Abstract
Background
Lower blepharoplasty has been used for rejuvenating lower eyelids, and diverse modifications have been used to treat conjunct deformities at the tear trough/lid-cheek junction. Strategies for recontouring prominent tear trough/lid-cheek junctions, including orbital fat manipulation, have been reported with good results in the literature. Micro-autologous fat transplantation (MAFT) is a previously unevaluated, potentially advantageous approach to blending the prominent tear trough/lid-cheek junction.
Objectives
We determined the long-term results after 3-step transcutaneous lower blepharoplasty with MAFT for patients with aging eyelids and prominent tear trough/lid-cheek junctions.
Methods
We evaluated 205 patients with aging lower eyelids who underwent transcutaneous lower blepharoplasty with MAFT between October 2010 and September 2016. The 3-step procedure involved a subciliary elliptical skin excision, resection of 3 orbital fat compartments, and MAFT for the tear trough/lid-cheek junction employing a MAFT-GUN under intravenous anesthesia.
Results
The mean patient age was 52 years (range, 34-78 years). The mean operating time was 61 minutes. The mean fat volumes delivered to the tear trough/lid-cheek junctions were 2.80 mL and 2.76 mL for the left and right sides, respectively. The average weights of the 3 resected orbital fat compartments were 0.58 g for the left side and 0.56 g for the right side. Patients showed significant improvement and maintenance at an average follow-up of 60.2 months (range, 18-90 months).
Conclusions
Three-step transcutaneous lower blepharoplasty with MAFT is an effective, reliable, and promising method with high patient satisfaction and minimal risk of complications. Long-term results demonstrated its utility for aging lower eyelid treatment.
Level of Evidence: 4

Restoration of periorbital areas to provide a more youthful and reinvigorated appearance accounts for the greatest number of aesthetic facial surgeries performed for humans. Throughout its evolution, transcutaneous lower blepharoplasty was intended to provide superior, long-lasting results and eliminate complications by repositioning excess or malpositioned orbital fat, managing excess lower eyelid skin, and recontouring the tear trough (nasojugal groove) and lid-cheek junction (palpebromalar groove).
In 1951, Costañares detailed the anatomy of eyelid fat compartments and precisely described the technique known as modern blepharoplasty.1 The first published report of the skin muscle flap in lower blepharoplasty was by Reidy in 1960,2 and several other investigators have discussed their experiences utilizing this technique.3-6 In the 1970 and 1980s, Furnas recognized the contribution of redundant orbicularis oculi (OO) muscles and focused on the resection of OO muscles to restore a more youthful appearance.7 However, Loeb illustrated that fat preservation and translocation rather than resection were effective for blending the transition between the lower eyelid and cheek.8 Hamra championed fat preservation and expanded the concept to complete release of the arcus marginalis with fat translocation to soften the lid-cheek junction.9 Meanwhile, autogenous “fat pearls” harvested from excess herniated fat pads have been utilized since the 1980s, with good results reported when employed as an adjunct to lower eyelid blepharoplasty.8,10,11 Alternatively, free fat or dermis-fat grafts may be harvested from other body sites and have special application in the correction of the patient with contour deficits as a result of prior blepharoplasty surgery.12 Moreover, autologous fat injections or fillers to restore volume to the periorbita may be applicable in more difficult cases that are not amenable to traditional eyelid procedures because of soft tissue atrophy.13,14
The senior author (T.L.) has developed a simple 3-step procedure for transcutaneous lower blepharoplasty that is intended to manage excess lower eyelid skin and protruding orbital fat and to blend/recontour the tear trough and lid-cheek junction employing micro-autologous fat transplantation (MAFT), which has been advocated since 2007.15-22 This study sought to determine the long-term results of this simple 3-step procedure, transcutaneous lower blepharoplasty with MAFT, for patients with aging lower eyelids and prominent tear trough and lid-cheek junctions.
METHODS
Patient Demographics
Between October 2010 and September 2016, 205 patients (183 women and 22 men) underwent transcutaneous lower blepharoplasty with MAFT to treat aging lower eyelids (Figure 1) and recontour the tear trough and lid-cheek junctions. Inclusion criteria were age 30 to 70 years, dermatochalasis of the lower eyelids, protruding orbital fat, and prominence of the tear trough/lid-cheek junction. Exclusion criteria for patient selection comprised a history of lower eyelid surgery, infra-orbital trauma, and filler injections. While dealing with aging lower eyelids with dermatochalasis, excision of the subciliary skin was indispensable. In this series, we retrospectively analyzed patients who had lower eyelid skin redundancy with baggy eye and received transcutaneous lower blepharoplasty to improve their aging lower eyelid appearance. However, the authors performed transconjunctival lower blepharoplasty in another group of patients who had baggy eye without skin redundancy (or minimal redundancy). They are excluded from this study because surgical procedures are different. Therefore, we recruited only patients who received transcutaneous lower blepharoplasty in this study. Regular follow-up evaluations were conducted at an outpatient clinic at 1 month, 3 months, and 6 months (or longer when possible) after surgery. The cosmetic results at last visit were evaluated using the 5-point Likert scale (1, very unsatisfied; 2, unsatisfied; 3, neutral; 4, satisfied; 5, very satisfied) with 3 items: improvement of baggy eyes appearance, well contouring of tear trough deformity/lid-cheek junction, and skin revitalization. These studies were approved by the Institutional Review Board-II of Kaohsiung Medical University in Taiwan (KMUHIRB-E(II)-20180150) and are in accordance with the Declaration of Helsinki. All patients provided signed consent.
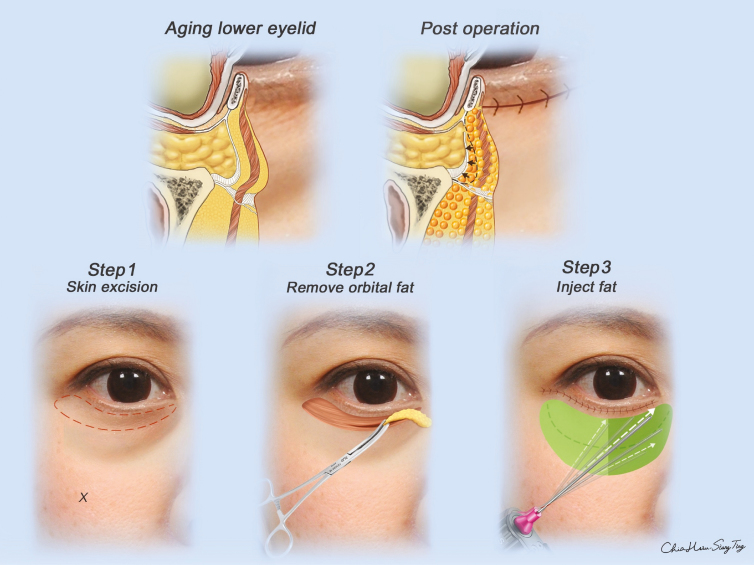
Figure 1.
The 3 simple steps of transcutaneous lower blepharoplasty with micro-autologous fat transplantation for treatment of the aging eyelid. Upper left: Sagittal section view of the aging lower eyelid shows skin dermatochalasis, bulging/prolapsed orbital fat, tear trough/lid-cheek junction depression, and sagging/weakening of the tear trough/orbicularis-retaining ligaments. Step 1: The planned skin excision is subciliary with lateral extension (lower left). The X point is the insertion site of the cannula for micro-autologous fat transplantation. Step 2: Three orbital fat compartments (medial, middle, and lateral parts) are resected appropriately (lower middle). Step 3: The micro-autologous fat transplantation technique is performed with a MAFT-GUN through insertion in the mid-cheek (lower right). Sagittal section view shows the main achievements after steps 1 to 3 (upper right). The skin is tightened after suturing, the bulging/prolapsed orbital fat is drawn back into the orbital septum after removal, multilayers are recontoured at the tear trough/lid-cheek junction, and the tear trough/orbicularis-retaining ligaments are reinforced by the micro-autologous fat transplantation technique.
