Abstract
Crimean-Congo hemorrhagic fever virus is a tick-borne bunyavirus of the Nairovirus genus that causes hemorrhagic fever in humans with high case fatality. Here, we report the development of subunit vaccines and their efficacy in signal transducer and activator of transcription 1 (STAT1) knockout mice. Ectodomains of the structural glycoproteins Gn and Gc were produced using a Drosophila insect cell–based expression system. A single vaccination of STAT129 mice with adjuvanted Gn or Gc ectodomains induced neutralizing antibody responses, which were boosted by a second vaccination. Despite these antibody responses, mice were not protected from a CCHFV challenge infection. These results suggest that neutralizing antibodies against CCHFV do not correlate with protection of STAT1 knockout mice.
Key Words: : Crimean–Congo hemorrhagic fever virus, Bunyavirus, Nairovirus, Vaccine, Neutralizing antibodies, Gn, Gc, STAT1, STAT129
Introduction
Crimean-Congo hemorrhagic fever virus (CCHFV) is a member of the Nairovirus genus within the family Bunyaviridae. The virus is transmitted among mammals by ixodid (hard) ticks, predominantly of the species Hyalomma marginatum. Humans can become infected via tick bite, crushing of engorged ticks, via contact with bodily fluids in a nosocomial setting, or via contact with blood or tissues of infected animals. CCHFV can cause a hemorrhagic syndrome in humans with mortality rates as high as 70%, whereas animal hosts show no overt signs of disease. Before the year 2000, CCHFV was associated with human disease in the Soviet Union, Bulgaria, and South Africa, whereas in more recent years, the virus has emerged in the Balkans, southwest Russia, the Middle East, and Turkey (Bente et al. 2013). No internationally approved vaccine or therapeutic is available.
In 1970, a vaccine became available in the former USSR that is based on aluminum hydroxide–adjuvanted formalin-inactivated mouse brain (Tkachenko et al. 1970, 1971). Since 1974, this vaccine has been used to protect military and medical personnel, farmers, and people residing in CCHFV endemic areas. Over a period of 21 years following the use of this vaccine in Bulgaria, a four-fold reduction in the number of reported CCHF cases was observed, although this observation cannot be ascribed with certainty to the use of the vaccine (Christova et al. 2010). In 2012, the potency of the vaccine was evaluated in healthy human volunteers. This study demonstrated that a single vaccination elicits low neutralizing antibody and cellular immune responses and that three booster vaccinations may be required to achieve protective immunity. The seemingly weak immunogenicity of the inactivated vaccine, together with the difficulty in preparing the vaccine from mouse brain in high biocontainment facilities, explains the need for a next-generation CCHF vaccine.
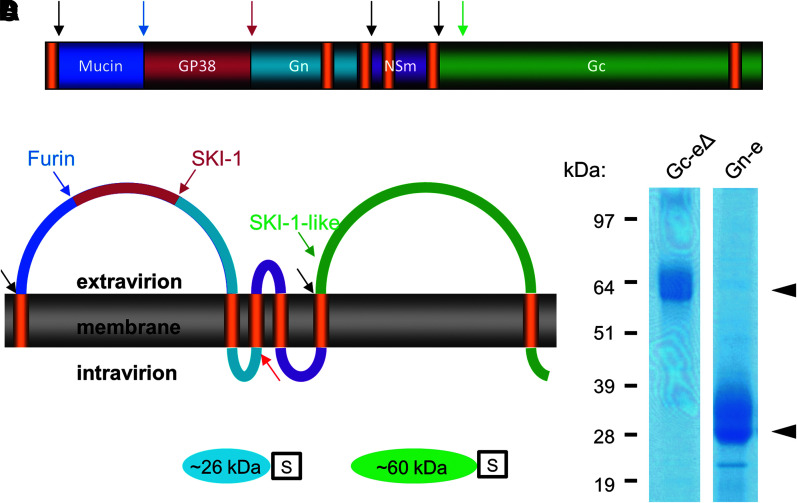
Like other members of the Bunyaviridae family, the CCHFV genome comprises a large (L), medium (M), and small (S) segment. The L and S segments encode the polymerase protein and nucleocapsid protein, respectively, that function together in genome replication and transcription. The M segment of the virus encodes an unusually large glycoprotein precursor (GPC) protein that is processed into seven proteins, of which the structural glycoproteins Gn and Gc comprise the outer surface of the virion (Fig. 1A, B; Sanchez et al. 2006). These surface glycoproteins are considered promising vaccine candidates because both were previously shown to be targets of neutralizing antibodies (Bertolotti-Ciarlet et al. 2005).
