Abstract
A 49-year-old male patient with residual cleft palate and missing pre-maxilla presented with an ill-fitting and unaesthetic maxillary denture. The posterior teeth were periodontally sound but crowded and had defective restorations and secondary caries. We restored the bilateral maxillary canines and first premolars with conical telescopic crowns having magnetic keepers. A metal-reinforced acrylic overdenture with magnetic attachments corresponding to the keepers of the telescopic crowns was fabricated. The telescopic crowns provided a single path of insertion, retention and stability to the prosthesis. The magnetic attachments provided additional retention and self-centring properties. The prosthesis effectively sealed the oronasal communication and enhanced the function, aesthetics and oral hygiene. The 6-month and 1-year follow-ups revealed that the patient was delighted, and the prosthesis provided excellent obturation and function. Periodic follow-up, maintenance, patient education and meticulous oral hygiene are vital for long-term success of such prostheses.
Keywords: dentistry and oral medicine, mouth
Background
The oral rehabilitation of cleft palate is primarily accomplished with surgical intervention, commonly performed in the patient’s early years by a maxillofacial or plastic surgeon. Nevertheless, the treatment is not complete without an interdisciplinary approach involving a paedodontist, orthodontist, prosthodontist, psychologist and speech therapist at appropriate times. Palatoplasty may have tissue scarcity, leading to excessive scar formation, palatal fistula and velopharyngeal dysfunction, mainly when the surgery is performed at a later age.1–5 Moreover, any remnant cleft after the surgical intervention may lead to impaired speech, mastication and deglutination, and could need prosthodontic intervention such as obturators.6 7
Prosthodontic rehabilitation of the cleft palate has several challenges, such as compromised retention and stability due to partial anodontia, crowding, unfavourable tilting, irregular residual alveolar ridge, scaring and so on. An implant-supported prosthesis is a good option but is often limited due to deficient bone and financial reasons. The prosthesis choice also depends on the deficient surrounding tissues, intermaxillary relationship, oral hygiene and general health of the patient. Magnetic attachments have several advantages in being user-friendly, economical, stress breaking, low maintenance and facilitating freedom of lateral movement and self-centring of the prosthesis.8 They are frequently made from neodymium-iron-boron magnets.
The double crown system, interchangeably called telescopic dentures,9 attain additional retention by friction and provide better support and stability due to total coverage of the tooth than a conventional removable partial denture. Telescopic dentures are easy and inexpensive to fabricate.10 Previously, telescopic crowns were designed with parallel sidewalls. Nowadays, conical telescopic crowns having tapered axial walls with convergence angles ranging from 2º–6º are more frequently used.9 10 They present fewer fabrication challenges and produce less oblique forces on the abutments.11 12 Magnotelescopic crown (MT crown) is the term used to describe a telescopic crown modified with magnetic attachment.13 Other modifications of the double crown system comprise the addition of retentive elements and resilient materials.9 10
The present report advocates prosthodontic intervention in non-operated/residual cleft palate with periodontally sound natural teeth using the MT overdenture. This kind of prosthesis may concurrently improve the retention, stability and aesthetics within a reasonable cost.
Case presentation
The patient provided written informed consent to publish the case report in a scientific journal and conferences with an agreement to display the lower one-third of the face and intraoral photographs.
A male patient aged 49 years visited the dental clinic at the College of Dentistry with an ill-fitting and unaesthetic upper denture. The denture replaced the missing anterior teeth and obturated the oronasal communication in the pre-maxilla (figure 1A, B). The phonetics and deglutination were compromised. The denture’s acrylic teeth were severely attrited, the polished surface was discoloured and the tissue surface showed biofilm accumulation. The old denture is devoid of posterior teeth replacement. The denture base was covering the natural teeth on the left side (figure 1C–E). The intercuspal position displayed a severe crossbite with the lower natural teeth anteriorly and posteriorly (figure 1F); there was an interocclusal space of 4 mm at the incisor region at centric relation position (figure 1G). The upper lip support with the old prosthesis was poor. The patient wanted better retention, aesthetics and function within his financial constraints. Intraoral examination revealed repaired cleft lip, missing pre-maxilla, direct communication with the nasal cavity (Aramany’s class IV defect), cluster-type crowded maxillary posterior teeth, anterior and posterior crossbite, defective amalgam restoration in the upper right first and second molars, dental caries in upper right canine, no mobility and periodontal pockets, adequate oral hygiene, generalised mild marginal gingivitis and acceptable attached gingival width (figure 1A–H).
