Abstract
Background
General practices in England have been encouraged by national policy to work together on a larger scale by creating primary care networks (PCNs). Policy guidance recommended that they should serve populations of 30 000–50 000 people to perform effectively.
Aim
To describe variation in the size and characteristics of PCNs and their populations.
Design and setting
Cross-sectional analysis in England.
Method
Using published information from January 2020, PCNs were identified that contained <30 000, between 30 000–50 000, and >50 000 people. Percentiles were calculated to describe variation in size and population characteristics. PCN composition within each commissioning region was also examined.
Results
In total, 6758 practices had formed 1250 PCNs. Seven hundred and twenty-six (58%) PCNs had the recommended population of 30 000–50 000 people. Eighty-four (7%) PCNs contained <30 000 people. Four hundred and forty (35%) PCNs contained >50 000 people. Thirty-four (3%) PCNs comprised just one practice and 77 (6%) PCNs contained >10 practices. Some PCNs contained more than double the proportions of older people and people with chronic conditions compared to other PCNs. More than half of the population were from very socioeconomically deprived areas in 172 (14%) PCNs. Only six (4%) of the 135 commissioning regions ensured all PCNs were in the recommended population range. All practices had joined a single PCN in three (2%) commissioning regions.
Conclusion
More than 40% of the PCNs were not of the recommended size, and there was substantial variation in their composition and characteristics. This high variability between PCNs is a risk to their future performance.
Keywords: clinical commissioning groups, cross-sectional studies, England, general practice, government, primary care networks, primary health care
INTRODUCTION
In response to concerns about the sustainability of the current model of primary care delivery, NHS England announced its intention to create primary care networks (PCNs) in the NHS Long Term Plan.1 This was a further development of policy to encourage primary care providers to work ‘at scale’.2
PCNs are composed of individual GP practices, led by a clinical director (usually a GP). Prospective PCNs are required to submit a draft network agreement specifying their GP practice members, patient populations, and geographical coverage to their local clinical commissioning group (CCG), the majority of which commission primary care services locally on behalf of NHS England under a delegation arrangement. This process requires CCGs to negotiate the composition of some PCNs with GP practices and approve a local configuration that ensures 100% patient population coverage in each area. PCNs were officially established in July 2019, just 6 months after their initial announcement.3 A national list of PCNs and their members was published in November 2019 and updated in January 2020.
PCNs have a range of intended functions and objectives including:
orchestrating the employment and work of new primary care staff;
ensuring the collaborative delivery of services beyond core general practice;
facilitating closer relationships across a geographical area with other providers and community groups; and
providing a stronger voice for primary care within the broader system.
PCNs will be required to deliver new services to their registered patients set out in seven national services specifications.4 CCGs continue to be the de facto commissioners of primary care services, and will be responsible for monitoring PCN performance and supporting their development.
Guidelines stated that each PCN should contain between 30 000–50 000 registered patients in order to reflect ‘natural communities’5 and allow PCNs to perform their functions effectively.1,6 PCNs of <30 000 patients were only anticipated to be approved by commissioners in ‘exceptional circumstances’; those PCNs approved that had >50 000 people were expected to consider forming smaller neighbourhood teams in order to reflect the population size specified as desirable by the policy.7 In this article, it is considered how well this guidance has been adhered to by the examination of the variations in the size of the PCNs that have emerged. The variations in the demographic, socioeconomic, and epidemiological pressures they face are also summarised. Finally, the configurations of PCNs that have emerged within CCGs are described, as are the new commissioner–provider relationships that have developed.
How this fits in
| New primary care networks (PCNs) have been created in England to encourage collaboration between groups of general practices. Presented here are findings from the first independent national evaluation of the size and characteristics of PCNs. National policy specifies that PCNs would be most effective if they served 30 000–50 000 people. Only 58% of the PCNs that have emerged are within this range, with 7% being smaller and 35% being larger than the recommended population size. Some PCNs face particular challenges, such as those with twice as many older people and people with chronic conditions as other PCNs. The differences in size and characteristics of PCNs will affect their performance, governance, and management. PCNs are the primary vehicle through which new investment is being channelled into general practices. It is therefore important to understand the factors that might affect their ability to utilise that investment effectively and equitably. |
METHOD
Information was obtained from the NHS Digital website about the PCN that each GP practice in England was a core partner of.8 This information was linked to data from NHS Digital on the size and age composition of the populations registered with each GP practice in January 2020.9 To avoid the loss of 44 practices that did not report data in January 2020, population counts were filled in using the most recently reported information. One of the 6758 GP practices in the PCN membership file could not be matched to the registered population data and was removed.
