical issues affect a large portion of the population after a disaster and negatively affect quality of life.14 There are likely several reasons why many of those with symptoms won’t receive specialized help, including financial considerations, general avoidance of traditional therapeutic interventions, and stigma associated with needing mental health help. Our proposed intervention (see below) directly addresses these barriers.
Hurricane Harvey hit Houston in August 2017 leaving ∼200,000 damaged homes and causing $125 billion in damage. The mental health effects of this hurricane have been described as significant,15,16 including both depression and PTSD symptoms. The degree of mental health issues was associated with that of exposure to traumatic situations.
Playback Theatre as a Possible Therapeutic Aid for Groups That Share Exposure to Traumatic Events
Playback Theatre (PT) is an improvisational form of theatre that was developed in the 1970s in New York by the Original Playback Company and has grown over time such that there are currently PT companies in many countries and in most large American cities.17–19 In a typical PT performance, there is a master of ceremonies (the conductor), a musician, and 3–5 actors on stage. After a brief introduction, the conductor asks members in the audience to share a moment or a feeling from their life. Once an audience member (the teller) shares a moment or feeling, the actors and musician play-back the moment with a brief enactment using one of several possible theatrical forms. These forms allow for re-telling the moment using different techniques, e.g., narrative, poetic, abstract, and humorous. Some of the techniques are similar to popular improvisation comedy, but with a very different general tone. Although PT usually has many funny moments, the underlying message is to honor the human experience, not to ridicule it. A rule is that tellers must share a true moment, experience, or feeling from their life. In performances with a set theme, like the ones we used in this study, the moments should all be related to a particular topic. PT is not a form of therapy in a clinical sense, but it can be adapted for use with therapeutic intentions by therapists, and PT itself shares elements with psychodrama.20
Houston PT is an amateur company founded in 1996, with 8 current members, some of whom have been performing for at least a decade and 3 new members who were participating as actors in their first PT performances ever. It is common that PT companies are formed by amateur actors and musicians, as the power of the form lies not in the beauty or professionalism of the art, but on the truthful telling (by the teller) and re-telling (by the actors) of personally important stories.
PT has already been used as a possible therapeutic help in trauma.21 In that report, participants with serious mental illness were given a course of PT (training more than performances). They showed, using self-report measures, that PT training was effective in terms of self-esteem, personal growth, and recovery.
We show here that a series of four PT performances specifically geared towards sharing experiences related to Hurricane Harvey in Houston, Texas were therapeutic, according to self-reports with brain imaging correlations. The number of performances was chosen based on James Pennebaker’s expressive writing studies that repeatedly showed that writing four times about one’s traumatic events result in measurable therapeutic effects.22
Resting State Functional Connectivity as a Biomarker of Mental Health Symptoms
Resting state functional connectivity (RSFC) is a non-invasive brain imaging technique that has gained notoriety in the last few years. Briefly, functional images are collected in an MRI scanner while the participant is not performing any task, but simply relaxing. Under these conditions, the correlations in low frequency signal fluctuations (spontaneous increases and decreases in brain activity) among different brain regions are a proxy for functional connectivity between those regions. This observation23 allowed for the study of differences in RSFC associated with specific illnesses. For example, subjects with PTSD have decreased strength of the default mode network. The default mode network (encompassing regions usually more active during rest) comprises aspects of the ventromedial prefrontal cortex, dorsomedial prefrontal cortex, posterior cingulate cortex, as well as the precuneus, medial temporal lobe, and the medial and lateral parietal cortices.24 The default mode network is known to be hyper-connected in brains of MDD patients,25 which suggests that self-referential processes are increased in the brains of depressed patients. In addition, the connectivity between the bilateral amygdala and the right26 and left27 supramarginal gyri is decreased in anxiety disorder patients. The amygdala process fear, while the supramarginal gyrus is involved, among other behaviors, with empathy,28 suggesting that decreased amygdala/supramarginal connectivity in anxiety patients may be associated to the interplay between social cognition and stress and fear. Although these are not necessarily individually actionable biomarkers because it is not (at least currently) possible to diagnose a patient by only measuring RSFC, these are statistically valid and robust biomarkers at the group level. Our objective for this work was to study whether a course of four PT performances can have a therapeutic effect on anxiety, depression, or PTDS symptoms in a group of people sharing a common traumatic event: the flooding of their house due to Hurricane Harvey, and whether a brain connectivity characteristic (amygdala connectivity) could be a possible biomarker of such effect. Our hypotheses were that a) Four weekly PT performances would decrease self-reported levels of anxiety (primary hypothesis), depression, and PTSD symptoms; and b) Changes in RSFC between before and after the four PT performances could help explain the possible mechanisms of such self-reported symptoms. Specifically, we hypothesized that amygdala RSFC could be altered in ways consistent with a decrease in anxiety and PTSD symptoms (thus amygdala connectivity may be a biomarker of improvement in anxiety in this setting, primary hypothesis). In addition, the default mode network, the attention network, and the saliency network could change in ways consistent with improvements in any of the three measures (thus, these networks could also act as biomarkers of improvement in our study).
