Abstract
Introduction
According to the World Health Organization (WHO), COVID-19 has become a Public Health Emergency of International Concern (PHEIC). Understanding patients’ hematologic findings in SARS-CoV-2 infection is essential to doing their prognosis, so adjusting care and improving outcomes.
Objective
In this review, we aim at summarizing changes in the hematopoietic system and hemostasis that occur in SARS-CoV-2 infected patients.
Findings
COVID-19 infection is often associated with laboratory hematologic features that can have important clinical implications. Careful revision of baseline hematologic data at diagnosis can predict the severity of illness and help clinicians tailoring the approach and management of patients whose condition can be guarded or critical. The levels of hematologic markers like D-dimer, procalcitonin, C-reactive protein, viral load, inflammatory cytokines, differential blood cell count, and peripheral smear are fundamental for the prognosis. Studies have also shown an association between some of these markers and severe COVID-19 infection requiring admission to the intensive care unit or complicated by acute respiratory distress syndrome (ARDS). Since, so far, a vaccine is not available, prevention of the infection is based on the avoiding people affected and the spreading of the virus; the treatment, in the absence of an effective antiviral agent, is symptomatic, and, in addition to oxygen support, finds in the anti-inflammatory drugs and anticoagulation fundamental therapeutic lines. According to the American Society of Hematology (ASH), all hospitalized patients with COVID-19 should receive pharmacologic thromboprophylaxis with LMWH.
Keywords: COVID-19, Hematology, Haemostasis
Introduction
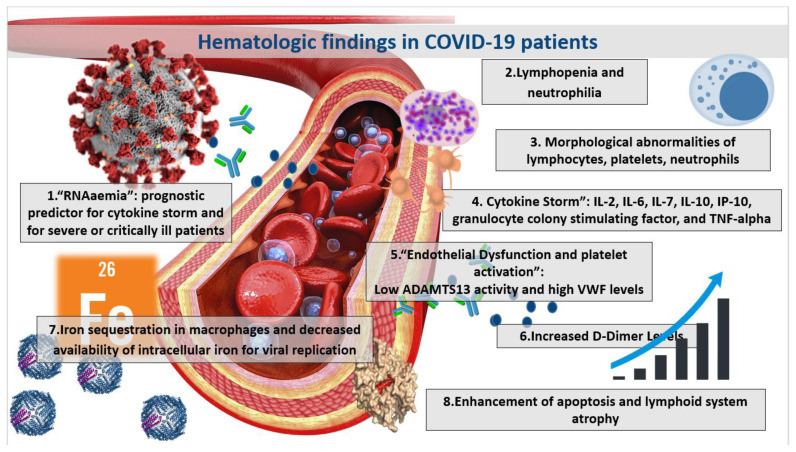
Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), causing COVID-19 infection, has emerged rapidly to involve more than 32 million individuals worldwide. According to the World Health Organization (WHO), COVID-19 has become a Public Health Emergency of International Concern (PHEIC).1 COVID-19 infection consists of a broad spectrum of clinical manifestations, ranging from fever, cough, and dyspnea to severe pneumonia, sepsis, and disturbed blood gas levels.2 While SARS-CoV-2 is considered a respiratory virus, data has shown that the COVID-19 is a systemic infection that involves various systems, including cardiovascular, gastrointestinal, respiratory, nervous, hematopoietic, and immune systems. As a result, not only patients with underlying lung disease are at risk for severe COVID-19 infection, but also SARS-CoV-2 can affect young, healthy individuals with potentially lethal complications, such as disseminated intravascular coagulopathy, myocarditis, venous thrombo-embolism, and severe lymphopenia.3–6 Understanding the hematologic findings of patients with COVID-19 infection is essential to promote their care and improve outcomes. Figure 1 summarizes the major hematologic findings in patients with COVID-19. In this review, we aim at summarizing changes in the hematopoietic system and hemostasis that occur in COVID-19 infected patients.
Figure 1.
Hematologic findings in COVID-19 patients.
Manifestations through the Complete Blood Count Test
The complete blood count (CBC) during the SARS-CoV-2 incubation period, lasting until 14 days, is usually normal. Around one to two weeks following the onset of clinical symptoms of patients with COVID-19 infection, lymphopenia can become evident. In a large study from China, including 1099 COVID-19 patients, most had lymphopenia (83.2%), and thrombocytopenia and leukopenia were present in 26.2% and 33.7% of patients, respectively.7 Studies have also shown an association between lymphopenia and severe COVID-19 infection, requiring admission to the intensive care unit or complicated by acute respiratory distress syndrome (ARDS).