PCNs were classified into three groups according to whether their population size was below, within, or above the recommended size of 30 000–50 000 persons. Variation in population size and numbers of GP practices across PCNs is presented.
The variation across PCNs was quantified by displaying the tenth, the median, and the 90th percentiles for summary measures of the demographic, economic, and epidemiological pressures they face. The decile ratio was also computed.10
The proportion of patients aged ≥65 years was computed for each PCN using the registrations data.9 Data on numbers of patients by GP practice and Lower-level Super Output Area (LSOA) were merged to information on LSOA rurality11 and deprivation,12 and the percentages of the population living in rural areas and in the least and most deprived 20% of areas were calculated.
Prevalence data were obtained for practices from the 2017/2018 Quality and Outcomes Framework (QOF),13 and aggregated to PCN level using population weights. Eight conditions were focused on representing a range of conditions likely to affect patients covered by the service specifications that the PCNs will need to deliver.
The ratio of weighted to unweighted registered population was calculated based on data available on GP practice payments made in the financial year April 2018 to March 2019.14 This measure of relative workload is based on the Global Sum weighted capitation formula.15 It accounts for age and sex, patient need, list turnover, market forces, rurality, and patients in nursing and residential homes.
The data were then aggregated into 135 CCGs, as of April 2020,16 to examine the variation in the commissioner–provider relationships that has emerged. The number of PCNs in each CCG and the percentage of PCNs in the target population range were counted. The percentages of the CCG’s population and practices within their largest PCN were calculated. The ratio of the largest PCN to the smallest for the 132 CCGs with at least two PCNs was also computed.
RESULTS
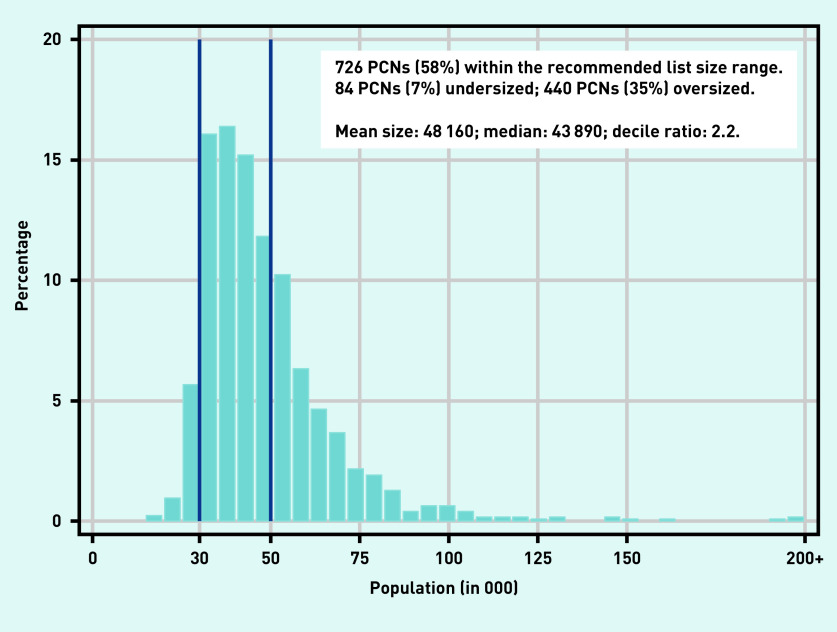
There were 1250 PCNs in January 2020. In Figure 1, the frequency histogram of the population size of each PCN is illustrated. Approximately six out of 10 (58%) PCNs were in the recommended population range of 30 000–50 000. The mean (median) size of a PCN is 48 000 (44 000) registered patients. About 7% of PCNs cover a list size population <30 000, with 1% of the total covering <24 000 patients. About 35% of PCNs have a population above the recommended range, with 5% of the total having >80 000 registered patients.
Figure 1.
Variation in the size of the registered population across PCNs.a
aThe decile ratio is the ratio of the upper bound value of the ninth decile (that is, the 10% of PCNs with highest values, P90 = 69 200 patients) to that of the first (P10 = 31 100 patients). PCN = primary care network. P10 = tenth percentile score. P90 = 90th percentile score.