FIG. 1.
Topology of the Crimean–Congo hemorrhagic fever virus (CCHFV) glycoprotein precursor protein and production of Gn and Gc ectodomains. The putative topology of the CCHFV glycoprotein precursor and the proteases involved in co-translational processing are depicted (A and B). Protease cleavage sites are depicted. (Black arrows) Signalase cleavage sites; (red arrow) cleavage by a yet unknown protease. Genes encoding the Gn or Gc ectodomains, each carboxy-terminally fused to a sequence encoding a triple Strep-Tag (S) (C), were expressed in Drosophila S2 cells, purified by Strep-Tactin sepharose columns, and analyzed by sodium dodecyl sulfate polyacrylamide gel electrophoresis (SDS-PAGE) (D). Gn-eΔ, Gc ectodomain of improved solubility; Gn-e, Gc ectodomain.
The first approach to developing a next-generation CCHF vaccine was reported in 2006. In this work, a DNA vaccine was developed that was shown to induce neutralizing antibodies in a subset of mice after three gene gun vaccinations (Spik et al. 2006). In another approach, the viral structural glycoproteins were expressed in tobacco plants. Mice feeding on the leaves of these plants developed CCHFV-specific serum immunoglobulin A (IgA) and IgG antibodies, although the neutralizing capacity of these antibodies was not evaluated (Ghiasi et al. 2011). The establishment of mouse models using adult immunocompromised mice deficient for either the signal transducer and activator of transcription 1 (STAT1) signaling molecule (Bente et al. 2010, Bowick et al. 2012) or the type I interferon receptor (Bereczky et al. 2010, Zivcec et al. 2013) now enables evaluation of the efficacy of candidate vaccines. The latter model was recently used to evaluate the efficacy of a Modified Vaccinia Ankara (MVA)-based vaccine (Buttigieg et al. 2014). The MVA vector was designed to express the complete GPC gene and was shown to induce GPC-specific cellular and humoral immune responses. After a homologous prime-boost vaccination, all type I interferon receptor knockout mice were fully protected from a lethal challenge dose (Buttigieg et al. 2014).
We here report the development of CCHF candidate subunit vaccines using a Drosophila insect cell–based expression system that was previously used successfully to develop candidate vaccines for the control of Rift Valley fever (de Boer et al. 2010). The efficacies of the experimental CCHF vaccines were evaluated in STAT1 knockout mice. Our results demonstrate that the vaccines induce high neutralizing antibody responses after a prime-boost vaccination, but that these responses do not correlate with protection.
Materials and Methods
Virus and cells
CCHFV strain IbAr10200 was provided by Dr. Thomas Ksiazek (University of Texas Medical Branch, Galveston, TX). The IbAr10200 virus was previously passaged 10 times in suckling mouse brain and three times in SW-13 cells. The titer was determined at 1.2 × 106 plaque-forming units (pfu)/mL. SW-13 cells (American Type Culture Collection [ATCC] #CCL-105) were maintained in L-15 medium containing 10% heat-inactivated fetal bovine serum (FBS), 100 mM L-glutamine, 50 U/mL penicillin, and 50 μg/mL streptomycin (all from Sigma, St. Louis, MO). The virus stock and inocula tested negative for pyrogen contamination using the PYROGENT Plus Test Kit (Lonza, Wakersville, MD).
Plasmid construction
Constructs for expression of genes in Drosophila Schneider 2 (S2) cells were based on the plasmid pMT/BiP/V5-HisA (Invitrogen, Carlsbad, CA). CCHFV sequences were derived from the M segment of CCHFV strain IbAr10200 (National Center for Biotechnology Information [NCBI] acc. no. AF467768). Gene synthesis and codon-optimization for optimal expression in insect cells was performed by the GenScript Corporation (Piscataway, NJ). For expression of the Gn ectodomain, a construct was designed that encodes amino acids 520–694 of the GPC, fused at the amino terminus to the BiP signal sequence, and fused at the carboxyl terminus to a FLAG-tag (DYKDDDDK) followed by three Strep-tags (WSHPQFEK), each separated by a glycine linker (GGGSGGGSGGGS). The triple Strep-tag was included to allow purification with Strep-Tactin Magnetic Beads (IBA GmbH). Two similar constructs were designed for expression of the Gc ectodomain, the first encoding amino acids 1041–1596 of the GPC and the second encoding amino acids 1041–1579. These proteins were named Gc ectodomain (Gc-e) and Gc ectodomain of improved solubility (Gc-eΔ), respectively.