In a retrospective cohort study in China, Wu et al. investigated the clinical characteristics associated with ARDS development and mortality. Increased neutrophils and decreased lymphocytes were associated with greater mortality rates for COVID-19 patients. In bivariate Cox regression analysis, risk factors associated with ARDS development and progression from ARDS to death included neutrophilia (HR, 1.14; 95% CI, 1.09–1.19; and HR, 1.08; 95% CI, 1.01–1.17, respectively). Compared to patients without ARDS, patients with ARDS had significantly decreased lymphocyte counts (difference, −0.34 ×109/mL; 95% CI, −0.47 to −0.22 ×109/mL; P < .001).5,8 Interestingly, a predominance of lymphoplasmacytoid-lymphocytes was reported in COVID-19 infected patients. Bain et al. reported the case of a COVID-19 patient whose blood film revealed atypical reactive lymphocytes. Among these lymphocytes were prominent lymphoplasmacytoid-lymphocytes with an eccentric nucleus and a basophilic cytoplasm.9 Zini et al. also found abnormal neutrophils with a pseudo-Pelger-like nucleus and giant vacuolated platelets.10
A variety of factors can contribute to the pathogenesis of CBC changes, particularly of the observed lymphopenia. SARS-CoV-2, which affects tissues that express angiotensin-converting enzyme 2 (ACE-2), namely the respiratory, cardiac, and gastrointestinal systems, has a predilection to lymphocytes, which express ACE-2 over their surface. Infection of these cells by SARS-CoV-2 results in cell lysis. COVID-19 infection is also characterized by a pronounced surge in inflammatory markers, including interleukins (IL) and tumor necrosis factor (TNF)-alpha. This peak in inflammatory markers, referred to as “cytokine storm”, is manifested by markedly increased serum levels of IL-2, IL-6, IL-7, granulocyte colony-stimulating factor, and TNF-alpha. The cytokine storm contributes to the lymphoid system’s apoptosis and reactive atrophy, promoting lymphopenia.3–5
COVID-19 cytokine storm has introduced a new entity to the spectrum of cytokine release syndrome (CRS). CRS can be associated with influenza infection, severe acute respiratory syndrome (SARS), autoimmune diseases, and hematologic conditions like hemophagocytic lymphohistiocytosis (HLH). The overlap in clinical and biochemical features between COVID-19 cytokine storm and cytokine release syndromes associated with other conditions may allow for more insight into the immune dysregulation in COVID-19 cytokine storm enhancing options for therapeutic intervention. Like other hematologic conditions, namely HLH, post-CART cell therapy, and idiopathic multicentric Castleman disease, COVID-CRS is manifested by fever and multi-organ dysfunction. COVID-CRS is also associated with thrombosis and a hypercoagulable state, similar to HLH, and with hypotension, tachycardia, and hypoxia, similar to post-CART cell therapy CRS.11
Moreover, IL-6 can be markedly elevated, even exceeding 10000 pg/ml, similar to post-CART cell therapy CRS. Determining if COVID-19 shows a marked increase in IL-6 level at the CART cell therapy CRS range is essential in managing critical patients with COVID-19. High IL-6 level has mortality implications and has been the primary endpoint of several ongoing clinical trials. In a case series of 5 patients with severe COVID-CRS, Hoiland et al. conducted a preliminary evaluation of tocilizumab on inflammatory cytokines, including IL-1β, IL-6, IL-10, and tumor necrosis factor-alpha (TNF-α). All patients had markedly increased peak serum IL-6 levels. This case series provides evidence that patients with severe COVID-19 may exhibit hypercytokinemia at ranges similar to CAR-T CRS. The reduction in serum inflammatory markers following tocilizumab administration correlates with improved clinical parameters.12
COVID-19 and Vascular Endothelial Dysfunction
In addition to lymphocytes and lung tissue, angiotensin-converting enzyme 2 (ACE-2) is expressed in endothelial cells, explaining the virus’s presence in endothelium and the clinical events observed in COVID-19, such as high blood pressure, thrombosis, and pulmonary embolism. Endothelial damage is a fundamental mechanism in this disease due to the viral infection and is of particular relevance in patients with previous vasculopathy, like people with diabetes or hypertension. The rate of hypertension among COVID-19 patients has been reported to reach up to 30%. Also, 60% of hypertensive patients with COVID-19 infection were likely to be admitted to ICU, which supports the hypothesis that hypertension can be common comorbidity and cause of ICU admission in this patient population.13–15 In addition to hypertension, diabetes is another comorbidity that is related to COVID-19 and endothelial dysfunction. Interestingly, fasting blood sugar level (FPG), other than sound diabetes, was independently associated with an increased hazard ratio of mortality and hypoxia in COVID-19 patients after controlling for age and gender. A glucose level above or equal to 7 mmol/l was an independent predictor of death in these patients.13
Not only endothelial dysfunction in the setting of comorbidities, including hypertension and diabetes, correlates to poor outcome in COVID-19 patients, but also vascular occlusion in the pulmonary and systemic circulation contributes. The strong relationship between inflammation and COVID-19 was further supported by a series of 7 lung autopsies from patients who died from COVID-19. They showed distinctive vascular features with the presence of endothelial injury, intracellular virus, and disrupted cell membranes. Pulmonary vessels showed diffuse thrombosis and microangiopathy.16
In a single-center cross-sectional study by Goshua et al., markers of endothelial cell dysfunction and platelet activation, including VWF antigen and soluble P-selectin, were significantly more elevated in ICU patients than non-ICU patients. Mortality was significantly associated with VWF antigen and soluble thrombomodulin among all 68 patients.17 Moreover, Morici et al. tested ADAMTS-13 levels in plasma from six patients admitted to the intensive care unit. Five of the six tested patients had plasma ADAMTS-13 levels lower than 45%, the lower limit of the normal range, possibly preventing the effective cleavage of VWF multimers, which favors the formation of local thrombin.18 These data were further supported by Blasi et al., who showed that COVID-19 patients had high von Willebrand factor levels and low ADAMTS13 activity.19 Interestingly, patients who died had significantly lower levels of ADAMTS-13 and higher levels of von Willebrand factor (vWF).20,21
COVID-19 and Risk of Coagulopathy
Strictly connected with the endothelial damage is the coagulopathy due to activation of the coagulative cascade, which can favor arterial and venous thrombosis, and, at last, bring about disseminated intravascular coagulation (DIC).21,22
Tang et al. retrospectively analyzed coagulation results and outcomes of 183 consecutive patients with confirmed severe novel coronavirus pneumonia in Tongji hospital, finding that the overall mortality was 11.5%. The non-survivors had significantly higher D-dimer and fibrin degradation product (FDP) levels, longer prothrombin time, and activated partial thromboplastin time compared to survivors on admission (P < .05); 71.4% of non-survivors and 0.6% survivors met the criteria of disseminated intravascular coagulation during their hospital stay.22 The DIC present in the COVID-19 has the particularity not to be followed by hyperfibrinolysis but by reduced fibrinolysis,23,24 and the spectacularly raised D-dimer levels may signify the fibrinolytic system’s failing attempt to remove fibrin and necrotic tissue from the lung parenchyma.23 Therefore, the use of fibrinolytic compounds have been suggested for COVID-19 ARDS.24
Moreover, Tang et al., utilizing SIC score (Sepsi induced coagulopathy of International Society of Thrombosis and Haemostasis) to identify an earlier phase of sepsis-associated DIC, found that only the patients whose SIC score was ≥4 when treated with heparin had a lower mortality rate 40.0% as compared to 64.2% for patients not treated with heparin (P=0.029). This was not the case for patients with SIC score <4 (29.0% vs 22.6%, P=0.419).25 In any case, the coagulopathy present in COVID-19 remains mostly a thrombotic coagulopathy.
