Abstract
Background:
Options to support adherence to physical activity in moderate-to-severe multiple sclerosis (MS) are needed. The primary aim was to evaluate adherence to a Web-based, individualized exercise program in moderate-to-severe MS. Secondary aims explored changes in 29-item Multiple Sclerosis Impact Scale, Hospital Anxiety and Depression Scale (HADS), grip strength, Timed 25-Foot Walk test, and Timed Up and Go (TUG) results.
Methods:
Participants were randomized (2:1) to a physiotherapist-guided Web-based home exercise program or a physiotherapist-prescribed written home exercise program. The primary outcome was adherence (number of exercise sessions over 26 weeks). Secondary outcomes were described in terms of means and effect sizes.
Results:
There were 48 participants: mean ± SD age, 54.3 ± 11.9 years; disease duration, 19.5 ± 11.0 years; and Patient-Determined Disease Steps scale score, 4.4 ± 1.6. There was no significant difference in mean ± SD adherence in the Web-based group (38.9 ± 28.1) versus the comparator group (34.6 ± 40.8; U = 198.5, P = .208, Hedges’ g = 0.13). Nearly 50% of participants (23 of 48) exercised at least twice per week for at least 13 of the 26 weeks. Adherence was highest in the Web-based subgroup of wheelchair users. Medium effect sizes were found for the HADS anxiety subscale and in ambulatory participants for TUG. There were no adverse events.
Conclusions:
There was no difference in exercise adherence between the Web-based and active comparator groups. There was no worsening of secondary outcomes or adverse events, supporting the safety of Web-based physiotherapy. More research is needed to determine whether wheelchair users might be most likely to benefit from Web-based physiotherapy.
Keywords: Adherence, Exercise, Multiple sclerosis (MS), Physiotherapy, Telerehabilitation
Despite the benefits of physical activity, adherence to regular physical activity when living with multiple sclerosis (MS) can be challenging.1–3 Physical activity programs must be flexible and evolve as MS symptoms and impairments change over time. Participation in physical activity may be enhanced through the provision of personalized programming with ongoing monitoring and professional support.4,5
Physical activity specifically in people with more advanced disability is associated with improvements in cardiorespiratory and muscular fitness and quality of life in the short-term.6 Structured exercise involving strength training and/or aerobic exercise at least twice a week seems to be tolerated and safe in people with more advanced disability.6 In advanced MS, supported programs with specialized equipment (ie, bodyweight-supported treadmill walking, cycle ergometry, rowing, or aquacise) are commonly reported. Access to professional support and specialized equipment for exercise is a challenge, especially in areas with a high MS prevalence but low population density, as is the case in Saskatchewan, Canada.7
A key question remains concerning how best to support persons with MS in participating in and adhering to their exercise programs. Various Web-based approaches have been proposed to meet this challenge. A recent systematic review of Web-based physical activity interventions concluded that Web-based approaches increased physical activity levels in people with mild-to-moderate MS who were ambulatory.8 The Web-based interventions were largely of shorter duration (ie, <3 months) and included wait-listed comparison groups.8 More research is needed to determine whether Web-based approaches are also appropriate for increasing adherence to physical activity through structured exercise programs for people with more moderate-to-severe MS.
The primary objective of this Saskatchewan-based study was to improve physical activity adherence in people with moderate-to-severe MS through a personalized, physiotherapist-prescribed Web-based exercise program over 6 months compared with a usual care exercise group. Secondary objectives of this pilot study were to explore changes in patient-reported symptoms according to the 29-item Multiple Sclerosis Impact Scale (MSIS-29) and the Hospital Anxiety and Depression Scale (HADS) and changes in physical function as measured by dominant-hand dynamic grip strength, the Timed 25-Foot Walk test (T25FW), and the Timed Up and Go (TUG) test.
Methods
This single-blinded pilot study invited people with MS with moderate-to-severe disability. We advertised for the study at the Saskatchewan MS Clinic and through the MS Society of Canada. The inclusion criteria were clinically definite MS, moderate-to-severe disability (Patient-Determined Disease Steps [PDDS] scale score of 2–7),9,10 age 18 years or older, and ability to access the internet from their current living environment. For participants not recruited through the MS clinic, consent was obtained to access their medical records from the treating neurologist to confirm the MS diagnosis. The exclusion criteria were current participation in exercise twice a week or more; residence greater than 300 km from Saskatoon, Saskatchewan, Canada; or severe cognitive impairment. Participants needed to demonstrate an ability to provide informed consent according to the clinical judgment of the research physiotherapists. No formal cognitive assessment tool was used to determine eligibility. The 300-km maximum distance, if not able to travel to Saskatoon for assessment visits, was chosen to allow the physiotherapists time to complete a home-visit assessment in 1 day. No monetary incentives were awarded for participating in or completing the study.
