Abstract
Structural mitochondrial abnormalities and genetic aberrations in mitochondrial proteins have been known in Myelodysplastic syndrome (MDS), yet there is currently little data regarding MDS's metabolic properties and energy production cells. In the current study, we used state-of-the-art methods to assess OXPHOS in peripheral blood cells obtained from MDS patients and healthy controls. We then assessed the effect of food supplements-Coenzyme Q10 and carnitine on mitochondrial function and hematological response. We show here for the first time that there is a significant impairment of mitochondrial respiration in peripheral blood cells in low-risk MDS, which can be improved with food supplements. We also show that these supplements may improve the cytopenia and quality of life.
Keywords: Myelodysplastic syndrome, Mitochondria, Coenzyme Q10, carnitine
Introduction
Normal hematopoiesis is a well-coordinated process in which cell proliferation, maturation, and apoptosis are tightly regulated in the bone marrow.1 In recent years, there is a growing understanding of the importance of the tight control of the metabolic program and the balance of glycolysis and mitochondrial oxidative phosphorylation (OXPHOS) in maintaining quiescence and ensuring adequate and timely maturation of hematopoietic stem cells.2 This growing understanding is mostly due to the development of better tools to assess oxygen consumption rate (OCR) such as the Seahorse XF analyzer (Agilent), which allows much more accurate OCR measurements under basal conditions and also under conditions that force the cell to utilize its spare respiratory capacity.
Myelodysplastic syndrome (MDS) is a heterogeneous clonal disease of the bone marrow which is manifested by ineffective hematopoiesis and genomic instability leading to worsening cytopenias and a high percentage of transformation to acute myeloid leukemia (AML).3 The treatment options in MDS are quite limited.4,5
There are several lines of evidence suggesting the importance of mitochondrial dysfunction in the pathogenesis of MDS. First, structural mitochondrial abnormalities have been known for many years;6 Second, the importance of genetic aberrations in mitochondrial proteins in the prognosis of MDS and AML has been demonstrated by numerous studies looking at the gene and protein expression.7–8 A recent study demonstrated early shedding of mitochondria from reticulocytes in a sub-group of MDS patients, showing impaired mitochondrial dynamics.9 However, there is currently little data regarding the metabolic properties and energy production of peripheral blood MDS cells. We thought that in view of treatment options that can improve mitochondrial energy production, it is crucial to develop such an assay.
Such a readily available and inexpensive option is Coenzyme Q10 (CoQ10). This vitamin-like compound is an essential component of the mitochondrial electron transport chain and plays a central role in mitochondrial oxidative phosphorylation and adenosine triphosphate (ATP) production. Significant improvement in mitochondrial respiration with a clinical improvement has been achieved by oral administration of therapeutic doses of CoQ10 in various diseases.10,11 Further support for the role of impairment of mitochondrial function in the pathogenesis of the disease as well as a possible novel therapeutic approach was seen in a pilot study on low-risk MDS patients in which treatment with CoQ10 resulted in about 25% hematologic response and even cytogenetic response in some of the patients.12
L-carnitine is required to transport fatty acids from the cytosol to the mitochondrial during the breakdown of lipids. It has also been used to improve mitochondrial function and has been shown to have a synergistic effect when combined with coenzyme Q10 in various medical conditions.13–16
Patients and methods
Clinical trial design
This was an open-label, investigator-initiated study. Inclusion criteria: low to intermediate 1 MDS according to IPSS, not requiring or not eligible for treatment other than supportive care, and having at the onset at least one of the following: Hgb<10.5g/dL, PLT<100x109/L or ANC<0.8X109/L. Concomitant erythropoietin-stimulating agents (ESAs) were permitted as long as patients were treated for at least twelve weeks without further hematological improvement. A minor effect (such as the need for blood transfusion every ten days instead of every week was allowed). The reason for this, was because we thought it was unethical to withhold treatment that the patients felt was beneficial to them.