Several case reports have been published about COVID-19 associated with venous thromboembolism (VTE), including deep venous thrombosis with pulmonary embolism.26,27 Among 81 patients with severe COVID-19 infection and admitted to ICU, Ciu et al. reported a 25% incidence of VTE. 40% of these patients who had VTE died. Interestingly, elevated levels of D-dimer above 1.5 μg/ml (normal range: 0.0–0.5 μg/ml) predicted VTE incidence with a sensitivity of 85.0%, a specificity of 88.5%, and a negative predictive value (NPV) of 94.7%.28
D-dimer has gained attention in COVID-19 infection as a predictor for ARDS, risk for admission to the intensive care unit (ICU), and death risk. In a multivariate analysis from a retrospective study by Tang et al., D-dimer was positively correlated with 28-day mortality.24 In another retrospective study by Zheng et al., including 99 hospitalized COVID-19 patients, critically ill patients had significantly greater D-dimer levels with a p-value of <0.001 compared to non-critically ill patients. A D-dimer level greater than 2.6 μg/ml was clinically manifested by critical illness.24 Liu et al. reported a significant difference in D-dimer levels between patients with mild and severe COVID-19 infection among a population of 76 patients (p=0.007).29 Measuring the D-dimer level in COVID-19 patients can help predict the severity of the disease, their risk of requiring admission to ICU, and the risk of mortality. All these data suggest anticoagulants’ active application, such as heparin, as recommended by China’s first experience.25 Although these data have not yet been validated by a perspectival study, according to the American Society of Hematology (ASH), all hospitalized patients with COVID-19 should receive pharmacologic thromboprophylaxis with LMWH, acknowledging the lack of quality published evidence regarding the appropriate dosage. Many institutional protocols have adopted an intermediate-intensity consisting of the usual LMWH dose twice daily or even a therapeutic-intensity dose strategy for thromboprophylaxis based on local experience. The ASH recommends participation in clinical trials and studies on thromboprophylaxis for COVID-19 patients when available. After discharge, the decision for thromboprophylaxis should consider the patient’s venous thromboembolism risk factors, the bleeding risk, and reduced mobility, in addition to feasibility.29
Furthermore, the possible association between D-dimer and venous thromboembolism indicates that D-dimer level-guided aggressive thromboprophylaxis regimens using higher doses of heparin may be warranted. In fact, in a retrospective French cohort study by Artifoni et al., of 71 non-ICU COVID-19 patients, 16 developed venous thromboembolism (22.5%) and seven pulmonary embolism (10%) despite adequate thromboprophylaxis.31 It was recommended that hospitalized COVID-19 patients be generally treated with higher Low Molecular Weight Heparin (LMWH) doses than recommended for thromboprophylaxis.30–33 Suggested doses included higher than prophylaxis dose up to full anticoagulant doses of LMWH or unfractionated heparin. Cassini et al. published a proposed set of recommendations for pharmacological thromboprophylaxis in COVID-19 patients in the acute setting. They recommend that all in-hospital COVID-19 patients should receive pharmacological thromboprophylaxis according to a risk stratification score, unless contraindicated.34 This use of LMWH was challenged by a Cattaneo et al., who questioned whether the observed pulmonary vessel occlusions described in reports on COVID-19 patients are exclusively caused by pulmonary embolism or somewhat reminiscent of pulmonary thrombi as they are not fully occlusive.35
Testing for Systemic Markers of Inflammation and Infection
Hyperinflammation plays a fundamental role in determining the main pathological feature of COVI-19. Lung injury is inflammation-mediated and induces progression to respiratory failure and death.4 The importance of inflammation in lung disease had been demonstrated previously in SARS-CoV-1 infection; lung tissue biopsy from patients infected showed SARS is associated with epithelial cell proliferation and an increase in macrophages in the lung.36 The presence of haemophagocytosis supports the contention that cytokine dysregulation may account, at least partly, for the severity of the clinical disease. An increase in inflammatory cytokines was found in SARS-CoV-1 and MERS, suggesting the occurrence of cytokines storm, responsible for lung disease.37,38
Similarly, in a retrospective study by Liu et al. showed a significant difference in IL-2R, IL-6, and IL-8 levels between patients with mild and severe COVID-19 infection (p = 0.022, 0.026, and 0.012, respectively).39
In a prospective study by Laguna-Goya et al., a cohort of 611 adult patients in whom COVID-19 was diagnosed between March 10 and April 12, 2020, in Madrid, Spain, in a tertiary hospital was analyzed.40 High IL-6 level, C-reactive protein level, lactate dehydrogenase (LDH) level, ferritin level, D-dimer level, neutrophil count, and neutrophil-to-lymphocyte ratio were all predictive of mortality, with an area under the curve that was greater than 0.70, as were low albumin level, lymphocyte count, monocyte count, and the ratio of peripheral blood oxygen saturation to the fraction of inspired oxygen (SpO2/FiO2). The authors developed a multivariate mortality risk model that showed high accuracy of predicting fatal outcome with an area under the curve of 0.94. This risk model consisted of SpO2/FiO2 ratio, neutrophil-to-lymphocyte ratio, LDH level, IL-6 level, and age.41 Similarly, a study by Herold et al. analyzing data from 89 patients aimed at validating biomarkers that allow identification of patients with an impending need for mechanical ventilation. The strongest association with the need for mechanical ventilation was maximal IL-6 levels before intubation followed by maximal CRP levels, with the area under the curve of 0.97 and 0.86, respectively. These can be used as a guide for escalation of management when treating patients with COVID-CRS.42
A recent meta-analysis by Lagunas-Rangel et al. investigated whether the IL-6/IFN-γ ratio can have a predictive value to rate the clinical severity in patients with COVID-19. Patients with severe COVID-19 disease had a significantly increased IL-6/IFN-γ ratio with a standardized mean difference of 0.739 (95% CI = 0.131–1.383).43 Pro-inflammatory cytokines can have an important clinical significance not only in identifying patients who are at risk for severe disease but also in management itself. Xu et al. reported the effective treatment of severe COVID-19 infections with tocilizumab, a humanized monoclonal antibody against IL-6. All 20 patients have been analyzed IL-6 expression levels before tocilizumab with a mean of 132.38 pg/ml, showing IL-6 upregulation in these severe and critical COVID-19 patients. This treatment provided a new strategy for severe COVID-19 disease and reflected the role of pro-inflammatory markers in disease severity..43 The classical steroid treatment of hyper inflammation conditions had been initially excluded in the fearing of favoring viral spreading. However, in the last few months, some important articles have demonstrated its efficacy,44–46 and in a prospective meta-analysis of clinical trials of critically ill patients with COVID-19, administration of systemic corticosteroids, compared with usual care or placebo, was associated with lower 28-day all-cause mortality.47