Participants were randomly assigned in a 2:1 ratio to either a Web-based exercise group (intervention) or a usual care exercise group (active comparator). We chose to allocate more participants to the intervention group because this approach can be advantageous in early trials exploring the feasibility or safety of an intervention.11 This was the first study we are aware of that explored including wheelchair users in a Web-based exercise intervention. Randomization was stratified according to self-reported method of usual community mobility: those reporting not using wheeled mobility and those using wheeled mobility most of the time. Randomized lists were created before the first participant’s first visit using an online service (www.random.org). Data collection occurred from March 2017 to October 2018. This study was approved by the University of Saskatchewan Biomedical Research Ethics Board and registered on ClinicalTrials.gov (study number: NCT03039400).
Interventions
At the baseline in-person visit, physiotherapists created and prescribed exercise programs and exercise monitoring diaries. Physiotherapists discussed maintaining function as part of the goal-setting process (ie, exercises for trunk control in sitting, upper-limb function for self-care, and lower-limb function for transfers). Programs were individualized in terms of exercises, level of difficulty, and number of sets and repetitions. A minimum of twice-per-week exercise sessions for 6 months was prescribed for all the participants (2 × 26 weeks = 52 exercise diary entries). Physiotherapists informed their participants to expect one follow-up telephone call from the physiotherapist at the end of the first week. The purpose of the follow-up call was to ensure that participants could access their exercise programs and that they had no questions or concerns about their program.
Nine physiotherapists were trained on the study protocol; seven provided exercise prescription and blinded assessments, and two provided only blinded assessments. Training of physiotherapists on the study protocol occurred in small groups or individual sessions, all led by a physiotherapist researcher (S.J.D.). All physiotherapists providing exercise prescription for the study had expertise in neurorehabilitation and a minimum of 5 years’ experience working with people with MS.
Intervention Arm
Individuals in the Web-based group had their exercise program and diary set up at the baseline in-person visit on webbasedphysio.com (now www.giraffehealth.com). The website contains exercises (videos, text and audio descriptions), which are individually prescribed by a physiotherapist at an initial assessment.12,13 The physiotherapist is able to review the electronic exercise diaries and remotely alter the exercises in response to comments from participants. The inventory of exercises and the educational materials were previously developed with input from people living with MS in the United Kingdom with mild-to-moderate disability.13 For this pilot study, a half-day focus group was held with two patient advisors with advanced disability secondary to MS, a physiatrist (K.B.K.), and four experienced physiotherapists, including the originator of webbasedphysio (L.P.). The purpose of the focus group was to create an additional inventory of exercises for the Web-based platform acceptable to people with more advanced disability. Additions included seated versions of existing exercises and novel exercises that focused on core and upper-extremity strength. Participants in the Web-based intervention arm were informed that every 2 weeks for the 6-month intervention period, the treating physiotherapist would review their online exercise diary and remotely alter their exercise program as appropriate by changing exercises, level of difficulty, and/or number of repetitions. Participants were also invited to contact their physiotherapist for a change in their program as needed. Online exercise diaries were collected on an ongoing basis.
Comparator Arm
Participants in the usual care exercise group were given a written, home-based exercise program consistent with the most common method for exercise prescription practice for outpatient physiotherapy services at our site. Participants were asked to keep an exercise diary, in paper format, and mail it to the study coordinator at the study midpoint (3 months) and end point (6 months). For this group, physiotherapists did not review the exercise diaries. Participants were advised that they could e-mail their physiotherapist to request a change in their program as needed.
Demographic data, including sex, age, PDDS scale score,9,10 disease duration, typical community ambulation status (walk vs wheel), and residence location, were collected. The PDDS scale is a self-assessment measure of disability status, primarily oriented to walking. For example, category 2 (moderate disability) notes no limitations in walking but acknowledges significant problems that limit activities in other ways. For category 7 (wheelchair/scooter use), a wheelchair is the main form of mobility, and walking is limited to less than 25 feet.
Outcomes
The primary outcome of exercise adherence was calculated as the number of exercise sessions over the study period of 26 weeks. All the participants were asked to keep an exercise diary, detailing their participation in their prescribed exercise sessions. If participants met the recommended participation adherence of exercise sessions twice per week, they would have participated in at least 52 exercise sessions during the study period.