Expression and purification of the CCHFV Gn and Gc ectodomains
Plasmids pMT-Gn, pMT-Gc-e, and pMT-Gc-eΔ were each co-transfected into S2 cells with the blasticidin resistance vector pCoBlast (Invitrogen) at a ratio of 19:1 using Cellfectin II Transfection Reagent (Invitrogen). Stably transformed cells were selected in serum-free InsectXpress Medium (Lonza, Westburg, Leusden, The Netherlands) containing 25 μg/mL blasticidin (Invitrogen) and maintained in culture medium containing 10 μg/mL blasticidin. For protein expression, cells were seeded at a density of 1.6 × 107 cells/mL in T150 flasks and induced by addition of copper sulfate (500 μM) to the culture medium. After incubation of 8–9 days at 28°C, supernatant was collected and stored at 4°C until protein purification. When required, cells were reseeded for a second induction.
Due to poor yield and solubility of the Gc-e protein, supernatant containing this protein was concentrated 10× using 30-kDa Amicon filters (Millipore) to obtain sufficient protein for vaccination of mice. In contrast, the Gc-eΔ and Gn-e proteins were highly soluble and could be purified efficiently using Strep-Tactin® Superflow® High-Capacity cartridges with a 1-mL bed volume (IBA GmbH) and an ÅKTA fast protein liquid chromatography (FPLC) purification system. Before loading onto the columns, the culture medium was incubated with avidin to prevent binding of contaminating biotinylated proteins. After 40 min incubation at 37°C with 25 μg/mL avidin, supernatants were cleared by slow-speed centrifugation. Purification was performed according to the instructions of the manufacturer (IBA GmbH).
To determine protein yields, samples were mixed with Laemmli sample buffer and loaded onto 4–12% NuPAGE gels. Proteins were visualized with GelCode Blue (Pierce) and protein concentrations were determined using a bovine serum albumin (BSA) standard.
Vaccination and challenge of mice
Female 4- to 6-week-old 129S6/SvEv-Stat1tm1Rds mice (STAT129, Taconic, Germantown, NY) were randomized and implanted with subdermal ID transponders to monitor body temperatures (Biomedic Data Solutions, Seaford, DE). CCHFV proteins were formulated with the Sigma Adjuvant System according to the instructions of the manufacturer (Sigma). Animals were kept under sterile barrier conditions in environmentally enriched ventilated cages (Tecniplast, Italy) with sterile food and water provided ad libitum.
In the first experiment, a group of five mice was vaccinated via the intraperitoneal route with a volume of 200 μL (100 μL in each of two caudal abdominal quadrants) containing 1.4 μg Gc-e on days 0 and 21. One group of mice (n = 5) received adjuvant only. Serum was collected by retro-orbital bleeds 3 weeks after the second vaccination and evaluated for the presence of neutralizing antibodies. On day 35, the mice were moved into the biosafety level 4 (BSL4) laboratory and allowed to acclimate for 7 days before challenge. On day 42, mice were challenged intraperitoneally with 100 pfu CCHFV strain IbAr10200 in a volume of 100 μL, which was expected to result in death of mock-vaccinated mice after 3–5 days (Bente et al. 2013).
In the second experiment, groups of 10 mice were vaccinated with a volume of 200 μL (100 μL in each of two caudal abdominal quadrants), containing 7.5 μg purified Gc-eΔ or 15 μg Gn-e per mouse on days 0 and 21. One group of five mice was inoculated with adjuvant only. On day 35, the mice were moved into the BSL4 laboratory and allowed to acclimate for 7 days until subcutaneous challenge (day 42). The titer and volume of the challenge inoculum were identical as in the first experiment. Blood samples were collected by retro-orbital bleed on days 0, 21, and 42 and serum was separated by centrifugation.