Of course, bacterial superinfection has a significant role in worsening virus pneumonitis and also the virus SARS-Cov-, so knowing the behavior of the typical t marker of bacterial infection could be useful. Procalcitonin seems to play an essential prognostic role in patients with severe coronavirus infection. A study by Hu et al. that included 95 patients with COVID-19 showed that the mean serum levels of procalcitonin in patients with severe infection were over four times higher than those with moderate infection, and levels were over eight times higher in those with a critical condition as compared to patients with moderate infection.48 This datum merits an interpretation, being well known that calcitonin does not increase during viral infection.
During bacterial infections, procalcitonin production is amplified and sustained by increased production of IL-1β, TNF-α, and IL-6. On the other hand, its production is downregulated by INF-γ, which increases in viral infections. As such, procalcitonin level would be expected to be within the normal range in patients with non-complicated SARS-CoV-2 infection, whereas patients with superimposed bacterial co-infection and thus developing a severe infection are more likely to have an elevated procalcitonin level.49 A meta-analysis by Lippi et al. suggested that serial procalcitonin measurement can predict evolution towards a more severe form of infection. Increased procalcitonin values were associated with a nearly 5-fold higher risk of severe infection (OR = 4.76; 95% CI: 2.74–8.29).49
In addition to procalcitonin, C-reactive protein also plays an important predictive role in COVID-19 infection. In a retrospective study by Liu et al., among 140 patients diagnosed with COVID-19, the proportion of patients with increased C-reactive protein, IL-6, and procalcitonin was significantly higher in patients with severe COVID-19 infection as compared to those with mild disease.50 In a meta-analysis by Zhu et al. including 38 studies of 3062 patients, elevated C-reactive protein was observed in 73.6% of patients and elevated procalcitonin levels in 17.5% of patients.51 Parallel to this paper, Zhang et al., in a study including 140 patients from Wuhan, showed that significantly higher levels of C-reactive protein, D-dimer, and procalcitonin were associated with severe COVID-19 infection compared to patients with non-severe infection with a p-value less than 0.001.52
Apart from pro-inflammatory cytokines, procalcitonin, and C-reactive protein, ferritin has also been considered a possible predictive marker of severe COVID-19. Serum ferritin level has been utilized by clinicians as part of a panel to assess iron stores. However, serum ferritin is also increased in response to infections, inflammation, and malignancy and is generally accepted as an acute phase reactant similar to C-reactive protein.53 In a retrospective study by Chen et al., the clinical and immunological characteristics were studied for 21 COVID-19 patients. Compared to moderate cases, severe cases more frequently had higher levels of ferritin.
Besides, these severe cases were more likely to have dyspnea, lymphopenia, and hypoalbuminemia, higher levels of alanine aminotransferase, lactate dehydrogenase, C-reactive protein, and D-dimer, and markedly higher levels of IL-2R, IL-6, IL-10, and TNF-α.54 All patients with worsening COVID-19 infection should be screened for hyper-inflammation using systemic markers, including D-dimer, ferritin, C-reactive protein as predictors for severity of the infection. However, while ferritin seems to be associated with disease severity, it does not seem positively correlated with mortality. In a multivariate analysis that included 218 patients, Mehta et al. showed that increased mortality among cancer patients with COVID-19 was significantly associated with D-dimer’s elevated levels but not ferritin.55
COVID-19 and Systemic Iron
Systemic iron and inflammatory cytokines, including IL-6 and IL-β, regulate hepcidin production. COVID-19 is associated with increased release of pro-inflammatory cytokines, which, in turn, induces T-helper-1 cell response and promotes hepcidin production, and enhances iron sequestration in macrophages. While it is hypothesized that increased iron availability may favor viral replication inside macrophages, hyperferritinemia is not a common feature of COVID-19, unlike patients with typical HLH.57–59 A therapeutic target for iron metabolism and COVID-19 replication is erythropoietin (EPO) produced by the kidneys through hypoxia-inducible factor-2, its primary transcription factor. In addition to increasing red blood cell mass, it has beneficial cytoprotective effects, including anti-ischemic and antiapoptotic effects on various tissues, including the lungs. More importantly, erythropoietin administration can result in the pro-inflammatory cytokines and hepcidin downregulation, which leads to increased release of iron by macrophages and increased iron absorption by the bone marrow. Iron redistribution could result in decreased availability of intracellular iron for viral replication.59 Chloroquine and hydroxychloroquine have also been shown to play a potential therapeutic role through iron metabolism. Experiments on mice have shown that treatment with chloroquine or hydroxychloroquine can inhibit the Tf/transferrin receptor (TFR1) complex endocytosis, which results in decreased intracellular iron levels. In addition to inhibiting the release of pro-inflammatory cytokines, they induce macrophage iron starvation, resulting in the macrophage population’s shift from pro-inflammatory macrophages M1 to anti-inflammatory macrophage M2, so attenuating COVID-19 infection.60,61 In addition to iron metabolism, viral proteins, including orf1ab, ORF10, and ORF3a, can target heme on the beta-1 chain of hemoglobin and dissociating iron to form porphyrin and that increases deoxyhemoglobin, which is more vulnerable to viral infection than oxidized hemoglobin.62 In conclusion, the virus attack will cause less and less hemoglobin that can carry oxygen and carbon dioxide, producing respiratory distress symptoms.