Secondary outcomes included MSIS-29 score, HADS score, dynamic grip strength and fatigability, T25FW score, TUG test score, and fall history. The MSIS-29 is an MS-specific symptom measure that inquires about symptom effect on day-to-day life in the past 2 weeks.14 The HADS is a brief measure containing 14 questions.15 It is designed to detect the presence and severity of anxiety and depression and has been validated in an MS population. Dynamic grip strength and fatigability were measured for the dominant hand using a portable hand dynamometer. Participants performed 15 maximum voluntary contractions in a row. Handgrip fatigability was calculated as a percentage decrease from the maximum voluntary contraction in the first three squeezes to the maximum voluntary contraction in the last three squeezes.16 The T25FW and the TUG test are validated measures for the assessment of mobility in MS and were used with ambulatory participants.17,18 Assessments were completed at the baseline appointment before the physiotherapist learning of the participant’s random assignment. Study exit (6-month) assessments were completed by a physiotherapist blinded to the participant’s group assignment. Blinded physiotherapists also collected fall history in the previous 3 months by participant self-report at baseline and study exit.
Analyses
For the primary outcome, adherence is described using mean ± SD, and the distributions between groups were compared at 6 months using the Mann-Whitney U test. Hedges’ g was calculated for effect size. Hedges’ g is a member of the Cohen’s d family of effect sizes and is interpreted in a similar manner: as a proportion of the pooled SD. Cohen proposed conventions for interpreting these effect sizes as small (d = 0.2), medium (d = 0.5), or large (d = 0.8).19 Adherence was performed on an intention-to-treat basis. We chose to replace all missing values for exercise adherence with zero because this is the most conservative approach, making the assumption for the worst possible adherence outcome, ie, no exercise performed. To explore the differences in adherence between those who were community walkers and those who were community wheelchair users, mean ± SD values were calculated.
For exploration of the secondary outcomes, mean ± SD values were described at baseline and at 6 months. Effect sizes for paired data (Cohen’s dz = t/√n) were calculated for within-group changes in secondary outcomes for the Web-based group, the comparator group, and the total study sample. Analysis of secondary outcomes was performed only on available data. For returned patient-reported questionnaires, missing items were replaced with the participant’s scale mean.
Results
Forty-eight people participated in the study: 32 in the Web-based group and 16 in the comparator group. Demographic characteristics are summarized in Table 1. Nine participants withdrew from the study before the midpoint: six (19%) from the Web-based group and three (19%) from the comparator group (Figure S1, which is published in the online version of this article at ijmsc.org). Reasons for withdrawal were hospitalization unrelated to the study protocol (n = 1), personal reasons related to relocation or family stressors (n = 3), and no reason provided (n = 5). No adverse events were reported related to the study protocol. Of the 48 participants, 21 (44%) reported no falls in the 3 months before baseline, 13 (27%) reported one fall, eight (17%) reported two falls, and six (13%) reported three or more falls. In the 3 months before study exit, of the 36 participants with fall data, 20 (56%) reported no falls, eight (22%) reported one fall, two (6%) reported two falls, and six (17%) reported three or more falls (12 participants were missing fall data at study end).
Table 1.
Demographic characteristics at baseline
| Characteristic | Web-based group (n = 32) | Comparator group (n = 16) | Total (N = 48) |
|---|---|---|---|
| Female sex | 20 (63) | 11 (69) | 31 (65) |
| Age, y | 54.6 ± 11.9 | 53.8 ± 12.2 | 54.3 ± 11.9 |
| PDDS scale score | 4.2 ± 1.6 | 4.8 ± 1.7 | 4.4 ± 1.6 |
| Disease duration from onset, y | 20.0 ± 11.3 | 18.4 ± 10.7 | 19.5 ± 11.0 |
| Community wheelchair users | 9 (28) | 5 (31) | 14 (29) |
| Residence | |||
| City | 18 (56) | 6 (38) | 24 (50) |
| Small city | 7 (22) | 2 (13) | 9 (19) |
| Town | 4 (13) | 6 (38) | 10 (21) |
| Rural | 3 (9) | 2 (13) | 5 (10) |
Note: Values are given as number (percentage) or mean ± SD.
Abbreviation: PDDS, Patient-Determined Disease Steps.
The mean ± SD number of exercise sessions for the Web-based group was 38.9 ± 28.1 and for the comparator group was 34.6 ± 40.8. The difference between group distributions for the primary adherence outcome was not significant (U = 198.5, P = .208). Hedges’ g was 0.13. Percentages of participants completing at least two exercise sessions in each week of the study are displayed in Figure 1. Considering the entire sample, almost 50% of participants (23 of 48) exercised two or more times per week for at least half of the 26-week study period.