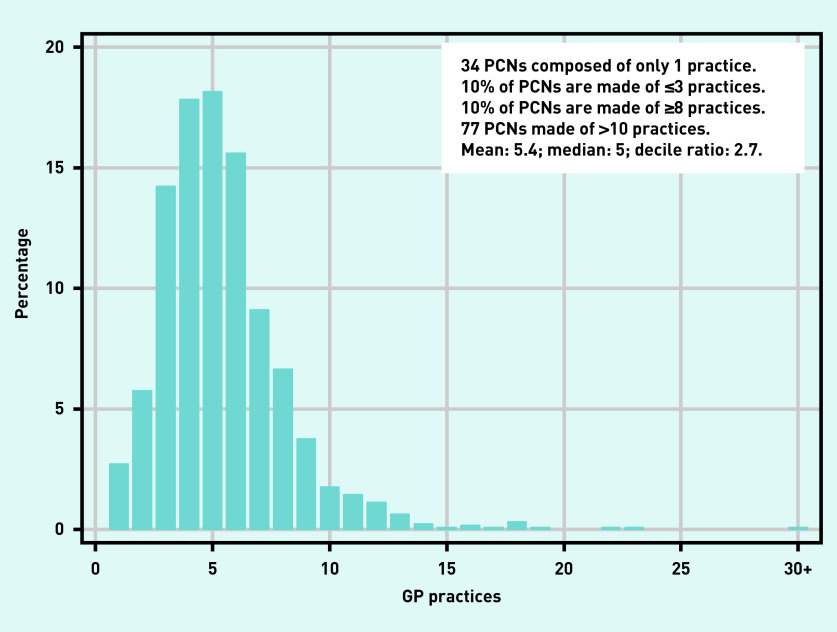
On average, a PCN is composed of five practices, with considerable variation around the mean (Figure 2). One-tenth of PCNs are formed by three practices or less. Another tenth is composed of eight or more practices. At the extremes, 34 PCNs comprise a single practice while 77 PCNs contain >10 practices.
Figure 2.
Variation in the number of GP practices across PCNs.a
aThe decile ratio is the ratio of the upper bound value of the ninth decile (that is, the 10% of PCNs with highest values, P90 = 3 practices) to that of the first (P10 = 8 practices). PCN = primary care network. P10 = tenth percentile score. P90 = 90th percentile score.
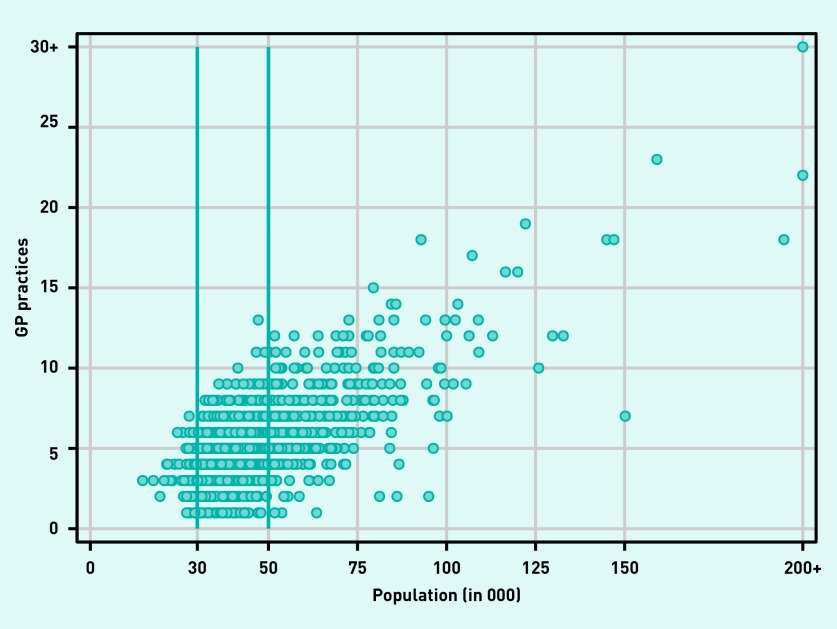
Figure 3 illustrates the joint variation in size of registered population and number of member practices across PCNs. Although the two measures of size are correlated, there is substantial variation in both dimensions. Even within the suggested range of population size of 30 000–50 000 there is much variation in the number of practices involved. Some peculiar PCN configurations, with a high number of patients and a relatively small number of practices, are located outside the range. For example, there are PCNs that contain only two (super-) practices but cover nearly 100 000 people. Similarly, there are PCNs with a large number of patients covered by a multitude of GP practices.
