Abstract
We examined whether romantic relationship involvement, a well-established protective factor against mental health problems among heterosexual adults, is also protective for sexual and gender minority emerging adults assigned female at birth (SGM-AFAB), a group at high risk for mental health issues. Using cross-sectional data from a community sample of 222 SGM-AFAB ages 18-20 years, we assessed associations between current relationship involvement and five mental health variables: depressive symptoms, anxiety symptoms, alcohol use problems, cannabis use problems, and illicit drug use. There were no differences by romantic involvement in problematic cannabis use or other illicit drug use. Overall, participants in a relationship reported fewer depressive symptoms, fewer anxiety symptoms, and less problematic alcohol use than participants who were single. Some associations differed, however, by participant gender identity, sexual orientation identity, and partner gender. Specifically, relationship involvement was associated with fewer depressive and anxiety symptoms for cisgender female participants (n=154) but not for gender minority participants (n=68), and for lesbian participants (n=38) but not for bisexual/pansexual participants (n=134) or those with other sexual orientation identities (n=50). Participants romantically involved with a cisgender female partner (n=43) had fewer depressive and anxiety symptoms than single participants (n=100), those with a cisgender male partner (n=56), and those with a gender minority partner (n=23). Together, these findings suggest that romantic involvement may promote mental health for many, but not all, SGM young adults, highlighting the importance of attending to differences among SGM subgroups in research and efforts to reduce mental health and substance use disparities.
Keywords: LGBT, romantic involvement, sexual and gender minorities, depression, anxiety, substance use, alcohol use, cannabis use
Likely driven by societal stigma against non-heterosexual and transgender identities (Meyer, 2003), sexual and gender minority (SGM) individuals experience disproportionately high rates of mental health problems, including depression, anxiety, and substance use disorders (Institute of Medicine, 2011). Although these disparities are present across the lifespan, they are particularly striking during emerging adulthood (Austin & Bozick, 2012; Shuler et al 2018), a developmental era roughly corresponding to ages 18-25 years (Arnett, 2005) when depression, anxiety, and substance use are highly prevalent (SAMHSA, 2007). Compared to their heterosexual counterparts, SGM emerging adults have higher rates of depression and anxiety (Lytle, De Luca, & Blosnich, 2014; Marshal et al., 2013; Needham, 2012; Oswalt & Lederer, 2017), and more problematic use of alcohol, marijuana, and other illegal drugs (Austin & Bozick, 2012; Needham, 2012; Talley, Sher, & Littlefield, 2010). Disparities in depression and substance use are largest for SGM young adults assigned female at birth (AFAB; Marshal et al. 2008, 2013; Shuler et al., 2018), who appear to be at particular risk for poor mental health outcomes, even compared to SGM assigned male at birth (AMAB; Meyer, 2003).
To address these mental health disparities, it is important to identify factors that may protect SGM-AFAB emerging adults from anxiety, depression, and substance use. Involvement in a committed romantic partnership is one well-established protective factor for mental health and substance use among heterosexual adults (e.g., Kamp Dush & Amato, 2005;Vanassche, Swicegood, & Matthijs, 2013). However, it is not clear if SGM-AFAB, particularly those who are emerging adults, also experience mental health benefits from their romantic relationships. In the current study, we assessed whether current romantic involvement was associated with depressive symptoms, anxiety symptoms, problematic alcohol and cannabis use, and use of other illicit drugs among 18-20 year old SGM-AFAB emerging adults. Further, we assessed whether these associations differed by gender identity (cisgender female vs. gender minority), sexual orientation identity (lesbian vs. bi/pansexual vs. other), race, or partner gender.
Romantic Involvement and Mental Health in Adults
Involvement in a committed relationship is theorized to benefit mental health in several ways. According to social control theories, spouses and serious romantic partners monitor one another’s behavior, encouraging healthy behaviors that promote emotional wellbeing (e.g., sleep, exercise) and discouraging risky behaviors such as heavy drinking and drug use (Umberson, 1987). Romantic involvement may also promote mental health by providing an intimate, emotionally fulfilling, and supportive relationship that satisfies individuals’ needs for social connection (House, Umberson, & Landis, 1988). Marriage and some other relationship types are also theorized to provide tangible legal and financial benefits, including access to partner income and health insurance benefits, which promote general health and wellbeing (e.g., Waite & Gallagher, 2000). Consistent with these theories, research on heterosexual adults has long documented the mental health benefits of marriage and other committed relationships. Compared to single adults, those who are married or committed to a romantic partner report better psychological wellbeing (e.g., Kamp Dush & Amato, 2005; Vanassche et al., 2013). Further, longitudinal studies show that entry into marriage or a committed relationship is followed by reduced depression (Lamb, Lee, & DeMaris, 2003) and alcohol and drug use (Duncan, Wilkerson, & England, 2006; Staff et al., 2010), suggesting a causal effect of romantic involvement on mental health.
Relationship Involvement and Mental Health among Emerging Adults
Although historically most theory and research has focused on the benefits of marriage for adult mental health (e.g., Waite & Gallagher, 2000), there is a growing literature exploring potential mental health benefits of involvement in a wider range of romantic relationship types during emerging and young adulthood. Compared to single young women, those in committed dating relationships have reported fewer depressive symptoms (Whitton, Weitbrecht, Kuryluk, & Bruner, 2013) and less alcohol consumption (Braithwaite et al., 2010; Whitton et al., 2013) but not less use of illicit drugs (Braithwaite et al., 2010; Simon & Barrett, 2010). Longitudinal research has yielded mixed findings. In some studies, young adult substance use declined upon entry into a dating (Furman & Collibee, 2014; Fleming, White, & Catalano, 2010) or nonmarital cohabiting relationship (Duncan et al., 2006; Staff et al., 2010). However, in other studies, entry into a relationship between ages 18 and 20 was not associated with reduced heavy drinking or marijuana use (Fleming, White, Oesterle, Haggerty, & Catalano, 2010) and romantic involvement predicted subsequent increases in depression in first-year college students (Davila, Steinberg, Kachadourian, Cobb, & Fincham, 2004).
These inconsistent findings raise the possibility that romantic involvement does not confer the same mental health benefits during emerging adulthood that it does later in life. There are several theoretical reasons why this might be the case. In contrast to adult spouses, young romantic partners may not monitor or exert social control over each other’s behavior, and the social pressure against engaging in risky behaviors when married may not be present. Young romantic relationships also do not typically provide legal or financial benefits that might ease stress and promote health. Further, during emerging adulthood, when many people pursue academic and occupational goals before settling down (Arnett, 2005), relationships often lack long-term commitment. Because highly committed relationships (e.g., marriage, cohabitation) most strongly promote subjective well-being and discourage risky substance use (Bachman et al., 1997; Kamp Dush & Amato, 2005), the less committed relationships of emerging adults may not confer strong mental health benefits.
On the other hand, there are reasons to think emerging adults should benefit psychologically from romantic involvement. Developing romantic competence represents a central developmental task of young adulthood (Roisman, Masten, Coatsworth, & Tellegen, 2004) and romance may provide an intimate, emotional connection not offered by other social partners. Romantic involvement may also discourage substance use among emerging adults by limiting engagement in the single “hook-up” culture where heavy drinking and drug use are prevalent (e.g., Owen, Rhoades, Stanley, & Fincham, 2010). More research is needed to clarify how romantic involvement is associated with mental health among emerging adults.