Figure 1.
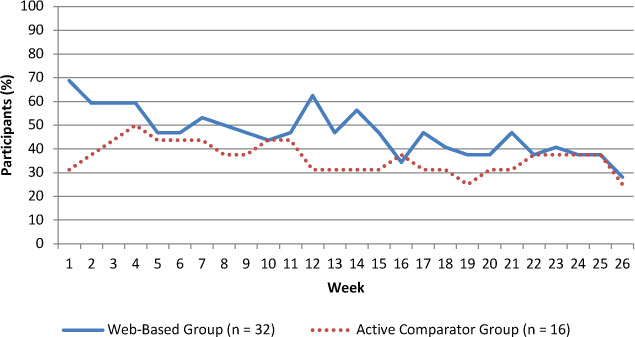
Percentages of participants exercising at least twice per week
Only 16 of the 32 diaries expected to be returned from the 16 originally enrolled participants in the comparator group were returned. This resulted in a disproportionate volume of missing data being replaced with zeroes in the comparator group for the adherence analyses.
In exploratory analyses, the highest group mean ± SD number of exercise sessions was seen in community wheelchair users in the Web-based exercise group (51.6 ± 28.9) (Table 2).
Table 2.
Number of exercise sessions for community walkers and community wheelchair users over 26 weeks
| Participants | PDDS scale score | Exercise sessions | ||
|---|---|---|---|---|
| Web-based group | Comparator group | Total sample | ||
| Community walkers | 3.75 ± 1.39 (median = 4) | 34.0 ± 26.8 (n = 23) | 34.0 ± 45.3 (n = 11) | 34.0 ± 33.2 (n = 34) |
| Community wheelchair users | 6.07 ± 0.73 (median = 6) | 51.6 ± 28.9 (n = 9) | 36.0 ± 33.5 (n = 5) | 46.0 ± 30.3 (n = 14) |
Note: Values are given as mean ± SD unless otherwise indicated. Target number of sessions per participant = 2 × per week × 26 weeks = 52 sessions.
Abbreviation: PDDS, Patient-Determined Disease Steps.
Results for most secondary outcomes are displayed in Table 3. The mean values at study exit were not worse than those at baseline, with moderate effect sizes seen for improvement in both groups for the HADS anxiety subscale (dz = 0.58) and among ambulatory participants for the TUG test (dz = 0.61). Medium effect sizes were also found for the MSIS-29 psychological scale in the Web-based group (dz = 0.65).
Table 3.
Secondary outcomes
| Outcome | Web-based group | Comparator group | Total sample |
|---|---|---|---|
| MSIS-29 physical scale score | |||
| Baseline | 38.4 ± 15.4 | 38.1 ± 10.4 | 38.3 ± 13.9 |
| Exit | 36.2 ± 18.9 | 35.1 ± 14.8 | 35.8 ± 17.5 |
| dz | 0.26 (n = 25) | 0.20 (n = 11) | 0.23 (n = 36) |
| MSIS-29 psychological scale score | |||
| Baseline | 29.9 ± 18.1 | 29.5 ± 16.4 | 29.8 ± 17.4 |
| Exit | 25.3 ± 18.9 | 26.8 ± 18.9 | 25.8 ± 18.6 |
| dz | 0.65a (n = 25) | 0.13 (n = 11) | 0.32 (n = 36) |
| HADS anxiety scale score | |||
| Baseline | 7.6 ± 4.2 | 7.8 ± 4.2 | 7.7 ± 4.1 |
| Exit | 6.2 ± 4.3 | 6.4 ± 4.4 | 6.3 ± 4.3 |
| dz | 0.58a (n = 25) | 0.53a (n=11) | 0.58a (n = 36) |
| HADS depression scale score | |||
| Baseline | 7.0 ± 4.0 | 6.1 ± 3.5 | 6.8 ± 3.8 |
| Exit | 6.2 ± 3.9 | 5.6 ± 3.6 | 6.0 ± 3.8 |
| dz | 0.35 (n = 25) | 0.25 (n = 11) | 0.33 (n = 36) |
| TUG test, s | |||
| Baseline | 15.6 ± 14.0 | 20.5 ± 19.5 | 17.1 ± 15.7 |
| Exit | 13.1 ± 10.5 | 17.6 ± 14.5 | 14.5 ± 11.8 |
| dz | 0.62a (n = 18) | 0.56a (n = 8) | 0.61a (n = 26) |
| T25FW, s | |||
| Baseline | 9.0 ± 6.1 | 20.3 ± 30.9 | 12.6 ± 18.2 |
| Exit | 8.9 ± 6.6 | 15.9 ± 17.2 | 11.1 ± 11.3 |
| dz | 0.04 (n = 17) | 0.29 (n = 8) | 0.17 (n = 25) |
| Dominant-hand maximal voluntary contraction, kg | |||
| Baseline | 27.2 ± 10.6 | 29.8 ± 10.7 | 28.0 ± 10.5 |
| Exit | 29.3 ± 13.0 | 29.1 ± 10.7 | 29.2 ± 12.2 |
| dz | −0.29 (n = 23) | 0.12 (n = 10) | −0.18 (n = 33) |
| Dominant-hand dynamic fatigue index, % | |||
| Baseline | 19.1 ± 23.5 | 16.1 ± 10.6 | 18.2 ± 20.4 |
| Exit | 7.5 ± 10.8 | 11.6 ± 21.7 | 8.7 ± 14.7 |
| dz | 0.49 (n = 23) | 0.30 (n = 10) | 0.44 (n = 33) |
Note: Values are given as mean ± SD unless otherwise indicated.