Figure 1.
Pre-treatment images. (A) Intraoral view displaying cleft palate in the pre-maxilla and overcrowding. (B) Intraoral view revealing posterior crossbite of natural teeth. (C–E) Old prosthesis exhibiting biofilm, discoloration and attrition. (F) The severe crossbite of the old prostheses. (G) Interocclusal space at centric relation position. (H) Orthopantograph.
Treatment
Primary impressions were recorded using alginate. Diagnostic mandibular movement and condylar positional analysis were performed using an electronic face bow (ARCUSdigma, KaVo Kerr, Biberach, Germany), and the intermaxillary relation was recorded. The casts were mounted on a fully adjustable articulator (PROTARdigma, KaVo Kerr) based on the setting dictated by the ARCUSdigma. After studying the intermaxillary relations and possible labial support for the prosthesis, the treatment sequence was planned (table 1).
Table 1.
Treatment plan
| Phase | Procedure |
| I | Diagnostic evaluation and treatment planning Patient education and oral hygiene instruction |
| II | Provisional restoration with 13 and 17 Pulp extirpation and Ca(OH)₂ dressing with 16 Scaling and root planning Patient education and oral hygiene instruction |
| III | Composite restorations with 13 and 17 Root canal treatment with 16 Gingivectomy to resolve the pseudopockets with 26 and 27 Restoration of 13, 14, 23 and 24 with conical telescopic crowns with magnetic keepers Patient education and oral hygiene instruction |
| IV | Fabrication and placement of metal-reinforced acrylic overdenture with magnetic attachments and obturator |
| V | Maintenance with frequent recall visits, every 4–6 months Reinforcement of patient education and motivation |
Bilateral maxillary canines and premolars were prepared for crowns. The gingiva was retracted using a #00 cord (Ultrapak E, Ultradent Products, Utah, USA), and an impression was recorded using polyvinylsiloxane (Aquasil, Dentsply International, USA). A 0.5 mm magnetic keeper attachment (Magfit DX400, Aichi Steel, Aichi, Japan) was attached to the conical crown’s occlusal surface using the cast-bonded keeper method.14 The crowns were milled with a minimal taper on a surveyor to enable a single insertion path. The conical walls of the crowns provided retention to the prosthesis by wedging action and friction.9 10
Cementation of the telescopic crowns was performed using self-adhesive resin cement (RelyX Unicem, 3M ESPE clicker) (figure 2A–D). A functional impression was recorded using polyether in a custom tray (Impregum PentaSoft Quick Step Medium Body, 3M Center, St. Paul, Minnesota, USA). Since the defect was small, treatment with an obturator without a bulb was planned. A cast metal framework and an acrylic overdenture were fabricated. The overdenture was tried in the patient’s mouth, and a cavity was created on the denture’s tissue surface for the magnetic assembly. The cavity was filled with a reline resin (TRIAD DuaLine Reline Material, Dentsply Sirona) and placed in the patient’s mouth while the magnet (Magfit DX400) was set on the corresponding keeper. The patient was instructed to occlude for a few minutes. After the material was set, we adjusted the occlusion and evaluated the patient for swallowing and phonetic functions.
Figure 2.
Treatment images. (A) Intra-oral view of the try-in denture in occlusion. (B) Intra-oral view displaying tooth preparation. (C) Cast showing telescopic crown. (D) Intra-oral view after telescopic crown cementation.
Outcome and follow-up
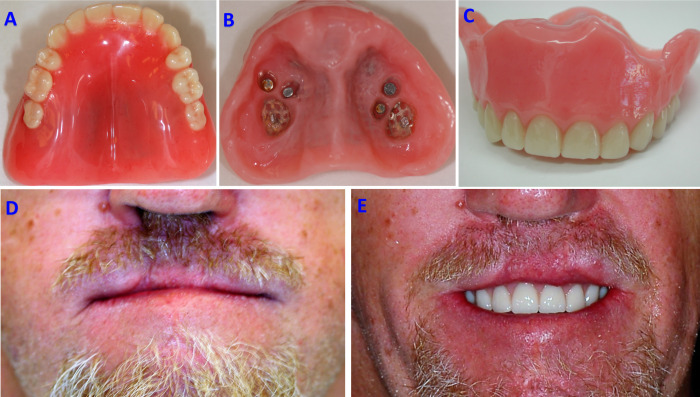
There was a significant improvement in the aesthetics of the patient. The smile line revealed anterior teeth up to the cervical margins, and some part of the denture base was visible due to a residual cleft lip defect. The dentures were very retentive and stable, following a single path of insertion and removal. There were posterior bilateral contacts in the crossbite and a slight anterior open bite. The denture obturated the residual cleft effectively, and the patient displayed reasonable phonetics. The patient was overjoyed with the aesthetic outcome (figure 3A–E).