Figure 3.
Scatterplot of number of GP practices and size of registered population across primary care networks.
Table 1 shows the variation across PCNs in some key characteristics of the population they cover. There is substantial variation in the challenges that PCNs will face to meet the needs of their populations. On average, about 18% of patients in PCNs are aged ≥65 years. However, when ranking PCNs according to the proportion of older people they cover, a 2.8-fold difference is found between the tenth (9.2%) and the 90th (25.6%) percentile.
Table 1.
Variation in the demographic, socioeconomic, and epidemiological characteristics across PCNs
| Population characteristic, %a | Mean | 10th percentile | Median | 90th percentile | Decile ratiob |
|---|---|---|---|---|---|
| Aged ≥65 years | 17.7 | 9.2 | 18 | 25.6 | 2.8 |
|
| |||||
| Living in rural area | 17.2 | 0 | 2.5 | 60.1 | — |
|
| |||||
| Living in deprived areac | 20.6 | 0 | 12.8 | 55.6 | — |
|
| |||||
| Living in affluent areac | 19.2 | 0.3 | 12.3 | 50.3 | — |
|
| |||||
| Diagnosed with:d | |||||
| Chronic obstructive pulmonary disease | 1.9 | 1.0 | 1.9 | 2.9 | 2.9 |
| Chronic kidney disease | 4.1 | 2.2 | 4.1 | 6.2 | 2.8 |
| Diabetes | 7.0 | 5.1 | 7.0 | 8.8 | 1.7 |
| Cardiovascular disease | 1.1 | 0.8 | 1.1 | 1.5 | 1.8 |
| Hypertension | 14.1 | 10.0 | 14.4 | 17.6 | 1.8 |
| Stroke and transient ischaemic attack | 1.8 | 1.0 | 1.8 | 2.5 | 2.6 |
| Serious mental illness | 1.0 | 0.7 | 0.9 | 1.3 | 2.0 |
| Obesity | 8.1 | 5.0 | 8.0 | 11.0 | 2.2 |
|
| |||||
| Workload indexe | 1.01 | 0.9 | 1.01 | 1.11 | 1.2 |
Unless otherwise stated.
The decile ratio is the ratio of the upper bound value of the ninth decile (that is, the 10% of PCNs with highest values, P90) to that of the first (P10).
Population living in the 20% most deprived/affluent Lower-level Super Output Areas according to the 2019 Index of Multiple Deprivation.
Statistics computed over 1249 PCNs using prevalence data from the 2017/18 Quality and Outcomes Framework.
Weighted registered population divided by unweighted registered population based on the weighted capitation formula. P10 = tenth percentile score. P90 = 90th percentile score. PCN = primary care network.
Marked differences were found when PCNs were ranked according to their coverage of patients living in rural areas and associated area levels of deprivation. Although about 10% of PCNs cover populations that are almost entirely located in urban or deprived areas, another 10% cover patients largely (>60%) living in urban areas. Similarly, there are some PCNs that cover populations mainly living in the most deprived areas (90th percentile score = 55.6%) whereas others tend to have patients living in the most affluent areas.
PCNs differ also in terms of the needs of the patients they cover. One-tenth of PCNs face prevalence rates ranging between 70% (for diabetes) and almost three times lower (for chronic obstructive pulmonary disease [COPD] and chronic kidney disease [CKD]) than the highest tenth. The workload factor in the lowest tenth of PCNs is on average 20% lower than that observed in the highest tenth.
For a stratification of these key characteristics by PCN size, see Supplementary Table S1. Undersized PCNs tend to serve patients living in rural areas who are considerably older, with higher prevalence rates of diagnosed conditions than patients served by PCNs that are above or within the recommended population range.