Abbreviations: HADS, Hospital Anxiety and Depression Scale; MSIS-29, 29-item Multiple Sclerosis Impact Scale; TUG, Timed Up and Go; T25FW, Timed 25-Foot Walk test.
aMedium effect size.
Discussion
There was no difference in the primary outcome of adherence between the Web-based and active comparator groups. Similar to other Web-based exercise studies, there were no adverse events related to participating in the exercise intervention. This pilot study invited only people who reported exercising less than twice a week to participate. During the study, nearly 50% of participants (23 of 48) exercised two or more times per week for at least half of the 26-week study period. There was a wide range of variability in participation in the exercise sessions, with some people reporting more than twice-weekly sessions. In any given week, 28% to 69% of participants in the Web-based group exercised at least twice per week. In comparison, in the active comparator group adherence ranged from 25% to 50%. The lowest rates of adherence were observed toward the end of the study for both groups. This participation rate in twice-weekly exercise is comparable with the 6-month, multicenter trial (n = 90) with webbasedphysio, except the previously reported multicenter trial included only ambulatory people.12
Comparing the present adherence results with those from other Web-based exercise research in MS is challenging because methods for defining and measuring adherence are not consistent in the literature.20 Studies reporting internet-delivered physical activity interventions for people with MS commonly describe physical activity levels measured by self-report questionnaire or describe objective activity levels with accelerometer data.21–24 A focus on activity levels may be appropriate for people with mild-to-moderate MS. For people with more advanced disability and in the absence of clear exercise guidelines for those with more advanced MS, it would seem appropriate to first consider participation adherence (ie, whether the person is safely participating in regular exercise).
Participation adherence data are also important from a service provider perspective,20 especially for those with restricted access to services who may have more advanced disability or who reside in more rural settings. In the present study, half of the participants had their primary place of residence outside of larger city centers, and nearly one-third were community wheelchair users. To better understand participation and access to structured exercise in MS as a means of physical activity, describing the place of residence of people with MS and the severity of their MS may be relevant.
We used stratified randomization according to ambulatory status based on the belief that wheelchair users may experience lower exercise adherence. The data suggest that this was not the case; overall, wheelchair users reported higher adherence rates, and wheelchair users in the Web-based group had the highest mean adherence rate. These data were unexpected given that previous research supports decreased participation in exercise and physical activity with advancing disability.25 These exploratory results are limited by small group; however, the results provide preliminary support that the Web-based platform was helpful to some wheelchair users for overcoming exercise barriers. Further research with this platform or similar platforms in wheelchair users is needed.
In the exploratory analysis of the secondary outcomes, for all the secondary outcomes, the means did not worsen in the Web-based group between baseline and 6 months. This is encouraging given the progressive nature of MS, the longer duration of this exercise trial, and the inclusion of people with more advanced disability. However, the selection of physical function outcomes was limited in this study. Strength asymmetry may not consistently have a dominant-nondominant pattern, and functional tasks rely on other factors besides grip strength.16 It would have been prudent to include other functional tasks as outcome measures. The exercise prescription process in this study was individualized with the goal of prioritizing function. As such, core strength, upper-limb strength, and sit-to-stand transfers were targeted, which may be important for the maintenance of longer-term independence.26 The goal-setting process of linking specific exercises with longer-term goals and priorities in people with more advanced MS was facilitated by physiotherapists with experience in MS. This process for goal setting could influence study results. For example, a functional goal to maintain sit-to-stand transfers to stay living at home alone with MS as long as possible might encourage longer-term adherence to a sit-to-stand exercise prescription.