For optimal enhancement of mitochondrial function, patients were given a combination of Ultrasome™ (a better-absorbed formulation of CoQ10)-180 mg/ day, L-carnitine-2000 mg/ day, and a standard vitamin-mineral complex to ensure that there will be no lack of essential vitamins or minerals (a kind donation of Herbamed LTD, Israel), to be taken daily for six months. Patients were allowed to continue treatment for an additional six months if they desired to do so, and it was deemed beneficial by the protocol committee. Quality of life (QOL) was assessed using the FACT questionnaire17 at the beginning and third-month endpoint. We thought it was important to assess patient-reported outcomes alongside the objective parameters.18 Samples for assessing in vitro mitochondrial energy production in peripheral blood cells were taken in some of the patients before and after six months of treatment.
Endpoints were: hematological response according to IWG criteria3 and meaningful improvement in the quality of life and functional ability after three months of treatment with food supplements.
The study was approved by local IRB and registered at the National Institute of Health (NIH), registry no. NCT02042482.
Assessment of mitochondrial function
Mitochondrial function was assessed in peripheral blood cells using the Seahorse XF Analyzer, as previously described.19 The XF Analyzer creates micro-chambers of only a few microliters in specialized cell culture microplates. This enables OCR (oxygen consumption rate) to be monitored in real-time. Briefly, cells were plated on a Cell-Tak™ coated 24 well XF V7 cell culture microplate at 0.5×106 cells per well in 50 μL of XF assay medium. Plates were centrifuged at 1200 rpm for 5 minutes to allow the cells to adhere. 450 ul XF assay medium containing 5mM glucose, 2mM pyruvate, and 2 mM Glutamax (Invitrogen) at pH 7.4 were added to each well. Cells were incubated for one hour without CO2 for equilibration before XF bioenergetic assay. Basal Oxygen Consumption Rate (OCR: picomoles of O2 per minute) was measured, followed by consecutive injections of the following: 1. Oligomycin (ATP synthase inhibitor); 2. the electron transport chain accelerator FCCP (5 μM gives the maximal OCR capacity of the cells); 3. The electron transport-chain-inhibitor rotenone and Antimycin A, which inhibit mitochondrial respiration.
We decided to perform all experiments on fresh peripheral blood cells, which were used to avoid the need for repeat bone marrow aspirations. This was based on the fact that since previous studies have shown that peripheral blood cells harbor the same mutations as less mature cells obtained from the bone marrow,20 thus making it likely that peripheral blood cells will harbor the same genetic aberrations which affect mitochondrial respiration. Blood cells were not separated, and we know that mostly neutrophils and platelets could contribute to the results.
In each experiment, samples from MDS patients were compared to samples obtained from matched volunteers without hematological disorders to control for inter-assay variability. The same controls were used for all samples obtained from the same patient.
Statistical analysis
Statistical analysis was performed using the paired student t-test. The significance level was set at p<0.05.
