Abstract
This study aimed to explore B-cell lymphoma cells’ proliferation and apoptosis under targeted regulation of FOXO3 by miR-155. We analyzed the differences between B-cell lymphoma cells and B lymphocytes in expressions of miR-155 and FOXO3, explored the effects of miR-155 on proliferation and apoptosis of B-cell lymphoma cells, and relevant mechanisms, and also analyzed the relationship between expressions of miR-155 and FOXO3 in 42 patients with diffuse large B-cell lymphoma (DLBCL) and clinical characteristics of them. B-cell lymphoma cells showed a higher expression of miR-155 and a low expression of FOXO3 than B lymphocytes (both P<0.05). B-cell lymphoma cells transfected with miR-155-inhibitor showed significantly decreased expression of miR-155, significantly weakened cell proliferation ability, and increased cell apoptosis rate (all P<0.05), and they also showed upregulated expression of FOXO3 (P<0.05). Dual-luciferase reporter assay revealed that there were targeted binding sites between miR-155 and FOXO3. Compared with B-cell lymphoma cells transfected with miR-155-inhibitor alone, those with co-transfection showed lower expression of FOXO3, higher proliferation and lower cell apoptosis rate (all P<0.05). The expression of miR-155 in DLBCL tissues was higher than that in tumor-adjacent tissues (P<0.05), and the expressions of miR-155 and FOXO3 were closely related to the international prognostic index (IPI) and the 5-year prognosis and survival of the patients (P<0.05). miR-155 can promote the proliferation of B-cell lymphoma cells and suppress apoptosis of them by targeted inhibition of FOCXO3, and both over-expression of miR-155 and low expression of FOXO3 are related to poor prognosis of DLBCL patients.
Keywords: miR-155, FOXO3, B-cell lymphoma, Proliferation, Apoptosis, Clinical characteristics
Introduction
B-cell lymphoma is a lymphoma from B cells, including Hodgkin’s lymphoma and non-Hodgkin’s lymphoma.1 Non-Hodgkin’s lymphoma accounts for about 3/4 of all B-cell lymphomas, and the most common non-Hodgkin’s lymphoma is diffuse large B-cell lymphoma (DLBCL), which accounts for about 30%–40% of non-Hodgkin’s lymphoma and shows an incidence increasing at a rate of 3% per year.2,3 Although therapeutic regimens for DLBCL have made significant progress, DLBCL patients’ prognosis is still not optimistic. For example, chemotherapy regimens based on anthracycline are only effective for 40%–50% of DLBC patients,4 so it is of great clinical significance to find a new therapeutic target.
miRNAs are a short-chain non-coding RNA with a length of about 20–24 nucleotides, which can inhibit the stability and translation of mRNA and thus regulate proteins’ expressions. miRNAs are abnormally expressed in nearly 400 human diseases, and it is of great significance to study the mechanism of miRNAs in the diagnosis and treatment of diseases.5,6 miR-155 is located in the exon 3 (21q21.3) of the B-cell integration cluster on human chromosome 21. In recent years, studies have reported that miR-155 is closely related to the occurrence and development of DLBCL. For example, a study by Zhang et al. found that miR-155 may affect the metastasis of DLBCL and prognosis of patients by regulating transcription factor forkhead box P3,7 and a study by Huang et al. also found that miR-155 promoted the growth of DLBCL cells by activating PI3K-AKT pathway through inhibiting endogenous PIK3R1.8 Forkhead-box class O transcription factor (FOXO) is an important tumor suppressor, which can inhibit tumor cell cycle progression and induce programmed death of tumor cells.9 FOXO3 is an essential member of the FOXO family, able to regulate the proliferation of immune cells such as B lymphocytes and T lymphocytes.10 Immune response disorder is an important factor inducting DLBCL,11 but there are few studies on FOXO3 in DLBCL. A study by Huang et al. pointed out that miR-155 could target FOXO3 to suppress apoptosis of monocytes,12 and Ling et al. also pointed out that miR-155 could target FOXO3 to regulate proliferation and invasion of gliomas13 and that may be another mechanism of miR-155 in DLBCL. This study explored B lymphocytes’ proliferation and apoptosis under targeted regulation of FOXO3 by miR-155 to find a new therapeutic target for DLBCL.
Materials and Methods
Cell culture
Human B-cell lymphoma cells DOHH2 and OCI-LY10 (BNCC338032 and BNCC337742) and human B lymphocyte AHH-1 (ATCC No. CRL-8146) were purchased from BeNa Culture Collection and ATCC core collection, respectively. AHH-1 was collected from the peripheral blood of a 33 years old human of Caucasian ethnicity. DOHH2 was cultured in 90% high-sugar Dulbecco’s modified eagle medium (DMEM) containing 4mmL of glutamine and sodium pyruvate and 10% fetal bovine serum (FBS), and AHH-1 and OCI-LY10 were cultured in 90% Roswell Park Memorial Institute-1640 (RPMI-1640) containing 10% FBS. The cells were all cultured under 95% air + 5% carbon dioxide at 37°C. The purchased cells were used after 2–3 times of passage. Cells at the logarithmic growth phase were collected and lysed with TRIzol lysate, and then the total RNA was extracted from the cells with chloroform, isopropanol, and ethanol in order. The purity, concentration, and integrity of the total RNA were determined using ultraviolet spectrophotometry and agarose gel electrophoresis. It was required that the ratio of these factors at 28s to these factors at 18s was larger than or equal to 2, and the ratio of A260/A280 was between 1.8 and 2.1.