Preoperative Planning and Photography
Patients underwent standard preoperative procedures and photography. Other basic data, including the weight of the resected medial and middle/lateral orbital fat compartments and the total volume of fat grafting used for recontouring the tear trough and lid-cheek junction, were recorded for the bilateral lower eyelids. Surgical planning for the MAFT area was performed with the patient in a standing position and according to the recipient areas outlined in Figure 1.
Anesthesiology and Transcutaneous Lower Blepharoplasty
Patients were under total intravenous anesthesia during the entire procedure. Approximately 0.5 mL of a local anesthetic solution comprising 2% Xylocaine with 1:1000 Epinephrine was subcutaneously infiltrated in the area of the planned skin excision. After 5 to 10 minutes, an elliptical strip of the skin was excised (or a strip inclusive of the tiny underlying OO muscle when indicated) (Figure 1) with meticulous attention to the achievement of hemostasis. Then, through a limited 10- to 15-mm slit achieved by muscle splitting, retro-OO muscle dissection was performed to conservatively expose the orbital septum. The orbital septum was opened and the medial fat compartment was approached and resected appropriately. Next, the middle and lateral compartments were resected similarly with meticulous attention to hemostasis (Figure 1). Attention was given to the lower eyelid middle lamina without further exploration or management. Neither dissection of the arcus marginalis nor release of the tear trough ligament (TTL)/orbicularis-retaining ligament (ORL) was performed. The procedure was completed and the skin was closed.
Micro-Autologous Fat Transplantation Procedure
The MAFT15-21 technique was performed after lower blepharoplasty. Briefly, the lipoaspirate was harvested mostly from the lower abdomen (or thigh) area after preinfiltration with a tumescent solution. Appropriate local anesthesia was injected at the insertion site for each patient. In accordance with the structural fat grafting technique proposed by Coleman, the extracted lipoaspirate was processed and purified using standard centrifugation at 3000 rpm (approximately 1200 × g) for 3 minutes.23 After centrifugation, the purified fat was transferred to a 1-mL syringe and then loaded in a MAFT-GUN (Dermato Plastica Beauty Co., Ltd., Kaohsiung, Taiwan) (Figure 2) (United States Patent US 7,632,251 B2, US 8,523,825 B2.). The volume of the fat parcel (each aliquot) for a trigger injection was set by adjusting the 6-grade dial to a setting of 240, which corresponded to 1/240 mL (0.0042 mL). The fat parcels were meticulously transplanted in 3 layers (deep, middle, and superficial layers) (Figure 1) to the tear trough and lid-cheek junction. The maneuver to transplant the tiny fat parcels is visually demonstrated in the Supplemental Digital Content (Videos 1 and 2, available online at www.aestheticsurgeryjournal.com). Written instructions regarding how to perform the MAFT procedure are provided here.
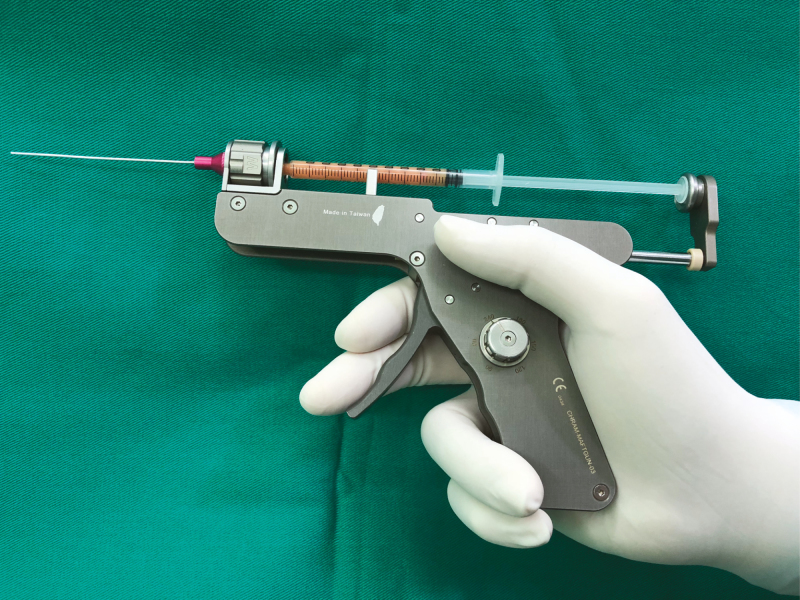
Figure 2.
The purified fat is transferred to a 1-mL syringe and then loaded in a MAFT-GUN (Dermato Plastica Beauty Co., Ltd., Kaohsiung, Taiwan). The volume of a single delivered fat parcel is set at 1/240 mL (0.0042 mL) by turning the 6-graded volume dial to 240.
Micro-Autologous Fat Transplantation Maneuver Technique: Fat Parcels in the Tear Trough
Using a number 11 blade, a 2- to 3-mm incision was made in the mid-cheek region (Figure 1). An 18-G, blunt-tip, side-hole injection cannula was vertically inserted through the incision until the periosteum (point near the junction of the maxillary and zygomatic bones) was reached. Then, the cannula was slanted and manipulated until it reached the top of the maxilla supra-periosteally (on top of the periosteum) in the medial canthal area. The 6-grade volume knob of the MAFT-GUN was turned to 240 to inject a volume of 1/240 mL per parcel per pull of the trigger. For recontouring the tear trough, fat parcels were first placed in the deep layer on top of the periosteum of the maxilla in a fan shape (Video 2). Nearly 25% of the total fat volume injection in the tear trough could be transplanted in this deep layer. After finishing the deep layer, the cannula was tilted horizontally and the fat was injected into the middle layer between the OO muscle and the periosteum. Another 50% of fat grafting was transplanted in this space. Finally, in the superficial layer, which is represented by the thin layer between the dermis and the OO muscle, the injection should be precisely performed with more cannula tilting. A bleached appearance was visible on the skin with the horizontal tilting of the cannula tip. This maneuver interrupted the adhesion of the OO muscle to the skin dermis, allowing fat parcels to be placed more superficially (ie, just under the dermis). In this layer, the remaining 25% of the total injection volume could be delivered. In the 3 layers of the tear trough area, repeat passing of the blunt injection cannula through the TTL made it seem like many fenestrated windows were made in the TTL. Therefore, the tiny fat parcels (1/240 mL per parcel) were transplanted to surround the TTL.
Micro-Autologous Fat Transplantation Maneuver Technique: Fat Parcels in the Lid-Cheek Junction
Through the same insertion site, transplantation using similar maneuvers to recontour the lid-cheek junction was subsequently performed (Figure 1; Video 2). The distribution ratio of fat volumes in the 3 layers was the same as in the tear trough area.