Limitations of this pilot study included incomplete data ascertainment due to dropouts, missing diaries from the active comparator group, and challenges in scheduling the blinded final assessments. The dropout rate in this study was 20%, similar to in other physical activity studies involving people with progressive MS with higher levels of disability.22 Reasons for dropping out of the present study were reassuringly not related to the intervention; yet, reasons for dropping out were not disclosed for five of the participants. Sixteen of the 32 comparator group diaries were not returned, and six participants in the active comparator group submitted no exercise diaries at all. All missing data were replaced with zeros in the intention-to-treat analysis, with a disproportionate amount of missing data in the comparator group. We can, therefore, be confident that the sensitivity to detect between-group differences in adherence was not reduced by the handling of missing data. Exercise adherence is underreported in this study because all missing data are unlikely to equate with zero exercise. Despite this, exercise adherence in this study in both groups still increased compared with that reported by participants at their screening baseline. We did not collect prerandomization exercise baseline behavior through diaries or other data potentially predictive of future exercise behavior that could be used to better characterize the study sample (ie, cognitive function, MS course, attributions and self-efficacy for exercise,27 and caregiver support28). Larger-scale, powered studies are required to improve our understanding of the potential benefits of Web-based exercise interventions and the predictors of adherence to Web-based platforms.
This study was also subject to the limitations related to design and measurement in most exercise adherence studies. A limitation of the randomized design is that randomization removes choice from participants regarding how they would like their exercise adherence supported. Some participants randomized to the active comparator group in this study expressed disappointment, and this perhaps contributed to the high number of nonreturned exercise diaries in the active comparator group. Future research aimed to increase exercise adherence might consider more pragmatic study designs, such as those that permit patient choice in selecting from a range of interventions that appeal most to the participant.
Diarizing was used as a measurement tool for adherence. However, diarizing is also a form of self-monitoring that may promote exercise beyond what is current usual practice, and knowing that monitoring is occurring may change behavior.29 Although we aimed to minimize monitoring in the comparator group to emulate usual care and facilitate physiotherapist support and monitoring in the Web-based group, this approach resulted in different diarizing methods for each group. The Web-based group exercise was diarized only through the Web-based online platform, allowing real-time monitoring by the physiotherapists. The comparator group was asked to submit paper diaries at only the study midpoint (3 months) and end point (6 months). A significant limitation of this study was missing diaries in the comparator group. One advantage of the online Web-based diary format is that participants did not need to return diaries because exercise adherence could be reviewed remotely through the Web-based program. Participants in both groups were still required to diarize their exercise. Challenges with diarizing as a means of measuring adherence may have affected exercise adherence outcomes.
There are also limitations with having a usual care comparator group. Although it is relevant to include usual care or active care comparison groups because any new interventions addressing physical activity participation should aim to achieve at least the same rates of participation as usual care with additional benefits (ie, lower costs, improved accessibility at the population level), in reality usual care is currently not standardized for access to support for physical activity. Some individuals in the comparator group may have received more support for physical activity than their usual care for physical activity.
There are other limitations and challenges with Web-based physiotherapist-prescribed exercise that we experienced in the conduct of this study. There were limitations in the accessibility of the internet for some and the challenge of changing established models of care. There was a continued desire for face-to-face contact between participants and prescribing therapists. Qualitative inquiry into Web-based programs to date is limited, and a more comprehensive understanding of the challenges warrant further study.8 There may be opportunities to improve adherence to Web-based exercise platforms with augmented patient-provider interactions and coaching2 and through social media supports.30
In moderate-to-severe MS, personalized home-based exercise programs of 6 months’ duration were well tolerated without evidence of systematic decline in patient-reported outcomes or measured function. A Web-based approach is one method that provides a safe way to facilitate participation in physical activity. Web-based approaches provide a widely accessible means of delivering personalized and professionally guided support for some individuals with MS. Further research is needed to determine which individuals may be most likely to benefit from this approach.
PRACTICE POINTS
People with moderate-to-severe MS safely participated in physiotherapist-prescribed home exercise for 6 months.
A customized Web-based platform was modified to include exercise options for users with advanced MS.
Wheelchair users in the Web-based exercise group of this pilot study demonstrated the highest rates of exercise adherence.