Material and Methods
Participants
We recruited 13 adult participants (5 females; age = 48.2 ± 4.0 (s.e.m) years old; 6 Hispanic, 6 White, 1 Asian) whose houses had flooded during Hurricane Harvey. We did not recruit for any specific levels of mental health symptoms. Importantly, about a year and a half had passed between Hurricane Harvey and the PT intervention, which highlights the sustained mental health effects following the trauma and suggests that it was not simply the 6 weeks that passed between the two measures having an effect intrinsically—the intervention itself may have helped. This is an important consideration to at least consider as traditionally one should be wary of confounding factors related to the passage of time when analyzing before/after effects. All participants were present at all four performances except for one participant who missed one of the performances. Inclusion criteria were: male and female adults (18-64 years old), having suffered flooding in their house due to Hurricane Harvey, and being able to consent. Contraindications for MRI were exclusionary only for the MRI part of the study, but not for performances and self-report. All participants self-reported being in good, very good, or excellent health both before and after Hurricane Harvey. Participants signed informed consent, and procedures were approved by Baylor College of Medicine Institutional Review Board.
Playback Theatre Performances
Participants were asked to be available for 6 consecutive weeks, once a week, 2 hours each time (no compensation was provided). On weeks 1 and 6, they answered a number of questionnaires and underwent fMRI scanning. During weeks 2-5, they attended PT performances at Baylor College of Medicine in Houston, Texas. The general content of the shared stories was qualitatively analyzed by Houston PT company members during informal discussions after each performance. These discussions included the content of stories (whether they had sad, fearful, and fun elements, for example), the choices made by the company at how to portray each story, whether there was any pattern on which participants told stories, whether there was a spontaneous “theme” for each performance as it is common in PT that one story told by a participant elicits a specific related story in another participant, etc.
Clinical Measures
Besides a questionnaire on demographics and exposure to Harvey, we used measures for anxiety (HAM-A29) PTSD symptoms (PCL530) and depression (QIDS-SR31). These were answered by participants both the week before the first and the week after the fourth PT performances. The questionnaires were chosen for ease of administration including being fast to be answered. Despite possibly not being a very reliable measure for changes in anxiety during treatment,32 the HAM-A has shown good intraclass correlation33 and is very commonly used so it was chosen for those reasons, and for ease and speed for administration. The scores range from 0–56, with scores < 7 typically accepted as non-anxious, 8–17 mild severity, 18–24 moderate, 25–30 moderate to severe, and >30 severe anxiety.34 QIDS-SR, with a total score from 0 to 27 (0–5 none, 6–10 mild, 11–15 moderate, 16–20 severe, 21–27 very severe), has shown high validity when compared to other more cumbersome measures such as QIDS-C (clinician rated) or the Hamilton Rating Scale for Depression.31 Finally, PCL-5 has shown good reliability and validity,35 with scores from 0 to 80 and a minimally important difference of 6.36 In all three questionnaires, higher scores equate more symptoms.
Brain Imaging
Participants were scanned about a week before the first performance and about a week after the fourth performance in a 3 T Siemens Prisma at the Core for Advanced MR Imaging at Baylor College of Medicine. We used a T1 structural sequence (1.3 mm isotropic, TR: 1900 ms, TE: 2.84 ms, 3.08 minutes) followed by a 7-minute resting state BOLD sequence (2.2 mm isotropic, TR: 925 ms, TE: 37 ms, multi-band acceleration factor: 6). We chose a 7 minute-long resting time, as previously published to be an adequate length of time.37
RSFC Analysis
Preprocessing of the functional data including functional realignment and unwarp, functional slice-timing correction, structural segmentation and normalization, functional normalization, ART-based functional outlier detection and scrubbing, and functional smoothing (6 mm Gaussian kernel) were done in MNI-space using the CONN fMRI Functional Connectivity toolbox v1638 with SPM8. The Artifact Detection Toolbox (ART; http://www.nitrc.org/projects/artifact_detect/) was used for outlier detection and scrubbing as implemented in CONN with default (intermediate stringency) parameters. Realignment, scrubbing, white matter, and cerebrospinal fluid were entered as potential confounders in the subject-level GLM. Using the anatomical component correction (aCompCor) method of flexibly removing physiological noise and movement confounds on a voxel-by-voxel level, each of these effects was regressed out of the BOLD signal before connectivity measures were computed by the toolbox. Functional images were temporally band-pass filtered to investigate low frequency correlations. To avoid multiple comparison issues during data analysis, for primary outcome we used seeds in the right (R) and left (L) amygdala only. We contrasted the RSFC between the R and L amygdala with all other voxels in the brain before (pre) vs. after (post) the PT intervention. In addition, exploratorily we studied both amygdalae and brain networks known or hypothesized to be important in depression, anxiety, and PTSD symptoms, as implemented in CONN (for the default mode network (4 seeds), attention network (4 seeds), and saliency network (7 seeds)), using the difference in values (for anxiety, PTSD, and depression symptoms) as covariates of interest in the analysis, to study whether pre/post changes in any of the studied RSFC (related to the bilateral amygdala or networks) correlate with clinical improvement. The choice of these networks (plus the amygdala) for this analysis was again to constrain the number of comparisons, using just the amygdala and three brain networks that have been shown to be involved in brain signaling relevant to the current study.25–27,39–41 We used, as customary, a p < .001 (uncorrected) for peak voxel and a p < .05 (FDR corrected) for cluster significance levels (https://web.conn-toolbox.org/fmri-methods/cluster-level-inferences).