Figure 3.
Post-treatment images. (A) The polished surface of the overdenture. (B) The tissue surface of the overdenture with magnetic attachments. (C) Labial view of the overdenture displaying aesthetic teeth arrangement. (D) Over-closure and unsupported lips evident in an extra-oral view of the patient, without denture. (E) Extra-oral view, with the mandible at rest position, demonstrating the aesthetic enhancement of the overdenture.
We demonstrated the removal and insertion of the prosthesis and allowed the patient to practice. Standard partial denture delivery instructions were given orally and in written format. Oral hygiene instructions regarding the use of a toothbrush, single-tufted toothbrush, mouthwash and dental floss were emphasised.
Immediate follow-up evaluation was done 2 and 7 days post insertion. Apart from reviewing patient complaints, evaluation for retention and oronasal seal, patient satisfaction survey were performed. Subsequent follow-ups were performed after 6 months and 1 year, repeating all the evaluations mentioned above. There were no adverse events, except for mild gingivitis. We performed oral prophylaxis and fluoride application during both the appointments. The importance of oral hygiene and periodic follow-ups was reinforced.
Discussion
The retention and stability of a removable prosthesis are affected in patients with a cleft palate. Dental implants may not always be feasible due to tissue deficiency or the financial condition of the patients. We used an overdenture with MT attachment to replace missing anterior teeth in a patient with a pre-maxillary cleft in the current report. The prosthesis evaluation and the patient satisfaction survey suggest that the technique effectively enhanced retention, stability, support and aesthetics of the prosthesis.
One of the demerits of telescopic overdenture compared with a conventional removable partial denture is that the tooth structure is sacrificed for the crowns. However, in this case, the remaining teeth were overcrowded in clusters, and some had caries, defective restorations and generalised marginal gingivitis. Truncated, inverted, cone-shaped full-coverage crown could improve the hygiene and reduce the adverse effects of cluster crowding. Additionally, conical crowns can lower the lateral forces on the abutments and simplify the fabrication; however, they are not as retentive as cylindrical crowns.9 10 In this case, there is a possibility of long-term retention loss from the conical crowns due to frictional abrasion and an abnormal wear pattern of acrylic, which replaced the secondary crown.15 16 Nonetheless, relining can rectify such retention deficit. Another demerit, in this case, is the possibility of food and biofilm accumulation under the overdenture and around the retained teeth due to unavoidable spaces between the denture base and tooth surfaces, increasing the risk of periodontitis and secondary caries.16 A study reported periodontitis, caries and fracture as the most common cause of abutment.17 Meticulous oral hygiene by the patient and periodic follow-ups are required to prevent such adverse effects.
Patients with cleft palate suffer from decreased size of the maxilla compared with normal individuals.18 Our patient had a severe crossbite anteriorly and posteriorly in his old denture. The post-treatment occlusion continued to be a posterior crossbite but to a reduced extent. The crossbite arrangement is obligatory in narrow maxilla cases for adequate stability of the denture.19 20 Anteriorly, the teeth were arranged to produce an open bite to reduce the denture base’s extent of visibility due to the deficient lip. The anterior teeth arrangement was made according to the specific requirement of the patient. We covered the posterior teeth from both sides; such coverage would usually increase the occlusal vertical dimension unless the opposing teeth were modified. However, in the current case, the patient’s old denture covered the left posterior teeth (figure 1D, E). While the right posteriors in the old dentures had direct occlusal contact, we performed an endodontic treatment on the right first molar due to necrotic pulp and reduced the occlusal surface to enable the coverage (figure 2C). Moreover, the patient’s old dentures had a deficiency in the occlusal vertical dimension (figure 1G).