Source of patients sample
The patients’ inclusion criteria were as follows: Patients confirmed based on histopathology, patients without other lymph node diseases, and patients with detailed case data and follow-up data. The researchers followed the Declaration of Helsinki. The patients’ exclusion criteria were as follows: patients with other tumors or history of tumors; patients with severe diseases in heart, brain, liver, kidney or vessel, or with a severe infection such as sepsis, pregnant women, or patients with cardiovascular diseases or hepatorenal diseases. This study was approved by the Ethics Committee of The First Affiliated Hospital of Fujian Medical University, and the patients and their families signed an informed consent form based on our consultation by telephone or letter. Tumor tissues and normal tumor-adjacent tissues were collected from the tissues of 42 DLBCL patients (30–80 years old) stored from March 2010 to May 2014. Total RNA was extracted using Qiazol reagent and RNAeasy Mini Kit (Qiagen, Hombrechtikon, Switzerland) according to the manufacturer’s instructions. Total RNA, 250 ng, was reverse transcribed, and the same RNA samples were used for qPCR, as described in the following section. For western blot, proteins from biopsy tissue were extracted using the RIPA lysis method. The total proteins’ concentration was determined using the BCA method and adjusted to 4μg/μL.
Main reagents and instruments
Lipofectamine TM2000 transfection kit (Invitrogen Company, United States, item number: 35050); TRIzol kit (Invitrogen Company, United States, item number: 15596018); EasyScript One-Step RT-PCR SuperMix kit (Beijing TransGen Biotech, China, item number: AE411-02); RIPA kit, bicinchoninic acid (BCA) protein kit, and electrochemiluminescence (ECL) kit (Thermo Scientific™, item numbers: 89901, 23250, and 35055); rabbit anti-FOXO3 polyclonal antibody and goat anti-rabbit immunoglobulin G (IgG) secondary antibody (monoclonal antibody) (Abcam Company, United States, item numbers: ab58518 and ab6721); cell counting kit- 8 (CCK8) kit (Beijing Beyotime Biotechnology, China, item number: C0037); Annexin V-FITC/PI apoptosis determination kit (Invitrogen Company, United States, item number: V35113).
Construction of expression vectors and transfection
All expression vectors were designed by Thermo Fisher Scientific (China), and the expression vectors included FOXO3 low expression vector (si-FOXO3), the miR-155 low expression vector (miR-155-inhibitor), miR-155 over-expression vector (miR-155-mimic), blank vector miR-NC, blank vector si-NC, pMiR-miR-155- 3UTR wild type (Wt), pMiR- miR-155-3UTR Mutant type (Mut) and blank vector pMiR-NC. Cells at the logarithmic growth phase were collected, digested with trypsin, and then resuspended. Subsequently, the cells were seeded into a 96-well plate and transfected with expression vectors when the fusion degree was up to about 80%. The specific operation steps were carried out by referring to the instructions of the kit. The cells were cultured in an incubator with 5% CO2 at 37°C for 48h, and the culture medium was replaced every 6h. Quantitative real-time polymerase chain reaction (qRT-PCR) and Western blot assay were employed to analyze the transfection results. Cells that did not receive any intervention were taken as a blank group.
qRT-PCR
This study carried out one-step RNA amplification in a total of 20μl of total reaction volume containing 1μg of RNA Template, 0.4μl of Forward GSP (10μM), 0.4μl of Reverse GSP (10μM), 10μl of 2*One-Step Reaction Mix, 0.4μl of EasyScript One-Step Enzyme Mix, and RNase-free water to adjust the volume. The reaction conditions were as follows: 40°C for 30 min, 94°C for 5 min, 94°C for 30 s, 60°C for 30 s, 72°C at 2kb/min, 72°C for 10 min, a total of 42 cycles. In order to normalize the target and target gene expression, U6 was used as an internal reference gene control. The data collected was analyzed as per 2− ΔΔCt method and expressed as folds over experimental control groups. These experiments were performed in three biological replicates. The primer sequences are shown in Table 1.
Table 1.
Primer sequences.
| miR-155 | FW 5′-TTAATGCTAATC-GTGATAG-3′ |
| RW 5′-ACCTGAGAGTAGACCAGA-3′ | |
| U6 | FW 5′-GCGCGTCGTGAAGCGTTC-3′ |
| RW 5′-GTGCAGGGTCCGAGGT-3′ |
Western blot
The total protein concentration in each sample was determined using the BCA method and normalized to 4μg/μL. The total protein was separated through 12% polyacrylamide gel electrophoresis. The initial voltage was 90V, and then the voltage was increased to 120V to move the sample to an appropriate position of the separation gel. After electrophoresis, the protein was transferred to a membrane under 100V constant voltage for 100min and blocked at 37°C for 60 min. Subsequently, the membrane was blocked with 5% skim milk powder for future immune response. The membrane was incubated with primary antibody (1:1000) at 4°C for one night, then washed with warm PBS three times, 5min each time. After washing, the membrane was incubated with secondary antibody (1: 1000) at room temperature for one h. After incubation, the protein was developed and fixed with an ECL agent. The expression of the U6 gene was used as an internal reference control. The scanned protein band was analyzed using Quantity One software, and the relative protein expression level = the gray value of the band/gray value reference.
Cell proliferation detection by CCK-8 assay
Cells at the logarithmic growth phase were collected, digested with trypsin, and resuspended. A total of 100μL of cells were seeded into a 96-well plate after the concentration was adjusted to 2*104/ml. The cells were added with 200μL of CCK8 mixed solution (10: 1) at 24h, 48h, 72h, and 96h after culturing, and after the 4-time points, the cells were cultured for 3h again, and then the optical density (OD) of each well at 450nm was determined.