Relationship Involvement and Mental Health among Sexual and Gender Minorities
Little is known about the effects of romantic involvement on the mental health and substance use of SGM, particularly emerging adults. The same-sex romantic relationships of adults, overall, are remarkably similar to adult different-sex relationships across multiple dimensions of relationship quality (e.g., Kurdek, 2005) and show similar associations between relationship quality and partners’ depressive symptoms (Whitton & Kuryluk, 2014). Further, sexual minority and heterosexual adults report similar efforts to promote healthy behaviors and discourage heavy substance use in their romantic partners (Reczek & Umberson, 2012). It seems likely, then, that the benefits of romantic involvement to mental health and substance use would generalize to SGM, at least during adulthood. During emerging adulthood, it is possible that SGM may benefit even more than heterosexuals from romantic involvement because a dating partner can provide emotional support that is commonly missing from parents and peers (Katz-Wise & Hyde, 2012; Huebner, Diaz, & Sanchez, 2009). Further, affiliation with members of the SGM community can buffer the effects of minority stress on young sexual minority women (Johns et al., 2013). On the other hand, dating a same-sex partner may activate internalized stigma, raise risk for family rejection by revealing same-sex attractions, and lead to experiences of relationship stigma (stigma targeting a couple based on their gender composition), all of which may increase risk for mental health and substance use problems (Newcomb & Mustanski, 2019; Rosenthal et al., 2019; Ryan et al., 2009).
Research on the associations between romantic involvement and mental health among SGM is sparse. In a handful of cross-sectional studies, adult lesbians in a committed relationship reported fewer depressive symptoms (Ayala & Coleman, 2000; Kornblith, Green, Casey, & Tiet, 2016; Oetjen & Rothblum, 2000) and better psychological wellbeing (Wayment & Peplau, 1995) than those who were single. Among sexual minority men, romantic involvement has been linked with lower depressive symptoms and less use of some illicit drugs (Parsons et al., 2013; Starks et al., 2019). However, romantically involved sexual minority men did not use less marijuana or alcohol than single men (Starks et al., 2019). Further, another study found that romantic involvement was not associated with rates of anxiety or depressive disorders among gay and lesbian adults, and was associated with higher odds of anxiety disorders among bisexual adults (Feinstein, Latack, Bhatia, Davila, & Eaton, 2016).
Studies on younger SGM are even more rare and have yielded inconsistent findings. Two found no consistent differences in psychological wellbeing between single and romantically-partnered male and female SGM youth ages 16-24 years (Baams, Bos, & Jonas, 2014) and ages 15-19 years (Bauermeister et al., 2010). Another found that involvement in a dating or cohabiting relationship was not associated with lower rates of marijuana or hard drug use in lesbian and gay 18-26 year olds (Austin & Bozick, 2012). In contrast, a longitudinal study of SGM-AFAB and -AMAB youth (spanning ages 16-26) indicated that SGM youth reported less psychological distress, alcohol consumption, and use of illicit drugs other than marijuana when they were romantically partnered than when they were single (Whitton, Dyar, Newcomb, & Mustanski, 2018a; Whitton, Dyar, Newcomb, & Mustanski, 2018b). However, the effects of romantic involvement were more positive for Black versus White youth, and bisexual youth reported more psychological distress and marijuana use when in a relationship than when single. Clearly, more research is needed, with consideration of potential differences between subgroups of sexual minority emerging adults.
Moderators of Associations between Relationship Involvement and Mental Health
Although often treated as a homogenous group, SGM young people are diverse along many dimensions, including gender identity, sexual identity (i.e., self-identified sexual orientation), and race. Further, they form romantic relationships with a variety of partners, including cisgender men and women (whose gender identity and sex assigned at birth match; e.g., James et al., 2016), and gender minority individuals. Understanding how relationship involvement may affect mental health among young SGM requires attention to potential differences along these demographic lines.
First, we must consider the increasing number of young people who identify as transgender (i.e., are assigned female at birth and identify as men; Flores, Herman, Gates, & Brown, 2016) or non-binary (e.g., gender nonconforming, genderqueer; Richards et al., 2016). These individuals, collectively labeled gender minorities, experience troublingly high rates of discrimination and violence (e.g., James et al., 2016). Romantic involvement may particularly benefit gender minority young adults by buffering them from the negative mental health effects of these experiences. Alternately, many partnered gender minorities encounter stigma against their romantic relationships, which is associated with depression (e.g., Gamarel, Reisner, Laurenceau, Nemoto, & Operario, 2014) and substance use (Reisner, Gamarel, Nemoto, & Operario, 2014), suggesting potential negative effects of involvement on mental health.
Specific sexual orientation identities may also influence how romantic involvement affects mental health and substance use. Whereas gay and lesbian people generally appear to benefit from relationships, romantic involvement has been associated with greater risk for anxiety disorders (Feinstein et al., 2016), more psychological distress (Whitton et al., 2018b), and more use of marijuana and other illicit drugs (Whitton et al., 2018a) among bisexuals. These differences may be attributable to unique stressors bisexuals face when involved in romantic relationships, including invalidation of their bisexual identity by others who assume they are lesbian/gay or heterosexual based on their current partner’s gender (Dyar, Feinstein, & London, 2014) and pressure from non-bisexual partners to change their sexual identity (Bostwick, Wendy & Hequembourg, 2014).
Exploring racial differences in how romantic involvement is associated with SGM mental health is needed as part of broader efforts to understand how co-occurring social identities may intersect to impact health (Institute of Medicine, 2011). Because SGM people of color experience discrimination, microaggressions, and harassment based on both their sexual and racial minority identities (Balsa et al., 2011) they may particularly benefit from the social support of a romantic relationship. Indeed, romantic involvement was associated with less psychological distress for Black and Latinx SGM youth, but not White SGM youth, in one study (Whitton et al., 2018b). However, because most studies have used samples lacking in racial and ethnic diversity, more research is needed.
Finally, though it is often assumed that sexual minorities only have same-sex partners, around one-fourth of sexual minority adolescents and one-fourth of lesbian adults report relationships with different-sex partners (Bauermeister et al., 2010; Diamond & Savin-Williams, 2000). There is some evidence that, for sexual minority adolescents, involvement in same-sex relationships is positively associated with psychological wellbeing, including lower anxiety and internalized heterosexism and higher self-esteem, but different-sex relationship involvement is not (Bauermeister et al., 2010; Russell & Consolacion, 2003). These initial findings support further investigation of potential differences by partner gender in the effects of relationships on SGM mental health beyond adolescence. Further, we are aware of no studies that have explored the mental health effects of relationships with gender minority partners (i.e., those who identify as transgender, genderqueer, non-binary, etc.), though many sexual minority women report sexual or romantic partnerships with them (Mereish, Katz-Wise, & Woulfe, 2017).
The Current Study
The current study aimed to advance our understanding of how relationship involvement is associated with the mental health of SGM-AFAB emergind adults. Using cross-sectional data provided by a community sample of 222 SGM-AFAB aged 18-20 years, we assessed associations between current relationship involvement and five mental health variables: depressive symptoms, anxiety symptoms, alcohol use problems, cannabis use problems, and illicit drug use. Further, we evaluated potential differences in these associations by participant gender identity, sexual orientation identity, race, and gender identity of the romantic partner.
Method
Participants and Procedure
Data were drawn from the late adolescent/emerging adult cohort of FAB400 (N=400; 16-20 years old at baseline), an ongoing longitudinal merged-cohort study of young SGM-AFAB, focused on their health, development, and intimate relationships (Whitton, Dyar, Mustanski, & Newcomb, 2019). Inclusion criteria required participants to be assigned female at birth, speak English, and either identify with a sexual or gender minority label, report same-gender attractions, or report same-gender sexual behavior. Consequently, the sample is comprised of sexual minority women, transgender men, and non-binary AFAB youth. Participants were recruited using various methods including venue-based, online, and peer-incentivized recruitment. Because design effects for each dependent variable, which quantify the extent to which the sampling error deviates from what would be expected if individuals were randomly assigned to clusters, was below the recommended cutoff of 2.0 (Muthén & Satorra, 1995), we did not account for clustering within recruitment chains in analyses.