In the current study, we used magnets (Magfit DX400), and each magnet produced a magnetic force of 400 gf. Though several other systems can produce superior magnetic forces, they usually have a higher thickness. This system has a keeper thickness of just 0.5 mm and a total magnetic assembly thickness of 1 mm, and it is particularly suitable for use on vital tooth abutment as it conserves the occlusal tooth surface. Moreover, having four magnets and telescopic crowns provided the right amount of retention, stability and support to the prosthesis. A conventional magnet is prone to corrosion in a moist environment;21 however, Magfit DX400 is protected from corrosion by an integral stainless steel hermetic casing. An earlier study reported the initial magnetic forces of Magfit DX400 to be slightly higher than the manufacturer’s claims (mean magnetic force=420 gf), and a reduction in the magnetic forces and rate of detachment in 6–9 years of clinical use was around 21% and 16%, respectively.22 In another study, a survival rate of 93.8% was reported for telescopic crowns after 7 years, with the most probable type of failure to be crown dislodgment.15
During the 6-month and 1-year follow-up appointments, the prosthesis and the supporting oral structures were found to be in excellent condition. There were no signs of failures in the crowns, abutments, denture base or magnets. The survival rate of the prosthesis can be predicted to be fair, considering the previous reports.15 22 23 To summarise, the telescopic magnetic overdenture is an effective method to rehabilitate patients with a cleft palate. However, 4–6 months of periodic follow-up to evaluate caries and periodontal health, oral prophylaxis, topical fluoride application and reinforcement of the need for meticulous oral hygiene is required.
Patient's perspective.
I was unhappy with my old dentures, which I was using for 4 years. I had difficulty smiling in public and was covering my face most of the time. The dentures were also loose. I was not aware of hygiene measures. After attending this clinic, I realised that I had several problems with the existing teeth. The doctor explained to me the treatment options and I choose to take a cost-effective treatment. Though multiple appointments bothered me a bit, I was overjoyed with the final aesthetic result. I am exercising good oral hygiene by means of regular tooth brush, interdental brush and mouth wash. I am attending the follow-up appointments punctually and am very positive about the durability of the dentures.
Learning points.
Tooth-supported, telescopic, magnetic overdentures can be a cost-effective treatment modality in patients with residual cleft palate.
The proposed technique could fulfil the patients' expectations regarding retention, stability, function and aesthetics.
Periodic follow-ups and maintenance appointments are critical parts of rehabilitation for long-term success.
Footnotes
Contributors: The authors, MAA and SS, equally contributed in the conception and design, acquisition of data, analysis and interpretation of data, and drafting the article and revising it critically for important intellectual content. We approve the submitted version and agree to be accountable for the article and ensure that all questions regarding the accuracy or integrity of the article are investigated and resolved.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Patient consent for publication: Obtained.
Ethics approval: The Scientific Research Committee of the College of Dentistry, King Khalid University, approved the present reporting (SRC/ETH/2018-19/090).
Provenance and peer review: Not commissioned; externally peer-reviewed.
References
- 1.Rossell-Perry P, Caceres Nano E, Gavino-Gutierrez AM. Association between palatal index and cleft palate repair outcomes in patients with complete unilateral cleft lip and palate. JAMA Facial Plast Surg 2014;16:206–10. 10.1001/jamafacial.2013.2537 [DOI] [PubMed] [Google Scholar]
- 2.de Blacam C, Smith S, Orr D. Surgery for velopharyngeal dysfunction: a systematic review of interventions and outcomes. Cleft Palate Craniofac J 2018;55:405–22. 10.1177/1055665617735102 [DOI] [PubMed] [Google Scholar]
- 3.Reisberg DJ. Dental and prosthodontic care for patients with cleft or craniofacial conditions. Cleft Palate Craniofac J 2000;37:534–7. 10.1597/1545-1569_2000_037_0534_dapcfp_2.0.co_2 [DOI] [PubMed] [Google Scholar]
