Abstract
Objective
This study aims to assess the magnitude of depression, anxiety, and stress among health care workers by the coronavirus disease (COVID-19) in Almadinah Almunawwarah, KSA.
Methods
This cross-sectional study examined 122 health care workers between April and May 2020 through the electronic use of the Hospital Anxiety and Depression (HAD) questionnaire, and Perceived Stress Scale (PSS). The perceptions of the participants towards stigmatisation of their profession during the COVID-19 pandemic were also assessed through a Likert's scale. The magnitude of anxiety, depression, and stress were analysed using a mean ± SD, correlation and percentages in respective statistics. A p value of <0.05 was considered significant.
Results
This study found that 32.9% of the healthcare workers frequently faced COVID-19 cases during the ongoing pandemic. As many as 35.6% were unusually anxious. A mean anxiety score of 8.43 ± 4.6 was noted, with significantly higher scores for women and those workers with inadequate training (p < 0.001 and 0.028). Moreover, a mean depression score of 7.6 ± 4.7 (p < 0.002) was recorded for the healthcare workers with inadequate training. About 27.9% of the participants were depressed. The mean stress score of the study cohort was 6.86 ± 2.5. From the cohort, 24.5% and 72.8% experienced mild and moderate stress, respectively. This study found that inadequate training for infection control was associated with a higher proportion of anxiety and depression [OR 1.86 (95% CI: 1.5–2.3; p < 0.043) and OR 2.21 (95% CI: 1.7–2.8; p < 0.018), respectively.
Conclusion
This study found a high prevalence of anxiety, depression, and moderate stress among healthcare workers, regardless of their job specifications. The associated risk factors for anxiety and depression included inadequate training for infection control, and pre-existing stress-provoking medical conditions.
Keywords: Anxiety, COVID -19, Depression, Health care workers, Perceived stress, Psychological impact
الملخص
أهداف البحث
تهدف هذه الدراسةإل قياس مدىالاكتئاب والقلق والإجهادبين العاملين في مجال الرعاية الصحيةبسبب مرض الفيروس التاجي ٢٠١٩(كوفيد-١٩) في المدينة المنورةبالمملكة العربية السعودية.
طرق البحث
أجريتدراسة مقطعيةعلى١٢٢ من العاملين في مجال الرعاية الصحية في المدينة المنورة خلال شهري أبريل ومايو ٢٠٢٠،باستخدام استبانةإلكترونيةلقياس القلق والاكتئاب في المستشفيات، ومقياس الإجهادالمتصور.كما تم تقييم تصور المشاركين تجاه وصم مهنتهم في الجائحة الحالية من خلال مقياس ليكرت. وقد تم تحليل القلق والاكتئاب والإجهاد من الناحيتين الكمية والنوعية باستخدام متوسط وحساب الارتباط والنسب المئوية في الإحصاءات المعنية بذلك.
النتائج
وجدت هذه الدراسة أن ٣٢.٩٪ من العاملين في مجال الرعاية الصحية تعاملوا مع حالات كوفيد-١٩بشكل متكرر أثناء الجائحة. وكان ما يصل إلى ٣٥.٦٪ قلقين بشكل غير عادي. ولوحظ أن متوسط درجة القلق ٨.٤٣ ± ٤.٦،مع درجات أعلى بكثير للنساء والعاملين الذين لم يتلقوا التدريب الكافي. وعلاوة على ذلك، تم تسجيل متوسط درجة اكتئاب٧.٦ ± ٤.٧للعاملين في مجال الرعاية الصحية الذين لم يتلقوا تدريبا كافيا، بينما كان ما يقارب ٢٧.٩٪ من المشاركين مكتئبين.وكانمتوسط درجة الإجهاد ٦.٨٦ ±٢.٥،بينما عانى٢٤.٥٪ من إجهاد خفيف، وعانى ٧٢.٨٪ من إجهادمعتدل. وجدت هذه الدراسة أن عدم كفاية التدريب على مكافحة العدوى كان مرتبطا بنسبة أعلى من القلق والاكتئاب لدى العاملين في الرعاية الصحية.
الاستنتاجات
وجدت الدراسة أنهناك نسبة عالية من القلق والاكتئابوالإجهاد المعتدل بين جميع العاملين في مجال الرعاية الصحية بغض النظر عنطبيعةاختلافوظائفهم. وكانت عوامل الخطر المصاحبة لكل من القلق والاكتئاب بسبب عدم كفاية التدريب على مكافحة العدوى والمشاكل الطبية المصاحبة للإجهاد الموجودة من قبل.