Correlation between COVID-19 Infection Severity and the Viral Load
Correlation between the SARS-CoV-2 viral load and disease severity has seldom been explored. An open-label non-randomized clinical trial by Gautret et al. was among the first studies during the pandemic to measure the viral load in COVID-19 patients. While the trial aimed at assessing response to hydroxychloroquine and azithromycin, the study did not correlate the viral load, as measured by serum real-time reverse transcription-polymerase chain reaction assay (RT-PCR), with the clinical course of patients.63 Two retrospective studies correlated the viral load with pro-inflammatory cytokines and disease severity. Chen et al. used RT-PCR to quantify the serum SARS-CoV-2 viral load and correlated it with IL-6 level and disease severity. Out of the 48 laboratory-confirmed COVID-19 patients enrolled, sharply increased IL-6 level was observed in critically ill patients, which was almost ten times that of severe patients, and all deaths exhibited extremely high IL-6 value. More importantly, the extremely high IL-6 level was closely correlated with the detection of RNAaemia with a correlation coefficient R=0.902.64
On the other hand, Liu et al. used quantitative RT-PCR from throat swab samples to quantify COVID-19 patients’ nasopharyngeal viral load. There was a significant positive correlation between the SARS-CoV-2 RNA load and IL-2R with a p-value of 0.002. The time needed for the nucleic acid test to turn negative was significantly shorter for patients in the mild group than for those in the severe group (Z = −6.713, p < 0.001). As such, the cytokine release can be closely related to the nasopharyngeal viral load of SARS-Cov-2, which could be a significant cause of COVID-19 disease severity.65
Conclusion and Take-Home Messages
In conclusion, COVID-19 infection is often associated with laboratory hematologic findings that have important clinical implications. However, the consequences of hematologic changes in COVID-19 patients are not yet fully delineated to date. Careful revision of baseline hematologic findings at diagnosis can predict the severity of illness and help clinicians tailor their management and approach to patients whose condition can be guarded or critical. Such markers include D-dimer, viral load, cytokine storm, lymphopenia, and endothelial damage markers, like vWF and thrombomodulin. More studies are needed to correlate these changes with COVID-19 pathology, including thrombosis and inflammation pathogenesis. The hematologic data can be of therapeutic and prognostic value in severely ill patients and can reduce the mortality rate from COVID-19. Currently ongoing research to enhance the understanding of the infection ensues and shall contribute to optimizing its management. We urgently need more studies to define appropriate management plans in the setting of hematologic findings. However, until, in the absence of a specific antiviral agent and vaccine, the therapy can be only symptomatic. For that, the hematologic data are fundamental, even it the gold standard approach remains the prevention by breaking the cycle of COVID-19, limiting the virus spread. Until more data arises, the summary we provide here can be used by hematologists to understand better the hematopoietic system and hemostasis in COVID-19 infected patients.
Table 1.
Take-Home Messages.
| Criterion | Hematologic Finding |
|---|---|
| Peripheral Blood Cells |
|
| Inflammatory Markers |
|
| Endothelial Lung Dysfunction |
|
| Coagulopathy |
|
| Viral Load |
|
| Systemic Iron |
|
Footnotes
Competing interests: The authors declare no conflict of Interest.