Cell apoptosis determination
The cells were digested with 0.25% trypsin. After digestion, the cells were washed with PBS two times, then added with 100μL of binding buffer to prepare 1*106 cells /mL suspension. The suspension was added with AnnexinV-FITC and PI in order, incubated at room temperature for 5min in the dark, and finally detected using the CytoFLE S flow cytometer system. The experiment was repeated three times, and the average value was taken.
Dual-luciferase reporter assay
Human embryonic kidney cell 293T (BeNa Culture Collection, BNCC100530) were cultured to the logarithmic growth phase and then transfected with pmirGLO-FOXO3- 3′UTR wild type (Wt), pmirGLO-FOXO3-3′UTR mutant type (Mut), miR-155-mimic, and miR-NC. At 48h after transfection, the cells’ fluorescence intensity was determined using the dual-luciferase determination system (CytoFLEX flow cytometer). The sequences were designed by Thermo Fisher Scientific (China).
Statistical analysis
SPSS 19.0 (Asia Analytics Formerly SPSS China) was adopted in this study. Measurement data were expressed by mean ± standard deviation (mean ± sd), and comparison between groups was analyzed using the independent-samples T-test. Receiver operating characteristic (ROC) curves were adopted for diagnostic value evaluation. Pearson correlation analysis was adopted to analyze correlation. P<0.05 indicated a significant difference. Separate biological replicates trails were conducted thrice, and the experimental data is showcased here as average and standard deviation.
Results
Expressions of miR-155 and FOXO3 in B-cell lymphoma cell lines
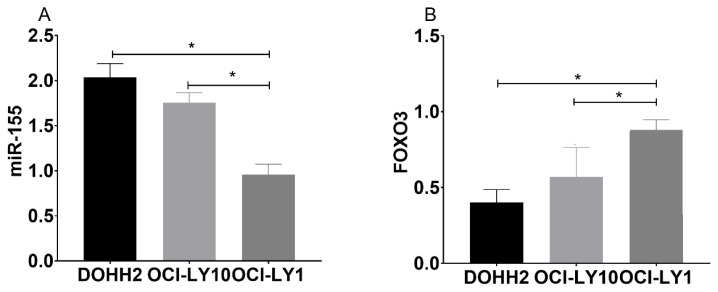
The qRT-PCR assay revealed that the expression of miR-155 in DOHH2 and OCI-LY10 cells was higher than that in AHH-1cells (P<0.05), while the expression of FOXO3 in DOHH2 and OCI-LY10 cells was lower than that in AHH-1cells (P<0.05) (Figure 1a). In Tumor tissues and normal tumoradjacent tissues samples of patients showed similar trends for the expression of miR-155 and FOXO3 (Figure 1b)
Figure 1. A. Expressions of miR-155 and FOXO3 in B-cell lymphoma cell lines.
Expression of miR-155 in B-cell lymphoma cell lines and Expression of FOXO3 in B-cell lymphoma cell lines. (Results are average of three biological replicates for each sample) * indicates P<0.05.
B. Expressions of miR-155 and FOXO3 in Tumor tissues (n=42) and normal tumor-adjacent tissues (n=42).
Expression of miR-155 in B-cell lymphoma cell lines. And expression of FOXO3 in B-cell lymphoma cell lines. (* indicates P<0.05; Results are average of three biological replicates for each sample).
Effects of inhibiting miR-155 on proliferation and apoptosis of B-cell lymphoma cells
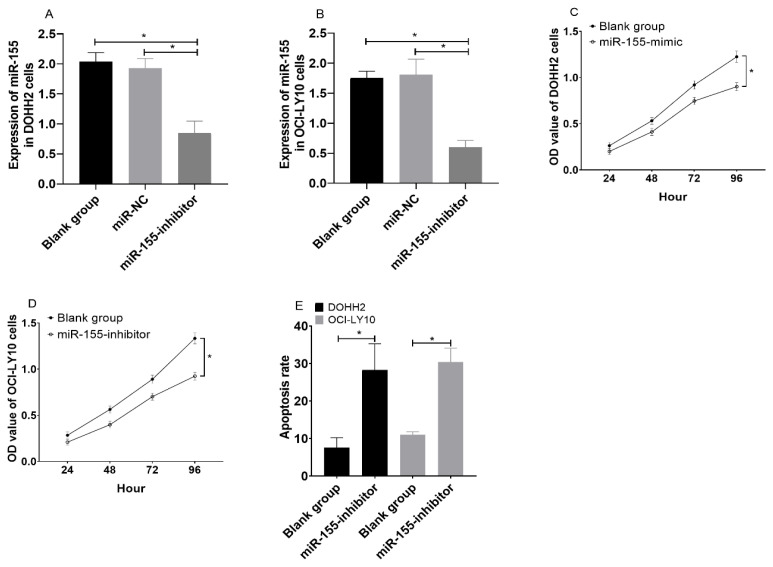
DOHH2 and OCI-LY10 cells transfected with miR-155-inhibitor showed significantly decreased expression of miR-155 (Figure 2a and 2b), significantly decreased cell proliferation ability (Figure 2c and 2d), and increased cell apoptosis rate (Figure 2e) (all P<0.05).
Figure 2. Effects of inhibiting miR-155 on proliferation and apoptosis of B-cell lymphoma cells.