Results
Clinical effect of food supplements
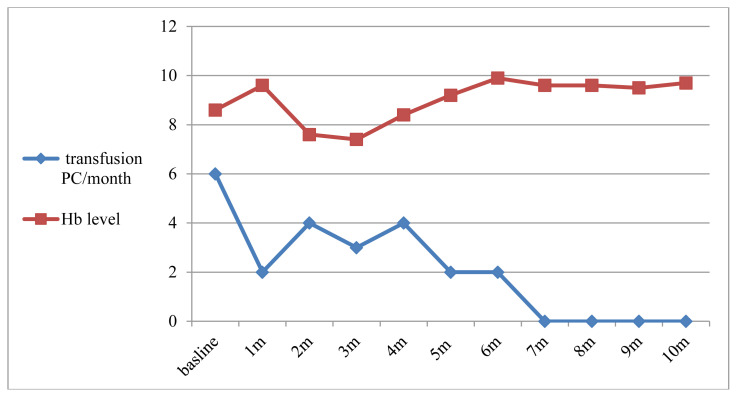
From May 2013 to April 2017, 33 MDS patients were enrolled in the clinical trial (Table 1). There were 20 males and 13 females, with a median age of 75 years (range: 56–93). The IPSS scoring showed a low risk in 19 (58%) and intermediate-1 risk in 14 (42%) patients; 13 patients (39%) had MDS with ring sideroblasts (MDS-RS). The median Hb level was 9.5 g/dL (range: 6.4–12.2). Seventeen patients (52%) were transfusion-dependent, requiring an average of 2.0 (range, 0.5–10) packed cell infusions per month. Twenty-eight patients completed the treatment protocol. Six patients (21.4%) achieved hematological improvement according to IWG criteria (four of these were previously transfusion-dependent, and one showed a bi-lineage response (see Figure 1 for a representative case). In 19 patients (67.8%) there was a stable disease at the end of the study. Interestingly, the hematological response in MDS-RS was similar to that seen in other MDS subtypes. The median time to initial response was nine weeks (range, 5–24), and the median duration of hematological improvement in responders was 54.5 weeks (range: 10–212).
Table 1.
Clinical characteristics of the patients.
| Age, median (range) years | 75(56–93) |
| Gender | Male 20(61%) Female 13(39) |
| 2016 WHO myelodysplastic syndrome subtypes | MDS with single lineage dysplasia - 5 (15%) MDS with ring sideroblasts (MDS-RS) - 13 ( 39%) MDS with multilineage dysplasia - 12 (37%) MDS with excess blasts - 2 (6%) MDS with isolated del(5q) - 1 (3%) |
| Karyotype | Normal karyotype-27 (82%), -Y-3., del20-1, trisomy 8-1., 5q-1. |
| IPSS | Low risk −19 (58%), Int-1 risk – 14 (42%) |
| IPSS-R | Very low risk – 7 (21%), Low – 21 (64%), Int. – 5 (15%) |
| Median time from diagnosis to study enrolment, months (range) | 12 (1 – 89.5) |
| Pretreatment Hb level, g/dL median (range) | 9.5 (6.5 – 12.2) |
| Primary failure of treatment with erythropoietin stimulating agents(%) | 16 (48%) |
| Red blood cells transfusion dependent n (%) | 17 (52%) |
Figure 1.
significant improvement in Hemoglobin ( Hb) level (red) and decreased need for Packed cell transfusion (blue) in a 56 year old man with MDS with ring sideroblasts following treatment with food supplements.
The FACT questionnaire was administered to 18 patients before and three months endpoint. There was a significant improvement in the mean FACT score (126.3±26.9 points before treatment vs. 117.3±26.3 after treatment; p=0.011). Notably, the scores' improvement was mostly in the physical well-being domains (mean, 22.2 points vs. 18.5; p=0.03) and not in the social and emotional domains. Interestingly These results demonstrated a moderate, though significant improvement in overall physical ability and quality of life, even in those patients that did not have a discernible hematological response.