The present study uses data from the FAB400 baseline assessment, collected from 2016-2017. Participants were paid $50 for completing a battery of self-report measures using computer-assisted self-interview. The study protocol was approved by the Institutional Review Board (IRB) at Northwestern University with a waiver of parental permission for participants under 18 years of age under 45 CFR 46, 408(c). We selected participants (N=242; 60.5%) in the age range of 18 to 20, given our focus on relationship involvement during emerging adulthood. We then excluded six participants who reported current involvement in more than one romantic relationship and one randomly selected partner from each of the 14 couples who reported on the same relationship to retain independence of data. This yielded an analytic sample of 222 emerging adult SGM-AFAB; demographic characteristics are presented in Table 1.
Table 1.
Demographic characteristics of analytic sample (N=222).
| Variable | Single (n=100) | Involved (n=122) |
|---|---|---|
| n (%) | n (%) | |
| Race/ethnicity | ||
| Black/African-American | 30 (30.0) | 43 (35.2) |
| Hispanic/Latinx | 21 (21.0) | 30 (24.6) |
| White | 30 (30.0) | 33 (27.0) |
| Other | 19 (19.0) | 16 (13.1) |
| Asian | 5 | 6 |
| Multiracial | 14 | 10 |
| Sexual Identity | ||
| Lesbian | 16 (16.0) | 22 (18.0) |
| Bisexual/Pansexual | 48 (48.0)a | 86 (70.5)b |
| Other Sexual Identity | 36 (36.0)a | 14 (11.5)b |
| Queer | 21 | 9 |
| Unsure/Questioning | 7 | 2 |
| Straight/Heterosexual | 1 | 0 |
| Asexual | 1 | 1 |
| Not Listed | 6 | 2 |
| Gender Identity | ||
| Cisgender Female | 62 (62.0)a | 92 (75.4)b |
| Gender Minority | 38 (38.0)a | 30 (24.6)b |
| Male | 7 | 4 |
| Transgender | 5 | 3 |
| Gender Non-Conforming | 11 | 7 |
| Gender Queer | 9 | 9 |
| Non-binary | 3 | 4 |
| Not listed | 3 | 3 |
| Partner Gender Identity | ||
| Cisgender Male | - | 56 (45.9) |
| Cisgender Female | - | 43 (35.2) |
| Gender Minority | - | 23 (18.9) |
| Not applicable: Participant is single | 100 (100) | - |
| Relationship Type | ||
| Casually dating | - | 26 (21.3) |
| Serious dating relationship | - | 88 (72.1) |
| Engaged to be married | - | 3 (2.5) |
| Domestic partnership | - | 1 (0.8) |
| Married | - | 1 (0.8) |
| Lifelong committed relationship | - | 3 (2.5) |
| Not applicable: Participant is single | 100 (100) | - |
Note. Proportions with different superscripts differ from each other at p < .05.
Measures
Relationship involvement.
Participants were asked to report on up to three sexual and/or romantic partnerships occurring in the last 6 months. If the participant reported any type of romantic partnership that was ongoing at the time of the interview (from casually dating to married), they were coded as romantically involved; otherwise, they were coded as single.
Depressive and anxiety symptoms.
The Patient-Reported Outcomes Measurement Information System (PROMIS) Depression Short Form 8b and Anxiety Short Form 8a (Pilkonis et al., 2011) were used to assess depressive and anxious symptoms in the past 7 days. Participants rated how frequently they experienced each of eight depressed feelings (e.g., unhappiness, helplessness) and eight anxious feelings (e.g., unease) on a five-point scale (1 = never to 5 = always). Scores were calculated by summing the eight items (α = .93 for depression, α = .93 for anxiety).
Problematic alcohol use.
The Alcohol Use Disorders Identification Test (AUDIT; Babor, Higgins-Biddle, Saunders, & Monteiro, 2001) measures the frequency and quantity of alcohol consumption and problems associated with alcohol use (e.g., “How often during the past 6 months have you had a feeling of guilt or remorse after drinking?”) in the previous 6 months. Scores represent the sum of all ten items (possible range = 0 to 40; α = .83); higher scores indicate more alcohol use problems.
Problematic cannabis use.
The Cannabis Use Disorders Identification Test-Revised (CUDIT; Adamson et al., 2010) measures marijuana use and problems associated with use in the past 6 months. Scores represent the sum of the eight items (possible range = 0 to 32; α = .80); higher scores indicate more cannabis use problems.
Other illicit drug use.
To assess other illicit drug use, all participants were asked if they had used any of the following non-prescription drugs in the past six months: Cocaine or crack, heroin, methamphetamines, GHB, ketamine, poppers, inhalants, hallucinogens, or ecstasy. Due to low counts of individual illicit drug use, a dichotomous variable was created indicating the presence or absence of illicit drug use.
Potential Moderators.
Gender identity.
Participants responded to the question, “What is your current gender identity?” with the following options: Male, female, transgender, gender non-conforming, genderqueer, non-binary, and not listed (please specify). Responses were used to assign participants to one of two groups: Cisgender women (self-identified as female) and gender minorities (participants who identified with any other gender identity).
Sexual identity.
Participants were asked, “Which of the following commonly used terms best describes your sexual orientation?” with the options: Gay, lesbian, bisexual, queer, unsure/questioning, straight/heterosexual, pansexual, asexual, and not listed (please specify). To provide adequate power for moderation analyses, sexual identity was recoded into three categories: monosexual (gay or lesbian), non-monosexual (bisexual/pansexual), and other.
Race/ethnicity.
Participants were asked to select the option(s) that best described their race from the following: American Indian or Alaskan Native, Asian, Black or African American, Native Hawaiian or Other Pacific Islander, White, or other (please specify). Participants also indicated if they identified as Hispanic or Latino/Latina/Latinx, regardless of race. As recommended by the National Institutes of Health (2001), all those who selected a Latinx ethnicity were classified as Latinx regardless of race. All others were classified based on the race they selected: Black, White, or other (including all other racial identities, due to low numbers).
Partner gender.
Participants were asked to indicate their partner’s gender identity, with the following options: Cisman, ciswoman, transman, transwoman, gender non-conforming, genderqueer, non-binary, and not listed (please specify). Responses were used to categorize partners’ gender as: Cisgender male, cisgender female, or gender minority.
Data Analytic Plan
We first tested for differences in each continuous mental health variable (depressive and anxiety symptoms, problematic alcohol and marijuana use) by relationship involvement using one-way analyses of covariance (ANCOVAs). For each ANCOVA, we entered a 2-level factor for romantic involvement (single vs. involved) and included gender, sexual identity, and race as covariates, given previous evidence that these demographic variables are associated with likelihood of romantic involvement, psychological symptoms, and substance use (Whitton et al., 2018a, 2018b). Because the illicit drug use variable was dichotomous, we entered relationship involvement and the control variables (gender, sexual identity, and race) into a logistic regression model predicting illicit drug use.
We then evaluated potential differences in these associations (i.e., moderating effects) by participant gender identity, sexual identity, and race using a single multivariate regression predicting each mental health variable. Each dependent variable was regressed onto relationship involvement, gender identity (cisgender female vs. gender minority), two dummy-coded variables representing sexual identity (bisexual/pansexual and other sexual identity) with lesbian as the reference group, three dummy-coded variables representing race (Black, Latinx, and other race) with White as the reference group, and six interaction terms multiplying relationship involvement and each of the moderator variables. This strategy allowed us to assess the unique moderating effects of gender identity, sexual identity, and race, controlling for the moderating effects of the others. Models were calculated using PROCESS for SPSS (Hayes, 2013), which not only provides regression coefficients for each predictor variable, but also tests of the highest order unconditional interaction (i.e., tests of whether a categorical variable with more than two levels has a significant moderating effect), simple slopes between relationship involvement and the dependent variable at each level of the categorical moderator, and adjusted means on the dependent variable for single and romantically involved participants at each level of the categorical moderator. We present both simple slopes and these adjusted means to facilitate interpretation of differences in the outcome variables by romantic involvement within each demographic subgroup.