- 4.Motegi K, Matsuo T, Ito S, et al. Treatment of restricted jaw movement due to scars after palatoplasty. Bull Tokyo Med Dent Univ 1975;22:161–3. [PubMed] [Google Scholar]
- 5.Sullivan SR, Marrinan EM, LaBrie RA, et al. Palatoplasty outcomes in nonsyndromic patients with cleft palate: a 29-year assessment of one surgeon's experience. J Craniofac Surg 2009;20(Suppl 1):612–6. 10.1097/SCS.0b013e318192801b [DOI] [PubMed] [Google Scholar]
- 6.Laine J, Vähätalo K, Peltola J, et al. Rehabilitation of patients with congenital unrepaired cleft palate defects using free iliac crest bone grafts and dental implants. Int J Oral Maxillofac Implants 2002;17:573–80. [PubMed] [Google Scholar]
- 7.Pinto JHN, da Silva Dalben G, Pegoraro-Krook MI. Speech intelligibility of patients with cleft lip and palate after placement of speech prosthesis. Cleft Palate Craniofac J 2007;44:635–41. 10.1597/06-061.1 [DOI] [PubMed] [Google Scholar]
- 8.Gillings BR, Samant A. Overdentures with magnetic attachments. Dent Clin North Am 1990;34:683–709. [PubMed] [Google Scholar]
- 9.Hakkoum MA, Wazir G. Telescopic denture. Open Dent J 2018;12:246–54. 10.2174/1874210601812010246 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Arnold C, Hey J, Setz JM, et al. Retention force of removable partial dentures with different double Crowns. Clin Oral Investig 2018;22:1641–9. 10.1007/s00784-017-2224-x [DOI] [PubMed] [Google Scholar]
- 11.Widbom T, Löfquist L, Widbom C, et al. Tooth-supported telescopic crown-retained dentures: an up to 9-year retrospective clinical follow-up study. Int J Prosthodont 2004;17:29–34. [PubMed] [Google Scholar]
- 12.Güngör MA, Artunç C, Sonugelen M. Parameters affecting retentive force of Conus Crowns. J Oral Rehabil 2004;31:271–7. 10.1111/j.1365-2842.2004.01036.x [DOI] [PubMed] [Google Scholar]
- 13.Tanaka Y, Nakamura Y, Hoshiai K. General remarks concerning magnetic attachments in dentistry. Proc Japan Acad Ser B Phys Bio Sci 2002;78:97–105. 10.2183/pjab.78.97 [DOI] [Google Scholar]
- 14.Anupam P, Anandakrishna GN, Vibha S, et al. Mandibular Overdenture retained by magnetic assembly: a clinical tip. J Indian Prosthodont Soc 2014;14:328–33. 10.1007/s13191-012-0194-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Schwindling FS, Dittmann B, Rammelsberg P. Double-crown-retained removable dental prostheses: a retrospective study of survival and complications. J Prosthet Dent 2014;112:488–93. 10.1016/j.prosdent.2014.02.017 [DOI] [PubMed] [Google Scholar]
- 16.de Albuquerque RF, Fromentin O, Lassauzay C, et al. Patient satisfaction versus retention of implant overdentures with two attachment systems: a randomized trial. Clin Implant Dent Relat Res 2019;21:21–31. 10.1111/cid.12675 [DOI] [PubMed] [Google Scholar]
- 17.Fenlon MR, disease P. Periodontal disease, periapical lesions and caries were, in that order, the causes of overdenture abutment loss. J Evid Based Dent Pract 2005;5:94–5. 10.1016/j.jebdp.2005.04.010 [DOI] [PubMed] [Google Scholar]
- 18.Friede H, Persson EC, Lilja J, et al. Maxillary dental arch and occlusion in patients with repaired clefts of the secondary palate. Influence of push back palatal surgery. Scand J Plast Reconstr Surg Hand Surg 1993;27:297–305. [PubMed] [Google Scholar]
- 19.Hardy IR. The developments in the occlusal patterns of artificial teeth. J Prosthet Dent 1951;1:14–28. 10.1016/0022-3913(51)90075-3 [DOI] [PubMed] [Google Scholar]
- 20.Sanghvi SJ, Bhatt NA, Bhargava K. An evaluation of cross-bite ridge relationships. A study of articulated jaw records of 150 edentulous patients. J Prosthet Dent 1981;45:24–9. 10.1016/0022-3913(81)90007-X [DOI] [PubMed] [Google Scholar]
- 21.Okuno O, Ishikawa S, Imuro FT, et al. Development of sealed cup yoke type dental magnetic attachment. Dent Mater J 1991;10:172–84. 10.4012/dmj.10.172 [DOI] [PubMed] [Google Scholar]
- 22.Leem H-W, Cho I-H, Lee J-H, et al. A study on the changes in attractive force of magnetic attachments for overdenture. J Adv Prosthodont 2016;8:9–15. 10.4047/jap.2016.8.1.9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kern J-S, Hanisch O, Hammächer C, et al. Telescopic Crowns on implants and teeth: evaluation of a clinical study after 8 to 12 years. Int J Oral Maxillofac Implants 2019;34:977–86. 10.11607/jomi.7204 [DOI] [PubMed] [Google Scholar]