Peripheral blood cells obtained from MDS patients have significant impairment of mitochondrial respiration, which can be reversed with food supplements
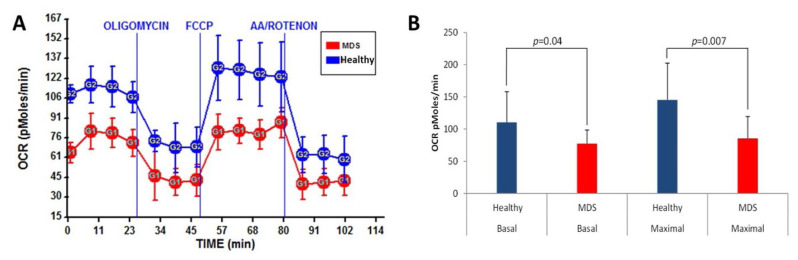
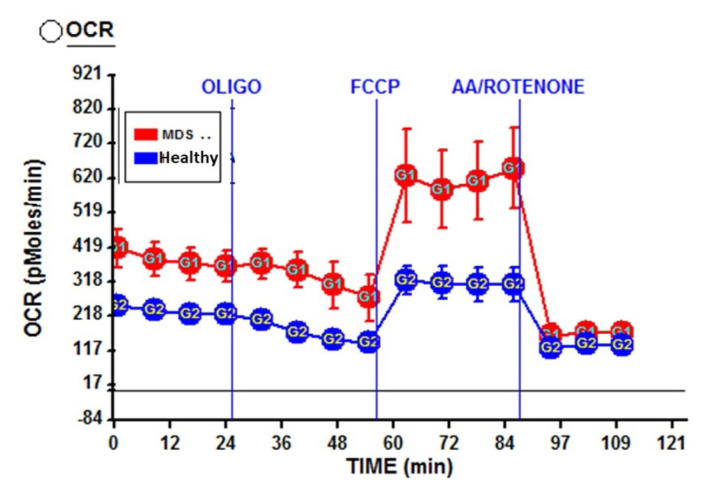
Mitochondrial oxidative phosphorylation was assessed in peripheral blood cells obtained from 20 MDS patients. Each experiment was done on a patient matched to a healthy control and repeated three times. In most patients (18/20), there was a significant decrease in basal oxygen consumption rate and the spare respiratory capacity (see Figure 2a for a representative patient) compared to healthy controls. This result was statistically significant (see Figure 2b). Interestingly, there was an increased oxygen consumption rate in two patients with excess of blasts in bone marrow (see Figure 3 for a representative patient).
Figure 2. Lower basal and maximal cellular respiration in fresh blood cells obtained from MDS patients as compared to healthy controls.
A. OCR measurements of peripheral blood cells obtained from an MDS patient (Red) in comparison to his matched healthy control (blue) under the same conditions. Cells were plated on a Cell-Tak™ coated 24 well XF V7 cell culture microplate at 0.5×106 cells per well in 50 μL of XF assay medium. Each dot represents the average of 3 repeats. B. Results shown are an average of 20 MDS patients and 20 healthy controls comparing the basal respiration (two left columns) and maximal respiration (two right columns) of the healthy controls (Blue) and MDS patients (Red). The error bars represent the standard deviation. Cellular respiration was assessed in fresh blood cells (two hours after collection from the patients at the hospital) using the Seahorse XF analyzer
Figure 3. Increased basal and maximal respiratory capacity in an MDS patient with excess of blasts.
OCR measurements of peripheral blood cells obtained from an MDS patient (Red) in comparison to his matched healthy control (blue). Each dot represents the average of 3 repeats. Cells were plated on a Cell-Tak™ coated 24 well XF V7 cell culture microplate at 0.5×106 cells per well in 50 μL of XF assay medium.
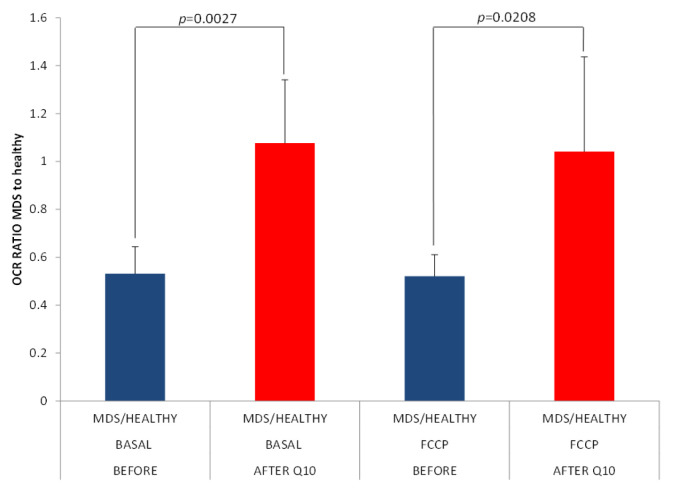
After six months of treatment, OCR assessment was done in five patients matched to their previous controls. The value pre-treatment was compared to the value post-treatment. A discernible improvement was seen in all the patients tested. The difference in OCR pre and post-treatment was statistically significant (p<0.05). (Figure 4).