Tests of whether partner gender moderated the association between romantic involvement and psychological functioning required a different approach. Because partner gender was only available for participants who were romantically involved (and missing for the 100 single participants), it could not be included as a predictor for all participants and we could not create a multiplicative interaction term. Therefore, we created a 4-level variable to represent both relationship involvement and partner gender (single vs. cisgender female partner vs. cisgender male partner vs. gender minority partner). We ran separate one-way ANCOVAs for each dependent variable using this variable as a 4-level factor, controlling for participant gender, sexual identity, and race, to test for differences in the continuous dependent variables between participants who were single, partnered with a male, partnered with a female, or partnered with a gender minority individual. To test for effects of involvement/partner gender on illicit drug use (a categorical outcome), we ran a logistic regression with three dummy-coded predictors (cisfemale partner, cismale partner, gender minority partner) with single as the reference group, controlling for gender, sexual identity, and race.
To interpret the magnitude of observed group differences, effect sizes were estimated using Cohen’s d (≥.2 = small effect, ≥.5 = medium effect, ≥ .8 large effect; Cohen, 1988) for continuous outcomes and φ (≥.1 = small effect, ≥.3 medium effect, ≥.5 a large effect; Cohen, 1988) for dichotomous outcomes (i.e., illicit drug use).
Results
Preliminary Analyses
Descriptive analyses indicated that 26 participants (11.7%) were “casually dating” their partner. Because these relationships might function differently from more committed relationships with respect to mental health, we first evaluated whether it was appropriate to include casual daters in the romantically involved group. Differences between casual daters and participants in more committed relationships (“serious dating relationships,” engaged, cohabiting, married, or lifelong committed relationships; n=96) on all of the continuous dependent variables were assessed using t-tests and differences on the dichotomous illicit drug use variable were assessed using chi-square analysis. None of the dependent variables differed by relationship type (all ps > .05) and effect sizes were quite small (ds ranging from .09 to .28 and φ = .15). Therefore, casual daters were included in the romantically involved group.
Next, we assessed for demographic differences between romantically involved and single participants. Age and race did not differ by relationship involvement (ps > .05). There were differences in gender by relationship involvement, χ2(1, N = 222) = 4.65, p = .03; the proportion of cisgender females was higher among romantically involved than single participants (75.4% vs. 62.0%). There were also differences by sexual identity, χ2(2, N = 222) = 19.41, p < .01; the proportion of lesbian participants was equivalent among romantically involved and single participants (18.0% vs. 16.0%), the proportion of bisexual/pansexual participants was higher among those romantically involved than single (70.5% vs. 48.0%), and the proportion with other sexual identities was lower in the romantically involved than the single group (11.5% vs. 36.0%).
Main Effects
Table 2 displays the means/proportions for each mental health variable by romantic involvement, adjusted for participant gender, sexual identity, and race, as well as test statistics and effect sizes from the ANCOVAs and logistic regression. These results show that relationship involvement was not associated with problematic marijuana use or illicit drug use. However, participants in a relationship reported fewer depressive symptoms, fewer anxiety symptoms, and less problematic alcohol use than participants who were single (small effects).
Table 2.
Means and proportions of mental health and substance use problems by relationship status.
| Single (n = 100) | Involved (n = 122) | Statistic | p-value | Effect Size | |
|---|---|---|---|---|---|
| Depressive Symptoms | 22.30 | 19.97 | F = 4.95 | .03 | d = .30 |
| Anxiety Symptoms | 24.28 | 21.18 | F = 8.74 | < .01 | d = .40 |
| Problematic Alcohol Use | 4.66 | 3.28 | F = 4.62 | .03 | d = .29 |
| Problematic Marijuana Use | 4.78 | 4.98 | F = .06 | .81 | d = .03 |
| Illicit Drug Use | 16.0% | 13.1% | b = −.24 | .56 | φ = .04 |
Note. All means and proportions are adjusted for participant gender, sexual identity, and race.
Moderation Analyses
Participant gender identity.
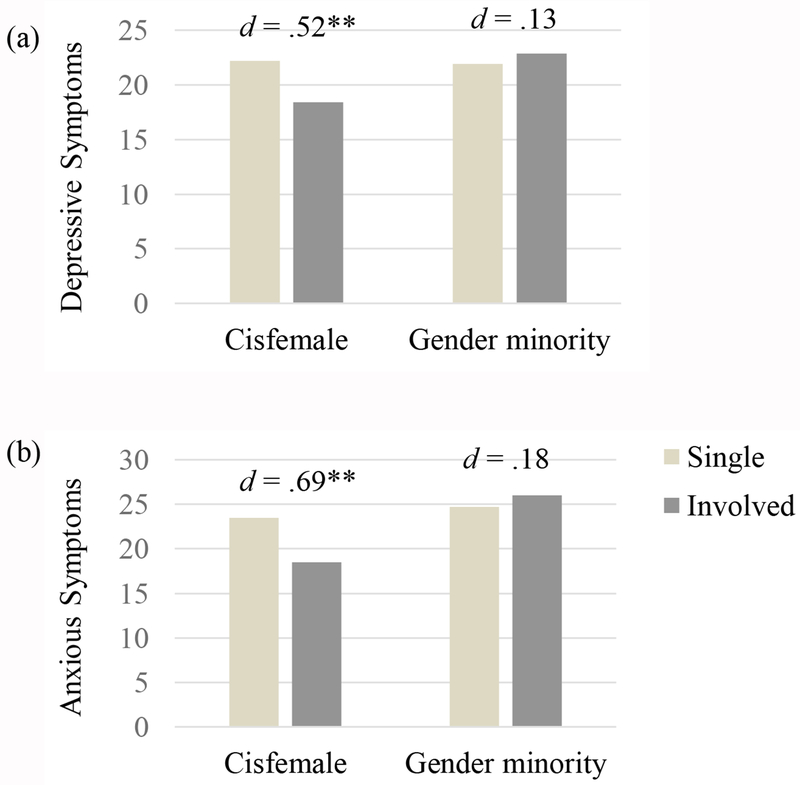
The interaction between relationship involvement and gender identity was significant only in the prediction of depressive symptoms, F(1,213) = 4.06, p = .045 and anxiety symptoms, F(1,213) = 6.51, p = .01. Simple slopes analysis indicated that cisgender females who were in a relationship reported fewer depressive symptoms (M = 18.42) than cisgender females who were single (M = 22.18), b = −9.43, t = −3.08, p < .01, d = .52. Among gender minorities, however, depressive symptoms did not significantly differ between those in a relationship (M = 22.88) and those who were single (M = 21.92), b = −4.84, t = −1.49, p = .14, d = .13. Similarly, cisgender females who were in a relationship reported fewer anxiety symptoms (M = 18.50) than single cisgender females (M = 23.51), b = −9.64, t = −3.46, p < .01, d = .69. In contrast, anxiety symptoms did not significantly differ between gender minorities who were in a relationship (M = 26.01) versus single (M = 24.68), b = −3.89, t = −1.28, p = .20, d = .18. These associations are displayed in Figures 1a–b.
Figure 1.
Associations between relationship involvement and (a) depressive symptoms and (b) anxiety symptoms by participant gender identity (cisgender female vs. gender minority).