Supplementary Material
Acknowledgments
The authors thank the research team advisors Rob Loewen and Patricia O’Donnell; study physiotherapists Anissa Van Dusen, Cathy Bousquet, Jan Klassen, Kari Froehlich, Lindsey Gerwing, Michelle Riendeau, Nicole Loucks, and Shona Nickel; and the Saskatchewan MS Clinic for assistance with recruitment. The PDDS scale was provided for use by the North American Research Committee on Multiple Sclerosis (NARCOMS) Registry (www.narcoms.org/pdds), and NARCOMS is supported in part by the Consortium of Multiple Sclerosis Centers (CMSC) and the CMSC Foundation.
Footnotes
Financial Disclosures: Dr Paul is co-inventor of the Web-based physiotherapy platform and now a director of the social enterprise Giraffe Healthcare. However, she was not involved with any data collection or analysis. The other authors declare no conflicts of interest.
Funding/Support: This study was supported by the Hermes Canada | Multiple Sclerosis Society of Canada Wellness Research Innovation Grant; the Saskatoon Health Region; and the College of Medicine, University of Saskatchewan.
References
- 1.Dalgas U. Exercise therapy in multiple sclerosis and its effect on function and the brain. Neurodegener Dis Manag. 2017;7:35–40. doi: 10.2217/nmt-2017-0040. [DOI] [PubMed] [Google Scholar]
- 2.Ploughman M. Breaking down the barriers to physical activity among people with multiple sclerosis: a narrative review. Phys Ther Rev. 2017;22:124–132. [Google Scholar]
- 3.Kayes NM, McPherson KM, Taylor D, Schlüter PJ, Kolt GS. Facilitators and barriers to engagement in physical activity for people with multiple sclerosis: a qualitative investigation. Disabil Rehabil. 2011;33:625–642. doi: 10.3109/09638288.2010.505992. [DOI] [PubMed] [Google Scholar]
- 4.Hale LA, Smith C, Mulligan H, Treharne GJ. “Tell me what you want, what you really really want…”: asking people with multiple sclerosis about enhancing their participation in physical activity. Disabil Rehabil. 2012;34:1887–1893. doi: 10.3109/09638288.2012.670037. [DOI] [PubMed] [Google Scholar]
- 5.Learmonth YC, Adamson BC, Balto JM et al. Multiple sclerosis patients need and want information on exercise promotion from healthcare providers: a qualitative study. Health Expect. 2017;20:574–583. doi: 10.1111/hex.12482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Pilutti LA, Edwards TA. Is exercise training beneficial in progressive multiple sclerosis? Int J MS Care. 2017;19:105–112. doi: 10.7224/1537-2073.2016-034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Al-Sakran LH, Marrie RA, Blackburn DF et al. Establishing the incidence and prevalence of multiple sclerosis in Saskatchewan. Can J Neurol Sci. 2018;45:295–303. doi: 10.1017/cjn.2017.301. [DOI] [PubMed] [Google Scholar]
- 8.Dennett R, Gunn H, Freeman JA. Effectiveness of and user experience with web-based interventions in increasing physical activity levels in people with multiple sclerosis: a systematic review. Phys Ther. 2018;98:679–690. doi: 10.1093/ptj/pzy060. [DOI] [PubMed] [Google Scholar]
- 9.Hohol MJ, Orav EJ, Weiner HL. Disease steps in multiple sclerosis: a longitudinal study comparing disease steps and EDSS to evaluate disease progression. Mult Scler. 1999;5:349–354. doi: 10.1177/135245859900500508. [DOI] [PubMed] [Google Scholar]
- 10.Learmonth YC, Motl RW, Sandroff BM, Pula JH, Cadavid D. Validation of Patient Determined Disease Steps (PDDS) scale scores in persons with multiple sclerosis. BMC Neurol. 2013;13:37. doi: 10.1186/1471-2377-13-37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hey SP, Kimmelman J. The questionable use of unequal allocation in confirmatory trials. Neurology. 2014;82:77–79. doi: 10.1212/01.wnl.0000438226.10353.1c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Paul L, Renfrew L, Freeman J et al. Web-based physiotherapy for people affected by multiple sclerosis: a single blind, randomized controlled feasibility study. Clin Rehabil. 2019;33:473–484. doi: 10.1177/0269215518817080. [DOI] [PubMed] [Google Scholar]
- 13.Paul L, Coulter EH, Miller L et al. Web-based physiotherapy for people moderately affected with multiple sclerosis; quantitative and qualitative data from a randomized, controlled pilot study. Clin Rehabil. 2014;28:924–935. doi: 10.1177/0269215514527995. [DOI] [PubMed] [Google Scholar]