Figure 4. Improved respiration in fresh blood cells obtained from patients who received food supplements.
Results shown are an average of five MDS patients comparing the Basal respiration of their blood cells before (Blue) and after (Red) treatment. The results are presented as the OCR ratio of the MDS patients to their healthy controls. Cellular respiration was assessed as described in Figure 1.
Safety and tolerability of combination supplement treatment
The treatment with food supplements was well tolerated; most adverse events were transient gastrointestinal symptoms of grade 2 or less. Surprisingly, two patients who had more advanced disease with an excess of blasts in the bone marrow developed disease progression within the first few weeks of treatment. Those patients also had increased OCR before treatment. Interestingly, it was shown that AML cells had increased OCR,21 suggesting that increased OXPHOS may be the first step in developing AML. As we could not rule out the possibility that the food supplements augmented progression, we amended the protocol to exclude patients with excess ( over 5%) of blasts. Another unexpected observation involved two patients who developed gastric diffuse large cell lymphoma one month and 30 months after cessation of treatment.
Discussion
The importance of mitochondrial energy metabolism is well recognized in normal hematopoiesis.2 Impairment of mitochondrial function in MDS has been strongly implied by the combination of structural mitochondrial abnormalities and early reticulocyte mitochondrial shedding present in some sub-groups,9 as well as abnormalities in genes essential for mitochondrial function8. However, such impairment of mitochondrial energy production was never demonstrated directly in peripheral blood cells. A previous study suggested a significantly impaired OCR in the bone marrow, but not in peripheral blood cells that harbor the same mutations.22 The discrepancy between this study and ours could be the inability of the Clark electrode used in that study to differentiate between different types of OCR.
In the current study, utilizing novel tools, we directly show for the first time that mitochondrial energy production is indeed impaired in peripheral blood cells obtained from patients with low-risk MDS. We showed that both the basal OCR and the spare respiratory capacity were significantly decreased compared to age-matched healthy controls. Those finding could have both diagnostic and therapeutic implications. It may also provide a non-invasive tool for monitoring response to treatment. Furthermore, we showed that this impairment in mitochondrial respiration can be partially reversed with food supplementations known to augment mitochondrial function. In some of the patients, this was also accompanied by a hematological response.
Galili et al. demonstrated a clinical benefit of high dose CoQ10 in some MDS patients.12 Likewise, combined treatment with CoQ10 and carnitine ameliorated anemia and RBC-transfusion-dependence in 6 out of 28 (21.4%) in our patient group. This improvement is noteworthy, as generally, low-risk MDS patients have minimal treatment options once they do not respond to ESAs. Interestingly, although the hematological response was achieved only in some of the patients treated with supplements, patient-reported outcomes of overall strength and physical ability were increased in most of them, along with improvement in mitochondrial respiration of peripheral blood cells.
The treatment was generally well tolerated. An unexpected observation, which is not in line with the reported side effects of the used food supplements, was a relatively high prevalence of second hematological malignancies in our cohort. It is hard to discern in such a small series of patients whether this is related to the treatment or coincidental with it. Progression to AML in MDS patients is frequent; also, lymphoid malignancies may be more prevalent than in the general population, and gastric lymphoma cases in patients with MDS have been described.23 Moreover, it has been shown that peripheral blood lymphocytes obtained from MDS patients harbor pre-malignant mutations.24 Overall, this treatment seems to be safe and effective in most low-risk MDS patients. Caution should be taken in patients with excess of blasts. This finding is important as many times patients take food supplements without the awareness of their clinicians.