الكلمات المفتاحية: الأثر النفسي, العاملون في مجال الرعاية الصحية, كوفيد-١٩, الاكتئاب, التوتر, القلق, المدينة المنورة
Introduction
Among the challenges of the 21st century are infectious diseases, which continue to be a major cause of death and morbidity due to new or re-emerging infectious pathogens.1, 2, 3 In January 2020, the World Health Organization (WHO) designated the outbreak of a new coronavirus disease, SARS-CoV2 (COVID-19), a Public Health Emergency. Later, in March 2020, the WHO declared the outbreak to be a pandemic,4 with estimates of global mortality at 3.4%.5 This was the time that fear, worry, and panic leading to stress were building, at a perceived or real threat throughout the populations of the world, especially among health care workers. Health workers are working under pressure, with long shift times and lack of personal protective equipment (PPE), in fear of transmitting the infection to their family, and at risk of self-exposure and infection.6 In addition, avoidance of community and lack of coping strategies also have negative effects on their mental health. The COVID-19 outbreak is a unique and unprecedented scenario for many workers across the world, particularly if they have not been involved in similar responses earlier.
A cross-sectional study among 1257 health care workers in Wuhan, China reported psychological symptoms such as depression in 50%, anxiety in 45%, insomnia in 34%, and mental distress in 71.5%, especially among female nurses and frontline health care workers, who were directly involved in the management and care for patients with COVID-19.7 Recently, in Singapore, a study of 470 health care practitioners found 14.5% to be positive for anxiety, 8.9% for depression, 6.6% for stress, and 7.7% for clinical concern of post-traumatic stress disorder (PTSD).8 Moreover, the stress and psychological effect among 79 patients were studied, 39% (n = 30) of sample were infected health care workers had suffered severe acute respiratory syndrome (SARS) in the 2003 outbreak. The health care workers completed the Perceived Stress Scale and showed significantly higher stress levels among positive cases compared with their matched healthy controls (n = 145). Along with stress, individuals also reported poor sleep, depressed mood, weepiness, nightmares, and poor concentration.9
Another study addressing the SARS and Ebola virus outbreaks has also shown that healthcare employees suffered burnout, traumatic stress, anxiety, and depressive symptoms even after the outbreak.10 The impact of the 2015 MERS outbreak on 1800 hospital practitioners in Korea was assessed using the total Impact of Events Scale-Revised. They found that 51.5% exceeded the cut-off score of 25 for a diagnosis of PTSD.11 One year after the SARS outbreak, a study found that health care workers that had survived a SARS infection still had elevated stress levels, worrying levels, and psychological distress.12
A similar research documented that 23.9% of SARS survivors still had PTSD at an 8-year follow-up.13 In KSA, a study in the oncology health team showed that physicians were recorded to have the highest rate of burnout (35.1%), followed by nurses (29%), and allied healthcare professionals (27%).14
Knowing the psychological impact of the COVID-19 outbreak among health care workers is thus imperative to guide future policies and plans for their psychological well-being, as well as ensuring an optimal health care service.
Our aim in this study was to assess the magnitude of psychological impact among health care workers, including depression, anxiety, and stress, and their perception of COVID-19 based on environmental factors, professional strength, and community stigmatisation in Al Almadinah Almunawwarah, KSA during this early phase of the pandemic.
Materials and Methods
This cross-sectional study was carried out among tertiary health care workers in Almadinah Almunawwarah City during April and May 2020. The required sample size was calculated to be 122 using the Open epi calculator for 10% prevalence and bond of error of 0.05 in the target population. The inclusion criteria were health care workers, including all cadres of doctors, nurses, technicians, and pharmacists working in secondary care hospitals for more than one year. All health care staff solely engaged in administrative work and not dealing directly with patient care were excluded. An electronic data form was developed in English, and distributed through WhatsApp among researchers in the target population of Almadinah Almunawwarah. There were four sections in the questionnaire: demographic and work details, a validated hospital anxiety and depression (HAD) scale questionnaire, perceived stress scale (PSS), and health care workers’ perceptions of the COVID 19 experience, based on their professional strength, working conditions, and also the stigmatisation of their profession12 in the current pandemic. SPSS version 22 was used for data entry and analysis. All descriptive analyses were performed using percentage and mean ± SD as suited to variables. Dependent variables (e.g., anxiety score, depression score, and stress level) were measured as mean ± SD, and correlations were measured using the Pearson r value. Moreover, the proportion of normal, borderline, and abnormal was driven out for anxiety and depression according to the respective scores of 0–7, 8–11, 12, and above. Whereas the 4-point PSS was used as the cut-off for low, moderate, and severe stress for respective score categories were 1–5, 6–11, and 12–16.