Statistics
The clinical outcomes were self-reported changes in anxiety, depression, and PTSD symptoms. Results were considered statistically significant if paired, two tailed Student’s t test had a p value of 0.05 or less. Although three independent tests were performed (anxiety, depression, PTSD symptoms), we did not feel the need for Bonferroni corrections for 3 comparisons because this work was mainly an exploratory pilot to decide whether our general hypotheses are worth further study.42 In addition, we calculated effect size (Cohen’s d) and 95% confidence intervals for the change between pre and post measure (DeltaAnxiety, DeltaPTSD, and DeltaDepression).
Results
Playback Theatre Performances
Participants shared moments, feelings, and short stories about their Hurricane Harvey experience. Some of these shared moments were:
Being in denial about the flood reaching their house and thinking the possible massive flooding was being blown out of proportion
Useless attempts to stop the flood waters from coming inside using towels or duct tape
Fearing for their lives from the rushing flood waters
Guilt about sitting comfortably in a hotel back in their home country while their family was in Houston, terrified
Feeling shame for showing up at rich neighbor’s elevated house in need of shelter
The frustration of dealing with insurance and contractors
Saving pets
Being uncomfortable due to having to deal/stay with strangers for long periods after the storm
Bonding with people that helped and becoming better friends with neighbors
Feeling grateful for unexpected help from fellow neighbors and strangers
Trying to find humor in their situations despite all of the chaos
Feeling strange when having to re-inhabit their rebuilt houses and feeling nostalgic about their time as Hurricane Harvey refugees
As is common in PT performances, stories tended to connect with each other. For example, in one of the performances there were 3 moments about dogs, all highlighting how important pets can be for a family. This spontaneous connection among stories is one of the reasons why we think PT would be most useful when audience members (and actors when possible) share the same traumatic experience.