Our study's limitation was that it was not randomized and that food supplements were given for a relatively short period. Further studies with a much longer follow-up are required to assess the safety and efficacy, as well as timing of treatment with the food supplements in different sub-groups of MDS patients.
Acknowledgments
We are grateful to Haim Aviv PhD for his help in the design of the research and donation of the food supplements.
Footnotes
Competing interests: The authors declare no conflict of Interest.
Funding. This study was funded by a grant from the Rising Tide Foundation and Israel Society of Hematology and Blood transfusion.
References
- 1.Maryanovich M, Oberkovitz G, Niv H, et al. The ATM-BID pathway regulates quiescence and survival of haematopoietic stem cells. Nat Cell Biol. 2012;14(5):535–41. doi: 10.1038/ncb2468. [DOI] [PubMed] [Google Scholar]
- 2.Haran M, Gross A. Balancing glycolysis and mitochondrial OXPHOS: lessons from the hematopoietic system and exercising muscles. Mitochondrion. 2014;19 doi: 10.1016/j.mito.2014.09.007. Pt A3-7. [DOI] [PubMed] [Google Scholar]
- 3.Kulasekararaj AG, Mohamedali AM, Mufti GJ. Recent advances in understanding the molecular pathogenesis of myelodysplastic syndromes. Br J Haematol. doi: 10.1111/bjh.12435. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 4.Greenberg PL, Sun Z, Miller KB, et al. Treatment of myelodysplastic syndrome patients with erythropoietin with or without granulocyte colony-stimulating factor: results of a prospective randomized phase 3 trial by the Eastern Cooperative Oncology Group (E1996) Blood. 2009;114(12):2393–2400. doi: 10.1182/blood-2009-03-211797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Fenaux P, Santini V, Spiriti MAA, et al. A phase 3 randomized, placebo-controlled study assessing the efficacy and safety of epoetin-α in anemic patients with low-risk MDS. Leukemia. 2018;32(12):2648–2658. doi: 10.1038/s41375-018-0118-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.van de Loosdrecht AA, Brada SJ, Blom NR, et al. Mitochondrial disruption and limited apoptosis of erythroblasts are associated with high risk myelodysplasia. An ultrastructural analysis. Leuk Res. 2001;25(5):385–93. doi: 10.1016/S0145-2126(00)00151-X. [DOI] [PubMed] [Google Scholar]
- 7.Gattermann N. From sideroblastic anemia to the role of mitochondrial DNA mutations in myelodysplastic syndromes. Leuk Res. 2000;24(1999):141–151. doi: 10.1016/S0145-2126(99)00160-5. [DOI] [PubMed] [Google Scholar]
- 8.Schildgen V, Wulfert M, Gattermann N. Impaired mitochondrial gene transcription in myelodysplastic syndromes and acute myeloid leukemia with myelodysplasia-related changes. Exp Hematol. 2011;39(6):666–675.e1. doi: 10.1016/j.exphem.2011.03.007. www.mjhid.org. [DOI] [PubMed] [Google Scholar]
- 9.Zhang Q, Steensma DP, Yang J, Dong T, Wu MX. Uncoupling of CD71 shedding with mitochondrial clearance in reticulocytes in a subset of myelodysplastic syndromes. Leukemia. 2019;33(1):217–229. doi: 10.1038/s41375-018-0204-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Nicolson GL, Conklin ÆKA. Reversing mitochondrial dysfunction, fatigue and the adverse effects of chemotherapy of metastatic disease by molecular replacement therapy. Clin Exp Metastasis. 2008:161–169. doi: 10.1007/s10585-007-9129-z. [DOI] [PubMed] [Google Scholar]