Inferential analysis was performed using chi-square for proportions of anxiety, depression, stress, and association of risk factors, while one-way ANOVA was applied for comparing mean dependent scores of anxiety, depression, and stress.
Results
Table 1 depicts the overall characteristics of the participating health care workers. Most (75%) of the participants were between 20 and 40 years old; 64.5% were female, and 76.3% were married. More than half (52.6%) were physicians, 15.8% were nurses, and 6.8% were emergency room (ER) physicians. It was reported that 74.3% were living with their families. Among all respondents, eight (10.5%) were current smokers. Regarding the occurrence of known medical problems, 71.6% reported no problem, whereas 10.8%, 6.7%, 5.6%, and 1.4% had asthma, hypertension, diabetes, and anxiety disorder, respectively. It was found that 32.9% were involved in COVID-19 cases frequently during this ongoing pandemic.
-
A)
PSYCHOLOGICAL IMPACT
Table 1.
Distribution of demographic details of health care workers [n = 118].
| Characteristics | Frequency | Percent |
|---|---|---|
| Age (years) | ||
| 20–30 | 25 | 21.2 |
| 31–40 | 64 | 54.2 |
| 41–50 | 12 | 10.1 |
| >50 | 17 | 14.4 |
| Gender: | ||
| Male | 42 | 35.6 |
| Female | 76 | 64.4 |
| Marital Status: | ||
| Married | 90 | 76.3 |
| Unmarried | 22 | 18.6 |
| Divorced | 6 | 5.1 |
| Job Category: | ||
| Physician | 62 | 52.5 |
| ER Physician | 8 | 6.8 |
| Surgeon/Anaesthetist | 5 | 4.2 |
| Pharmacist | 4 | 3.3 |
| Pathologist | 5 | 4.2 |
| Nurse | 19 | 16.1 |
| Dietician | 9 | 7.6 |
| Technician | 6 | 5.1 |
| Living with family: n = 111 | ||
| Yes | 83 | 74.6 |
| No | 28 | 25.4 |
| Smoking Status: | ||
| Current Smoker | 12 | 10.2 |
| Non- Smoker | 99 | 83.9 |
| Ex- Smoker | 07 | 5.9 |
| Any Known Medical Problem: n = 111 | ||
| None | 80 | 72.0 |
| Asthma | 12 | 10.8 |
| Anxiety | 02 | 1.8 |
| Hypertension | 07 | 6.3 |
| Diabetes mellitus | 06 | 5.4 |
| Hypo-thyroidsm | 03 | 2.8 |
| Epilepsy | 01 | 0.9 |
| How often faced COVID cases | ||
| All time | 3 | 2.6 |
| Frequent | 39 | 33.0 |
| Never | 26 | 22.0 |
| Occasionally | 50 | 42.3 |
The HAD scale was used to analyse anxiety and depression, and PSS was used to analyse stress among participants to measure psychological impact. The reliability of the HAD scale was calculated as 0.86 for anxiety, and 0.77 for depression. The mean anxiety score was reported as 8.43 ± 4.6. Regarding anxiety, 35.6% and 21.2% participants had an abnormal and borderline score, respectively. The mean depression score was 7.6 ± 4.7, and the respective proportions for borderline and abnormal scores were 21.2% and 27.9%. The mean stress score was 6.86 ± 2.5. A total of 24.5% experienced mild stress (score between 0 and 5 on PSS), while 72.8% experienced moderate stress (score between 6 and 11 on PSS) [ see Table 2].
Table 2.
Analysis of HAD &PSS of participants n = 118.
| Anxiety | Depression | Perceived Stress | |
|---|---|---|---|
| Mean ± SD Median Range |
8.43 ± 4.6 9.00 0–19 |
7.6 ± 4.7 7.00 0–14 |
6.86 ± 2.5 8.00 0–12 |
| Normal Borderline Abnormal score |
51 (43.2%) 25 (21.2%) 42 (35.6%) |
60 (50.8%) 25 (21.2%) 33 (27.9%) |
Low Stress: 29 (24.5%) Moderate: 86 (72.8%) Severe: 3 (2.6%) |
| Crohnbach alpha | 0.86 | 0.77 | 0.69 |
We detected a statistically significant positive correlation between anxiety and depression scores (r = 0.58, p < 0.000), between anxiety and PSS scores (r = 0.335, p < 0.000) and between PSS and depression scores (r = 0.481, p < 0.000).