The amount of fat grafting depends on the accommodating tissues volume (recipient volume of tissue in lower eyelid area includes tear trough and lid-cheek junction areas) of an individual patient. The grafting volume is roughly set at the base of 1.5 mL for each tear trough and lid-cheek junction at preoperative planning. The variable factors include individual deepening of tear trough/lid-cheek junction, laxity of skin, bony structure, and so on. All the factors play an important role in adjusting the volume that is finally transplanted. Basically, the ratios of transplanted fat volume in deep layer (supra-periosteum), middle layer (between OO muscle and periosteum), and superficial layer (between skin dermis and OO muscle) were grossly 25%:50%:25%. However, a maneuver of finger palpation (Video 2) to detect any unevenness or irregularity will indicate the necessity of further minor adjustment of fat volume. Normally, the technique of MAFT wound not emphasize on overcorrection. A fullness sensation with relative skin tightness (no delay of capillary refilling time) was also an indicator for final determination of volume.
A sensation of encountering denser tissue while advancing the injection cannula through the fenestrations of the ORL ensured that even and precise transplantation of fat parcels was performed accordingly. Further use of MAFT for the treatment of the crow’s feet area might be considered for improving the lateral canthal depression or wrinkles of some patients. At the end of the procedure, the insertion site was sutured with one 6-0 nylon stitch.
Post-Micro-Autologous Fat Transplantation Management
Regular postoperative care, including the administration of oral antibiotics and nonsteroidal anti-inflammatory drugs, was performed routinely for 3 days after the procedure. Immediately after surgery, the application of an ice pack for 30 minutes was suggested. No other management of the surgical field was necessary. Gentle lymphatic drain massage was suggested 7 days after surgery to relieve swelling.
RESULTS
The mean age of the 205 patients (183 women and 22 men) was 52 years (range, 34-78 years). The entire procedure including transcutaneous lower blepharoplasty and MAFT comprised an average of 61 minutes (range, 52-80 minutes) to complete, and the mean resected fat (from the medial, middle, and lateral orbital fat compartments) volumes were 0.58 g for the left eye and 0.56 g for the right eye (range, 0.2-1.3 g and 0.2-1.2 g for left and right eyes, respectively). The total fat volumes delivered to the tear trough and lid-cheek junction were 2.80 and 2.76 mL for the left side and right side, respectively (range, 1.2-6.0 mL and 1.0-6.0 mL, respectively). Patients were monitored for an average of 60.2 months (range, 18-90 months). No major complications such as severe scleral show, prolonged ectropion after lower blepharoplasty or nodulation, and fibrosis for fat grafting occurred. Mild to moderate swelling was noted in the operative areas but subsided after 7 to 10 days. Transient postoperative retraction was noted in 4 cases (2.0%) due to severe lower eyelid edema and swelling; however, all of them proved to be uneventful within 1 month.
The patient satisfactory scores by 5-point Likert scale were 0/205 very unsatisfied, 2/205 (1%) unsatisfied, 8/205 (4%) neutral, 39/205 (19%) satisfied, and 156/205 (76%) very satisfied. The patients’ mean postoperative satisfaction was 4.702, which was significantly higher than the midpoint value of 3 (average) on the 5-point scale (mean difference, ∆μ = 1.702, t = 41.362, with P < 0.001) and indicated patients were mostly (95%, 39 + 156/205) pleased with their overall improvement (satisfied or very satisfied). Nine patients (4.4%) requested a secondary touch-up to refine the contouring in the tear trough. Six cases demonstrating the 3 simple steps of blepharoplasty with MAFT for treatment of the lower eyelid are illustrated in Figures 3-6 and Supplemental Figures 1 and 2.
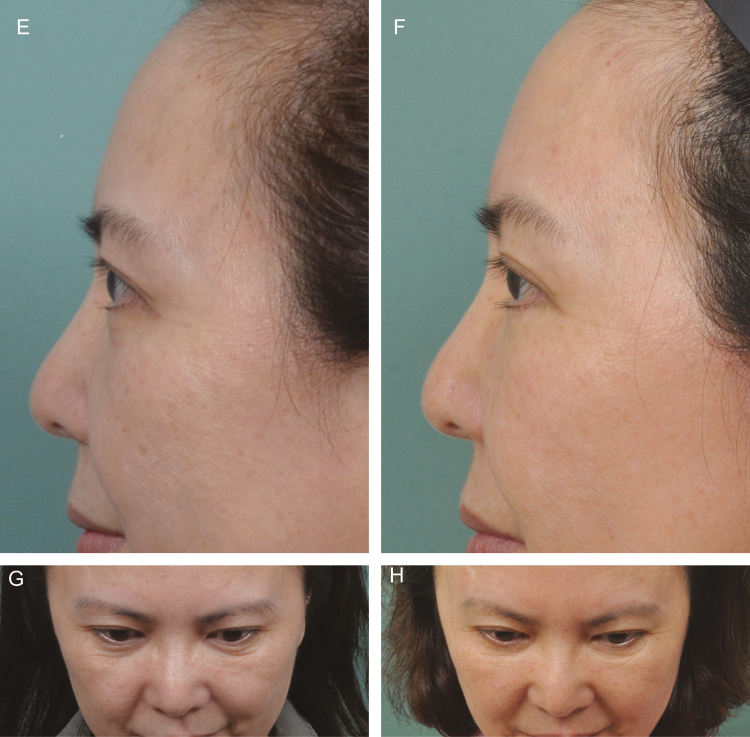
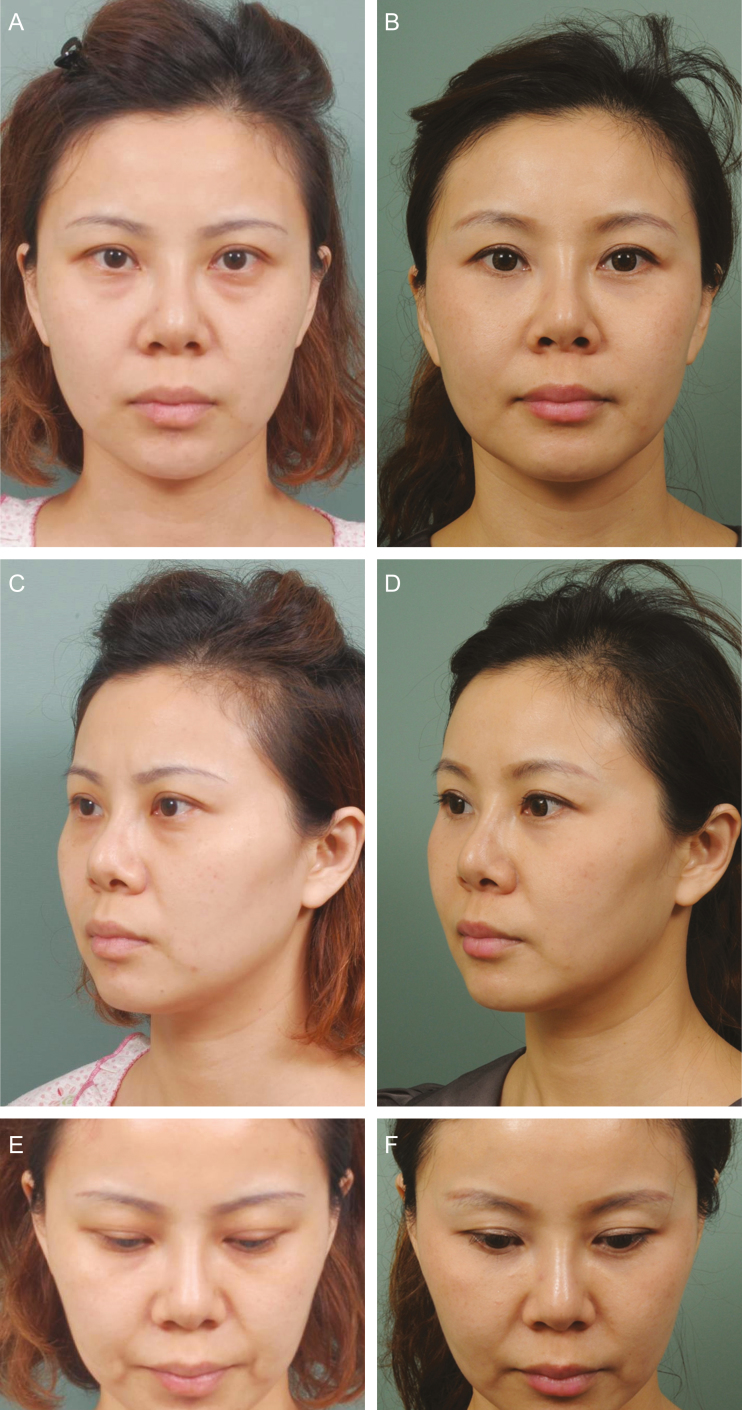
Figure 3.