All animal work was reviewed and approved by the Institutional Animal Care and Use Committee and Institutional Biosafety Committee of the University of Texas Medical Branch.
Virus neutralization test
Fifty microliters of L-15 medium containing 5% FBS, 1% l-glutamine, and 1% penicillin-streptomycin was added to each well of a 96-well plate. Subsequently, 50 μL of prediluted mouse sera (1:5) was added to the first row and diluted by two-fold dilution steps. Next, 50 μL of diluted CCHFV stock (103 50% tissue culture infective dose [TCID50]/mL) was added to each well, after which the plates were incubated at room temperature for 2 h. Consequently, 50 μL of SW-13 cell suspension containing 800,000 cells/mL was added to each well, resulting in 40,000 cells per well. Plates were sealed and placed in an incubator at 37°C. After 4 days, plates were stained with Crystal Violet in 10% buffered formalin and 80% end-point titers determined using the Spearman–Kärber method.
Results
Production and vaccine efficacy of the Gc ectodomain
A Drosophila Schneider 2 (S2) cell line stably expressing Gc-e was readily created. However, analysis of supernatant by polyacrylamide gel electrophoresis (PAGE) demonstrated that the Gc-e protein was of low yield and poorly soluble. Accordingly, detection of the protein on polyacrylamide gels required preincubation of culture medium with 1% Triton X-100 (data not shown). Protein concentrations were determined using a BSA standard. To obtain sufficient Gc-e protein for vaccination, culture supernatant was concentrated using Amicon filters (Millipore).
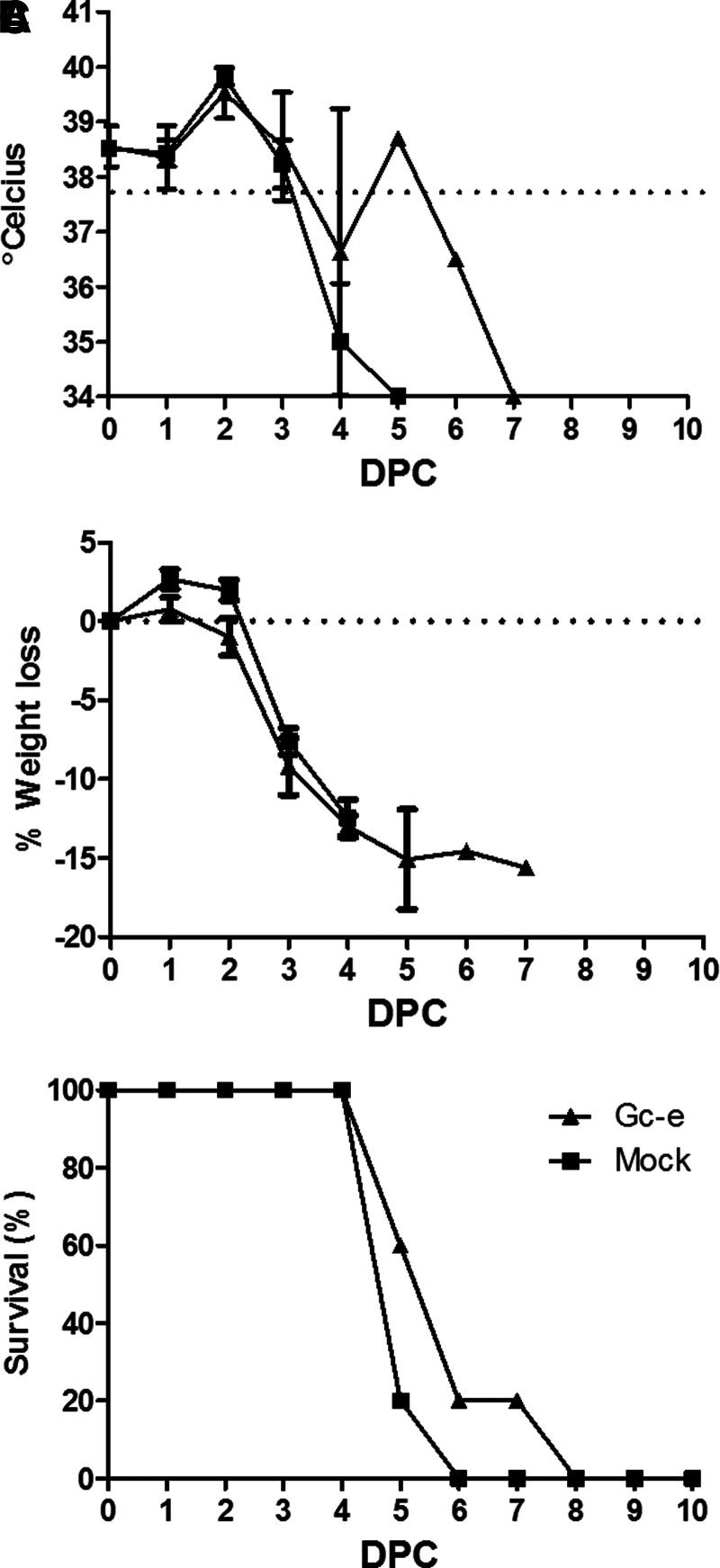
Prime-boost vaccination of STAT129 mice (n = 5) with a 1.4-μg Gc-e/dose resulted in an average 80% end-point titer of 333, whereas no neutralizing antibodies were detected in mice inoculated with adjuvant only. To our surprise, despite the presence of neutralizing antibodies, intraperitoneal challenge of the vaccinated mice resulted in elevated temperatures on 2 days postinfection (dpi), hypothermia on 4 dpi, and significant weight loss (>10%) as previously described for CCHFV challenge of naïve STAT129 mice (Bente et al. 2010), and all mice succumbed to the infection (Fig. 2).
FIG. 2.