Note. **p < .01. All means are adjusted for main and moderating effects of sexual identity and race.
Sexual identity.
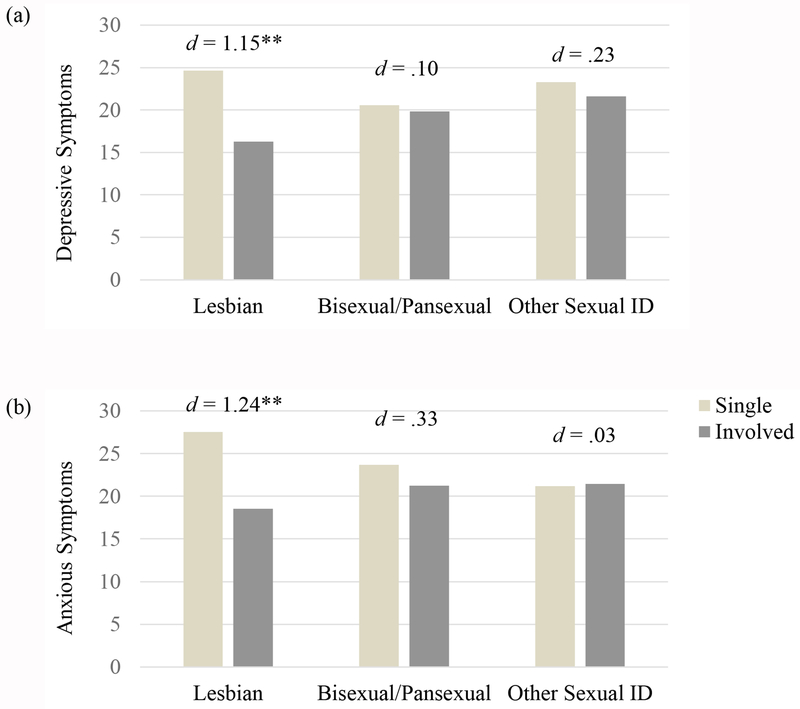
The interaction between sexual identity and relationship involvement was significant in predicting depressive symptoms, F(2,212) = 3.67, p = .03, and anxiety symptoms, F(2,212) = 3.49, p = .03, but not other outcomes. Simple slopes analysis (shown in Figures 2a–b) indicated that, among lesbian participants, those in a relationship reported fewer depressive symptoms (M = 16.27) than those who were single (M = 24.66), b = −9.43, t = −3.08, p < .01, d = 1.15. In contrast, depressive symptoms did not differ by romantic involvement among among bisexual/pansexual participants (Minvolved = 19.85; Msingle = 20.58, b = −1.96, t = −.90, p = .37, d = .10) or among those with other sexual identities (M involved = 21.62; Msingle = 23.29, b = −4.07, t = −1.29, p = .20, d = .23).
Figure 2.
Associations between relationship involvement and (a) depressive symptoms and (b) anxiety symptoms by sexual identity (lesbian vs. bisexual/pansexual vs. other sexual identity).
Note. **p < .01. All means are adjusted for main and moderating effects of participant gender identity and race.
Results were fairly similar for anxiety symptoms. Among lesbian participants, those in a relationship reported significantly fewer anxiety symptoms (M = 18.55) than those who were single (M = 27.55), b = −10.35, t = −3.40, p < .01, d = 1.24. Among bisexual/pansexual participants, those in a relationship (M = 21.26) reported marginally fewer anxiety symptoms than those who were single (M = 23.67), b = −3.79, t = −1.76, p = .08, d = .33. Anxiety symptoms did not differ by romantic involvement for participants with other sexual identities (M involved = 21.43; M single = 21.20), b = −2.32, t = −.75, p = .46, d = .03.
Race.
The interaction between relationship involvement and race was not significant in any analysis (all ps > .05), indicating that race did not moderate the association between relationship involvement and any dependent variable.
Partner gender.
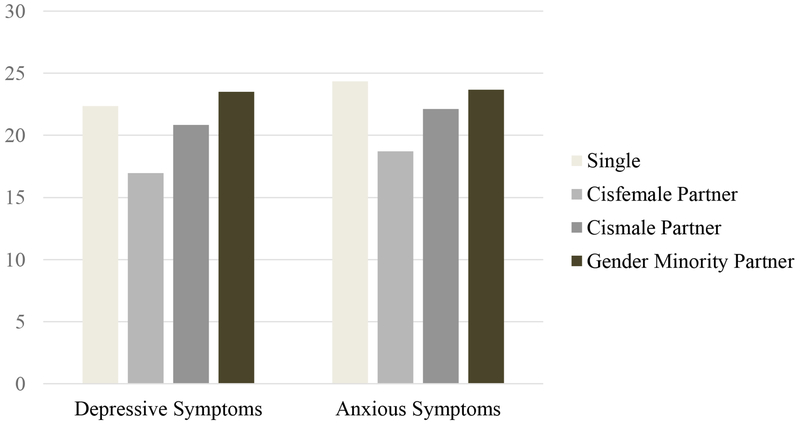
There were no differences in problematic alcohol use, marijuana use, or illicit drug use by involvement/partner gender (all ps > .05). Depressive symptoms, however, differed by involvement/partner gender, F(3, 212) = 6.11, p < .01 (see Figure 3). Pairwise comparisons using Fisher’s Least Significant Difference (LSD) test demonstrated that participants with a cisgender female partner (M = 16.96) had fewer depressive symptoms than those with a cisgender male partner (M = 20.85; p = .01; d = .51), those with a gender minority partner (M = 23.50; p < .01; d = .65), and those who were single (M = 22.36; p < .01; d = .45). There were no other group differences in depressive symptoms. Anxiety symptoms also differed by involvement/partner gender, F(3, 212) = 5.67, p < .01. Pairwise comparisons showed that participants with a cisgender female partner (M = 18.73) had fewer anxiety symptoms than those with a cisgender male partner (M = 22.11; p = .02; d = .49), a gender minority partner (M = 23.69; p < .01; d = .63), and single participants (M = 24.35; p < .01; d = .44). In addition, participants with a cisgender male partner had fewer anxiety symptoms than participants who were single (p = .03; d = .40). There were no other group differences in anxiety symptoms.
Figure 3.
Depressive and anxiety symptoms by involvment with partners of different genders.
Note. All means are adjusted for participant gender, sexual identity, and race. Participants with cisgender female partners had fewer depressive and anxiety symptoms than all other groups. Those with cisgender male partners had fewer anxiety symptoms than single participants.
Discussion
In this sample, SGM-AFAB emerging adults currently involved in a romantic relationship reported fewer depressive symptoms, fewer anxiety symptoms, and less problematic alcohol use than those who were single. Together with similar findings for heterosexual emerging adults (e.g., Kamp Dush & Amato, 2005; Simon & Barrett, 2010; Whitton et al., 2013) and SGM late adolescents and young adults (Whitton et al., 2018a; Whitton et al., 2018b), these findings suggest that romantic relationships may be a broad protective factor for mental health among young people, whether their identity is heterosexual or non-heterosexual.
Findings were most robust for alcohol consumption; romantic involvement was associated with less problematic drinking for SGM-AFAB participants of all races, gender identities, and sexual identities. Further, the association was consistent across SGM-AFAB’s relationships with cisgender female, cisgender male, and gender minority partners. These results echo previous evidence that SGM adolescents and young adults drink less alcohol at times when they are romantically partnered than at times when they are single, and that this is equally true across gay/lesbian and bisexual identities and across cisgender and gender minority identities (Whitton et al., 2018a). It appears that the reductions in heavy drinking associated with marriage in adults do extend to the romantic relationships of SGM emerging adults. Though the mechanisms of effect are unclear, it may be that romantically partnered young SGM-AFAB disengage from the heavy-drinking party scene populated by single adults who are uninterested in relationships or attempting to meet new partners (e.g., Claxton et al., 2015; Owen et al., 2010).