This 51-year-old woman (A) presented for transcutaneous lower blepharoplasty with micro-autologous fat transplantation to improve her aging lower eyelid. Transcutaneous lower blepharoplasty with skin-only excision was performed in conjunction with micro-autologous fat transplantation to remove right and left orbital fat (0.31 g and 0.43 g, respectively) that was then transplanted in the right and left tear troughs and lid-cheek junctions (4.0 mL and 4.0 mL, respectively). (B) At 57 months after surgery, retention of the fat volume in her tear trough and lid-cheek junction areas was maintained. The (C,D) oblique and (E,F) close-up profile views show good recontouring in the tear troughs and lid-cheek junctions at 57 months postoperatively. The fine wrinkles over the crow’s feet area and the skin dyspigmentation were improved and maintained. (G,H) A downward view demonstrates not only the eliminated infra-orbital fine wrinkles but also rejuvenation of the entire area with appropriate volume restoration.
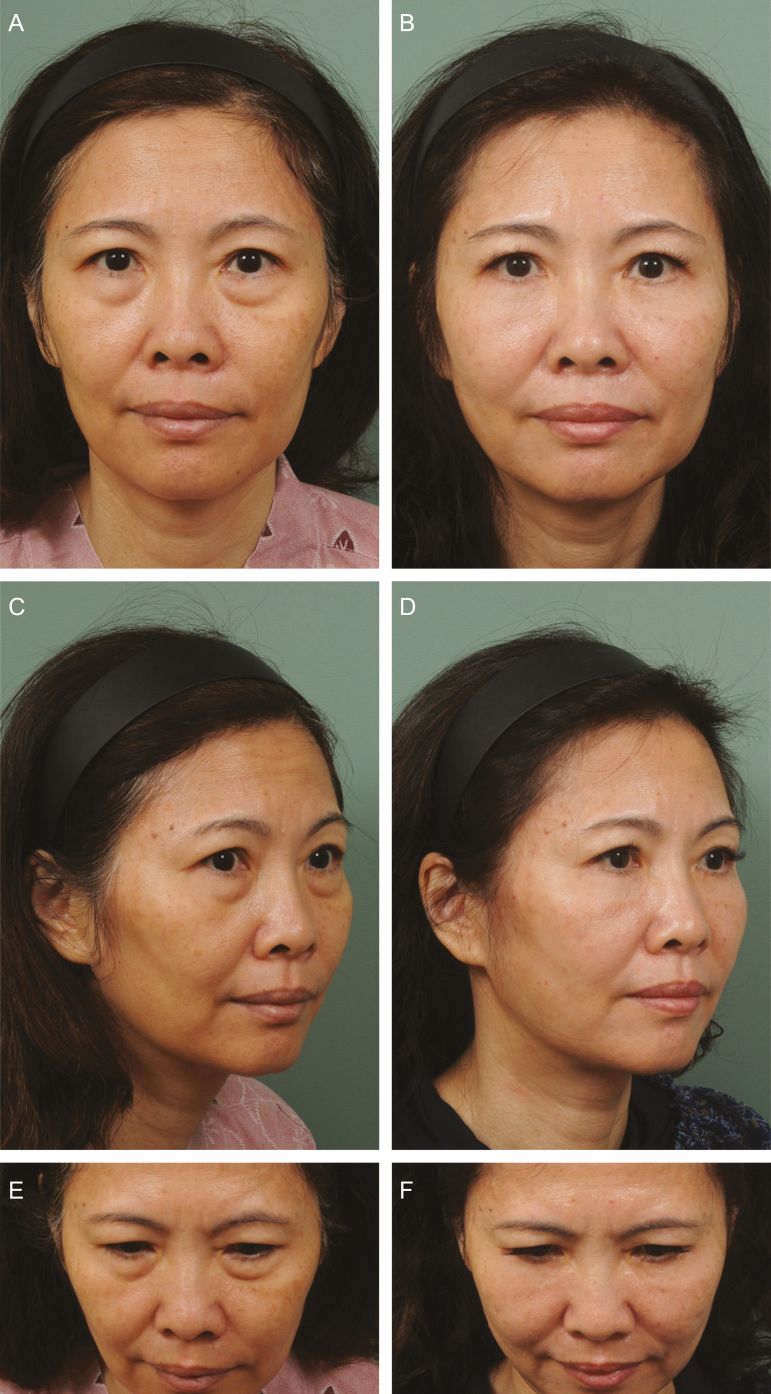
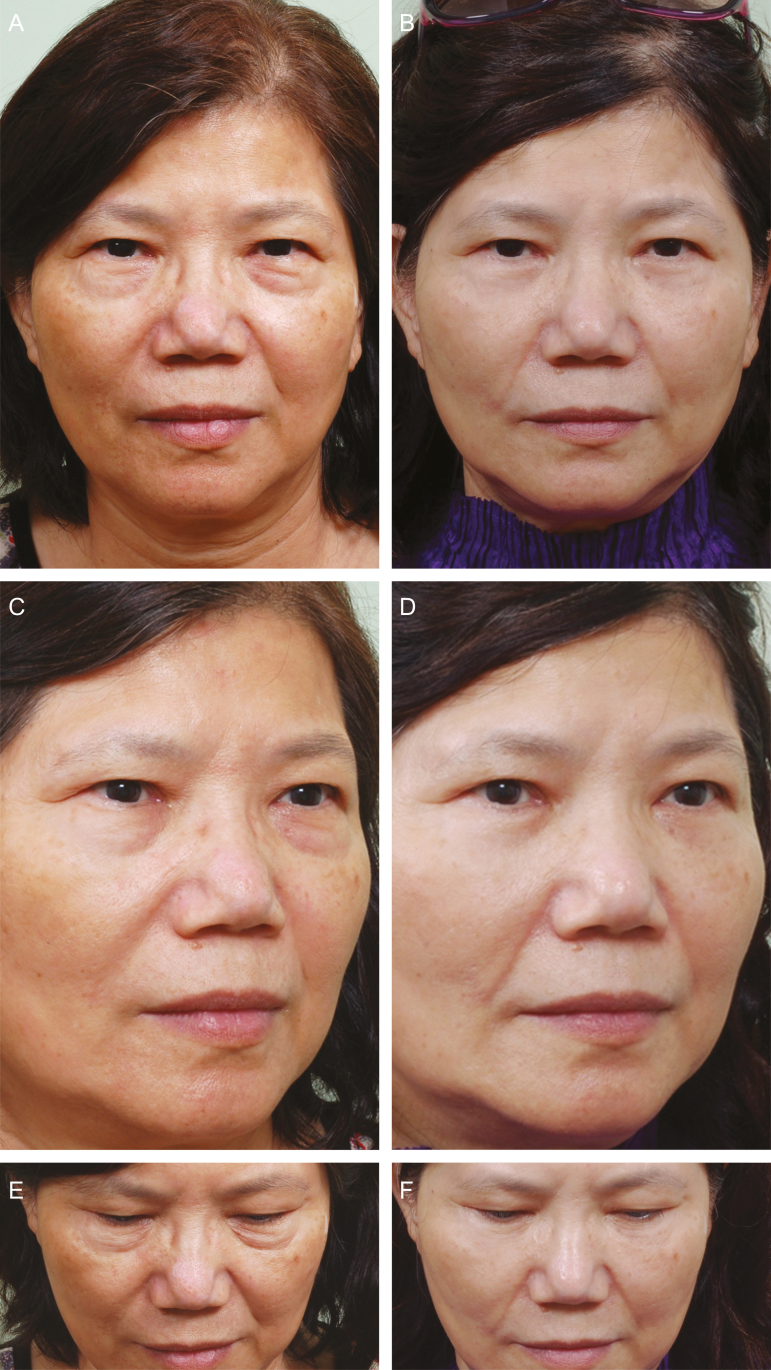
Figure 6.