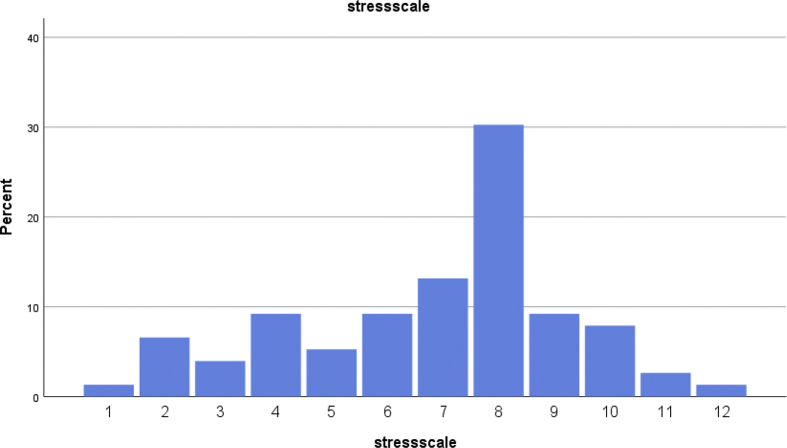
The maximum stress score among participants was 12, which was reported by only 3%. The most frequently reported score was 8.0, reported by 30% (n = 36) of the respondents. In this left-skewed curve, the mean score was 6.8 [Figure 1].
Figure 1.
Dynamics of Stress score among participants.
As shown in Table 3, higher anxiety scores were detected for females, and for those who did not have adequate training in infection control (p < 0.001 and P = 0.028, respectively). The depression score was significantly higher (p < 0.002) among inadequately trained health workers, while there was no significant association between the PSS score and any other independent variable.
Table 3.
Comparison of mean scores of anxiety, depression and PSS.
| Variable | Indices | Groups | Mean square | F | Siga |
|---|---|---|---|---|---|
| Gender | Anxiety score | Between group | 234.8 | 12.07 | 0.001 |
| Within group | 19.4 | ||||
| Depression score | Between group | 17.06 | 0.792 | NS | |
| Within group | 21.51 | ||||
| Perceived stress score | Between group | 1.28 | 0.238 | NS | |
| Within group | 5.4 | ||||
| Training in infection control | Anxiety score | Between group | 102.02 | 5.06 | 0.028 |
| Within group | 20.36 | ||||
| Depression score | Between group | 188.14 | 9.94 | 0.002 | |
| Within group | 18.92 | ||||
| Perceived stress score | Between group | 1.66 | 0.31 | NS | |
| Within group | 5.4 |
One− way ANOVA is applied
Inadequate training was significantly associated with a higher proportion of anxiety and depression [OR 1.86 (95% CI: 1.5–2.3; p < 0.043) and OR 2.21 (95% CI: 1.7–2.8; p < 0.018), respectively]. Meanwhile, stress was significantly associated with known medical problems among participants (OR 1.8 (95% CI: 1.1–3.6; p < 0.04) [Table 4].
-
b)
PERCEPTION OF COVID-19
Table 4.
Association of Risk factors to Anxiety, Depression and Stress.
| Factors | Anxiety |
Depression |
Perceived Stress |
|||
|---|---|---|---|---|---|---|
| OR (95%CI) | p-value | OR (95%CI) | p-value | OR (95%CI) | p-value | |
| Inadequate training for Infection Control | 1.86 (1.5–2.3) | 0.043∗ | 2.21 (1.7–2.8) | 0.018∗ | 0.73 (0.7–7) | 0.78 |
| Job category | 1.38 (0.55–3.4) | 0.48 | 0.9 (0.36–2.2) | 0.81 | 1.03 (0.8–1.34) | 0.91 |
| Working frequently with COVID | 1.32 (0.5–3.5) | 0.24 | 1.05 (0.4–2.7) | 0.41 | 1.26 (0.4–3.7) | 0.67 |
| Associated medical Condition | 1.07 (0.5–2.2) | 0.84 | 1.125 (0.78–1.6) | 0.36 | 1.8 (1.1–3.6) | 0.04∗ |
Gender and age were layered in this model.
∗Significant P-value.
It was revealed that 53.9% of participants were satisfied with the adequacy of their training, compared to only 48.7% towards the PPE provisions. Similarly, 69.7% were confident in explaining the infection control procedures at their facility, compared to 61.7% on the acquisition of special training in infection control. Likewise, the majority (51.5%) showed a lack of confidence towards the PPE provision, compared to 46%, 38.2%, and 30.3% for overall training, special infection control training, and on-site explanation of infection control procedures respectively [Table 5].
Table 5.