The median CCG deals with six PCNs (mean of 9.3), but with significant variation ranging from one PCN (three CCGs) to >42 PCNs in one CCG (Table 2). The number of PCNs in one-tenth of CCGs is 4.5 times lower than that in another tenth. Over half of the PCNs in a CCG are within the list size range, with a three-fold difference from the lowest tenth (25%) to the highest tenth (80%). Only six of the 135 CCGs managed to get all PCNs in the targeted list size. In seven CCGs, all PCNs are outside the expected list size range.
Table 2.
Variation in the PCN configurations across CCGs
| Mean | P10 | Median | P90 | Decile ratioa | |
|---|---|---|---|---|---|
| PCNs, n | 9.3 | 4.0 | 6.0 | 18.0 | 4.5 |
| PCNs in target population size range, % | 54.8 | 25.0 | 57.1 | 80.1 | 3.2 |
| CCG population in CCG’s largest PCN, % | 24.2 | 9.6 | 21.7 | 40.4 | 4.2 |
| CCG practices in CCG’s largest PCN, % | 25.5 | 10.8 | 22.2 | 40.0 | 3.7 |
| Ratio of largest to smallest PCN population in the CCGb | 2.4 | 1.5 | 2.2 | 3.5 | 2.4 |
The decile ratio is the ratio of the upper bound value of the ninth decile (that is, the 10% of PCNs with highest values, P90) to that of the first (P10).
Analysis restricted to 132 CCGs (over 135) with at least two PCNs.
CCG = clinical commissioning group. P10 = tenth percentile score. P90 = 90th percentile score. PCN = primary care network.
On average, around one-quarter of a CCG’s population are covered by its largest PCN, with large dispersion around this figure (decile ratio = 4.2). Similarly, one-quarter of practices in a CCG are associated with the largest PCN. However, one-tenth of CCGs have about 11% of the total practices nested in the largest PCN, whereas another tenth of CCGs have 40% of their practices affiliated with the largest PCN. Among the 132 CCGs with at least two PCNs, the largest PCN is approximately 2.4 times the size of the smallest, but with considerable variation around this figure (decile ratio = 2.4).
DISCUSSION
Summary
The precise form and purpose of PCNs has evolved since their initial announcement and is still under negotiation. It is likely, however, that PCNs will become a feature of the inter-organisational landscape of the English NHS for years to come, and represent a network model that is part of a broader trend of organisational delivery.
The aim of this study was to describe the variation in size and characteristics of PCNs and their populations in the context of policy recommendations about the population size that was required to perform effectively. It was found that approximately 60% of PCNs are within the recommended range of 30 000–50 000 population. A significant proportion (35%) were above the range, while 7% were undersized. PCNs vary also in terms of the number of associated GP practices. There is a range of different organisational structures, from PCNs composed of a single practice (often a super-practice) to PCNs composed of >10 practices. Although large PCNs tend to be formed by a larger number of practices, this is not always the case. Some peculiar PCN configurations have emerged, most notably the case of PCNs composed of a relatively small number of practices covering large populations. Marked differences were also documented in the sociodemographic and epidemiological pressures that PCNs face, with undersized PCNs serving higher proportions of people living in rural areas, predominantly older people,17 and people with associated healthcare needs.
One particular implication concerns the relationships between PCNs and their commissioners. CCGs continue to be the (delegated) purchasers of primary care services in most areas, and so will be responsible for operationalising the PCN contract locally and monitoring PCN performance.3 They may also have a role in the future in distributing incentive payments associated with the ‘investment and impact funding’ stream, and will continue to be responsible for negotiating existing additional local contracts (known as ‘locally enhanced services’).
The ability of CCGs to perform their core functions of purchasing, regulation, and financing may depend on the relative sizes of the PCNs that have emerged in their area. This study has documented some of these differences, and noted that the bargaining power may be stronger for large PCNs in some CCGs. Where there are few PCNs, the new provider groups may be able to take advantage of the strength of their position in local negotiations. Where there are multiple PCNs, the purchasers will be able to undertake benchmarking and make the most of the purchasing power. However, it may also be the case that some of those PCNs above or below the suggested size were able to successfully negotiate their composition because they possessed sufficient power to do so, and these PCNs may enjoy relatively higher degrees of influence in their local systems.