References
- 1.Boulos M, et al. Geographical tracking and mapping of coronavirus disease COVID-19/severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) epidemic and associated events around the world: how 21st century GIS technologies are supporting the global fight against outbreaks and epidemics. Int J Health Geogr. 2020;19:8. doi: 10.1186/s12942-020-00202-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Marietta M, Ageno W, Artoni A. De Candia ECOVID-19 and haemostasis: a position paper from Italian Society on Thrombosis and Haemostasis (SISET) Blood Transfus. 2020. Apr 8, [DOI] [PMC free article] [PubMed]
- 3.Driggin E, Madhavan MV, Bikdeli B, et al. Cardiovascular Considerations for Patients, Health Care Workers, and Health Systems During the Coronavirus Disease 2019 (COVID-19) Pandemic. J Am Coll Cardiol. 2020. Mar 18, [DOI] [PMC free article] [PubMed]
- 4.Mehta P, McAuley DF, Brown M, et al. COVID-19: consider cytokine storm syndromes and immunosuppression. Lancet. 2020 Mar 28;395(10229):1033–1034. doi: 10.1016/S0140-6736(20)30628-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Terpos E, Ntanasis-Stathopoulos I, Elalamy I, et al. Hematological findings and complications of COVID-19. American Journal of Hematology. [DOI] [PMC free article] [PubMed]
- 6.Mao L, Jin H, Wang M, et al. Neurologic Manifestations of Hospitalized Patients With Coronavirus Disease 2019 in Wuhan, China. JAMA Neurol. doi: 10.1001/jamaneurol.2020.1127. Published online April 10, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Guan WJ, Ni ZY, Hu Y, et al. Clinical Characteristics of Coronavirus Disease 2019 in China. N Engl J Med. 2020 Feb 28; doi: 10.1056/NEJMoa2002032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wu Z, McGoogan JM. Characteristics of and Important Lessons From the Coronavirus Disease 2019 (COVID-19) Outbreak in China: Summary of a Report of 72314 Cases From the Chinese Center for Disease Control and Prevention. JAMA. 2020. Feb 24, [DOI] [PubMed]
- 9.Foldes D, Hinton R, Arami S, Bain BJ. Plasmacytoid lymphocytes in SARS-CoV-2 infection (Covid-19) Am J Hematol. 2020. Apr 16, [DOI] [PMC free article] [PubMed]
- 10.Zini G, Bellesi S, Ramundo F, d’Onofrio G. Morphological anomalies of circulating blood cells in COVID-19. Am J Hematol. 2020 Jul;95(7):870–872. doi: 10.1002/ajh.25824. doi: 10.1002/ajh.25824. Epub 2020 April 22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.England JT, Abdulla A, Biggs CM, et al. Weathering the COVID-19 storm: Lessons from hematologic cytokine syndromes. Blood Rev. 2020:100707. doi: 10.1016/j.blre.2020.100707. doi: 10.1016/j.blre.2020.100707. [published Online First: 2020/05/20] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hoiland RL, Stukas S, Cooper J, et al. Amelioration of COVID-19 related cytokine storm syndrome: Parallels to chimeric antigen receptor-T cell cytokine release syndrome. Br J Haematol. 2020 doi: 10.1111/bjh.16961. doi: 10.1111/bjh.16961. [published Online First: 2020/06/26] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sardu C, Gambardella J, Morelli MB, Wang X, Marfella R, Santulli G. Is COVID-19 an Endothelial Disease? Clinical and Basic Evidence Preprints. 2020 doi: 10.20944/preprints202004.0204.v1. 2020040204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Turco S, Vianello A, Ragusa R, et al. COVID-19 and cardiovascular consequences: Is the endothelial dysfunction the hardest challenge? Thromb Res. 2020 Dec;196:143–151. doi: 10.1016/j.thromres.2020.08.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Jung F, Krüger-Genge A, Franke RP, Hufert F, Küpper JH. COVID-19 and the endothelium. Clin Hemorheol Microcirc. 2020;75(1):7–11. doi: 10.3233/CH-209007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ackermann M, Verleden SE, Kuehnel M, et al. Pulmonary Vascular Endothelialitis, Thrombosis, and Angiogenesis in Covid-19. N Engl J Med. 2020;383(2):120–128. doi: 10.1056/NEJMoa2015432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Goshua G, Pine AB, Meizlish ML, et al. Endotheliopathy in COVID-19-associated coagulopathy: evidence from a single-centre, cross-sectional study. Lancet Haematol. 2020;7(8):e575–e582. doi: 10.1016/S2352-3026(20)30216-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Morici N, Bottiroli M, Fumagalli R, et al. Role of von Willebrand Factor and ADAMTS-13 in the Pathogenesis of Thrombi in SARS-CoV-2 Infection: Time to Rethink. Thromb Haemost. 2020 Sep;120(9):1339–1342. doi: 10.1055/s-0040-1713400. [DOI] [PubMed] [Google Scholar]
- 19.Blasi A, von Meijenfeldt FA, Adelmeijer J, et al. In vitro hypercoagulability and ongoing in vivo activation of coagulation and fibrinolysis in COVID-19 patients on anticoagulation. J Thromb Haemost. 2020;00:1–8. doi: 10.1111/jth.15043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bazzan, Montaruli B, Sciascia S, Cosseddu D, Norbiato C, Roccate D. Low ADAMTS 13 plasma levels are predictors of mortality in COVID 19 patients. Internal and Emergency Medicine. 2020;15:861–863. doi: 10.1007/s11739-020-02394-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Escher R, Breakey N, Lämmle B. Severe COVID-19 infection associated with endothelial activation. Thromb Res. 2020 Jun;190:62. doi: 10.1016/j.thromres.2020.04.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Tang N, Li D, Wang X, Sun Z. Abnormal coagulation parameters are associated with poor prognosis in patients with novel coronavirus pneumonia. J Thromb Haemost. 2020;18(4):844–847. doi: 10.1111/jth.14768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Medcalf RL, Keragala CB, Myles PS. Fibrinolysis and COVID-19: A plasmin paradox. J Thromb Haemost. 2020. Jun 16, [DOI] [PMC free article] [PubMed]
- 24.Wang J, Hajizadeh N, Moore EE, et al. Tissue Plasminogen Activator (tPA) treatment for COVID-19 associated acute respiratory distress syndrome (ARDS): a case series. J Thromb Haemost. 2020 doi: 10.1111/jth.14828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Tang N, Bai H, Chen X, et al. Anticoagulant treatment is associated with decreased mortality in severe coronavirus disease 2019 patients with coagulopathy. J Thromb Haemost. 2020 doi: 10.1111/jth.14817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Danzi GB, Loffi M, Galeazzi G, Gherbesi E. Acute pulmonary embolism and COVID-19 pneumonia: a random association? Eur Heart J. 2020. [DOI] [PMC free article] [PubMed]
- 27.Kollias A, Kyriakoulis KG, Dimakakos E, et al. Thromboembolic risk and anticoagulant therapy in COVID-19 patients: Emerging evidence and call for action. Br J Haematol. 2020. Apr 18, [DOI] [PMC free article] [PubMed]
- 28.Cui S, Chen S, Li X, Liu S, Wang F. Prevalence of venous thromboembolism in patients with severe novel coronavirus pneumonia. J Thromb Haemost. 2020. [DOI] [PMC free article] [PubMed]
- 29.Zheng Y, Xu H, Yang M, et al. Epidemiological characteristics and clinical features of 32 critical and 67 noncritical cases of COVID-19 in Chengdu. J Clin Virol. 2020;127:104366. doi: 10.1016/j.jcv.2020.104366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kreuziger L, et al. COVID-19 and VTE/Anticoagulation: Frequently Asked Questions (Version 3.0; last updated May 18, 2020) https://www.hematology.org/covid-19/covid-19-and-vte-anticoagulation.