Vaccination with the Gc ectodomain is not protective in a lethal Crimean–Congo hemorrhagic fever (CCHF) challenge model. STAT129 mice (n = 5/group) were vaccinated via the intraperitoneal route two times, with a 3-week interval, with purified Gc ectodomain (Gc-e) formulated with the Sigma Adjuvant System or with adjuvant only (mock). Mice were challenged 3 weeks after the second vaccination with Crimean–Congo hemorrhagic fever virus (CCHFV) strain IbAr10200 via the intraperitoneal route. Body temperatures (A), % weight loss (B), and % survival (C) are depicted. Error bars represent standard error (SE). DPC, days postinfection.
Production and vaccine efficacy of a Gc ectodomain of improved solubility and the Gn ectodomain
The absence of any vaccine-mediated protection in the face of neutralizing antibody responses led us to suggest that intraperitoneal challenge may be too intense in this model to evaluate the efficacy of candidate subunit vaccines. To elucidate if the neutralizing antibodies would protect against a less rigorous virus challenge, we decided to perform another vaccination experiment in which mice are challenged via the subcutaneous route, which leads to a later onset of disease and only occasionally results in mortality (Bente, unpublished observation). Because uniform lethality cannot be used as a read-out in this model, efficacy was assessed by monitoring temperature, weight loss, and clinical signs. To improve the solubility of the Gc ectodomain and thereby facilitate production of a new vaccine batch, we truncated the protein by 17 carboxy-terminal amino acids, corresponding to the membrane-proximal stem region (FFYGLKNMLSGIFGNVF). Considering that antibodies against Gn can also be protective (Bertolotti-Ciarlet et al. 2005), a cell line constitutively producing the Gn ectodomain (Gn-e, amino acids 520–694 of the M segment open reading frame [ORF]) was also developed. The resulting Gc-eΔ and Gn-e proteins were found to be highly soluble and could be purified efficiently from the culture medium using Strep-Tactin beads by virtue of a carboxy-terminally added triple Strep-Tags. Proteins were detected with GelCode Blue (Pierce), and protein concentrations were determined using a BSA standard. Purified Gn-e and Gc-eΔ proteins migrated at the ∼26-kD and ∼60-kD positions, respectively, in NuPAGE gels (Fig. 1C, D).