A. Results about transfection of miR-155-inhibitor into DOHH2 cells. B. Results about transfection of miR-155-inhibitor into OCI-LY10 cells. C. Effects of transfection of miR- 155-inhibitor on proliferation ability of DOHH2 cells. D. Effects of transfection of miR-155-inhibitor on proliferation ability of OCI-LY10 cells. E. Effects of transfection of miR-155-inhibitor on apoptosis of B-cell lymphoma. (*indicates P<0.05; Results are average of three biological replicates).
Effects of inhibiting miR-155 on expression of FOXO3 in B-cell lymphoma cells
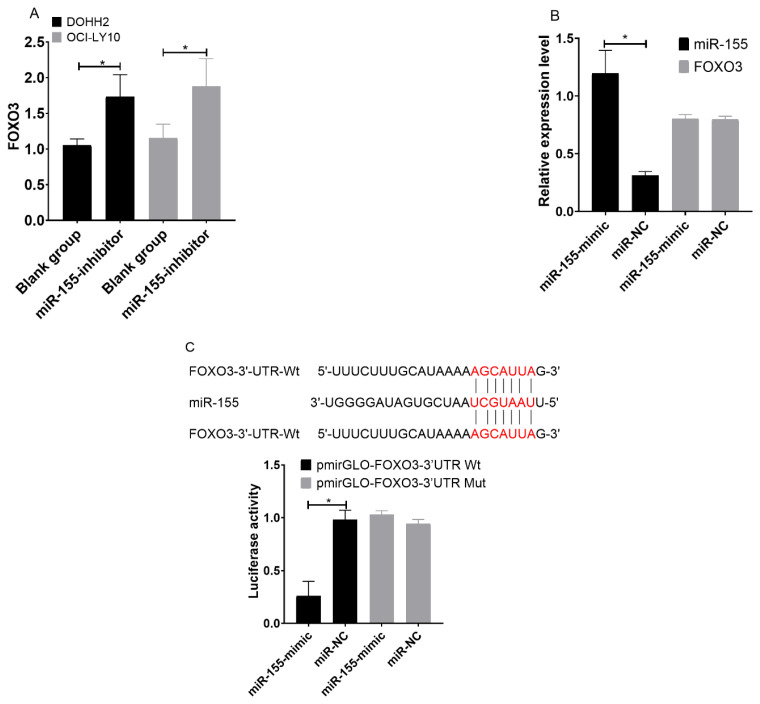
In western blot results, DOHH2 and OCI-LY10 cells transfected with miR-155- inhibitor showed increased expression of FOXO3 (Figure 3a) (P<0.05). Relative expression of miR-155 was more in miR-155-mimic, while FOXO3 was comparable in both (Figure 3b). The conclusion of predication by TargetScanHuman 7.2 indicated that there were targeted binding sites between miR-155 and FOXO3. Dual-luciferase reporter assay revealed that after transfection with miR-155-mimic, the fluorescence intensity of cells in the pmirGLO-FOXO3-3′UTR Wt group was significantly lower than that in cells in the pmirGLO-FOXO3-3′UTR Mut (P<0.05). (Figure 3c)
Figure 3. Effects of inhibiting miR-155 on the expression of FOXO3 in B-cell lymphoma cells.
A. Changes in the expression of FOXO3 in B-cell lymphoma cells after transfection with miR-155-inhibitor. B. Changes in the expressions of miR-155 and FOXO3 in B-cell lymphoma cells after transfection with miR-155-mimic. C. Sequence of FOXO3-3’-UTR mutant and dual luciferase reporter assay result. (*indicates P<0.05; Results are average of three biological replicates).
Effects of inhibiting FOXO3 on tumor-promoting action of miR-155
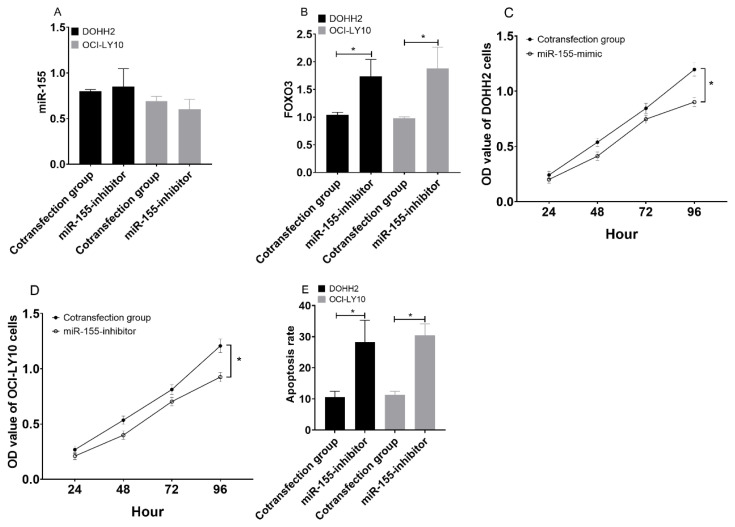
DOHH2 and OCI-LY10 cells co-transfected with miR-155-inhibitor + si-FOXO3 were not different from those transfected with miR-155-inhibitor alone (P>0.05) (Figure 4a), but showed significantly lower expression of FOXO3 than those transfected with miR- 155-inhibitor alone (P<0.05) (Figure 4b). In addition, DOHH2 and OCI-LY10 cells co-transfected with miR- 155-inhibitor + si-FOXO3 showed stronger cell proliferation ability (Figure 4c and d) and lower cell apoptosis rate than those transfected with miR-155- inhibitor alone (both P<0.05) (Figure 4f).