- 31.Wang T, Chen R, Liu C, et al. attention should be paid to venous thromboembolism prophylaxis in the management of COVID-19. Lancet Haematol. 2020 doi: 10.1016/S2352-3026(20)30109-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Artifoni M, et al. Systematic assessment of venous thromboembolism in COVID-19 patients receiving thromboprophylaxis: incidence and role of D-dimer as predictive factors. J Thromb Thrombolysis. 2020 May;25:1–6. doi: 10.1007/s11239-020-02146-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Klok FA, Kruip MJHA, van der Meer NJM, et al. Incidence of thrombotic complications in critically ill ICU patients with COVID-19. Thromb Res. 2020 doi: 10.1016/j.thromres.2020.04.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Casini A, Alberio L, Angelillo-Scherrer A, et al. thromboprophylaxis and laboratory monitoring for in-hospital patients with COVID-19 - a Swiss consensus statement by the Working Party Hemostasis. Swiss Med Wkly. 2020;150:w20247. doi: 10.4414/smw.2020.20247. Published 2020 April 11. [DOI] [PubMed] [Google Scholar]
- 35.Cattaneo M, Bertinato EM, Birocchi S, et al. Pulmonary Embolism or Pulmonary Thrombosis in COVID-19? Is the Recommendation to Use High-Dose Heparin for Thromboprophylaxis Justified? [published online ahead of print, 2020 April 29] Thromb Haemost. 2020 doi: 10.1055/s-0040-1712097. doi: 10.1055/s-0040-1712097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Nicholls JM, Poon LL, Lee KC, Ng WF, Lai ST, Leung CY, et al. Lung pathology of fatal severe acute respiratory syndrome. Lancet. 2003;361(9371):1773–8. doi: 10.1016/S0140-6736(03)13413-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Channappanavar R, Perlman S. Pathogenic human coronavirus infections: causes and consequences of cytokine storm and immunopathology. Semin Immunopathol. 2017 Jul;39(5):529–539. doi: 10.1007/s00281-017-0629-x. doi: 10.1007/s00281-017-0629-x. Epub 2017 May 2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.He L, Ding Y, Zhang Q, Che X, He Y, Shen H, Wang H, Li Z, Zhao L, Geng J, Deng Y, Yang L, Li J, Cai J, Qiu L, Wen K, Xu X, Jiang S. Expression of elevated levels of pro-inflammatory cytokines in SARS-CoV-infected ACE2+ cells in SARS patients: relation to the acute lung injury and pathogenesis of SARS. J Pathol. 2006 Nov;210(3):288–97. doi: 10.1002/path.2067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Liu F, Li L, et al. Prognostic Value of interleukin-6, C-reactive Protein, and Procalcitonin in Patients With COVID-19. J ClinVirol. 2020 Jun;127:104370. doi: 10.1016/j.jcv.2020.104370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Laguna-Goya R, Utrero-Rico A, Talayero P, et al. IL-6-based mortality risk model for hospitalized patients with COVID-19. J Allergy ClinImmunol. 2020 doi: 10.1016/j.jaci.2020.07.009. doi: 10.1016/j.jaci.2020.07.009. [published Online First: 2020/07/28] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Herold T, Jurinovic V, Arnreich C, et al. Elevated levels of IL-6 and CRP predict the need for mechanical ventilation in COVID-19. J Allergy Clin Immunol. 2020 doi: 10.1016/j.jaci.2020.05.008. doi: 10.1016/j.jaci.2020.05.008. [published Online First: 2020/05/20] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Lagunas-Rangel FA, Chávez-Valencia V. High IL-6/IFN-γ ratio could be associated with severe disease in COVID-19 patients. J Med Virol. 2020. Apr 16, [DOI] [PMC free article] [PubMed]
- 43.Xu Xiaoling, Han Mingfeng, Li Tiantian, et al. Effective Treatment of Severe COVID-19 Patients with Tocilizumab. Hospital of University of Science and Technology of China. http://www.chinaxiv.org/abs/202003.00026. [DOI] [PMC free article] [PubMed]
- 44.Horby P, Lim WS, Emberson JR, Mafham M, Bell JL, Linsell L, Staplin N, Brightling C, Ustianowski A, Elmahi E, Prudon B, Green C, Felton T, Chadwick D, Rege K, Fegan C, Chappell LC, Faust SN, Jaki T, Jeffery K, Montgomery A, Rowan K, Juszczak E, Baillie JK, Haynes R, Landray MJ. RECOVERY Collaborative Group. Dexamethasone in Hospitalized Patients with Covid-19 - Preliminary Report. N Engl J Med. 2020. Jul 17, NEJMoa2021436. [DOI]