- 11.Quinzii CM, Hirano M. Coenzyme Q and mitochondrial disease. Dev Disabil Res Rev. 2010;16(2):183–188. doi: 10.1002/ddrr.108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Galili N, Sechman EV, Cerny J, et al. Clinical response of myelodysplastic syndromes patients to treatment with coenzyme Q10. Leuk Res. 2007;31(1):19–26. doi: 10.1016/j.leukres.2006.04.009. [DOI] [PubMed] [Google Scholar]
- 13.Lee JH, Kim MJ, Park SH, Chae JH, Shin K. Case study of an inborn error manifested in the elderly: A woman with adult-onset mitochondrial disease mimicking systemic vasculitis. Int J Rheum Dis. 2019;22(6):1152–1156. doi: 10.1111/1756-185X.13575. [DOI] [PubMed] [Google Scholar]
- 14.Lowry E, Marley J, McVeigh JG, McSorley E, Allsopp P, Kerr D. Dietary Interventions in the Management of Fibromyalgia: A Systematic Review and Best-Evidence Synthesis. Nutrients. 12(9) doi: 10.3390/nu12092664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hajihashemi P, Askari G, Khorvash F, Reza Maracy M, Nourian M. The effects of concurrent Coenzyme Q10, L-carnitine supplementation in migraine prophylaxis: A randomized, placebo-controlled, double-blind trial. Cephalalgia. 2019;39(5):648–654. doi: 10.1177/0333102418821661. [DOI] [PubMed] [Google Scholar]
- 16.Hirschey MD, Shimazu T, Goetzman E, et al. SIRT3 regulates mitochondrial fatty-acid oxidation by reversible enzyme deacetylation. Nature. 2010;464(7285):121–5. doi: 10.1038/nature08778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Brandenburg NA, Yu R, Revicki DA. Reliability and Validity of the FACT-AN In Patients with Low or Int-1-Risk Myelodysplastic Syndromes with Deletion 5q. Blood. 116(21) doi: 10.1182/blood.V116.21.3827.3827. [DOI] [Google Scholar]
- 18.Mercieca-Bebber R, King MT, Calvert MJ, Stockler MR, Friedlander M. The importance of patient-reported outcomes in clinical trials and strategies for future optimization. doi: 10.2147/PROM.S156279. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Mufti GJ, Bennett JM, Goasguen J, et al. Diagnosis and classification of myelodysplastic syndrome: International Working Group on Morphology of myelodysplastic syndrome (IWGM-MDS) consensus proposals for the definition and enumeration of myeloblasts and ring sideroblasts. Haematologica. 2008;93(11):1712–7. doi: 10.3324/haematol.13405. [DOI] [PubMed] [Google Scholar]
- 20.AMM, JGMA, et al. Comparison of peripheral blood and bone marrow molecular profiling in primary Myelodysplastic Syndromes (MDS) Blood. [Epub ahead of print] [Google Scholar]
- 21.Sriskanthadevan S, Jeyaraju DV, Chung TE, et al. MYELOID NEOPLASIA AML cells have low spare reserve capacity in their respiratory chain that renders them susceptible to oxidative metabolic stress. 2015;125(13):2120–2131. doi: 10.1182/blood-2014-08-594408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Bowen D, Peddie C. Mitochondrial oxygen consumption and ineffective haematopoiesis in patients with myelodysplastic syndromes. Br J Haematol. 2002;118(1):345–346. doi: 10.1046/j.1365-2141.2002.03576_2.x. [DOI] [PubMed] [Google Scholar]
- 23.Dozzo M, Zaja F, Volpetti S, et al. Two cases of concomitant diffuse large B-cell lymphoma and myelodysplastic syndrome. Am J Hematol. 2014;89(10):1011–1013. doi: 10.1002/ajh.23783. [DOI] [PubMed] [Google Scholar]
- 24.Shlush LI. Change comes like a little wind: tales in MDS evolution. Blood. 2016;128(9):1162–3. doi: 10.1182/blood-2016-07-722660. [DOI] [PubMed] [Google Scholar]