This 52-year-old woman presented for management of her severe baggy lower eyelid and prominent tear trough and lid-cheek junction. Skin-only transcutaneous lower blepharoplasty and micro-autologous fat transplantation for recontouring the tear trough deformity and lid-cheek junction were performed. (A) The total resected orbital fat volumes were 0.23 g and 0.31 g (right side and left side, respectively), and the total amount of fat volumes grafted to the tear trough and lid-cheek junction were 2.0 mL and 2.0 mL (right side and left side, respectively). (B) The improved appearance of her lower eyelid at 12 months after a single micro-autologous fat transplantation session and lower blepharoplasty is shown. (C,D) The recontoured tear trough and lid-cheek junction with recontouring of the baggy lower eyelid are shown in the oblique view. (E,F) Downward-looking view further illustrates that contouring of the infra-orbital area was well preserved.
Figure 4.
This 38-year-old woman presented for fat grafting to improve her aging lower eyelid including moderate baggy eye, skin redundant, and dark circles. Transcutaneous lower blepharoplasty with micro-autologous fat transplantation for recontouring the tear trough deformity and lid-cheek junction was performed. (A) Fat graft volumes of 3.5 mL and 3.0 mL were placed in the right side and left side, respectively, after removal of orbital fat volumes of 0.11 g and 0.12 g from the right side and left side, respectively. (B) Four years after a single micro-autologous fat transplantation session and lower blepharoplasty, the improved appearance of her lower eyelid was maintained. (C,D) The recontoured tear trough and the lid-cheek junction with an improved appearance of the baggy lower eyelid are shown in the oblique view. (E,F) Close-up, downward-looking view further indicates the skin rejuvenation effects with diminished dark circles.
DISCUSSION
Numerous surgical techniques focusing on the management of protruding orbital fat, lower eyelid dermatochalasis, tear trough deformity, and prominence of the lid-cheek junction are available to treat the aging lower eyelid.2-12 Although these approaches are reliable and achieve acceptable results in selected cases, the invasiveness and potential complications remain a challenge for patients and surgeons.24,25 Rohrich et al summarized various techniques and documented 5-step lower blepharoplasty emphasizing the necessity of simultaneous blending of the eyelid-cheek junction.26 According to the concept of augmentation blepharoplasty reported by Tonnard et al, greater emphasis has been placed on recontouring the tear trough and lid-cheek junction. This has convinced surgeons that managing the orbit-malar sulcus is crucial for total rejuvenation in lower blepharoplasty.14 Although fat grafting has become popular in the past decade,27 several unresolved issues exist for fat grafting procedures. Particularly, with peri-orbital fat grafting, patient dissatisfaction often occurs because of unpredictable absorption rates and potential morbidities such as visible nodulation and fibrosis. There remains a lack of evidence regarding long-term outcomes.28-34 Lin et al demonstrated the clinical feasibility of MAFT for facial recontouring and rejuvenation of the temple,16 forehead,17 sunken upper eyelid,18,21 and nasal dorsum.19 They also recently proposed a new strategy for combined augmentation of the nasolabial groove, ergotrid, and upper lip for the treatment of gummy smile.15
The concept of MAFT, as proposed by Lin et al in 2007,22 emphasized that the volume of each delivered parcel should be less than 1/100 mL (<0.01 mL) to avoid potential fat grafting morbidities. The MAFT-GUN instrument provides surgeons with a tool to control the parcel volume and avoid central necrosis and its associated complications. The long-term clinical results specifically demonstrated accurate and consistent control of the tiny fat parcels (1/60, 1/90, 1/120, 1/150, 1/180, and 1/240 mL) by avoiding occasional dislodgement of larger parcels (Video 3, available online at www.aestheticsurgeryjournal.com). Dislodgement might result with central necrosis and subsequent nodularity and skin irregularity.
The reasons for the promising results demonstrated by simple 3-step transcutaneous lower blepharoplasty with MAFT utilized for contouring the tear trough and lid-cheek junction might be further elucidated by skin excision, orbital fat removal, and MAFT itself (Table 1).
Table 1.
Technical Details, Indications, and Considerations for Simple Three-Step Transcutaneous Lower Blepharoplasty With MAFT
| Technique details | Indications and purposes | Other considerations and comments | |
|---|---|---|---|
| Skin excision | Ciliary margin: 3- to 4-mm skin excision, as in Figure 1, is extended laterally (animation and video) | Indicated for dermatochalasis to alleviate fine skin wrinkles and offer upward and lateral vector lifts | Avoids extensive skin excision-induced ectropion |
| No extensive dissection to the arcus marginalis | Preservation of the anterior and middle lamina of the lower eyelid in a well-vascularized recipient for fat grafting | Decreases postoperative edema | |
| Could be combined with resection of a strip of the OO muscle | Corrects hypertrophic pretarsal fullness | Should be conservative to decrease severe damage to motor nerve innervation to the OO muscle and potential ectropion development37-42 | |
| Adjunctive OO plication to create pretarsal fullness43 | Indicated for the recreation of aesthetic pretarsal fullness or pretarsal flatness due to previous lower blepharoplasty | Aesthetic improvement is expected | |
| Orbital fat removal | Approach to the medial orbital septum using medial splitting to create a slit in the pretarsal portion of the OO muscle (animation and video) | Intended for the removal of medial, middle, and lateral compartments of orbital fat | An appropriate amount of orbital fat is resected according to the individual’s and surgeon’s preferences |
| The fat compartments might be minced for the creation of fat grafts, although the total amount is quite small (average: 0.57 g in this study) | Blending the tear trough and lid-cheek junction necessitates large amounts of fat (average: 2.78 mL of fat grafted in this study) that are inadequately recontoured using orbital fat via a repositioning method | Long-term effectiveness demonstrates that recontouring the tear trough and lid-cheek junction is promising | |
| MAFT | Supporting: Structured fat graft survives via the MAFT technique by supporting immediate tissue edema with strong consolidating support to prevent sequelae such as tissue sagging or transient ectropion. MAFT is performed securely through many fenestrated windows between the ligaments (TTL/ORL) by creating an anchoring effect in the surrounding tissue | Such support might alleviate the sagging and loosened supporting of the TTL/ORL due to the aging process | Compared with a widely adopted concept, the present study did not release the TTL/ORL reinforced by muscular or skin traction, which further induces potential sequelae such as ectropion or mid-face sagging; MAFT showed stable and promising long-term tissue support |
| Recontouring: MAFT was performed using tiny parcels (1/240 mL [0.0042 mL] per parcel) in 3 layers: deep layer, supra-periosteum; middle layer, between the OO muscle and bone; and superficial layer, between the dermis and the OO muscle (animation and video) | MAFT technique presents a reliable clinical effect by avoiding the potential morbidities of nodulation, cyst formation, fibrosis, etc.16-23 | MAFT offers complete and simultaneous contouring by blending the tear trough and lid-cheek junction, the effects of which are often requested with lower blepharoplasty | |
| Rejuvenating: Fat parcels were meticulously placed in the superficial layer in tiny amounts of 1/240 mL per parcel; these were consistently delivered using the MAFT-GUN | Well-performed fat grafting, as demonstrated in the literature,44-46 shows the effects of increasing dermal thickness and collagen formation, which were also illustrated in the improvement of fine wrinkles, dark circles, and skin texture (aging spots) in the present study (Figures 3-8) | Fine wrinkles in the subciliary area and crow’s feet were improved in the close-up view postoperatively in this study |
MAFT, micro-autologous fat transplantation; OO, orbicularis oculi; ORL, orbicularis-retaining ligament; TTL, tear trough ligament.