Professional attitude towards training and technical resources n = 118.
| Attitude | Adequacy of overall training Fx (%) |
Training acquired in infection control fx(%) | Infection control procedures explained fx(%) | Provided with PPE fx(%) |
|---|---|---|---|---|
| Fully Confident | 22 (18.4%) | 36 (30.3%) | 54 (46%) | 26 (22.4%) |
| Fairly Confident | 42 (35.5%) | 32 (31.6%) | 28 (23.7%) | 31 (26.3%) |
| Not confident at all | 8 (6.6%) | 8 (6.6%) | 9 (7.9%) | 12 (10.5%) |
| Slightly confident | 26 (22.4%) | 17 (14.5%) | 20 (17.1%) | 23 (19.7%) |
| Somewhat Confident | 20 (17.1%) | 20 (17.1%) | 6 (5.3%) | 25 (21.1%) |
Table 6 shows the participants’ responses to institutional support. Most (34.2%) showed no confidence in emotional support, followed by 19.7% for their care, and 18.4% each for being appreciated, and having a supportive environment.
Table 6.
Institutional Support in crisis situation n = 118.
| Our well- being was important fx(%) | Emotional Support provided as needed fx(%) | Felt appreciated fx(%) | Supportive environment fx(%) | |
|---|---|---|---|---|
| Not Confident | 23 (19.7) | 40 (34.2) | 22 (18.4) | 22 (18.4) |
| Slightly Confident | 30 (25) | 14 (11.9) | 28 (23.7) | 26 (22.4) |
| Somewhat confident | 12 (15.8) | 26 (22.4) | 16 (13.2) | 25 (21.1) |
| Fairly confident | 31 (26.3) | 23 (19.8) | 23 (19.8) | 25 (21.1) |
| Completely Confident | 16 (13.2) | 14 (11.9) | 25 (21.1) | 16 (13.2) |
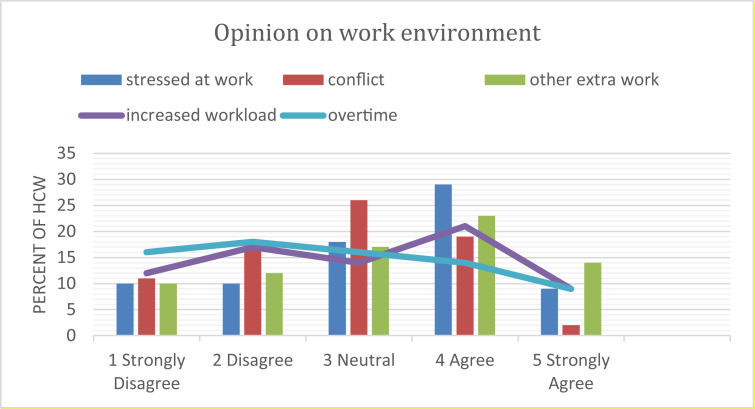
Thirty-eight percent agreed with the statement that they felt stressed at work, with equal proportions for strongly agree and strongly disagree (11.8%). A large proportion (34.2%) were neutral towards having a conflict with colleagues, and only 25% agreed with this statement [Figure 2].
Figure 2.
Opinion of participants regarding work environment.
Regarding increased workload and other extra work that had been done, both the agree and disagree categories (38.2% and 30.3%, respectively) saw nearly equal responses.
Opinion regarding overtime was nearly equally distributed for all categories, except strongly agreed (which accounted for just 11% of responses) [Figure 2].
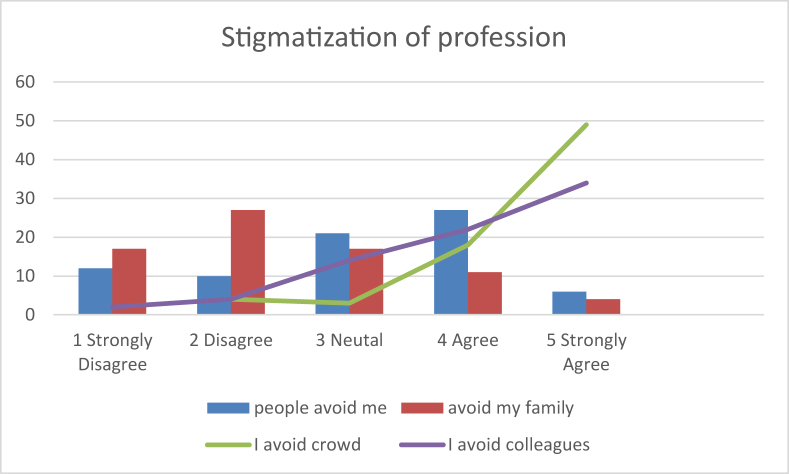
More than one-third (35.5%) of health workers agreed that people avoided them because of the risk of disease transmission, while most of them (75.8%) disagreed that people also avoided their family members. Most (88.2%) of the health workers agreed that they avoided crowds, while 73.6% also avoided colleagues to prevent the spread of infection [Figure 3].