Hurricane Harvey stories spontaneously emerged following a chronology of the events that could be described as (1) denial and preparation; (2) clean-up and rescues; (3) rebuilding and coming back. These three broad topics were loosely chronological with stories about denial and preparation being told mostly in the first performance, while feelings of shame, guilt, resentment, and puzzlement emerged mainly during performances 2–4 after audience members became familiar with each other. Accordingly, most stories about coming back were told at the last of the four performances.
Clinical Results
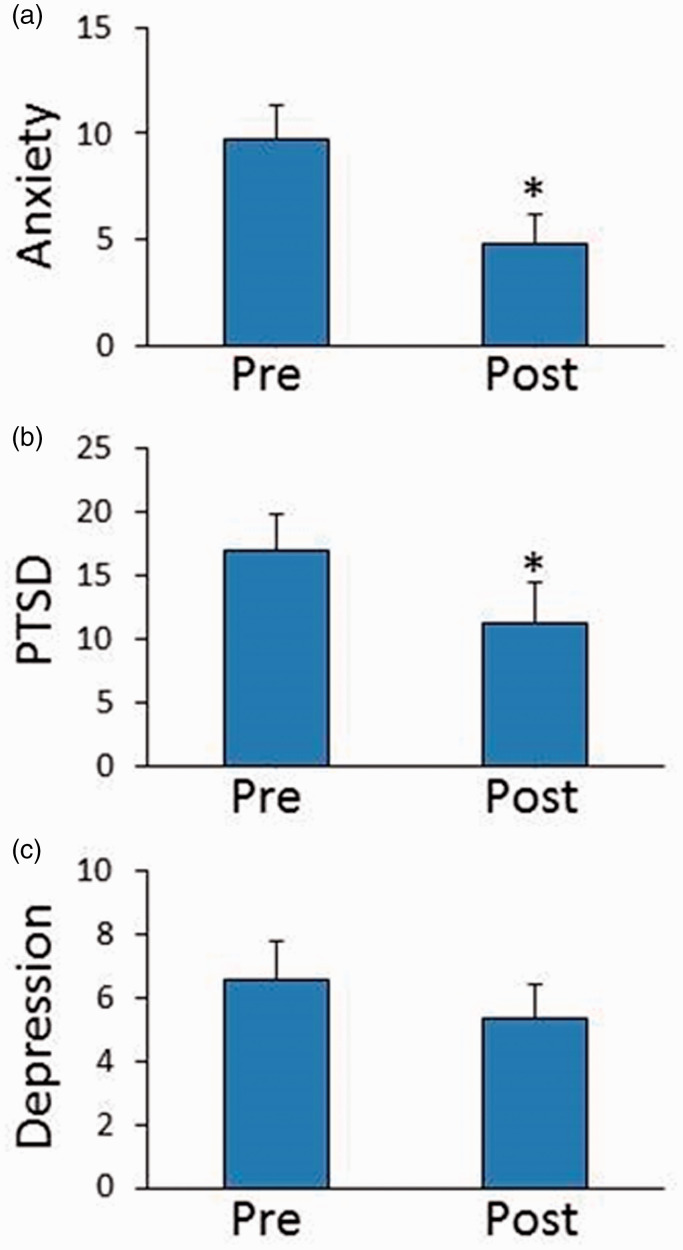
According to self-report from the participants, there were no adverse events; furthermore, none of the participants received any kind of therapy for anxiety, PTSD, depression or any other psychiatric illness during the study. In clinical self-reports we found that the participants started with mild levels of anxiety, depression, and PTSD symptoms. After the PT intervention, all three measures were decreased (Figure 1), with anxiety (mean (S.D.) pre: 9.8 (5.4), post: 4.8 (5.1); p = .001; Cohen’s d = –1.25) and PTSD (pre: 16.9 (10.5), post: 11.2 (11.6); p = .002; Cohen’s d = –1.0) showing significant changes, while depression showed a non-significant decrease (pre: 6.5 (4.5), post: 5.3 (4.1); p = .18; Cohen’s d = –0.39). For the post minus pre results, we obtained (mean (95% confidence intervals)) DeltaAnxiety = 4.98 (2.25, 6.92); DeltaPTSD = 5.77 (2.59, 8.95); DeltaDepression = 1.23, (–0.63, 3.10). Importantly, the anxiety scores shifted from mild (7–17) to no anxiety (0-7), suggesting a clinically relevant change. In addition, the minimally important difference in PCL5 is 6, and these scores changed by 5.8, suggesting clinically significant changes are likely.
Figure 1.
(a) Anxiety, (b) PTSD, and (c) depressive symptoms before (“Pre”) and after (“Post”) the 4-week playback theatre intervention. *p < 0.005 (two-tailed paired t-test).
Brain Imaging Results
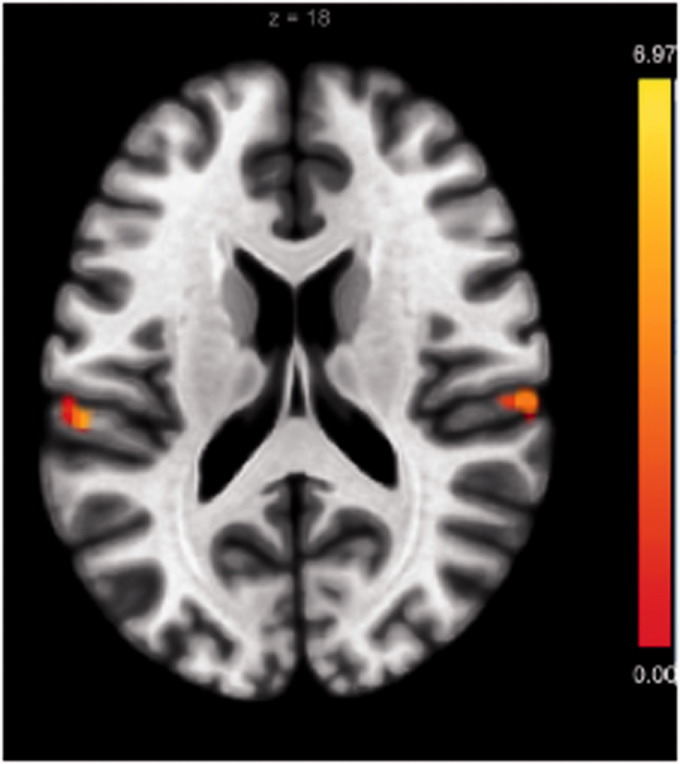
In primary MRI analysis, when we used L and R amygdala as seeds, we found that the L amygdala showed increased connectivity with the bilateral supramarginal gyri in the post- as compared to the pre- condition (Figure 2, Table 1).
Figure 2.
Resting state functional connectivity using left amygdala as seed is increased after the playback theatre intervention in two clusters in the bilateral supramarginal gyri. (Peak voxel p < 0.001, cluster p < 0.05 FDR corrected.).
Table 1.
Brain imaging results.