Figure 4. Effects of inhibiting FOXO3 on tumor-promoting action of miR-155.
A. Effects of co-transfection with miR-155-inhibitor + si- FOXO3 on expression of miR-155 in B-cell lymphoma. B. Effects of co-transfection with miR-155-inhibitor + si-FOXO3 on expression of FOXO3 in B-cell lymphoma. C. Effects of the co-transfection on proliferation ability of DOHH2 cells. D. Effects of the co-transfection on proliferation ability of OCI-LY10 cells. E. Effects of the co-transfection on apoptosis of B-cell lymphoma. (*indicates P<0.05; Results are average of three biological replicates).
Correlation of miR-155 and FOXO3 with clinicopathological features of DLBCL patients
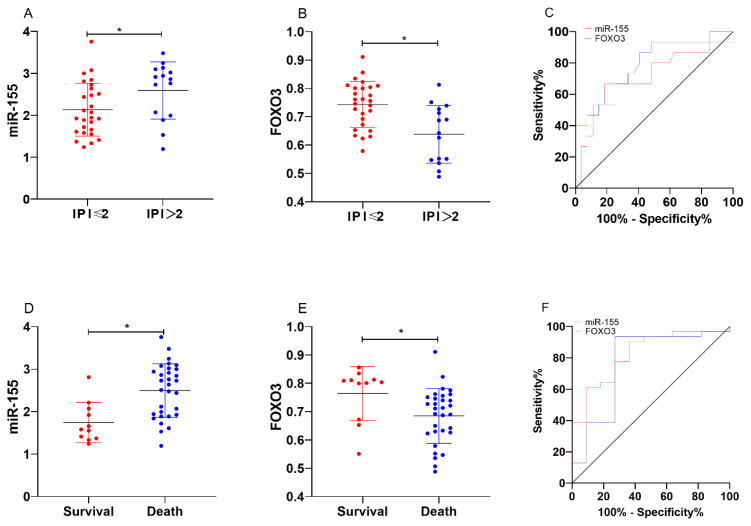
DLBCL tissues also showed increased expression of miR-155 and decreased expression of FOXO3 (both P<0.05). Analysis of the correlation of miR-155 and FOXO3 with clinicopathological features of DLBCL patients revealed that miR-155 and FOXO3 were closely related to the international prognostic index (IPI) score and 5-year prognosis and survival of the patients (P<0.05). ROC analysis revealed that the area-under-the- curve (AUC) of miR-155 for evaluating IPI score and 5-year prognosis and survival of DLBCL patients was 0.710 and 0.824, respectively, and the AUC of FOXO3 for them was 0.786 and 0.768, respectively. (Table 2 and Figure 5)
Table 2.
Correlation of miR-155 and FOXO3 with clinicopathological features of DLBCL patients.
| n | miR-155 | t | P | FOXO3 | t | P | |
|---|---|---|---|---|---|---|---|
| Tissues | 8.822 | <0.001 | 17.843 | <0.001 | |||
| Tumor | 42 | 2.298±0.677 | 0.699±0.104 | ||||
| Tumor-adjacent tissues | 42 | 1.317±0.246 | 1.728±0.357 | ||||
| Sex | 1.720 | 0.093 | 0.041 | 0.968 | |||
| Male | 19 | 2.491±0.782 | 0.705±0.110 | ||||
| Female | 23 | 2.139±0.544 | 0.706±.097 | ||||
| Age | 0.938 | 0.354 | 0.732 | 0.469 | |||
| ≤60 years old | 22 | 2.392±0.700 | 0.717±0.111 | ||||
| >60 years old | 20 | 2.195±0.653 | 0.693±0.092 | ||||
| Hans typing | |||||||
| GCB | 20 | 2.291±0.621 | 0.068 | 0.946 | 0.734±0.084 | ||
| Non-GCB | 22 | 2.305±0.739 | 0.680±0.111 | ||||
| Disease site | 0.547 | 0.587 | 0.621 | 0.538 | |||
| Within lymph node | 30 | 2.335±0.703 | 0.699±0.101 | ||||
| Outside lymph node | 12 | 2.207±0.627 | 0.721±0.106 | ||||
| Ann Arbor staging | 1.025 | 0.312 | 0.167 | 0.868 | |||
| I–II | 13 | 2.458±0.796 | 0.709±0.111 | ||||
| III–IV | 29 | 2.226±0.619 | 0.704±0.099 | ||||
| Tumor size | 1.295 | 0.203 | 0.677 | 0.502 | |||
| ≤10cm | 29 | 2.388±0.727 | 0.713±0.091 | ||||
| >10cm | 13 | 2.098±0.520 | 0.690±0.124 | ||||
| IPI score | 2.180 | 0.035 | 3.669 | 0.001 | |||
| ≤2 | 27 | 2.136±0.630 | 0.743±.081 | ||||
| >2 | 15 | 2.591±0.681 | 0.638±0.102 | ||||
| 5-year prognosis | 3.601 | 0.001 | 2.346 | 0.024 | |||
| Survival | 11 | 1.742±0.473 | 0.764±0.095 | ||||
| Death | 31 | 2.495±0.632 | 0.685±0.097 | ||||
Figure 5. Correlation of miR-155 and FOXO3 with clinicopathological features of DLBCL patients.