In contrast, the associations of romantic involvement with depressive and anxiety symptoms differed based on gender identity, sexual orientation identity, and partner gender. This suggests that the psychologically protective effects of relationship involvement may only be present for some, but not all, SGM-AFAB emerging adults. Most strikingly, whereas romantic involvement was associated with fewer depressive and anxiety symptoms for cisgender female participants, it was not for gender minority participants. The reduced symptom levels associated with romatic involvement among cisgender women in relationships is consistent with a prior longitudinal study of predominantly cisgender SGM late adolesents and young adults (Whitton et al., 2018b); however, it is unclear why romantic involvement was not similarly associated with less internalizing symptoms among gender minority participants. One possibility is that the stigma against and devaluation of gender minority romantic relationships (e.g., Gamarel et al., 2014) cancels out any positive psychological effects of romantic involvement. If the present findings are replicated, it will be important to explore factors that may interfere with gender minorities benefiting from romantic involvement in the way that heterosexuals (e.g., Kamp Dush & Amato, 2005) and cisgender sexual minorities (e.g., Whitton et al., 2018b) generally do.
Sexual orientation identity also moderated the associations between romantic involvement and psychological symptoms. Specifically, involvement was associated with depressive and anxiety symptoms for lesbian participants only, and not for those with non-monosexual (i.e., bisexual, pansexual) or other sexual orientation identities (including queer, unsure/questioning, and asexual). This finding adds to a growing body of research suggesting that romantic involvement does not have psychological benefits for bisexual individuals (Feinstein et al., 2016; Whitton et al., 2018b), although we did not observe involvement in a relationship to increase bisexual’s anxiety and psychological distress as those studies did. It may be that, for non-monsexuals, any mental health benefits of having a romantic partner are outweighed by stressors inherent in the relationship. Many bisexual women report that when they are romantically involved, their sexual identity is erased by outsiders assuming that they are lesbian or heterosexual based on the gender of their partner (Dyar et al., 2014) and by pressure from their partners to change their sexual identity to match their current relationship (Bostwick et al., 2014). Future research is needed to test whether such experiences explain why romantic involvement may not psychologically benefit non-monsexual people, and to identify strategies to improve the supportiveness of their relationships.
A novel finding from the present study is that, for SGM-AFAB emerging adults, relationships with cisgender female partners may be particularly beneficial to psychological health. Participants involved with a female partner reported fewer anxiety and depressive symptoms than any other group, including not only single participants but also those with male or gender minority partners. These results echo findings from studies of sexual minority adolescents indicating that involvement in same-sex relationships, but not different-sex relationships, is positively associated with psychological wellbeing (Bauermeister et al., 2010; Russell & Consolacion, 2003). Perhaps some young SGM-AFAB date cisgender men in part due to fear of deviating from compulsive heterosexuality norms or a lack of available female partners interested in a same-sex relationship; such relationships may not confer the psychological benefits that a relationship based in sexual attraction and emotional connections would. However, this explanation is not likely for participants who identified as bisexual and are likely attracted to men. It is also possible that involvement with a woman tends to be met with social approval within SGM-AFAB communities, whereas involvement with a man can elicit disapproval and criticism from lesbian peers (Hayfield, Clarke, & Halliwell, 2014). It is not clear why partnering with a gender minority individual was not associated with fewer depressive and anxiety symptoms, though stigma against gender minority romantic relationships (e.g., Gamarel et al., 2014) may play a role. More research is needed, particularly to explore whether the effects of romantic involvement on psychological health differ by partner gender within individuals over time, and what mechanisms may explain those differences.
Unexpectedly, we found no racial differences in the associations between romantic involvement and any mental health variable. This is contrast to findings from a study using a within-person design (Whitton et al., 2018b), which found that these associations were stronger among Black, and to some extent Latinx, SGM youth than White SGM youth. It is possible that the current study had more power to detect effects in White participants due to a larger sample size. Alternately, it may be that the discrepant findings are due to differences in the age range of the samples: We focused just on 18-20 year old emerging adults, while they captured adolescence through young adulthood (16-26 years). Future research should explore potential differences in the association beween romantic involvement and mental health across varying ages.
There were also no differences in use of marijuana or other illicit drugs between single and romantically involved participants in this sample. These findings add to a growing literature suggesting that the “marriage benefit” to marijuana use does not extend to the non-marital different-sex relationships of young adults (Duncan et al., 2006; Fleming et al., 2010) or to the relationships of lesbian and cisgender female SGM youth (Whitton et al., 2018a). Especially in light of the increasing decriminalization and availability of marijuana, it will be important to identify factors other than romantic involvement that may protect SGM-AFAB against problematic cannibus and other illicit drug use.
Several study limitations should be noted. First, the cross-sectional data cannot speak to direction of effects; the observed associations may reflect that good mental health promotes entry into a relationship rather than relationship involvement promoting mental health. Once multiwave longitudinal data are available from this sample, we will be better able to explore directionality by testing whether romantic involvement prospecitively predicts psychological functioning within individuals. We also did not explore whether the quality of participants’ relationships was associated with their mental health; future research is needed to identify specific relationship characteristics (e.g., satisfaction, communication, commitment) that may promote psychological health among SGM-AFAB emerging adults. It is possible that differences in relationship quality may help to explain observed differences between demographic subgroups. The non-probability sample limits the extent to which findings can be viewed as representative of the general population of SGM-AFAB emerging adults. Because many participants were recruited via SGM-focused events or social media connections, they may be more embedded in the LGBT community and more likely to be “out” than the average SGM-AFAB emerging adult. This might reduce potential negative effects of involvement in a romantic relationship, particularly with a cisgender female or gender minority partner. Because all participants were recruited from Chicago, findings may not reflect the experiences of SGM-AFAB living in other regions, especially those less accepting of non-heterosexuality.
Conclusions
Despite these limitations, this study provides new and valuable information about the association between romantic involvement and mental health among SGM-AFAB emerging adults. The current findings extend a small literature suggesting positive mental health effects of romantic relationship involvement for heterosexual emerging adults by demonstrating that it is associated with fewer depressive symptoms, fewer anxiety symptoms, and less problematic alcohol use among SGM-AFAB emerging adults as well. Interestingly, the results suggest that SGM-AFAB who are romantically involved with another woman experience fewer depressive symptoms than not only single SGM-AFAB, but also than those who are romantically involved with a cisgender man. This is contrary to concerns that dating a same-sex partner may raise vulnerability to psychological difficulties by activating internalized stigma or revealing a non-heterosexual orientation to unaccepting others. As such, these results suggest the potential utility of efforts to encourage and support romantic relationships -- including same-sex relationships -- among SGM emerging adults, which may help to address the mental health disparities experienced by this population. Such efforts might include programs to encourage dating among SGM (e.g., through planned LGBT-focused social events), and to teach healthy relationship skills (Mustanski, Greene, Ryan, & Whitton, 2015). However, the potential benefits of romantic involvement may not extend to all SGM-AFAB, particularly those who identify as a gender minority or whose sexual identity is not lesbian, highlighting the importance of attending to differences among SGM subgroups in research, theory, and efforts to reduce mental health and substance use disparities.
Acknowledgments
Authors’ note. This research was supported by a grant from the National Institute of Child Health and Human Development (R01 HD086170; PI: Whitton). The content is solely the responsibility of the authors and does not necessarily represent the official views of the funding agencies. We gratefully acknowledge the FAB400 research team, including Kitty Beuhler, Christina Dyar, Parks Dunlap, Jazz Stephens, Greg Swann, Arielle Zimmerman, and Brian Mustanski. We also thank the FAB400 participants for their invaluable contributions toward understanding the health of the sexual and gender minority community. These findings were presented at the 2019 meeting of the Association for Behavioral and Cognitive Therapies, Atlanta, GA.