Skin Excision
While dealing with aging lower eyelids with dermatochalasis, excision of the subciliary skin (or the skin plus a strip of the OO muscle) was indispensable. In this study, the mean age was 52 years (range, 34-78 years), indicating that transcutaneous lower blepharoplasty was prerequisite. However, the OO muscle was conservatively excised to preserve its integrity as much as possible because the innervating motor nerve runs perpendicularly, as clearly illustrated.35-40 Moreover, extensive excision of the OO muscle might induce potential morbidities such as ectropion and flatness of the pretarsal area. However, in certain candidates, hypertrophy of the OO muscle could be eliminated while still achieving the desired aesthetic appearance (Figure 5). In turn, pretarsal fullness, which many members of the Asian population regard as a symbol of good fortune and blessings, might be simultaneously recreated during lower blepharoplasty.41 The subciliary incision often heals well without visible scarring (Figures 3-6; Supplemental Figures 1 and 2). Fat grafting creates a rejuvenating effect by improving fine wrinkles and dark circles. These improvements result from the increasing dermal thickness (up to 200%)42-44 and shading of the surviving fat grafting between the OO muscle and skin dermis (Figures 3-6; Supplemental Figures 1 and 2), which might be attributed to effective and reliable MAFT techniques.15-19,21 Certain skin textures were reported to provide a moisturizing sensation over the fat-grafted area (Figures 3-6; Supplemental Figures 1 and 2).
Figure 5.
This 63-year-old woman presented for rejuvenation of her aging lower eyelid including skin redundancy, eye bags, and prominence in the tear trough deformities/lid-cheek junction depressions. Transcutaneous lower blepharoplasty (skin with a tiny strip muscle flap) with total resected orbital fat volumes of 0.15 g and 0.18 g (right side and left side, respectively) was performed. (A) Micro-autologous fat transplantation was followed by 2.5-mL and 2.8-mL (right side and left side, respectively) fat grafts that were transplanted to her tear trough and lid-cheek junction. (B) At 18 months after a single micro-autologous fat transplantation session and lower blepharoplasty, the volume was maintained in the infra-orbital areas. (C,D) Her contouring significantly improved without visible scarring, as seen in the close-up oblique view. (E) Recontouring of the tear trough and lid-cheek junction shows the long-term effects after micro-autologous fat transplantation. (F) The rejuvenated skin texture (wrinkles, aging spots, and skin color) is also noted in a close-up, downward-looking view.
Orbital Fat Removal
Unlike many maneuvers advocated for in the literature that necessitate extensive dissection to the arcus marginalis and release the TTL/ORL,8-12 a meticulous but limited (10- to 15-mm slit) retro-muscular dissection (retro-OO muscle) was performed through the split in the medial one-third subciliary incision (Video 2). The 3 parts of the orbital fat compartments were exposed and removed accordingly. The main reason that the authors abandoned the traditional method of recontouring tear troughs and/or lid-cheek junctions with orbital fat reposition is the fact that the average amounts of fat grafts were 2.80 mL and 2.76 mL for the left and right sides, respectively. However, the average weights of the resected orbital fats were 0.58 g and 0.56 g for the left and right eyes, respectively, in this study. This mismatching of resected fat volumes to transplanted fat volumes further elucidated the effectiveness of repositioning/relocating orbital fat for blending the tear trough/lid-cheek junction and was neither promising nor long-lasting during long-term follow-up.
MAFT
In this study, the absence of the violation of the lower eyelid middle lamina, the avoidance of releasing the TTL/ORL, and the lack of caudal periosteum dissection further provide a niche for the survival of the transplanted fat parcels. With multiple fenestrating windows made by advancing blunt injection cannulas through the TTL/ORL, the integrity of the ligaments was disrupted. However, the volumizing support of the transplanted fat grafting and the resulting rejuvenation over the aging prolapsed/weakened ligaments thoroughly reconsolidated and provided homogeneous contouring at the tear trough and lid-cheek junction. Therefore, the commonly seen caterpillar-like fibrosis that occurs after traditional fat grafting because of a partition effect of the TTL/ORL that forms the floor of the lower preseptal space and the roof of the prezygomatic and premaxillary spaces might be eliminated.36 MAFT-GUN utilization assured accurate, precise, and consistent delivery of fat parcels and resulted in increased survival rates and decreased morbidities, such as nodulation and fibrosis. During transplantation, a triggering motion delivers a tiny volume (1/240 mL [0.0042 mL]) per parcel to the deep, middle, and superficial layers of the tear trough and lid-cheek junction, further providing exact restoration volumes without overcorrection. Moreover, the youthful profile after MAFT is enhanced by the augmentation of this area (Figures 3-6; Supplemental Figures 1 and 2).