Figure 3.
Stigmatization of medical profession and their own attitude during pandemic.
Discussion
The COVID-19 outbreak has led to significant repercussions across various domains, including the economy, sporting, education, and health. The pandemic is a health crisis that impacts physical and mental health. For instance, the quarantine and communicating restrictions have resulted in people being stuck indoors and fearing infection. At the same time, anxiety due to fear of infection or transmitting the infection to loved ones, and depression among family and friends as a result of an altered lifestyle, social distancing, and guilt of spreading the virus, are some of the issues that health workers are experiencing. The world has experienced various infectious disease outbreaks, such as the SARS outbreak in 2003, which was contained through various quarantine measures. However, the severity of the COVID-19 pandemic has had a significantly higher impact on mental distress among health workers.
In our study, the rates of anxiety, depression, and moderate stress were found to be 35.5%, 27.9%, and 72% among health care workers, respectively. These increased levels of anxiety and depression suggest the potential for an increase in stress-related disorders. All three anxiety, depression, and stress scores were found to be positively correlated. It was evident that anxiety and depression rates were significantly associated with the lack of training in infection control. In contrast, a severe level of stress was only associated with existing medical problems. This is because the medical practitioners at the forefront of the fight against the virus are experiencing traumatic events arising from the patients' conditions and high death rates. There have been reports of traumatic stress among medical practitioners in the fight against COVID-19, including cases of medical practitioners ending their lives. This is in accordance with the notion that the elevation of traumatic stress results in low physical integrity and subjective response, which poses a threat to one's well-being15(Maunder et al., 2006). This might significantly impact their physical well-being in the long run. This is supported by a similar study done in China by Xiao et al. (2020), which found negative associations between the effect of social support on sleep, self-efficacy, anxiety, and stress levels of medical staff.16 Another recent study, measuring depression and anxiety among health care providers in KSA by AlAteeq et al. (2020) reported depressive disorder (55.2%), ranging from mild (24.9%), moderate (14.5%), and moderately severe (10%) to severe (5.8%). Half of the sample had a generalized anxiety disorder (51.4%), which ranged from mild (25.1%) and moderate (11%), to severe (15.3%). These statistics are almost double to those of our study, which could be due to our smaller sample size (122 as compared to 502), and more diversity in their sample.17 A similar result of 37.3% regarding anxiety was recorded by Anoop Krishna et al. among Nepalese health workers. However, depression was much lower at 8%, compared to 27.6% in our study.18
We found that 34.2% of the participants cited an absence of emotional support. Kang et al. (2020) have claimed that in the COVID-19 pandemic, health practitioners are handling the high risk of getting infected, inadequate protections that increase risk of infection, discrimination, patients with negative emotions, isolation, frustration, exhaustion and not being able to contact their families.19 These findings suggest that the absence of emotional support could be attributed to medical practitioners isolating themselves to lower the risk of infecting their family members. Family is a principal form of emotional support. Thus, significant disruption of emotional support due to helping and protecting others resulted in participants reporting an absence of social support. Moreover, the absence of social support reported by our participants can be attributed to the lack of safety measures taken by health institutions to protect their staff, resulting in participants’ development of psychological strain, as they not only face the threat of battling the pandemic, but also of being attacked.
In addition, stigmatisation against health workers is another aspect identified in this research, with 35.5% of participants reporting incidents of stigmatisation. When individuals are faced with potential disease threats, they might develop avoidant behaviours, such as the avoidance of contact with people having similar symptoms, and strictly obeying social distancing norms20 (Li et al., 2020). With the increase of fear based on the threat that the pandemic poses, the re-entry process of medical practitioners into society is characterised by people viewing them as a potential threat. In the case of the COVID-19 outbreak, the cause and progression of the disease are unclear; thus, there is an opportunity for the emergence of rumours and close-minded attitudes. The SARS outbreak resulted in an increase in anxiety levels in Hong Kong, where it was reported that 70% of the population expressed anxiety21 (Torales et al., 2020). People from Wuhan were stigmatised for the outbreak of COVID-19 by other Chinese people, and now, Chinese people are being stigmatised in the international community. Medical staff who are at the forefront in the fight against COVID-19 are also experiencing interpersonal isolation arising from fears they might infect their loved ones. In our study, medical practitioners reported not only isolating themselves from their loved ones, but also their fellow colleagues. This might impact their willingness to seek medical care or get tested, based on increased fear of being shunned, thus increasing the risk of infection.