| Seed | Clusters (x,y,z) | Size | Size p-FDR | Size p-unc | Peak p-unc | Main region |
|---|---|---|---|---|---|---|
| Left amygdala | +60 −22 + 18 | 151 | .043 | .0023 | .000035 | Supramarginal Gyrus, anterior division Right, 87 voxels |
| Left amygdala | −56 −28 + 18 | 128 | .043 | .0044 | .000007 | Supramarginal Gyrus, anterior division Left, 45 voxels |
| Right Insula salience network | −54 −30 + 48 | 373 | .00031 | .000011 | .000001 | Supramarginal Gyrus, anterior division Left, 229 voxels |
| Right Insula salience network | +40 −34 + 42 | 221 | .0044 | .000352 | .000013 | Supramarginal Gyrus, anterior division Right, 92 voxels |
| Right Insula salience network | +58 −18 + 32 | 112 | .046 | .0051 | .000044 | Postcentral Gyrus Right, 101 voxels |
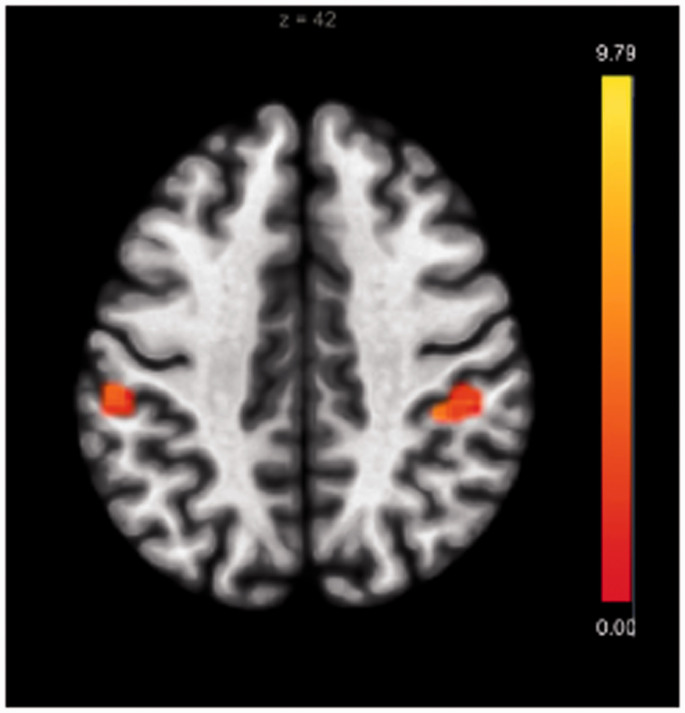
In exploratory MRI analysis, we found that when changes in HAM-A scores were used as covariates of interest, RSFC between the bilateral supramarginal gyri (supramarginal gyri, SMG) and the right anterior insula saliency network (one of the exploratory seeds used) was positively associated with improvement in anxiety self-report (Figure 3, Table 1). Despite this analysis being exploratory, the results of the association survived Bonferroni correction for all 17 comparisons studied.
Figure 3.
Resting state connectivity using anterior insula salience network and regression on HAM-A score improvement. Increased connectivity with the bilateral supramarginal gyri correlates with decreased anxiety scores. (Peak voxel p < 0.001, cluster p < 0.05 FDR corrected.).
Discussion
As discussed, Hurricane Harvey had serious mental health effects on Houstonians, and after disasters help is not readily available for many. Our data indicate that PT is a possible therapeutic aid for groups of people who share a common traumatic experience. Not only did we show that PT decreased anxiety and PTSD symptoms, we found a possible brain mechanism for that effect (increased RSFC between bilateral SMG and bilateral amygdala and anterior insula salience network). This is in agreement with previously published papers on brain connectivity signatures in anxiety disorders.26,27
PT is inexpensive and easy to deploy: A single person with sufficient PT experience can recruit a small group of actors/musicians (remember there is no need for these to be professional artists) and train them in ∼2 months. Given the obvious success of our pilot project (both subjectively by judging from the stories told and the comments from the audience, and from the quantitative results), we believe that PT can be successfully deployed with limited training (remember three of the actors were performing for the very first time), especially if there is guidance from more experienced practitioners. PT training is usually done by attending rehearsals in which new actors learn the mechanism of each improvisational form and perhaps more importantly, learn how to respond to real-life stories told by other members of the company. Our PT performances were done over a year after the traumatic event, so it is clear that for PT to benefit a population, it does not need to occur immediately following the event. This is mentioned here as well to consider the possibility of time being a factor here in the recovery process: Traditionally, when analyzing before and after tests, one should at least consider confounding factors related to the natural passage of time. For example, one should consider if the recovery was merely due to the passage of time that had elapsed after the hurricane-related events or if the intervention itself truly had an effect.
In terms of relating this work with that done by others in the field, Moran and Alon have conducted a study on PT and recovery in mental health, but with only self-report measures instead of also incorporating neuroimaging analyses for biomarkers. In Moran and Alon’s study, they assert that while participants may have various traumas or experiences that differ from one another, the sharing of many personal stories can help establish a setting that produces an environment in which stories can be received and responded to and connects one’s own story to others’ stories.21 Trauma itself is thought to disrupt the ability to create and process narratives, contributing to symptoms post-traumatic stress.43 Veterans have used first-person narrative telling, with a public audience, as a means to enhance connection between each other.44 Playback Theatre is somewhat unique in that participants both engage in first-person narrative telling and then get to be an observer as their story is re “played,” and it may be that the combination of these two parts fosters greater personal insight, narrative coherency, and interconnectedness, all of which may reduce symptoms of anxiety and post-traumatic stress. Additionally, ideas on how Playback Theatre may facilitate recovery for its audience are listed in the following:
See one’s perspective from the lens of another.
Re-author one’s personal story.