A. Relationship between miR-155 and IPI score. B. Relationship between FOXO3 and IPI score. C. Abilities of miR-155 and FOXO3 in evaluating IPI score of DLBCL patients. D. Relationship between miR-155 and 5-year prognosis and survival. E. Relationship between FOXO3 and 5-year prognosis and survival. F. Abilities of miR-155 and FOXO3 in evaluating the 5-year prognosis and survival of DLBCL patients. (*indicates P<0.05; Results are average of three biological replicates).
Discussion
MiR-155 plays a role in various physiological and pathological processes.8,9 Exogenous molecular control in vivo of miR-155 expression may inhibit malignant growth9,11 viral infections,12 and enhance the progression of cardiovascular diseases.13 MiR-155 is a microRNA that, in humans, is encoded by the MIR155 host gene or MIR155HG. The MIR155HG was initially identified as a transcriptionally activated gene by promoter insertion; its RNA transcript does not contain a long open reading frame (ORF); however, it does include an imperfectly base-paired stem-loop that is conserved across species.15 Once miR-155 primiRNA is transcribed, this transcript is cleaved by the nuclear microprocessor complex, of which the core components are the RNase III type endonuclease Drosha and the DiGeorge critical region 8 (DGCR8) protein, to produce a 65-nucleotide stem-loop precursor miRNA (pre-mir-155).16,17 The 23-nucleotide single-stranded miR-155, which is harbored in exon 3, is subsequently processed from the parent RNA molecule.14 Very few studies have investigated the expression levels of miR- 155-3p, Landgraf et al. established that expression levels of this miRNA were very low in hematopoietic cells. Additionally, PCR analyses found that while miR-155- 3p was detectable in many human tissues, the expression levels of this miRNA were 20–200 fold less compared to miR-155-5p levels.24,25 In previous studies, many scholars had reported on the correlation of miR-155, FOXO3 with tumors as follows: The expression of miR- 155 was upregulated in tumors and played a role in promoting cancer,14,15 while the expression of FOXO3 was down-regulated, and could inhibit the occurrence and development of tumors.16,17 Recent studies have indicated that miR-155 and FOXO families are related to B-cell lymphoma’s occurrence and diffusion.18,19 However, the role of FOXO3 in B-cell lymphoma is still under investigation, and whether there was a regulatory relationship between miR-155, FOXO3, and B-cell lymphoma is also under investigation.
This study analyzed the roles of miR-155 and FOXO3 in two B-cell lymphoma cell lines, compared with normal B lymphocytes; B-cell lymphoma cells showed significantly increased expression of miR-155, which was consistent with previous studies, showing tumor-promoting effects on B-cell lymphoma.20 In our study, we also found that inhibiting the expression of miR-155 in B-cell lymphoma cells led to significantly decreased proliferation ability and increased apoptosis rate of B-cell lymphoma cells, and it also led to decreased expression of FOXO3 in them. However, we also found that inhibiting the expression of miR-155 led to increased expression of FOXO3 in B-cell lymphoma cells. It indicated that FOXO3 might play a similar role in B-cell lymphoma as FOXO3 in breast cancer and pancreatic cancer by inhibiting tumor development.20,21 In order to verify this hypothesis, we co-transfected inhibition vectors of miR-155 and FOXO3 into B-cell lymphoma cells, finding the following situations: B-cell lymphoma cells co-transfected with inhibition vectors were not different from those transfected with inhibition vector of miR-155 alone in the expression of miR-155, but showed lower expression of FOXO3 than those transfected with inhibition vector of miR-155 alone. In addition, B-cell lymphoma cells co-transfected with inhibition vectors showed higher cell proliferation ability and lower cell apoptosis rate than those transfected with miR-155-inhibitor. It suggested that FOXO3 could suppress the tumor-promoting action of miR-155 in B-cell lymphoma cells. Dual-luciferase reporter assay revealed that there were targeted binding sites between miR-155 and FOXO3. Based on the above results, we preliminarily verified that miR-155 promoted B-cell lymphoma cells’ proliferation ability and inhibited apoptosis by targeted inhibition of FOCXO3.
In recent years, some studies have also pointed out that miR-155 plays a regulatory role in tumors by targeting FOXO3. For example, a study by Kim et al. reported that miR-155 suppressed glucose uptaking and metabolism of breast cancer cells and inhibited tumor growth through the PIK3R1-FOXO3a-cMYC signal axis.22 A study by Zhang et al. also indicated that miR-155 could target inhibition of FOCXO3 and promote proliferation and metastasis of non-small cell lung cancer cells and inhibit apoptosis.23 A study by Ji et al. pointed out that miR-155 could promote proliferation, colony formation, migration, invasion of renal clear cell carcinoma by targeted inhibition of FOCXO3, and suppress block and apoptosis of the cells in the G1 phase.24 The role of FOXO3 against B-cell lymphoma is related to the immune function regulation by FOXO3. As we all know, the occurrence of B-cell lymphoma is bound up with both immune dysfunction.25 FOXO3 was reportedly able to promote the proliferation of T lymphocytes and B lymphocytes.26,27 However, in this study, we have not conducted in vivo cell experiments to verify it in future studies.