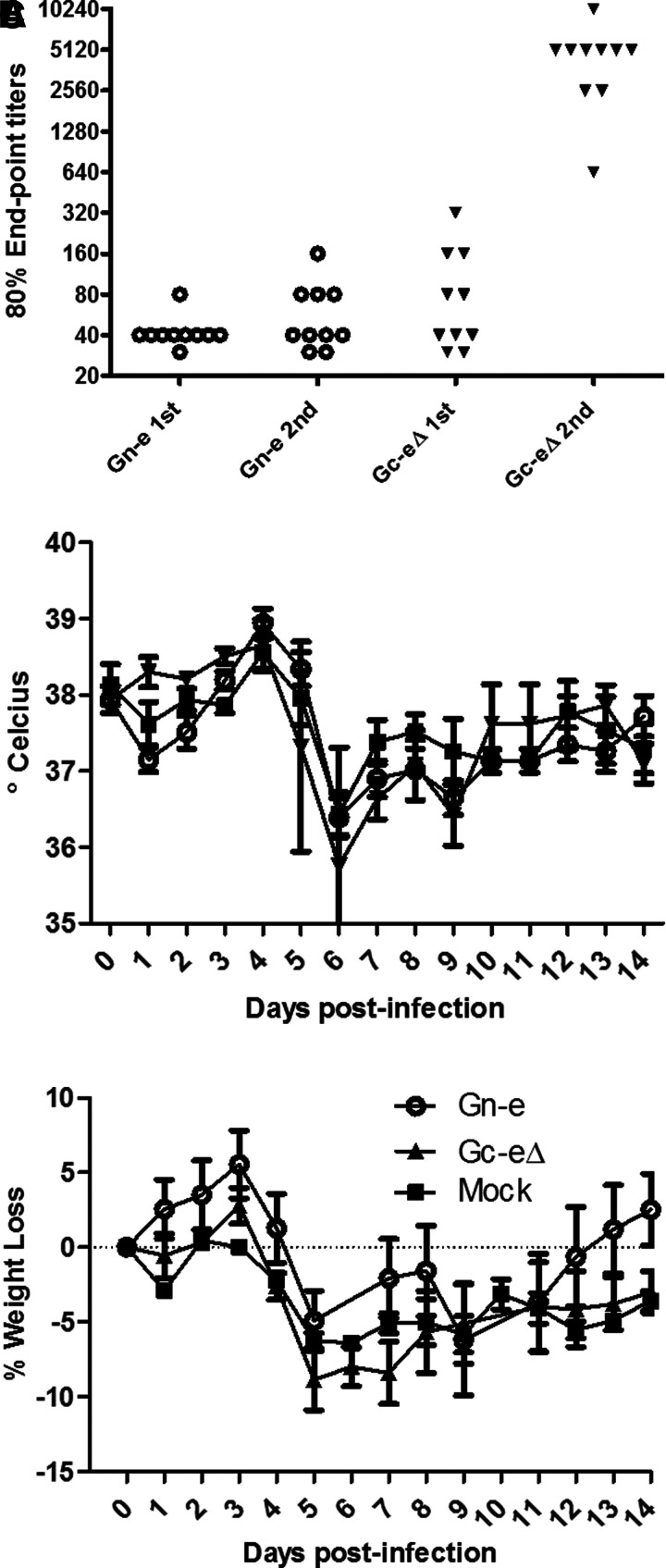
Serum was collected 3 weeks after the first and second vaccinations and evaluated for the presence of neutralizing antibodies. All sera were found to contain neutralizing antibodies at 3 weeks after the first vaccination, and antibody levels were boosted by the second vaccination (Fig. 3A). Whereas Gn-specific antibody levels increased from an mean 80% end-point titer of 40–62, mean Gc-specific neutralizing antibody titers increased from 98 to 5120. This result suggests that the Gc-e formulation was most immunogenic. Mice were challenged 3 weeks after the second vaccination with CCHFV strain IbAr10200. All mice displayed rises and subsequent drops in body temperatures (Fig. 3A) as well as significant weight loss (Fig. 3B) and clinical signs (data not shown) similar to the mock control group, demonstrating that vaccination did not change the clinical course of the infection. One of the Gc-e-vaccinated mice reached the previously defined humane end point (Bente et al. 2010) on day 6 postinfection and was euthanized by cervical dislocation after inhalation of isoflurane. Even in this less severe challenge model, vaccination with the candidate subunit vaccines did not protect from disease.
FIG. 3.