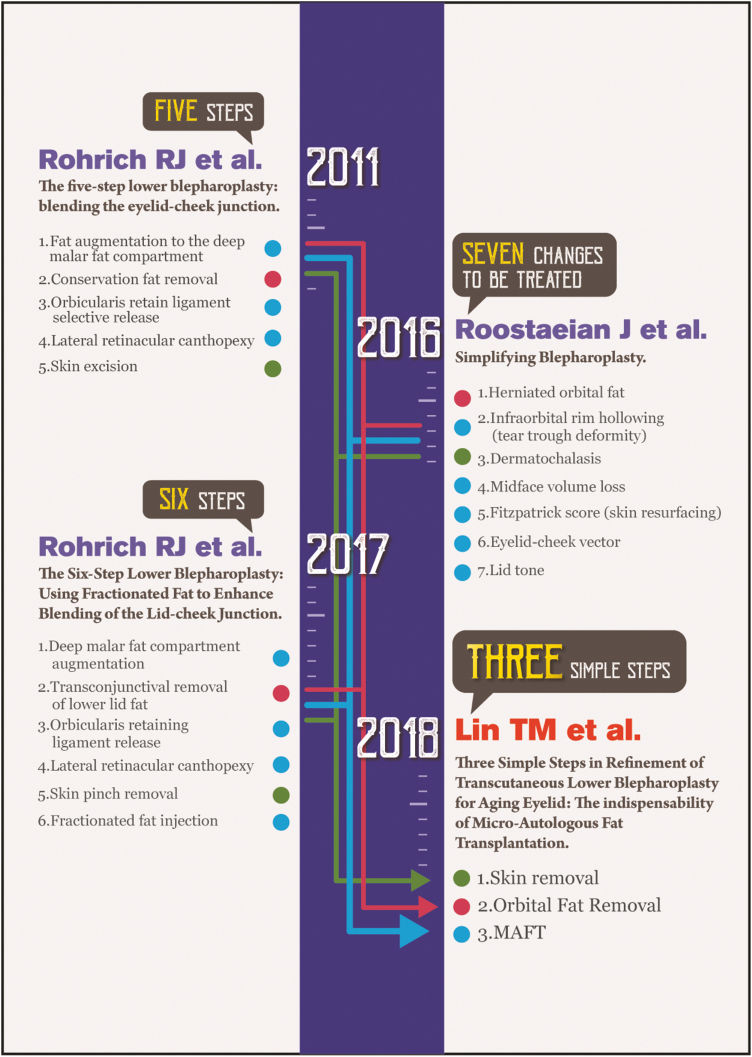
Canthoplasty, which is often adopted as an adjunct to lower blepharoplasty to provide lateral traction and avoid malpositioning (such as sclera show or ectropion), is not always mandatory in our opinion. In this series, 20% of patients (45/205) were older than 60 years, and only one of them underwent canthoplasty. The supporting infra-orbital mechanism could be elucidated by the synergism between the viable fat in this area after the MAFT technique and the rejuvenation of the surrounding soft tissue components, including the periosteum, OO muscle, tear trough/ORLs, and skin.42-44 The ages of the patients featured in Figure 5 and Supplemental Figures 1 and 2 were 63 years, 64 years, and 64 years, respectively, and the postoperative photos further demonstrated the feasibility of our method for aged patients. However, in the poor snap-back test patients (Grade IV, never returns to position and continues to hang down in frank ectropion after the snap-back test), the adjunctive canthoplasty might be indispensable. Neoformation of collagen and elastin further decreased postoperative tissue edema, fibrotic tissue formation, and the subsequent potential for scleral show or ectropion. Therefore, the recommendations and guidelines for lower blepharoplasty by Rohrich26,45 and Roostaeian46 were revised by the present 3 simple steps for refining transcutaneous lower blepharoplasty with MAFT for recontouring the tear trough/lid-cheek junction. The rejuvenating effect of MAFT corrected some associated problems that needed to be solved. However, the extensibility and feasibility remained the same (Figure 7).
Figure 7.
A summary of the concepts and procedures of Rohrich et al (2011, 2017), Roostaeian et al (2016), and the present study (2018) for lower blepharoplasty. In the present study, the procedures of skin removal (green dot) and orbital fat removal (red dot) shared indications with the ones proposed by Rohrich and Roostaeian et al. However, micro-autologous fat transplantation (light blue) elucidated many clinical advantages and simplified the procedures emphasized previously.
Although most patients in our series underwent only one MAFT procedure (94%; 193/205), a secondary touch-up could be considered 4 to 6 months after the first MAFT for those who desire additional improvement in the tear trough and lid-cheek junction. The estimated fat retention rate in this study was not accurately measured, but the overall results were good and the fat survival appeared to be acceptable at the average follow-up time point (60.2 months). The present study is associated with several limitations. Severe preoperative retraction and senile ectropion might be relative contraindications to this method. The results of our subjective measure of patient satisfaction were favorable, but an objective validation of MAFT is lacking from this study. Future work should include 3-dimensional imaging of MAFT results over time to evaluate fat retention and survival.
CONCLUSIONS
In conclusion, this study presented a simple, reliable, and consistent procedure developed based on the MAFT technique and transcutaneous lower blepharoplasty for treating the aging lower eyelid. Favorable outcomes with sustainable long-term effectiveness were obtained during this study, further confirming that the 3 simple steps of lower blepharoplasty with MAFT comprise an innovative alternative for the treatment of the aging lower eyelid.
Disclosures
Dr Tsai-Ming Lin owns the patent rights of the MAFT-GUN and is a scientific adviser for Dermato Plastica Beauty Co., the manufacturer of the MAFT-GUN device. The other authors declared no potential conflicts of interest with respect to the research, authorship, and publication of this article.
Funding
We acknowledge the grant support for this study provided by the Ministry of Science and Technology of Taiwan (107-2314-B-037 -063 -MY2), Ministry of Health and Welfare (MOHW107-TDU-B-212-123006), and Kaohsiung Medical University Hospital (KMUH 105-5R69, 106-6R30).
Supplementary Material
REFERENCES
- 1. Castanares S. Blepharoplasty for herniated intraorbital fat; anatomical basis for a new approach. Plast Reconstr Surg (1946). 1951;8(1):46-58. [PubMed] [Google Scholar]
- 2. Reidy JP. Swellings of eyelids. Br J Plast Surg. 1960;13:256-267. [DOI] [PubMed] [Google Scholar]
- 3.R. B. Surgical treatment of senile changes in the eyelids: the McIndoe-Beare technique. In: Smith B, Converse JM, eds. Proceedings of the Second International Symposium of Plastic and Reconstructive Surgery of the Eye and Adnexa St Louis, Mo: Mosby; 1967:362-366. [Google Scholar]
- 4. Rees TD, Dupuis C. Cosmetic blepharoplasty in the older age group. Ophthalmic Surg. 1970;29:1: 30. [Google Scholar]
- 5. Adamson JE, McCraw JB, Carraway JH. Use of a muscle flap in lower blepharoplasty. Plast Reconstr Surg. 1979;63(3):359-363. [DOI] [PubMed] [Google Scholar]
- 6. Aston SJ. Skin-muscle flap lower lid blepharoplasty: an easier dissection. Aesthetic Plast Surg. 1982;6(4):217-219. [DOI] [PubMed] [Google Scholar]
- 7. Furnas DW. The orbicularis oculi muscle. Management in blepharoplasty. Clin Plast Surg. 1981;8(4):687-715. [PubMed] [Google Scholar]
- 8. Loeb R. Fat pad sliding and fat grafting for leveling lid depressions. Clin Plast Surg. 1981;8(4):757-776. [PubMed] [Google Scholar]
- 9. Hamra ST. The role of orbital fat preservation in facial aesthetic surgery. A new concept. Clin Plast Surg. 1996;23(1):17-28. [PubMed] [Google Scholar]
- 10. Shorr N, Christenbury JD, Goldberg RA. Free autogenous “pearl fat” grafts to the eyelids. Ophthalmic Plast Reconstr Surg. 1988;4(1):37-40. [DOI] [PubMed] [Google Scholar]
- 11. Loeb R. Naso-jugal groove leveling with fat tissue. Clin Plast Surg. 1993;20(2):393-400; discussion 401. [PubMed] [Google Scholar]
- 12. Espinoza GM, Holds JB. Evaluation and treatment of the tear trough deformity in lower blepharoplasty. Semin Plast Surg. 2007;21(1):57-64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Glasgold M, Lam SM, Glasgold R. Volumetric rejuvenation of the periorbital region. Facial Plast Surg. 2010;26(3):252-259. [DOI] [PubMed] [Google Scholar]
- 14. Tonnard PL, Verpaele AM, Zeltzer AA. Augmentation blepharoplasty: a review of 500 consecutive patients. Aesthet Surg J. 2013;33(3):341-352. [DOI] [PubMed] [Google Scholar]
- 15. Huang SH, Huang YH, Lin YN, et al. Micro-autologous fat transplantation for treating a gummy smile. Aesthet Surg J. 2018;38(9):925-937. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Lee SS, Huang YH, Lin TY, et al. Long-term outcome of microautologous fat transplantation to correct temporal depression. J Craniofac Surg. 2017;28(3):629-634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Chou CK, Lee SS, Lin TY, et al. Micro-autologous fat transplantation (MAFT) for forehead volumizing and contouring. Aesthetic Plast Surg. 2017;41(4):845-855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Lin TM, Lin TY, Huang YH, et al. Fat grafting for recontouring sunken upper eyelids with multiple folds in Asians-novel mechanism for neoformation of double eyelid crease. Ann Plast Surg. 2016;76(4):371-375. [DOI] [PubMed] [Google Scholar]
- 19. Kao WP, Lin YN, Lin TY, et al. Microautologous fat transplantation for primary augmentation rhinoplasty: long-term monitoring of 198 Asian patients. Aesthet Surg J. 2016;36(6):648-656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Pu LLQ, Chen YR, Li QF, Wei FC, eds. Total facial rejuvenation with micro-autologous fat transplantation (MAFT). Aesthetic Plastic Surgery in Asians: Principles and Techniques. 1st ed. St. Louis, MO; 2015:127-146. [Google Scholar]
- 21. Lin TM, Lin TY, Chou CK, Lai CS, Lin SD. Application of microautologous fat transplantation in the correction of sunken upper eyelid. Plast Reconstr Surg Glob Open. 2014;2(11):e259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Lin TM, Lai CS.. The treatment of nasolabial fold with free fat graft: preliminary concept of Micro-Autologous Fat Transplantation (MAFT). Paper presented at: 2nd Academic Congress of Taiwan Cosmetic Association Taipei; 2007; Taiwan.