We analyzed the correlation of miR-155 and FOXO3 with clinicopathological features of DLBCL patients, finding that miR-155 and FOXO3 were closely related to IPI score and 5-year prognosis and survival of the patients, which indicated that miR-155 and FOXO3 were strongly linked to the prognosis of DLBCL patients. A study by Hanne et al. pointed out that overexpression of miR-155 was related to poor prognosis of patients with B-cell lymphoma,28 and a study by Ahmadvand et al. also drew similar conclusions.29 It may be related to the effects of miR-155 and FOXO3 on chemotherapy to B-cell lymphoma. miR-155 can regulate the sensitivity of tumor cells to radiotherapy by targeting FOXO3. A study by Khoshinani et al. revealed that miR-155 reduced colorectal cancer cells’ sensitivity to radiotherapy by targeted inhibition of FOCXO3.30 It provides a direction for our future research. Namely, targeted inhibition of FOXO3 by miR-155 may also affect B-cell lymphoma cells’ sensitivity to radiotherapy and chemotherapy. To sum up, miR-155 can promote the proliferation of B-cell lymphoma cells and suppress apoptosis of them by targeted inhibition of FOCXO3, and both overexpression of miR-155 and low expression of FOXO3 are related to poor prognosis of DLBCL patients.
Footnotes
Competing interests: The authors declare no conflict of Interest.
References
- 1.Ren W, Ye X, Su H, Li W, Liu D, Pirmoradian M, Wang X, Zhang B, Zhang Q, Chen L, et al. Genetic landscape of hepatitis B virus-associated diffuse large B-cell lymphoma. Blood. 2018;131:2670–2681. doi: 10.1182/blood-2017-11-817601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Swerdlow SH. WHO classification of tumours of haematopoietic and lymphoid tissues. WHO classification of tumours 22008. 2008:439. [Google Scholar]
- 3.Horwitz SM, Zelenetz AD, Gordon LI, Wierda WG, Abramson JS, Advani RH, Andreadis CB, Bartlett N, Byrd JC, Fayad LE, et al. NCCN guidelines insights:non-Hodgkin’s lymphomas, version 3.2016. J Natl Compr Canc Netw. 2016;14:1067–1079. doi: 10.6004/jnccn.2016.0117. [DOI] [PubMed] [Google Scholar]
- 4.Lenz G, Wright GW, Emre NC, Kohlhammer H, Dave SS, Davis RE, Carty S, Lam LT, Shaffer AL, Xiao W, et al. Molecular subtypes of diffuse large B-cell lymphoma arise by distinct genetic pathways. Proc Natl Acad Sci U S A. 2008;105:13520–13525. doi: 10.1073/pnas.0804295105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gonçalves OSL, Wheeler G, Dalmay T, et al. Detection of miRNA cancer biomarkers using light activated Molecular Beacons. Rsc Advances. 2019;9:12766–12783. doi: 10.1039/C9RA00081J. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mullany LE, Herrick JS, Sakoda LC, Samowitz W, Stevens JR, Wolff RK, Slattery ML. miRNA involvement in cell cycle regulation in colorectal cancer cases. Genes Cancer. 2018;9:53. doi: 10.18632/genesandcancer.167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Zhang J, Wei B, Hu H, Liu F, Tu Y, Zhao M, Wu D. Preliminary study on decreasing the expression of FOXP3 with miR-155 to inhibit diffuse large B-cell lymphoma. Oncol Lett. 2017;14:1711–1718. doi: 10.3892/ol.2017.6345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Huang X, Shen Y, Liu M, Bi C, Jiang C, Iqbal J, McKeithan TW, Chan WC, Ding SJ, Fu K. Quantitative proteomics reveals that miR-155 regulates the PI3K-AKT pathway in diffuse large B-cell lymphoma. Am J Pathol. 2012;181:26–33. doi: 10.1016/j.ajpath.2012.03.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Coomans de Brachène A, Demoulin JB. FOXO transcription factors in cancer development and therapy. Cell Mol Life Sci. 2016;73:1159–1172. doi: 10.1007/s00018-015-2112-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Obrador-Hevia A, Serra-Sitjar M, Rodríguez J, Villalonga P, Fernández de Mattos S. The tumour suppressor FOXO3 is a key regulator of mantle cell lymphoma proliferation and survival. Br J Haematol. 2012;156:334–345. doi: 10.1111/j.1365-2141.2011.08951.x. [DOI] [PubMed] [Google Scholar]
- 11.He B, Yan F, Wu C. Overexpressed miR-195 attenuated immune escape of diffuse large B-cell lymphoma by targeting PD-L1. Biomed Pharmacother. 2018;98:95–101. doi: 10.1016/j.biopha.2017.11.146. [DOI] [PubMed] [Google Scholar]
- 12.Huang J, Jiao J, Xu W, Zhao H, Zhang C, Shi Y, Xiao Z. MiR-155 is upregulated in patients with active tuberculosis and inhibits apoptosis of monocytes by targeting FOXO3. Mol Med Rep. 2015;12:7102–7108. doi: 10.3892/mmr.2015.4250. [DOI] [PubMed] [Google Scholar]
- 13.Ling N, Gu J, Lei Z, Li M, Zhao J, Zhang HT, Li X. microRNA-155 regulates cell proliferation and invasion by targeting FOXO3a in glioma. Oncol Rep. 2013;30:2111–2118. doi: 10.3892/or.2013.2685. [DOI] [PubMed] [Google Scholar]