Contributor Information
Sarah W. Whitton, University of Cincinnati
Lisa M. Godfrey, University of Cincinnati
Shariell Crosby, Institute for Sexual and Gender Minority Health and Wellbeing, Northwestern University.
Michael E. Newcomb, Institute for Sexual and Gender Minority Health and Wellbeing, Northwestern University
References
- Adamson SJ, Kay-Lambkin FJ, Baker AL, Lewin TJ, Thornton L, Kelly BJ, & Sellman JD (2010). An improved brief measure of cannabis misuse: The Cannabis Use Disorders Identification Test-Revised (CUDIT-R). Drug and Alcohol Dependence, 110(1), 137–143. [DOI] [PubMed] [Google Scholar]
- Arnett JJ (2005). The developmental context of substance use in emerging adulthood. Journal of drug issues, 35, 235–254. [Google Scholar]
- Austin EL, & Bozick R (2012). Sexual orientation, partnership formation, and substance use in the transition to adulthood. Journal of Youth and Adolescence, 41, 167–178. [DOI] [PubMed] [Google Scholar]
- Ayala J, & Coleman H (2000). Predictors of depression among lesbian women. Journal of Lesbian Studies, 4(3), 71–86.24802684 [Google Scholar]
- Baams L, Bos HMW, & Jonas KJ (2014). How a romantic relationship can protect same-sex attracted youth and young adults from the impact of expected rejection. Journal of Adolescence, 37(8), 1293–1302. [DOI] [PubMed] [Google Scholar]
- Babor TF, Higgins-Biddle JC, Saunders JB, & Monteiro MG (2001). The Alcohol Use Disorders Identification Test: Guidelines for use in primary care. Geneva: World Health Organization. [Google Scholar]
- Balsam KF, Molina Y, Beadnell B, Simoni J, & Walters K (2011). Measuring multiple minority stress: The LGBT people of color microaggressions scale. Cultural Diversity and Ethnic Minority Psychology, 17(2), 163–174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bauermeister JA, Johns MM, Sandfort TGM, Eisenberg A, Grossman AH, & D’Augelli AR (2010). Relationship trajectories and psychological well-being among sexual minority youth. Journal of Youth and Adolescence, 39(10), 1148–1163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bostwick W, & Hequembourg A (2014). ‘Just a little hint’: Bisexual-specific microaggressions and their connection to epistemic injustices. Culture, Health & Sexuality, 16(5), 488–503. [DOI] [PubMed] [Google Scholar]
- Braithwaite SR, Delevi R, & Fincham FD (2010). Romantic relationships and the physical and mental health of college students. Personal Relationships, 17(1), 1–12. [Google Scholar]
- Claxton SE, DeLuca HK, van Dulmen MH (2015). The association between alcohol use and engagement in casual sexual relationships and experiences: A meta-analytic review of non-experimental studies. Archives of Sexual Behavior, 44, 837–856. [DOI] [PubMed] [Google Scholar]
- Cochran SD, Grella CE, & Mays VM (2012). Do substance use norms and perceived drug availability mediate sexual orientation differences in patterns of substance use? Results from the California Quality of Life Survey II. Journal of Studies on Alcohol and Drugs, 73, 675–685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen J (1988). Statistical power analysis for the behavioral sciences. New York, NY: Routledge Academic. [Google Scholar]
- Davila J, Steinberg SJ, Kachadourian L, Cobb R, & Fincham F (2004). Romantic involvement and depressive symptoms in early and late adolescence: The role of a preoccupied relational style. Personal Relationships, 11(2), 161–178. [Google Scholar]
- Diamond LM, & Savin-Williams R (2000). Explaining diversity in the development of same-sex sexuality among young women. Journal of Social Issues, 56(2), 297–313. [Google Scholar]
- Duncan GJ, Wilkerson B, & England P (2006). Cleaning up their act: The effects of marriage and cohabitation on licit and illicit drug use. Demography, 43(4), 691–710. [DOI] [PubMed] [Google Scholar]
- Dyar C, Feinstein BA, & London B (2014). Dimensions of sexual identity and minority stress among bisexual women: The role of partner gender. Psychology of Sexual Orientation and Gender Diversity, 1(4), 441–451. [Google Scholar]
- Feinstein BA, Latack JA, Bhatia V, Davila J, & Eaton NR (2016). Romantic relationship involvement as a minority stress buffer in gay/lesbian versus bisexual individuals. Journal of Gay & Lesbian Mental Health, 20(3), 237–257. [Google Scholar]
- Fleming CB, White HR, Oesterle S, Haggerty KP, & Catalano RF (2010). Romantic relationship status changes and substance use among 18- to 20-year-olds. Journal of Studies on Alcohol and Drugs, 71(6), 847–856. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Flores AR, Herman JL, Gates GJ, & Brown TNT (2016). How many adults identify as transgender in the United States? Los Angeles, CA: The Williams Institute. [Google Scholar]
- Furman W, & Collibee C (2014). A matter of timing: Developmental theories of romantic involvement and psychosocial adjustment. Development and Psychopathology, 26(4pt1), 1149–1160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gamarel KE, Reisner SL, Laurenceau J, Nemoto T, & Operario D (2014). Gender minority stress, mental health, and relationship quality: A dyadic investigation of transgender women and their cisgender male partners. Journal of Family Psychology, 28, 437–447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayes AF (2013). Introduction to mediation, moderation, and conditional process analysis. New York, NY: The Guilford Press. [Google Scholar]
- Hayfield N, Clarke V, & Halliwell E (2014). Bisexual women’s understandings of social marginalisation: ‘The heterosexuals don’t understand us but nor do the lesbians’. Feminism & Psychology, 24(3), 352–372. [Google Scholar]
- House JS, Umberson D, & Landis KR (1988). Structures and processes of social support. Annual Review of Sociology, 14(1), 293–318. [Google Scholar]
- Institute of Medicine. (2011). The health of lesbian, gay, bisexual, and transgender people: Building a foundation for better understanding. Washington, DC: The National Academies Press. [PubMed] [Google Scholar]
- James SE, Herman JL, Rankin S, Keisling M, Mottet L, & Anafi M (2016). The report of the 2015 U.S. transgender survey. Washington, DC: National Center for Transgender Equality. [Google Scholar]
- Johns MM, Pingel ES, Youatt EJ, Soler JH, McClelland SI, & Bauermeister JA (2013). LGBT community, social network characteristics, and smoking behaviors in young sexual minority women. American Journal of Community Psychology, 52, 141–154. [DOI] [PubMed] [Google Scholar]
- Kamp Dush CM, & Amato PR (2005). Consequences of relationship status and quality for subjective well-being. Journal of Social and Personal Relationships, 22, 607–627. [Google Scholar]
- Katz-Wise S, & Hyde JS (2012). Victimization experiences of lesbian, gay, and bisexual individuals: A meta-analysis. The Journal of Sex Research, 49, 142–167. [DOI] [PubMed] [Google Scholar]
- Kornblith E, Green R, Casey S, & Tiet Q (2016). Marital status, social support, and depressive symptoms among lesbian and heterosexual women. Journal of Lesbian Studies, 20, 157–173. [DOI] [PubMed] [Google Scholar]
- Kurdek LA (2005). What do we know about gay and lesbian couples? Current Directions in Psychological Science, 14(5), 251–254. [Google Scholar]
- Lamb KA, Lee GR, & DeMaris A (2003). Union formation and depression: Selection and relationship effects. Journal of Marriage and Family, 65(4), 953–962. [Google Scholar]