Shed one’s current identity and instead take on a new identity with varied and nuanced roles, e.g., mother or father, wife or husband, friend.21
One of the most often cited effects among PT practitioners (however, take with caution as this is merely anecdotal evidence) is a shared feeling of commonality in human experience. Therefore, we believe that for PT to be therapeutic it may be important that the audience members share the traumatic experience, which may enhance communication (in this case, all participants had their houses flooded during Hurricane Harvey).
Several limitations of this study include first, a small sample size (n = 13). However, this was partially mitigated by using a paired analysis which increases statistical power. The median sample size of fMRI studies is ∼3045 so it is possible that our power was close to average. In addition, the lack of a control group is another limitation and should be addressed in a follow up study: it is well known that both pharmacological and non-pharmacological treatments have large placebo effects, especially in depression46 and we cannot rule out placebo effects, or simply effects that are not truly associated with PT but with other factors. Furthermore, the way in which the PT (Playback Theatre) is conducted can matter and affect how audience members feel while participating in the performances as audience members or as tellers. For Houston PT, the guidelines that the team follow are that participation ought to be voluntary, and that no one is coerced into being a teller—one should feel comfortable and willing to tell of their own accord of whatever details and stories they wish to share. This distinction can be important, as we believe intimidating the audience to tell their stories can have a negative impact on audience members’ experiences. However, all participants in our study were tellers at two or more of the performances.
The results indicate that anxiety and PTSD symptoms, as measured by self-reported, validated scales, had decreased after PT performances. Moreover, this study provides a possible mechanism for the effect through the use of fMRI, namely the increased RSFC between SMG and both the amygdala and anterior insula salience network. However, the intervention did not demonstrate a statistically significant decrease in depressive symptoms. Possible explanations for this include that the depression manifested by participants was not related to the experience of Harvey, whereas the anxiety and traumatic stress symptoms may have been more specifically associated with the hurricane and therefore relieved by having a PT forum. Alternatively, it is possible that the pre-intervention levels of depression were very low in our small sample of participants, creating a floor effect. It is also possible that Playback, as suggested,21 enhances a sense of connection with and empathy for others. Empathy has previously been demonstrated as a treatment for anxiety and PTSD,47 and may be mediated by the supramarginal gyrus.28
In terms of the relevance of the use or importance of PT for natural disasters like hurricanes—a recent survey conducted by the Kaiser Family Foundation and the Episcopal Health Foundation indicated that three out of ten Gulf Coast residents’ lives continued to be affected by Harvey, one year later. Those most likely to say they aren’t getting the help they need to recover disproportionately tend to be racial minorities and low-income individuals.48 This can be an additional reason of importance for the availability of PT interventions for individuals who may be suffering from trauma due to natural disaster-related phenomena, as PT would be an easy to deploy, inexpensive intervention.
In the future, other questions to explore include whether there is a difference in intervention outcomes between people who share their stories (tellers) as opposed to audience members who do not actively participate in telling their stories but only listen; whether the fact that participants share the traumatic event is relevant; and whether the effect of PT has on participants is acute or sustained over time.
Acknowledgements
The authors thank the Core for Advanced MRI at Baylor College of Medicine, the Houston Playback Theatre company, and participants.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was supported by the International Playback Theatre Network, the McNair Medical Institute; the Veteran Health Administration (VHA5I01CX000994, VHA1I21RX002588); and the American Foundation for Suicide Prevention (SRG-2-125-14). This research was also partially supported by the Shirley and David Toomim Family Foundation and by Menninger Clinic. This material is the result of work supported with resources and the use of facilities at the Michael E. DeBakey VA Medical Center, Houston, Texas. These data included herein were collected through the use of facilities and resources at The Menninger Clinic, Houston, Texas USA. The contents do not represent the views of the U.S. Department of Veterans Affairs or the United States Government.
ORCID iDs
Peter K. Bolin https://orcid.org/0000-0002-2018-2070
Ramiro Salas https://orcid.org/0000-0002-1105-566X
Notes
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
The data sets generated during and/or analyzed during the current study are available from the corresponding author (Ramiro Salas) upon reasonable request.