Strengths and limitations
This article presents findings from the first independent national evaluation of the size and characteristics of 1250 PCNs using the latest released (January 2020) administrative data, made available through NHS England combined with other administrative sources. To avoid the loss of GP practices that had missing values in one of the indicators used for the analysis, gaps were filled in using the latest information available. Although this approach may not accurately reflect current practice in the context of rapid changes in population size and structures, it permitted a fuller representation of PCNs in England. Only one GP practice was omitted from the analysis; this practice served mainly asylum seekers and refugees, and as such it was not possible to gather population characteristics for this practice.
Practices were treated with the same surgery codes as single providers. In other words, it was not possible to identify, and treat as a single entity, pre-existing practice ventures (for example, ‘super partnerships’) whose members have retained separate surgery codes.2 This would reduce the number of delivery units within a PCN, affecting the results presented in Figures 2 and 3. However, there is no up-to-date national dataset on these super-partnerships.
Comparison with existing literature
A descriptive analysis of the variation in population size of PCNs has been published online.18 That analysis was extended by this study in several ways. First, variation in size with respect to list size population and number of practices involved was documented systematically. Second, the analysis was extended to a range of sociodemographic and health indicators. Third, some of the complexities CCGs may face in operationalising their roles as local commissioner, regulator, and financer were highlighted.
Implications for research and practice
The variation in the size, composition, and characteristics of PCNs is a consequence of the decision to allow practices to choose the local configuration of their PCN (albeit with CCG oversight).19 This may help to ensure that there are good collaborative relationships between the constituent members. However, at present, little is known about practice-level satisfaction with local PCN arrangements or the strength of inter-practice relationships. These will be crucial to the delivery of collaborative services in the future.
The variability documented also creates considerable challenges for all parties involved. PCNs will face different organisational challenges in delivering services contingent on their size, the characteristics of the populations they serve, and the delivery units they will contain. Furthermore, CCGs are likely to face a variety of commissioner–provider relationships with newly developed PCNs. For example, one of the intended roles for PCNs is to deliver services collaboratively between practices, working closely with other providers such as community service providers and voluntary sector organisations. The configuration of PCNs in a given local area will materially affect the development of such collaborations, as large providers may be required to engage with multiple PCNs, which may differ significantly in their organisation and ways of working.
CCGs are working in a rapidly changing context, with many merging to form larger groups20 and some uncertainty around their role in newly developing integrated care systems.21 Research suggests effective commissioning of primary care services requires detailed local knowledge of practices and populations.22 Relationships between commissioners and their local PCNs will therefore be crucial in determining the outcomes associated with the new policy. This analysis suggests that there will be significant variation in the workload connected with the development and maintenance of these important relationships.
Acknowledgments
The authors are grateful to the wider team members and the advisory group for their suggestions in all phases of the research.
Funding
This research was carried out by the Policy Research Unit in Health and Social Care Systems and Commissioning (PRUComm). PRUComm is funded by the National Institute for Health Research (NIHR) Policy Research Programme (reference number: PR-PRU-1217-20801). The views expressed are those of the authors and not necessarily those of the NIHR or the Department of Health and Social Care.
Ethical approval
Ethical approval was not required for this study.
Provenance
Freely submitted; externally peer reviewed.
Competing interests
The authors have declared no competing interests.
Discuss this article
Contribute and read comments about this article: bjgp.org/letters
REFERENCES
- 1.NHS The NHS Long Term Plan. 2019 https://www.longtermplan.nhs.uk/publication/nhs-long-term-plan (accessed 27 Oct 2020). [Google Scholar]
- 2.Forbes LJ, Forbes H, Sutton M, et al. How widespread is working at scale in English general practice? An observational study. Br J Gen Pract. 2019 doi: 10.3399/bjgp19X705533. [DOI] [PMC free article] [PubMed]
- 3.Fisher R, Thorlby R, Alderwick H. Briefing: understanding primary care networks. The Health Foundation. 2019 https://www.healthwatchswindon.org.uk/sites/healthwatchswindon.org.uk/files/Understanding%20primary%20care%20networks.pdf (accessed 27 Oct 2020). [Google Scholar]
- 4.NHS England Investment and evolution: Update to the GP contract agreement 2020/21–2023/24. 2020 https://www.england.nhs.uk/publication/investment-and-evolution-update-to-the-gp-contract-agreement-20-21-23-24 (accessed 27 Oct 2020).
- 5.NHS England Primary Care Networks: Frequently asked questions. 2019 https://www.england.nhs.uk/wp-content/uploads/2019/04/pcn-faqs-000429.pdf (accessed 27 Oct 2020).