Vaccination mice with Gc and Gn ectodomains does not protect mice from a sublethal Crimean–Congo hemorrhagic fever virus (CCHFV) infection. Mice were vaccinated via the intraperitoneal route two times, with a 3-week interval, with purified Gn ectodomain (Gn-e) or Gc ectodomain lacking the stem region (Gc-eΔ), formulated with the Sigma Adjuvant System. Virus neutralization tests were performed on individual sera collected 3 weeks after the second immunization. The results are depicted as 80% end-point titers (n = 10). Titers were calculated using the Spearman–Kärber method (A). Mice were challenged 3 weeks after the second vaccination with CCHFV strain IbAr10200 via the subcutaneous route. Body temperatures (B) and % weight loss (C) are depicted. Error bars represent standard error (SE). Gn-eΔ, Gc ectodomain of improved solubility; Gn-e, Gc ectodomain.
Discussion
Structural glycoproteins of bunyaviruses are the targets for neutralizing antibodies and are therefore preferred candidates for subunit vaccine development (Pekosz et al. 1995, de Boer et al. 2010, Brown et al. 2011). Previous studies on monoclonal antibodies (mAbs) capable of neutralizing CCHFV have, however, suggested that the correlation between neutralization and protection is complex. Comprehensive studies on CCHFV neutralization were performed by Bertolotti-Ciarlet and co-workers, who demonstrated that Gc is the dominant target for neutralizing antibodies (Bertolotti-Ciarlet et al. 2005). Surprisingly, some of these Gc-specific neutralizing mAbs were relatively poorly protective in suckling mice. These authors also demonstrated that antibodies against Gn were generally more protective, even though these antibodies did not neutralize infectivity of the virus on SW-13 cells. The imperfect correlation between neutralization and protection, as observed in these previous studies as well as in the current work, can be explained by a mechanistic difference between virus infection in vitro and in vivo.
The recently published study of Buttigieg and co-workers demonstrated that a prime homologous boost with an MVA vector expressing the CCHFV GPC (MVA-GP) fully protects type I interferon receptor knockout mice from a lethal challenge dose (Buttigieg et al. 2014). Vaccination was shown to induce both cellular and humoral immune responses, although neutralizing activity of the antibodies was not reported. It is important to note that not all vaccinated and subsequently challenged mice developed a detectable antibody response, suggesting that protection did not correlate with antibodies. Although further studies are required to firmly establish correlates of protection from CCHFV infection, the combined results of our work and those of Buttigieg underscore the previous conclusion of Bertolotti-Ciarlet that there is an imperfect correlation between neutralization and protection from CCHFV infection, at least in sucking mice and adult mice with defective interferon response pathways.
Despite the absence of type I and II interferon function, STAT129 mice were shown to develop strong adaptive immune responses to virus infections (Vancott et al. 2003, Franceschi et al. 2015) or vaccination with experimental subunit vaccines (Vancott et al. 2003, Raymond et al. 2011). Although this suggests that the model is suitable for the evaluation of candidate vaccines, the high susceptibility of STAT129 mice to virus infection may result in undervaluing the vaccine potential of experimental vaccines. Therefore, it is important to continue efforts to develop alternative CCHF animal models that can be used to evaluate the efficacy of glycoprotein-based subunit vaccines.
Acknowledgments
We thank Karel Riepema for assisting with the ÅKTA FPLC purification system. This work was performed under the umbrella of the Castellum program, which is financed by the Dutch Ministry of Economic Affairs. D.A.B. received funding from a Western Regional Center of Excellence for Biodefense and Emerging Infectious Diseases Research (WRCE) Development grant.
Author Disclosure Statement
No competing financial interests exist.