- Lytle MC, De Luca SM, & Blosnich JR (2014). The influence of intersecting identities on self-harm, suicidal behaviors, and depression among lesbian, gay, and bisexual individuals. Suicide and Life-Threatening Behavior, 44, 384–391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marshal MP, Dermody, Sarah S, Cheong J., Burton CM, Friedman MS, Aronda F, & Hughes T. (2013). Trajectories of depressive symptoms and suicidality among heterosexual and sexual minority youth. J Youth Adolescence, 42,1243–1256 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mereish EH, Katz-Wise SL, & Woulfe J (2017). Bisexual-specific minority stressors, psychological distress, and suicidality in bisexual individuals: The mediating role of loneliness. Prevention Science, 18(6), 716–725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meyer IH (2003). Prejudice, social stress, and mental health in lesbian, gay, and bisexual populations: Conceptual issues and research evidence. Psychological Bulletin, 129(5), 674–697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mustanski B, Greene GJ, Ryan D, & Whitton SW (2015). Feasibility, acceptability, and initial efficacy of an online sexual health promotion program for LGBT youth: The queer sex ed intervention. The Journal of Sex Research, 52(2), 220–230. [DOI] [PubMed] [Google Scholar]
- Muthén BO, & Satorra A (1995). Technical aspects of Muthén’s liscomp approach to estimation of latent variable relations with a comprehensive measurement model. Psychometrika, 60, 489–503. [Google Scholar]
- National Institutes of Health. (2001). NIH policy on reporting race and ethnicity data. Retrieved from http://grants.nih.gov/grants/guide/notice-files/NOT-OD-01-053.html
- Needham BL (2012). Sexual attraction and trajectories of mental health and substance use during the transition from adolescence to adulthood. Journal of Youth and Adolescence, 41, 179–190. [DOI] [PubMed] [Google Scholar]
- Newcomb ME, & Mustanski B (2010). Internalized homophobia and internalizing mental health problems: a meta-analytic review. Clinical Psychology Review, 30, 1019–1029. doi: 10.1016/j.cpr.2010.07.003 [DOI] [PubMed] [Google Scholar]
- Oetjen H, & Rothblum ED (2000). When lesbians aren’t gay. Journal of Homosexuality, 39, 49–73. [DOI] [PubMed] [Google Scholar]
- Oswalt S, & Lederer A (2017). Beyond depression and suicide: The mental health of transgender college students. Social Sciences, 6, 20. [Google Scholar]
- Owen JJ, Rhoades GK, Stanley SM, & Fincham FD (2010). “Hooking up” among college students: Demographic and psychosocial correlates. Archives of Sexual Behavior, 39, 653–663. [DOI] [PubMed] [Google Scholar]
- Pilkonis PA, Choi SW, Reise SP, Stover AM, Riley WT, & Cella D (2011). Item banks for measuring emotional distress from the Patient-Reported Outcomes Measurement Information System (PROMIS®): Depression, anxiety, and anger. Assessment, 18, 263–283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reczek C, & Umberson D (2012). Gender, health behavior, and intimate relationships: Lesbian, gay, and straight contexts. Social Science & Medicine, 74(11), 1783–1790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reisner SL, Gamarel KE, Nemoto T, & Operario D (2014). Dyadic effects of gender minority stressors in substance use behaviors among transgender women and their non-transgender male partners. Psychology of Sexual Orientation and Gender Diversity,1, 63–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Richards C, Bouman WP, Seal L, Barker MJ, Nieder TO, & T’Sjoen G (2016). Non-binary or genderqueer genders. International Review of Psychiatry, 28(1), 95–102. [DOI] [PubMed] [Google Scholar]
- Roisman GI, Masten AS, Coatsworth JD, & Tellegen A (2004). Salient and emerging developmental tasks in the transition to adulthood. Child Development, 75(1), 123–133. [DOI] [PubMed] [Google Scholar]
- Rosenthal L, Deosaran A, Young DL, & Starks TL (2019). Relationship stigma and well-being among adults in interracial and same-sex relationships. Journal of Social and Personal Relationships, 1–21. DOI: 10.1177/0265407518822785 [DOI] [Google Scholar]
- Russell ST, & Consolacion TB (2003). Adolescent romance and emotional health in the United States: Beyond binaries. Journal of Clinical Child & Adolescent Psychology, 32, 499–508. [DOI] [PubMed] [Google Scholar]
- Ryan C, Huebner D, Diaz RM, & Sanchez J (2009). Family rejection as a predictor of negative health outcomes in White and Latino lesbian, gay, and bisexual young adults. Pediatrics, 123, 346–352. [DOI] [PubMed] [Google Scholar]
- Schuler MS, Rice CE, Evans-Polce RJ, & Collins RL (2018). Disparities in substance use behaviors and disorders among adult sexual minorities by age, gender, and sexual identity. Drug and alcohol dependence, 189, 139–146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simon RW, & Barrett AE (2010). Nonmarital romantic relationships and mental health in early adulthood: Does the association differ for women and men? Journal of Health and Social Behavior, 51, 168–182. [DOI] [PubMed] [Google Scholar]
- Staff J, Schulenberg JE, Maslowsky J, Bachman JG, O’Malley PM, Maggs JL, & Johnston LD (2010). Substance use changes and social role transitions: Proximal developmental effects on ongoing trajectories from late adolescence through early adulthood. Development and Psychopathology, 22(4), 917–932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Starks TJ, Robles G, Bosco SC, Dellucci TV, Grov C, & Parsons J (2019). The prevalence and correlates of sexual arrangements in a national cohort of HIV-negative gay and bisexual men in the United States. Archives of Sexual Behavior 48, 369–382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Talley AE, Sher KJ, & Littlefield AK (2010). Sexual orientation and substance use trajectories in emerging adulthood. Addiction, 105, 1235–1245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Umberson D (1987). Family status and health behaviors: Social control as a dimension of social integration. Journal of Health and Social Behavior, 28, 306–319. [PubMed] [Google Scholar]
- Vanassche S, Swicegood G, & Matthijs K (2013). Marriage and children as a key to happiness? Cross-national differences in the effects of marital status and children on well-being. Journal of Happiness Studies, 14, 501–524. [Google Scholar]
- Waite L, & Gallagher M (2000). The case for marriage: Why married people are happier, healthier and better off financially. New York, NY: Doubleday. [Google Scholar]
- Wayment HA, & Peplau LA (1995). Social support and well-being among lesbian and heterosexual women: A structural modeling approach. Personality and Social Psychology Bulletin, 21(11), 1189–1199. [Google Scholar]
- Whitton SW, Dyar C, Newcomb ME, & Mustanski B (2018a). Effects of romantic involvement on substance use among young sexual and gender minorities. Drug and Alcohol Dependence, 191, 215–222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whitton SW, Dyar C, Newcomb ME, & Mustanski B (2018b). Romantic involvement: A protective factor for psychological health in racially-diverse young sexual minorities. Journal of Abnormal Psychology, 127(3), 265–275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whitton SW, & Kuryluk AD (2014). Associations between relationship quality and depressive symptoms in same-sex couples. Journal of Family Psychology, 28(4), 571–576. [DOI] [PubMed] [Google Scholar]
- Whitton SW, Dyar CE, Mustanksi B, & Newcomb ME (2019). Intimate partner violence experiences of sexual and gender minority adolescents and young adults assigned female at birth. Psychology of Women Quarterly, 43, 232–249. Doi: 10.1177/0361684319838972 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whitton SW, Weitbrecht EM, Kuryluk AD, & Bruner MR (2013). Committed dating relationships and mental health among college students. Journal of American College Health, 61(3), 176–183. [DOI] [PubMed] [Google Scholar]