In this study, 38% of the respondents reported increased levels of stress in their working environment. The current acute health crisis has placed health services under severe pressure, resulting in a more stressful working environment. This is evidenced from only 48.7% of the participants feeling confident about their provision of PPE, and compounded by the potential threat of acquiring the virus. Although the study results report mild levels (72%) of stress, the situation could worsen as the workload increases, resulting in a shortage of medical personnel.
The characteristics of the study population can be linked to the psychological issues addressed in the study. Most (74.3%) of the respondents live with their families, and 34.2% reported not having confidence in the available emotional support because of the withdrawal of their primary source of social support, the family. With most of the participants living with their family, emotional support from the family realm is of great importance. However, the risk of infecting their families might result in withdrawal of close attachment with family members, thus explaining the registered incidences of lack of emotional support.
Limitations
The study's small sample size is a limitation, as is the fact that the information was collected online due to strict lockdown restrictions at that time. The sample of health care workers was widely diverse, which could have influenced the study in particular ways.
The precision of the study might be low because of relatively smallerThe study'ssamplesample size and data collection procedure, that was done through electronic questionnaire due to strict lockdown restrictions at that time. The sample of health care workers was widely diverse depending on their cadre, job description and duty hours, that again might have influenced the effect size somehow.
Conclusion
There was a high rate of anxiety and depression among healthcare workers regardless of their job specification. We found that all health care workers were experiencing stress, but few reported severe stress. Inadequate training proved to be associated with higher anxiety and depression, while comorbidity was associated with severe stress. Moreover, the mean scores of anxiety and depression were significantly higher among workers with inadequate training in infection control, whereas the mean anxiety score alone was significantly higher among females.
Regarding perception of COVID-19, more than half of the participants were not confident on the provision of PPE. More than one third felt stressed at work, and stigmatised by the general population due to the risk of spreading the infection.
Recommendations
Medical practitioners at the forefront in the fight against the virus should undergo psychological evaluations. The development of psychological issues among medical practitioners poses a threat in the fight against COVID-19 by reducing the effectiveness of medical personnel, and should therefore be addressed urgently.
Source of funding
Author declares that this research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Conflict of interest
The authors have no conflict of interest to declare.
Ethical approval
Ethical approval was obtained from the research administration, Ministry of Health, Almadinah Almunawwarah [IRB 433-19/08/1441 H, dated 13th April, 2020].
Authors contributions
AMS conceptualized the idea of research based on the topic's importance and relevance, and contributed in the literature search, provided research materials, collected and organized data and references, and provided logistic support. FAM identified the appropriate methods of analysis, interpreted the results of study, and wrote the final draft of the article. AAA helped in enriching references, and writing the study discussion. All the authors have critically reviewed and approved the final draft, and are responsible for the content and similarity index of the manuscript.
Acknowledgment
The authors are grateful to all the study participants for providing valuable information during the COVID -19 pandemic.
Footnotes
Presentation at a meeting: This is the first time the search is displayed
Peer review under responsibility of Taibah University.
References
- 1.Cassell G.H., Mekalanos J. Development of antimicrobial agents in the era of new and reemerging infectious diseases and increasing antibiotic resistance. J Am Med Assoc. 2001;285:601–605. doi: 10.1001/jama.285.5.601. [DOI] [PubMed] [Google Scholar]
- 2.World Health Organization . WHO; Geneva (CH): 2004. The World Health Report 2004—changing history: deaths by cause, sex and mortality stratum in WHO regions, estimates for 2002. [Google Scholar]
- 3.World Health Organization . WHO; Geneva (CH): 1999. The world health report on infectious disease. [Google Scholar]
- 4.Statement on the second meeting of the International Health Regulations (2005) Emergency Committee regarding the outbreak of novel coronavirus (2019-nCoV). World Health Organization. Director-General's remarks at the media briefing on 2019-nCoV on 11 February 2020. https://www.who.int/dg/speeches/detail/who-director-general-s-remarks-at-the-media-briefing-on-2019-ncov-on-11-february-2020.