- 23. Coleman SR. Structural fat grafting. Aesthet Surg J. 1998;18(5):386, 388. [DOI] [PubMed] [Google Scholar]
- 24. Boehm KA, Nahai F, ed. Lower eyelid blepharoplasty. 2016. In: Scuderi N, Toth Bryant A, eds. International Textbook of Aesthetic Surgery, Berlin, Heidelberg, Germany: Springer; 2016: 761-772. [Google Scholar]
- 25. Karimnejad K, Walen S. Complications in eyelid surgery. Facial Plast Surg Clin North Am. 2016;24(2):193-203. [DOI] [PubMed] [Google Scholar]
- 26. Rohrich RJ, Ghavami A, Mojallal A. The five-step lower blepharoplasty: blending the eyelid-cheek junction. Plast Reconstr Surg. 2011;128(3):775-783. [DOI] [PubMed] [Google Scholar]
- 27. The American Society of Plastic Surgeons; 2017 Plastic surgery statistics report. Available at https://www.plasticsurgery.org/documents/News/Statistics/2017/plastic-surgery-statistics-report-2017.pdf. Accessed October 9, 2018.
- 28. Khawaja HA, Hernández-Pérez E. Fat transfer review: controversies, complications, their prevention, and treatment. Int J Cosmet Surg Aesthetic Dermatol. 2002;4(2):131-138. [Google Scholar]
- 29. Çetinkaya A, Devoto MH. Periocular fat grafting: indications and techniques. Curr Opin Ophthalmol. 2013;24(5):494-499. [DOI] [PubMed] [Google Scholar]
- 30. Chiu CY, Shen YC, Zhao QF, Hong FL, Xu JH. Treatment of tear trough deformity: fat repositioning versus autologous fat grafting. Aesthetic Plast Surg. 2017;41(1):73-80. [DOI] [PubMed] [Google Scholar]
- 31. Ciuci PM, Obagi S. Rejuvenation of the periorbital complex with autologous fat transfer: current therapy. J Oral Maxillofac Surg. 2008;66(8):1686-1693. [DOI] [PubMed] [Google Scholar]
- 32. Miranda SG, Codner MA. Micro free orbital fat grafts to the tear trough deformity during lower blepharoplasty. Plast Reconstr Surg. 2017;139(6):1335-1343. [DOI] [PubMed] [Google Scholar]
- 33. Strong AL, Cederna PS, Rubin JP, Coleman SR, Levi B. The current state of fat grafting: a review of harvesting, processing, and injection techniques. Plast Reconstr Surg. 2015;136(4):897-912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Trepsat F. Periorbital rejuvenation combining fat grafting and blepharoplasties. Aesthetic Plast Surg. 2003;27(4):243-253. [DOI] [PubMed] [Google Scholar]
- 35. DiFrancesco LM, Anjema CM, Codner MA, McCord CD, English J. Evaluation of conventional subciliary incision used in blepharoplasty: preoperative and postoperative videography and electromyography findings. Plast Reconstr Surg. 2005;116(2):632-639. [DOI] [PubMed] [Google Scholar]
- 36. Hashem AM, Couto RA, Waltzman JT, Drake RL, Zins JE. Evidence-based medicine: a graded approach to lower lid blepharoplasty. Plast Reconstr Surg. 2017;139(1):139e-150e. [DOI] [PubMed] [Google Scholar]
- 37. Hwang K, Nam YS, Choi HG, Han SH, Hwang SH. Cutaneous innervation of lower eyelid. J Craniofac Surg. 2008;19(6):1675-1677. [DOI] [PubMed] [Google Scholar]
- 38. McCord S, Codner M, Nahai F, Hester R. Analysis of the nerve branches to the orbicularis oculi muscle of the lower eyelid in fresh cadavers. Plast Reconstr Surg. 2006;118(2):556-557; author reply 557. [DOI] [PubMed] [Google Scholar]
- 39. Moss CJ, Mendelson BC, Taylor GI. Surgical anatomy of the ligamentous attachments in the temple and periorbital regions. Plast Reconstr Surg. 2000;105(4):1475-1490; discussion 1491. [PubMed] [Google Scholar]
- 40. Oscar M, Ramirez RS. Spatial orientation of motor innervation to the lower orbicularis oculi muscle. Aesthet Surg J. 2000;20(2):107-113. [Google Scholar]
- 41. Jeon YR, Rah DK, Lew DH, Roh TS, Kim YS, Choi HL. Pretarsal augmented lower blepharoplasty. Plast Reconstr Surg. 2016;138(1):74-82. [DOI] [PubMed] [Google Scholar]
- 42. Covarrubias P, Cárdenas-Camarena L, Guerrerosantos J, et al. Evaluation of the histologic changes in the fat-grafted facial skin: clinical trial. Aesthetic Plast Surg. 2013;37(4):778-783. [DOI] [PubMed] [Google Scholar]
- 43. Mojallal A, Lequeux C, Shipkov C, et al. Improvement of skin quality after fat grafting: clinical observation and an animal study. Plast Reconstr Surg. 2009;124(3):765-774. [DOI] [PubMed] [Google Scholar]
- 44. Trivisonno A, Rossi A, Monti M, et al. Facial skin rejuvenation by autologous dermal microfat transfer in photoaged patients: clinical evaluation and skin surface digital profilometry analysis. J Plast Reconstr Aesthet Surg. 2017;70(8):1118-1128. [DOI] [PubMed] [Google Scholar]
- 45. Pezeshk RA, Sieber DA, Rohrich RJ. The six-step lower blepharoplasty: using fractionated fat to enhance blending of the lid-cheek junction. Plast Reconstr Surg. 2017;139(6):1381-1383. [DOI] [PubMed] [Google Scholar]
- 46. Zoumalan CI, Roostaeian J. Simplifying blepharoplasty. Plast Reconstr Surg. 2016;137(1):196e-213e. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.