References
- 1.Burkle FM., Jr. Acute-phase mental health consequences of disasters: implications for triage and emergency medical services. Ann Emerg Med. 1996; 28(2): 119–128. [DOI] [PubMed] [Google Scholar]
- 2.Kessler RC, Sonnega A, Bromet E, Hughes M, Nelson CB. Posttraumatic stress disorder in the national comorbidity survey. Arch Gen Psychiatry. 1995; 52(12): 1048–1060. [DOI] [PubMed] [Google Scholar]
- 3.Norris FH, Friedman MJ, Watson PJ, Byrne CM, Diaz E, Kaniasty K. 60,000 Disaster victims speak: part I. An empirical review of the empirical literature, 1981-2001. Psychiatry. 2002; 65(3): 207–239. [DOI] [PubMed] [Google Scholar]
- 4.Shultz JM, Forbes D. Psychological first aid: rapid proliferation and the search for evidence. Disaster Health. 2014; 2(1): 3–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.McFarlane AC, Papay P. Multiple diagnoses in posttraumatic stress disorder in the victims of a natural disaster. J Nerv Ment Dis. 1992; 180(8): 498–504. [DOI] [PubMed] [Google Scholar]
- 6.Galea S, Nandi A, Vlahov D. The epidemiology of post-traumatic stress disorder after disasters. Epidemiol Rev. 2005; 27: 78–91. [DOI] [PubMed] [Google Scholar]
- 7.Neria Y, Nandi A, Galea S. Post-traumatic stress disorder following disasters: a systematic review. Psychol Med. 2008; 38(4): 467–480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Acierno R, Ruggiero KJ, Kilpatrick DG.Resnick HS, Galea S. Risk and protective factors for psychopathology among older versus younger adults after the 2004 Florida hurricanes. Am J Geriatr Psychiatry. 2006; 14(12): 1051–1059. [DOI] [PubMed] [Google Scholar]
- 9.Amstadter AB, Koenen KC, Ruggiero KJ, et al. NPY moderates the relation between hurricane exposure and generalized anxiety disorder in an epidemiologic sample of hurricane-exposed adults. Depress Anxiety. 2010; 27(3): 270–275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Tracy M, Norris FH, Galea S. Differences in the determinants of posttraumatic stress disorder and depression after a mass traumatic event. Depress Anxiety. 2011; 28(8): 666–675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Galea S, Ahern J, Resnick H, et al. Psychological sequelae of the September 11 terrorist attacks in New York city. N Engl J Med. 2002; 346(13): 982–987. [DOI] [PubMed] [Google Scholar]
- 12.Mellman TA, Kulick-Bell R, Ashlock LE.Nolan B. Sleep events among veterans with combat-related posttraumatic stress disorder. Am J Psychiatry. 1995; 152(1): 110–115. [DOI] [PubMed] [Google Scholar]
- 13.Abad VC, Guilleminault C. Sleep and psychiatry. Dialogues Clin Neurosci. 2005; 7(4): 291–303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.White T. Subclinical psychiatric symptoms and the brain: what can developmental population neuroimaging bring to the table? J Am Acad Child Adolesc Psychiatry. 2015; 54(10): 797–798. [DOI] [PubMed] [Google Scholar]
- 15.Schwartz RM, Tuminello S, Kerath SM, Rios J, Lieberman-Cribbin W, Taioli E. Preliminary assessment of Hurricane Harvey exposures and mental health impact. Int J Environ Res Public Health. 2018; 15(5) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Storch EA, Shah A, Salloum A, et al. Psychiatric diagnoses and medications for Hurricane Harvey sheltered evacuees. Community Ment Health J. 2019; 55(7): 1099–1102. [DOI] [PubMed] [Google Scholar]
- 17.Chung KSY, Lee ESL, Tan JQ, et al. Effects of playback theatre on cognitive function and quality of life in older adults in Singapore: a preliminary study. Australas J Age. 2018; 37(1): E33–E36. [DOI] [PubMed] [Google Scholar]
- 18.Salas R, Steele K, Lin A, Loe C, Gauna L, Jafar-Nejad P. Playback theatre as a tool to enhance communication in medical education. Med Educ Online. 2013; 18: 22622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Smigelsky MA, Neimeyer RA. Performative retelling: healing community stories of loss through playback theatre. Death Stud. 2018; 42(1): 26–34. [DOI] [PubMed] [Google Scholar]
- 20.David Read Johnson RE, ed. Current Approaches in Drama Therapy. 2nd ed Springfield, IL: Charles C Thomas Publisher; 2009:540. [Google Scholar]
- 21.Moran G, Alon U. Playback theatre and recovery in mental health: preliminary evidence. Arts in Psychother. 2011; 38(5): 318–324. [Google Scholar]
- 22.Pennebaker JW. The effects of traumatic disclosure on physical and mental health: the values of writing and talking about upsetting events. Int J Emerg Ment Health. 1999; 1(1): 9–18. [PubMed] [Google Scholar]
- 23.Biswal B, Yetkin FZ, Haughton VM, Hyde JS. Functional connectivity in the motor cortex of resting human brain using echo-planar MRI. Magn Reson Med. 1995; 34(4): 537–541. [DOI] [PubMed] [Google Scholar]
- 24.Akiki TJ, Averill CL, Wrocklage KM, et al. Default mode network abnormalities in posttraumatic stress disorder: a novel network-restricted topology approach. Neuroimage. 2018; 176: 489–498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Li BJ, Friston K, Mody M, Wang HN, Lu HB, Hu DW. A brain network model for depression: from symptom understanding to disease intervention. CNS Neurosci Ther. 2018; 24(11): 1004–1019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Makovac E, Meeten F, Watson DR, et al. Alterations in amygdala-prefrontal functional connectivity account for excessive worry and autonomic dysregulation in generalized anxiety disorder. Biol Psychiatry. 2016; 80(10): 786–795. [DOI] [PubMed] [Google Scholar]