References
- Bente DA, Alimonti JB, Shieh WJ, Camus G, et al. Pathogenesis and immune response of Crimean-Congo hemorrhagic fever virus in a STAT-1 knockout mouse model. J Virol 2010; 84:11089–11100 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bente DA, Forrester NL, Watts DM, McAuley AJ, et al. Crimean-Congo hemorrhagic fever: History, epidemiology, pathogenesis, clinical syndrome and genetic diversity. Antiviral Res 2013; 100:159–189 [DOI] [PubMed] [Google Scholar]
- Bereczky S, Lindegren G, Karlberg H, Akerstrom S, et al. Crimean-Congo hemorrhagic fever virus infection is lethal for adult type I interferon receptor-knockout mice. J Gen Virol 2010; 91:1473–1477 [DOI] [PubMed] [Google Scholar]
- Bertolotti-Ciarlet A, Smith J, Strecker K, Paragas J, et al. Cellular localization and antigenic characterization of Crimean-Congo hemorrhagic fever virus glycoproteins. J Virol 2005; 79:6152–6161 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bowick GC, Airo AM, Bente DA. Expression of interferon-induced antiviral genes is delayed in a STAT1 knockout mouse model of Crimean-Congo hemorrhagic fever. Virol J 2012; 9:122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown KS, Safronetz D, Marzi A, Ebihara H, et al. Vesicular stomatitis virus-based vaccine protects hamsters against lethal challenge with Andes virus. J Virol 2011; 85:12781–12791 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buttigieg KR, Dowall SD, Findlay-Wilson S, Miloszewska A, et al. A novel vaccine against Crimean-Congo haemorrhagic fever protects 100% of animals against lethal challenge in a mouse model. PLoS One 2014; 9:e91516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Christova I, Kovacheva O, Georgieva G, Ivanova S, et al. Vaccine against Crimean-Congo haemorrhagic fever virus—Bulgarian input in fighting the disease. Problems of Infectious Parasitic Diseases 2010; 37:7–8 [Google Scholar]
- de Boer SM, Kortekaas J, Antonis AF, Kant J, et al. Rift Valley fever virus subunit vaccines confer complete protection against a lethal virus challenge. Vaccine 2010; 28:2330–2339 [DOI] [PubMed] [Google Scholar]
- Franceschi V, Parker S, Jacca S, Crump RW, et al. BoHV-4-based vector single heterologous antigen delivery protects STAT1(−/−) mice from monkeypoxvirus lethal challenge. PLoS Negl Trop Dis 2015; 9:e0003850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ghiasi SM, Salmanian AH, Chinikar S, Zakeri S. Mice orally immunized with a transgenic plant expressing the glycoprotein of Crimean-Congo hemorrhagic fever virus. Clin Vaccine Immunol 2011; 18:2031–2037 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pekosz A, Griot C, Stillmock K, Nathanson N, et al. Protection from La Crosse virus encephalitis with recombinant glycoproteins: Role of neutralizing anti-G1 antibodies. J Virol 1995; 69:3475–3481 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Raymond J, Bradfute S, Bray M. Filovirus infection of STAT-1 knockout mice. J Infect Dis 2011; 204(Suppl 3):S986–S990 [DOI] [PubMed] [Google Scholar]
- Sanchez AJ, Vincent MJ, Erickson BR, Nichol ST. Crimean-Congo hemorrhagic fever virus glycoprotein precursor is cleaved by furin-like and SKI-1 proteases to generate a novel 28-kilodalton glycoprotein. J Virol 2006; 80:514–525 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spik K, Shurtleff A, McElroy AK, Guttieri MC, et al. Immunogenicity of combination DNA vaccines for Rift Valley fever virus, tick-borne encephalitis virus, Hantaan virus, and Crimean Congo hemorrhagic fever virus. Vaccine 2006; 24:4657–4666 [DOI] [PubMed] [Google Scholar]
- Tkachenko EA, Butenko AM, Butenko SA, Zaradova TI, et al. Prophylactic characteristics of a protective Crimean hemorrhagic fever vaccine. In: Chumakov MP, ed. Crimean Hemorrhagic Fever—Materials of the 3rd Scientific-Practical Conference in Rostov-na-donu Region. USSR, Moscow, 1970:136–138. [Google Scholar]
- Tkachenko EA, Butenko AM, Badalov MY, Zaradova TI, et al. Investigation of immunogenic activity of killed brain vaccine against Crimean hemorrhagic fevers. In: Chumakov MP, ed. Viral Hemorrhagic Fevers. Moscow, USSR: Trudi Instituta Poliomielita i Virusnykh Entsefalitov, USSR Adademy of Medical Sciences, 1971:119–129 [Google Scholar]
- Vancott JL, McNeal MM, Choi AH, Ward RL. The role of interferons in rotavirus infections and protection. J Interferon Cytokine Res 2003; 23:163–170 [DOI] [PubMed] [Google Scholar]
- Zivcec M, Safronetz D, Scott D, Robertson S, et al. Lethal Crimean-Congo hemorrhagic fever virus infection in interferon alpha/beta receptor knockout mice is associated with high viral loads, proinflammatory responses, and coagulopathy. J Infect Dis 2013; 207:1909–1921 [DOI] [PMC free article] [PubMed] [Google Scholar]