- 45.Jeronimo CMP, Farias MEL, Val FFA, et al. Methylprednisolone as adjunctive therapy for patients hospitalized with COVID-19 (Metcovid) Clin Infect Dis. doi: 10.1093/cid/ciaa1177. Published online August 12, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Docherty AB, Harrison EM, Green CA, et al. Features of 20 133 UK patients in hospital with COVID-19 using the ISARIC WHO Clinical Characterisation Protocol. BMJ. 2020;369:m1985. doi: 10.1136/bmj.m1985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.WHO Rapid Evidence Appraisal for COVID-19 Therapies (REACT) Working Group. Sterne JAC, Murthy S, Diaz JV, Slutsky AS, Villar J, Angus DC, Annane D, Azevedo LCP, Berwanger O, Cavalcanti AB, Dequin PF, Du B, Emberson J, Fisher D, Giraudeau B, Gordon AC, Granholm A, Green C, Haynes R, Heming N, Higgins JPT, Horby P, Jüni P, Landray MJ, Le Gouge A, Leclerc M, Lim WS, Machado FR, McArthur C, Meziani F, Møller MH, Perner A, Petersen MW, Savovic J, Tomazini B, Veiga VC, Webb S, Marshall JC. Association Between Administration of Systemic Corticosteroids and Mortality Among Critically Ill Patients With COVID-19: A Meta-analysis. JAMA. 2020 Sep 2;324(13):1–13. doi: 10.1001/jama.2020.17023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Hu R, Han C, Pei S, Yin P, Chen X. Procalcitonin levels in COVID-19 patients. International Journal of Antimicrobial Agents. 2020. [DOI] [PMC free article] [PubMed]
- 49.Lippi G, Plebani M. Procalcitonin in patients with severe coronavirus disease 2019(COVID-19): Ameta-analysis. Clin Chim Acta. 2020 Jun;505:190–191. doi: 10.1016/j.cca.2020.03.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Liu F, Li L, et al. Prognostic Value of interleukin-6, C-reactive Protein, and Procalcitonin in Patients With COVID-19. J Clin Virol. 2020 Jun;127:104370. doi: 10.1016/j.jcv.2020.104370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Zhu J, Ji P, Pang J, et al. Clinical characteristics of 3,062 COVID-19 patients: a meta-analysis [published online ahead of print, 2020 April 15] J Med Virol. 2020. [DOI] [PMC free article] [PubMed]
- 52.Zhang JJ, Dong X, Cao YY, et al. Clinical characteristics of 140 patients infected with SARS-CoV-2 in Wuhan, China [published online ahead of print, 2020 February 19] Allergy. 2020. [DOI] [PubMed]
- 53.Zandman-Goddard G, Shoenfeld Y. Ferritin in autoimmune diseases. Autoimmun Rev. 2007;6:457–63. doi: 10.1016/j.autrev.2007.01.016. doi: 10.1016/j.autrev.2007.01.016. [DOI] [PubMed] [Google Scholar]
- 54.Chen G, et al. Clinical and immunological features of severe and moderate coronavirus disease 2019. J Clin Invest. 2020;130(5):2620–2629. doi: 10.1172/JCI137244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Mehta V, et al. Case Fatality Rate of Cancer Patients with COVID-19 in a New York Hospital System. Cancer Discov. 2020. May 1, [DOI] [PMC free article] [PubMed]
- 56.Liu W, Zhang S, Nekhai S, et al. Depriving Iron Supply to the virus Represents a Promising Adjuvant Therapeutic Against Viral Survival. Curr Clin Microbiol Rep. 2020 Apr;20:1–7. doi: 10.1007/s40588-020-00140-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Taher AT, Weatherall DJ, Cappellini MD. Thalassaemia. Lancet. 2018;391(10116):155–167. doi: 10.1016/S0140-6736(17)31822-6. [DOI] [PubMed] [Google Scholar]
- 58.Kumari N, Ammosova T, Diaz S, Lin X, Niu X, Ivanov A, et al. Increased iron export by ferroportin induces restriction of HIV-1 infection in sickle cell disease. Blood Adv. 2016;1(3):170–83. doi: 10.1182/bloodadvances.2016000745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Hadadi A, Mortezazadeh M, Kolahdouzan K, Alavian G. Does recombinant human erythropoietin administration in critically ill COVID-19 patients have miraculous therapeutic effects? J Med Virol. 2020 Jul;92(7):915–918. doi: 10.1002/jmv.25839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Quiros Roldan E, Biasiotto G, Magro P, Zanella I. The possible mechanisms of action of 4-aminoquinolines (chloroquine/hydroxychloroquine) against Sars-Cov-2 infection (COVID-19): A role for iron homeostasis? Pharmacol Res. 2020;158:104904. doi: 10.1016/j.phrs.2020.104904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Giamarellos-Bourboulis EJ, Netea MG, Rovina N, et al. Complex Immune Dysregulation in COVID-19 Patients with Severe Respiratory Failure. Cell Host Microbe. 2020;27(6):992–1000.e3. doi: 10.1016/j.chom.2020.04.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Liu W, Li W. COVID-19:Attacks the 1-Beta Chain of Hemoglobin and Captures the Porphyrin to Inhibit Human Heme Metabolism. ChemRxiv Preprint. 2020 doi: 10.26434/chemrxiv.11938173.v8. [DOI] [Google Scholar]
- 63.Gautret, et al. Hydroxychloroquine and azithromycin as a treatment of COVID-19: results of an open-label non-randomized clinical trial. International Journal of Antimicrobial Agents. 2020. In Press March 17, 2020 - [DOI] [PMC free article] [PubMed]
- 64.Chen X, Zhao B, Qu Y, Chen Y, Xiong J, Feng Y, et al. Detectable serum SARS-CoV-2 viral load (RNAaemia) is closely correlated with drastically elevated interleukin 6 (IL-6) level in critically ill COVID-19 patients. Clinical Infectious Diseases. 2020 doi: 10.1093/cid/ciaa449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Liu Y, Liao W, Wan L, Xiang T, Zhang W. Correlation Between Relative Nasopharyngeal Virus RNA Load and Lymphocyte Count Disease Severity in Patients with COVID-19. Viral Immunol. 2020. Apr 10, [DOI] [PubMed]