- 5.WHO Director-General’s opening remarks at the media briefing on COVID-19. 3 March 2020. https://www.who.int/dg/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---3-march-2020 [Google Scholar]
- 6.Shanafelt T., Ripp J., Trockel M. Understanding and addressing sources of anxiety among health care professionals during the COVID-19 pandemic. J Am Med Assoc. 2020 Apr 07 doi: 10.1001/jama.2020.5893. Epub. [DOI] [PubMed] [Google Scholar]
- 7.Lai J., Ma S., Wang Y., Cai Z., Hu J., Wei N. Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019. JAMA Netw Open. 2020;3(3) doi: 10.1001/jamanetworkopen.2020.3976. Published 2020 Mar 2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Tan B.Y., Chew N.W., Lee G.K., Jing M., Goh Y., Yeo L.L. Psychological impact of the COVID-19 pandemic on health care workers in Singapore. Ann Intern Med. 2020:M20–M1083. doi: 10.7326/M20-1083. ooo. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chua S.E., Cheung V., McAlonan G.M., Cheung C., Wong J.W., Cheung E.P. Stress and psychological impact on SARS patients during the outbreak. Can J Psychiatr. 2004;49:385–390. doi: 10.1177/070674370404900607. [DOI] [PubMed] [Google Scholar]
- 10.Tam C.W., Pang E.P., Lam L.C., Chiu H.F. Severe acute respiratory syndrome (SARS) in Hong Kong in 2003: stress and psychological impact among frontline healthcare workers. Psychol Med. 2004;34(7):1197–1204. doi: 10.1017/s0033291704002247. [DOI] [PubMed] [Google Scholar]
- 11.Lee S.M., Kang W.S., Cho A.R., Kim T., Park J.K. Psychological impact of the 2015 MERS outbreak on hospital workers and quarantined hemodialysis patients. Compr Psychiatr. 2018;87:123–127. doi: 10.1016/j.comppsych.2018.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lee A.M., Wong J.G., McAlonan G.M., Cheung V., Cheung C., Sham P.C. Stress and psychological distress among SARS survivors 1 Year after the outbreak. Can J Psychiatr. 2007;52(4):233–240. doi: 10.1177/070674370705200405. [DOI] [PubMed] [Google Scholar]
- 13.Kapfhammer H.P., Rothenhausler H.B., Krauseneck T., Stoll C., Schelling G. Posttraumatic stress disorder and health-related quality of life in long-term survivors of acute respiratory distress syndrome. Am J Psychiatr. 2004;161:45–52. doi: 10.1176/appi.ajp.161.1.45. [DOI] [PubMed] [Google Scholar]
- 14.Hamdan A.B., Alshammary S., Javison S., Tamani J., AlHarbi M. Burnout among healthcare providers in a comprehensive cancer center in Saudi Arabia. Cureus. 2019 Jan;11(1) doi: 10.7759/cureus.3987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Maunder R.G., Lancee W.J., Balderson K.E., Bennett J.P., Borgundvaag B., Evans S. Long-term psychological and occupational effects of providing hospital healthcare during SARS outbreak. Emerg Infect Dis. 2006;12(12):1924–1932. doi: 10.3201/eid1212.060584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Xiao H., Zhang Y., Kong D., Li S., Yang N. The effects of social support on sleep quality of medical staff treating patients with coronavirus disease 2019 (COVID-19) in january and february 2020 in China. Med Sci Mon Int Med J Exp Clin Res. 2020;26 doi: 10.12659/MSM.923549. Published 2020 Mar 5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.AlAteeq D.A., Aljhani S., Althiyabi I., Majzoub S. Mental health among healthcare providers during coronavirus disease (COVID-19) outbreak in Saudi Arabia. J Infect Publ Health. 2020 Sep 10 doi: 10.1016/j.jiph.2020.08.013. S1876-0341(20)30635-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Gupta A.K., Mehra A., Niraula A., Kafle K., Deo S.P., Singh B. Prevalence of anxiety and depression among the healthcare workers in Nepal during the COVID-19 pandemic. Asian J Psychiatr. 2020 Jun;54:102260. doi: 10.1016/j.ajp.2020.102260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kang L., Li Y., Hu S., Chen M., Yang C., Yang B. The mental health of medical workers in Wuhan, China dealing with the 2019 novel coronavirus. Lancet Psychiatr. 2020;7:E14. doi: 10.1016/S2215-0366(20)30047-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Li S., Wang Y., Xue J., Zhao N., Zhu T. The impact of COVID-19 epidemic declaration on psychological consequences: a study on active Weibo users. Int J Environ Res Publ Health. 2020;17(6):2032. doi: 10.3390/ijerph17062032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Torales J., O'Higgins M., Castaldelli-Maia J.M., Ventriglio A. The outbreak of COVID-19 coronavirus and its impact on global mental health. Int J Soc Psychiatr. 2020;66(4):317–320. doi: 10.1177/0020764020915212. [DOI] [PubMed] [Google Scholar]