- 14.Hobart J, Lamping D, Fitzpatrick R, Riazi A, Thompson A. The Multiple Sclerosis Impact Scale (MSIS-29): a new patient-based outcome measure. Brain. 2001;124:962–973. doi: 10.1093/brain/124.5.962. [DOI] [PubMed] [Google Scholar]
- 15.Watson TM, Ford E, Worthington E, Lincoln NB. Validation of mood measures for people with multiple sclerosis. Int J MS Care. 2014;16:105–109. doi: 10.7224/1537-2073.2013-013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Severigns D, Lamers I, Kerkhofs L, Feys P. Hand grip fatigability in persons with multiple sclerosis according to hand dominance and disease progression. J Rehabil Med. 2015;47:154–160. doi: 10.2340/16501977-1897. [DOI] [PubMed] [Google Scholar]
- 17.Kaufman M, Moyer D, Norton J. The significant change for the Timed 25-Foot Walk in the Multiple Sclerosis Functional Composite. Mult Scler. 2000;6:286–290. doi: 10.1177/135245850000600411. [DOI] [PubMed] [Google Scholar]
- 18.Sebastiao E, Sandroff BM, Learmonth YC, Motl RW. Validity of the Timed Up and Go Test as a measure of functional mobility in persons with multiple sclerosis. Arch Phys Med Rehabil. 2016;97:1072–1077. doi: 10.1016/j.apmr.2015.12.031. [DOI] [PubMed] [Google Scholar]
- 19.Cohen J. A power primer. Psychol Bull. 1992;112:155–159. doi: 10.1037//0033-2909.112.1.155. [DOI] [PubMed] [Google Scholar]
- 20.Hawley-Hague H, Horne M, Skelton DA et al. Review of how we should define (and measure) adherence in studies examining older adults’ participation in exercise classes. BMJ Open. 2016;6:e011560. doi: 10.1136/bmjopen-2016-011560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Dlugonski D, Motl R, Mohr D et al. Internet-delivered behavioral intervention to increase physical activity in persons with multiple sclerosis: sustainability and secondary outcomes. Psychol Health Med. 2012;17:636–651. doi: 10.1080/13548506.2011.652640. [DOI] [PubMed] [Google Scholar]
- 22.Pilutti L, Dlugonski D, Sandroff B, Klaren R, Motl R. Randomized controlled trial of a behavioral intervention targeting symptoms and physical activity in multiple sclerosis. Mult Scler. 2014;20:594–601. doi: 10.1177/1352458513503391. [DOI] [PubMed] [Google Scholar]
- 23.Tallner A, Streber R, Hentschke C et al. Internet-supported physical exercise training for persons with multiple sclerosis: a randomized controlled study. Int J Mol Sci. 2016;17:1667. doi: 10.3390/ijms17101667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Conroy SS, Zhan M, Culpepper WJ, II et al. Self-directed exercise in multiple sclerosis: evaluation of a home automated tele-management system. J Telemed Telecare. 2018;24:410–419. doi: 10.1177/1357633X17702757. [DOI] [PubMed] [Google Scholar]
- 25.Klaren RE, Motl RW, Dlugonski D et al. Objectively quantified physical activity in persons with multiple sclerosis. Arch Phys Med Rehabil. 2013;94:2342–2348. doi: 10.1016/j.apmr.2013.07.011. [DOI] [PubMed] [Google Scholar]
- 26.Finlayson M, Van Denend T. Experiencing the loss of mobility: perspectives of older adults with MS. Disabil Rehabil. 2003;25:1168–1180. doi: 10.1080/09638280310001596180. [DOI] [PubMed] [Google Scholar]
- 27.Nickel D, Spink K, Andersen M, Knox K. Attributions and self-efficacy for physical activity in multiple sclerosis. Psychol Health Med. 2019;19:433–441. doi: 10.1080/13548506.2013.832783. [DOI] [PubMed] [Google Scholar]
- 28.Wood V, Kasser SL. Spousal support and self-determined physical activity in individuals with multiple sclerosis: a theory-informed qualitative exploration. Disabil Health J. 2020;13:100835. doi: 10.1016/j.dhjo.2019.100835. [DOI] [PubMed] [Google Scholar]
- 29.Moseley GL. Do training diaries affect and reflect adherence to home programs? Arthritis Rheum. 2006;55:662–664. doi: 10.1002/art.22086. [DOI] [PubMed] [Google Scholar]
- 30.Zhang J, Brackbill D, Yang S, Centola D. Efficacy and causal mechanism of an online social media intervention to increase physical activity: results of a randomized controlled trial. Prev Med Rep. 2015;2:651–657. doi: 10.1016/j.pmedr.2015.08.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