- 6.British Medical Association . The primary care network handbook. London: 2019. https://www.bma.org.uk/media/2144/bma-pcn-handbook-march-2020.pdf (accessed 27 Oct 2020). [Google Scholar]
- 7.NHS England Primary Care Networks: frequently asked questions: second iteration. 2019 https://www.england.nhs.uk/wp-content/uploads/2019/03/pcn-faqs-may-2019.pdf (accessed 27 Oct 2020).
- 8.NHS Digital Primary Care Networks (epcn). In GP and GP practice related data. https://digital.nhs.uk/services/organisation-data-service/data-downloads/gp-and-gp-practice-related-data (accessed 27 Oct 2020).
- 9.NHS Digital Patients registered at a GP practice. https://digital.nhs.uk/data-and-information/publications/statistical/patients-registered-at-a-gp-practice (accessed 27 Oct 2020).
- 10.Gravelle H, Sutton M. Inequality in the geographical distribution of general practitioners in England and Wales 1974–1995. J Health Serv Res Policy. 2001;6(1):6–13. doi: 10.1258/1355819011927143. [DOI] [PubMed] [Google Scholar]
- 11.Office for National Statistics Rural urban classification 2011 of Lower Layer Super Output Areas in England and Wales. 2018 https://data.gov.uk/dataset/b1165cea-2655-4cf7-bf22-dfbd3cdeb242/rural-urban-classification-2011-of-lower-layer-super-output-areas-in-england-and-wales (accessed 27 Oct 2020).
- 12.Ministry of Housing Communities & Local Government English indices of deprivation. 2019 https://www.gov.uk/government/statistics/english-indices-of-deprivation-2019 (accessed 27 Oct 2020).
- 13.NHS Digital Quality and Outcomes Framework, achievement, prevalence and exceptions data 2018–19. 2019 https://digital.nhs.uk/data-and-information/publications/statistical/quality-and-outcomes-framework-achievement-prevalence-and-exceptions-data/2018-19-pas (accessed 27 Oct 2020).
- 14.NHS Digital NHS payments to general practice — England, 2018/19. 2019 https://digital.nhs.uk/data-and-information/publications/statistical/nhs-payments-to-general-practice/england-2018-19 (accessed 27 Oct 2020).
- 15.British Medical Association Focus on the global sum allocation formula (Carr-Hill Formula) 2015 https://www.gloslmc.com/downloads/GPC%20Guidance%20Docs/1507%20Focus%20on%20the%20Global%20Sum%20Allocation%20Formula%20-%20July%202015.pdf (accessed 27 Oct 2020).
- 16.NHS Digital Changes to organisation reference data: sustainability and transformation partnerships reconfiguration. 2020 https://digital.nhs.uk/services/organisation-data-service/changes-to-ord-stp-reconfiguration (accessed 27 Oct 2020).
- 17.Department for Environment, Food & Rural Affairs Rural population and migration. 2020 https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/862320/Rural_population_and_migration_Jan_20.pdf (accessed 27 Oct 2020).
- 18.Bostock N. More than 2 in 5 PCNs not on ‘natural’ scale envisaged by NHS England. 2020 https://www.gponline.com/2-5-pcns-not-natural-scale-envisaged-nhs-england/article/1669532 (accessed 27 Oct 2020).
- 19.NHS England, British Medical Association Investment and evolution: a five-year framework for GP contract reform to implement the NHS Long Term Plan. 2019 https://www.england.nhs.uk/wp-content/uploads/2019/01/gp-contract-2019.pdf (accessed 27 Oct 2020). [Google Scholar]
- 20.NHS Digital Change summary — 2020 STP, CCG and Commissioning Hub reconfiguration. https://digital.nhs.uk/services/organisation-data-service/change-summary---stp-reconfiguration#what-we-are-changing-on-1-april-2020 (accessed 27 Oct 2020).
- 21.British Medical Association Briefing: integrated care systems. 2019 https://www.bma.org.uk/media/1978/bma-integrated-care-systems-briefing-jan-19.pdf (accessed 27 Oct 2020).
- 22.Checkland K, McDermott I, Coleman A, et al. Planning and managing primary care services: lessons from the NHS in England. Public Money & Management. 2018;38(4):261–270. [Google Scholar]