- 27.Pannekoek JN, Veer IM, van Tol M-J, et al. Resting-state functional connectivity abnormalities in limbic and salience networks in social anxiety disorder without comorbidity. Eur Neuropsychopharmacol. 2013; 23(3): 186–195. [DOI] [PubMed] [Google Scholar]
- 28.Kogler L, Müller VI, Werminghausen E, Eikhoff SB, Derntl B. Do I feel or do I know? Neuroimaging meta-analyses on the multiple facets of empathy. Cortex. 2020; 129: 341–355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hamilton M. The assessment of anxiety states by rating. Br J Med Psychol. 1959; 32(1): 50–55. [DOI] [PubMed] [Google Scholar]
- 30.Blevins CA, Witte TK, Weathers FW. Factor structure of the Cambridge depersonalization scale in trauma-exposed college students. J Trauma Dissociation. 2013; 14(3): 288–301. [DOI] [PubMed] [Google Scholar]
- 31.Rush AJ, Trivedi MH, Ibrahim HM, et al. The 16-Item quick inventory of depressive symptomatology (QIDS), clinician rating (QIDS-C), and self-report (QIDS-SR): a psychometric evaluation in patients with chronic major depression. Biol Psychiatry. 2003; 54(5): 573–583. [DOI] [PubMed] [Google Scholar]
- 32.Maier W, Buller R, Philipp M, Heuser I. The Hamilton anxiety scale: reliability, validity and sensitivity to change in anxiety and depressive disorders. J Affect Disord. 1988; 14(1): 61–68. [DOI] [PubMed] [Google Scholar]
- 33.Bruss GS, Gruenberg AM, Goldstein RD, Barber JP. Hamilton anxiety rating scale interview guide: joint interview and test-retest methods for interrater reliability. Psychiatry Res. 1994; 53(2): 191–202. [DOI] [PubMed] [Google Scholar]
- 34.Matza LS, Morlock R, Sexton C, Malley K, Feltner D. Identifying HAM-A cutoffs for mild, moderate, and severe generalized anxiety disorder. Int J Methods Psychiatr Res. 2010; 19(4): 223–232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Sveen J, Bondjers K, Willebrand M. Psychometric properties of the PTSD checklist for DSM-5: a pilot study. Eur J Psychotraumatol. 2016; 7(1): 30165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Kroenke K, Baye F, Lourens SG. Comparative responsiveness and minimally important difference of common anxiety measures. Med Care. 2019; 57(11): 890–897. [DOI] [PubMed] [Google Scholar]
- 37.Tomasi DG, Shokri-Kojori E, Volkow ND. Temporal evolution of brain functional connectivity metrics: could 7 min of rest be enough? Cereb Cortex. 2017; 27(8): 4153–4165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Whitfield-Gabrieli S, Nieto-Castanon A. Conn: a functional connectivity toolbox for correlated and anticorrelated brain networks. Brain Connect. 2012; 2(3): 125–141. [DOI] [PubMed] [Google Scholar]
- 39.Akiki TJ, Averill CL, Abdallah CG. A network-based neurobiological model of PTSD: Evidence from structural and functional neuroimaging studies. Curr Psychiatry Rep. 2017; 19(11): 81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Kaiser RH, Andrews-Hanna JR, Wager TD, Pizzagalli DA. Large-scale network dysfunction in major depressive disorder: a meta-analysis of resting-state functional connectivity. JAMA Psychiatry. 2015; 72(6): 603–611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Yang Z, Gu S, Honnorat N, et al. Network changes associated with transdiagnostic depressive symptom improvement following cognitive behavioral therapy in MDD and PTSD. Mol Psychiatry. 2018; 23(12): 2314–2323. [DOI] [PubMed] [Google Scholar]
- 42.Armstrong RA. When to use the Bonferroni correction. Ophthal Physiol Opt. 2014; 34(5): 502–508. [DOI] [PubMed] [Google Scholar]
- 43.Wigren J. Narrative completion in the treatment of trauma. Psychotherapy: Theory Res Pract Train. 1994; 31(3): 415–423. [Google Scholar]
- 44.Wilson RM, Leary S, Mitchell M, Ritchie D. Military veterans sharing first‐person stories of war and homecoming: a pathway to social engagement, personal healing, and public understanding of veterans’ issues. Smith Coll Stud Soc Work. 2009; 79(3–4): 392–423. [Google Scholar]
- 45.Turner BO, Paul EJ, Miller MB, Barbey AK. Small sample sizes reduce the replicability of task-based fMRI studies. Commun Biol. 2018; 1: 62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Brunoni AR, Lopes M, Kaptchuk TJ, Fregni F. Placebo response of non-pharmacological and pharmacological trials in major depression: a systematic review and meta-analysis. PLoS One. 2009; 4(3): e4824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Wilson JP, Thomas RB. Empathy in the treatment of trauma and PTSD. In: Brunner-Routledge Psychosocial Stress Series New York, NY: Brunner-Routledge; 2004.
- 48.Liz Hamel BW, Brodie M, Sim S-C, Wu B, Marks E. One Year after the Storm: Texas Gulf Coast Residents’ Views and Experiences With Hurricane Harvey Recovery. Washington, DC: The Kaiser Family Foundation/Episcopal Health Foundation Harvey Anniversary Survey; 2018. [Google Scholar]