- 14.Van Roosbroeck K, Fanini F, Setoyama T, Ivan C, Rodriguez-Aguayo C, Fuentes-Mattei E, Xiao L, Vannini I, Redis RS, D’Abundo L, et al. Combining anti-miR-155 with chemotherapy for the treatment of lung cancers. Clin Cancer Res. 2017;23:2891–2904. doi: 10.1158/1078-0432.CCR-16-1025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Zargar S, Tomar V, Shyamsundar V, Vijayalakshmi R, Somasundaram K, Karunagaran D. A feedback loop between microRNA 155 (miR-155), programmed cell death 4, and activation protein 1 modulates the expression of miR-155 and tumorigenesis in tongue cancer. Mol Cell Biol. 2019;39:e00410–18. doi: 10.1128/MCB.00410-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Yao S, Fan LY, Lam EW. The FOXO3-FOXM1 axis:A key cancer drug target and a modulator of cancer drug resistance[C]//Seminars in cancer biology. Semin Cancer Biol. 2018;50:77–89. doi: 10.1016/j.semcancer.2017.11.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kumazoe M, Takai M, Bae J, Hiroi S, Huang Y, Takamatsu K, Won Y, Yamashita M, Hidaka S, Yamashita S, et al. FOXO3 is essential for CD44 expression in pancreatic cancer cells. Oncogene. 2017;36:2643. doi: 10.1038/onc.2016.426. [DOI] [PubMed] [Google Scholar]
- 18.Slezak-Prochazka I, Kluiver J, de Jong D, Smigielska-Czepiel K, Kortman G, Winkle M, Rutgers B, Koerts J, Visser L, Diepstra A, et al. Inhibition of the miR-155 target NIAM phenocopies the growth promoting effect of miR-155 in B-cell lymphoma. Oncotarget. 2016;7:2391. doi: 10.18632/oncotarget.6165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ushmorov A, Wirth T. FOXO in B-cell lymphopoiesis and B cell neoplasia[C]//Seminars in cancer biology. Semin Cancer Biol. 2018;50:132–141. doi: 10.1016/j.semcancer.2017.07.008. [DOI] [PubMed] [Google Scholar]
- 20.Zhang L, Cai M, Gong Z, Zhang B, Li Y, Guan L, Hou X, Li Q, Liu G, Xue Z, et al. Geminin facilitates FoxO3 deacetylation to promote breast cancer cell metastasis. J Clin Invest. 2017;127:2159–2175. doi: 10.1172/JCI90077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kumazoe M, Takai M, Hiroi S, Takeuchi C, Kadomatsu M, Nojiri T, Onda H, Bae J, Huang Y, Takamats uK, et al. The FOXO3/PGC-1β signaling axis is essential for cancer stem cell properties of pancreatic ductal adenocarcinoma. J Biol Chem. 2017;292:10813–10823. doi: 10.1074/jbc.M116.772111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kim S, Lee E, Jung J, Lee JW, Kim HJ, Kim J, Yoo HJ, Lee HJ, Chae SY, Jeon SM, et al. microRNA-155 positively regulates glucose metabolism via PIK3R1-FOXO3a-cMYC axis in breast cancer. Oncogene. 2018;37:2982. doi: 10.1038/s41388-018-0124-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Zhang Y, Zhao H, Zhang L. Identification of the tumor suppressive function of circular RNA FOXO3 in non small cell lung cancer through sponging miR 155. Mol Med Rep. 2018;17:7692–7700. doi: 10.3892/mmr.2018.8830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ji H, Tian D, Zhang B, Zhang Y, Yan D, Wu S. Overexpression of miR 155 in clear cell renal cell carcinoma and its oncogenic effect through targeting FOXO3a. Exp Ther Med. 2017;13:2286–2292. doi: 10.3892/etm.2017.4263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Andor N, Simonds EF, Czerwinski DK, Chen J, Grimes SM, Wood- Bouwens C, Zheng GXY, Kubit MA, Greer S, Weiss WA, et al. Single-cell RNA-Seq of follicular lymphoma reveals malignant B-cell types and coexpression of T-cell immune checkpoints. Blood. 2019;133:1119–1129. doi: 10.1182/blood-2018-08-862292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Togher S, Larange A, Schoenberger SP, Feau S. FoxO3 is a negative regulator of primary CD8+ T – cell expansion but not of memory formation. Immunol Cell Biol. 2015;93:120–125. doi: 10.1038/icb.2014.78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ottens K, Hinman RM, Barrios E, Skaug B, Davis LS, Li QZ, Castrillon DH, Satterthwaite AB. Foxo3 Promotes Apoptosis of B Cell Receptor- Stimulated Immature B Cells, Thus Limiting the Window for Receptor Editing. J Immunol. 2018;201:940–949. doi: 10.4049/jimmunol.1701070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Due H, Svendsen P, Bødker JS, Schmitz A, Bøgsted M, Johnsen HE, El-Galaly TC, Roug AS, Dybkær K. miR-155 as a Biomarker in B-Cell Malignancies. Biomed Res Int. 2016;2016:1–14. doi: 10.1155/2016/9513037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ahmadvand M, Eskandari M, Pashaiefar H, Yaghmaie M, Manoochehrabadi S, Khakpour G, Sheikhsaran F, Montazer Zohour M. Over expression of circulating miR-155 predicts prognosis in diffuse large B-cell lymphoma. Leuk Res. 2018;70:45–48. doi: 10.1016/j.leukres.2018.05.006. [DOI] [PubMed] [Google Scholar]
- 30.Khoshinani HM, Afshar S, Pashaki AS, Mahdavinezhad A, Nikzad S, Najafi R, Amini R, Gholami MH, Khoshghadam A, Saidijam M. Involvement of miR-155/FOXO3a and miR-222/PTEN in acquired radioresistance of colorectal cancer cell line. Jpn J Radiol. 2017;35:664–672. doi: 10.1007/s11604-017-0679-y. [DOI] [PubMed] [Google Scholar]