Highlights
-
•
The majority of people with OCD were negatively affected by the COVID-19 pandemic
-
•
Negative effects were more pronounced in people with washing compulsion
-
•
Worsening of OCD was associated with reduced mobility and interpersonal conflicts
-
•
Dysfunctional hygiene-related beliefs were related to greater symptom progression
Keywords: Obsessive-compulsive disorder, COVID-19, SARS-CoV-2, Pandemic, Contamination fear
Abstract
The COVID-19 pandemic has prompted global measures to prevent infection. Experts assume that it is particularly affecting people with obsessive-compulsive disorder (OCD), especially those with washing compulsions. Data, however, are currently lacking.
394 participants with OCD (n = 223 washers) participated in an online survey. Change in severity of OCD symptoms, reasons participants reported for the change (e.g., reduced mobility, reduced availability of cleaning products, economic factors, interpersonal conflicts), as well as participants’ beliefs and experience associated with COVID-19 were assessed.
72 % of the participants reported an increase in OCD. This increase was significantly stronger in washers compared to non-washers. The worsening of symptoms was primarily associated with reduced mobility and interpersonal conflicts. Dysfunctional hygiene-related beliefs were significantly higher in washers than non-washers and were associated with greater symptom progression. Washers were more confident than non-washers about providing other people with helpful advice related to infection preventions. Washers, however, received more negative feedback from others in response to the advice they provided than non-washers.
The majority of participants with OCD were negatively affected by the COVID-19 pandemic, and the negative effects were more pronounced in washers than in non-washers. Rapid interventions for OCD should be implemented to prevent long-term deterioration.
1. Introduction
With the outbreak of the COVID-19 pandemic (WHO, 2020), a large percentage of the world’s population has been exposed to multiple burdens, including immediate hazards such as the risk of infection as well as social isolation and economic insecurity. Based on the diathesis-stress model, which helps explain the development and maintenance of many mental disorders, these stresses may particularly affect people with preexisting mental disorders (Pfefferbaum & North, 2020; Yao, Chen, & Xu, 2020) due, for example, to low resilience, fewer social contacts, and reduced psychiatric care. Thus, an increase in symptom severity can be assumed and has already been noted; for example, the prevalence of anxiety and depression increased from 4% in 2019 to 20 % in 2020 in the Chinese general population (Li et al., 2020). Besides depression and anxiety, an increase at the start of the COVID-19 pandemic has also been suggested for substance use disorders (Ornell et al., 2020), eating disorders (Touyz, Lacey, & Hay, 2020), and obsessive-compulsive disorder (OCD, Fineberg et al., 2020; Fontenelle & Miguel, 2020).
For people with OCD, particularly those with contamination-related OCD (C-OCD) and washing compulsions (‘washers’), the situation during the COVID-19 pandemic is unique (Fontenelle & Miguel, 2020). Social distancing and frequent as well as ritualized washing behaviors, which patients themselves usually consider senseless or exaggerated (Abramowitz & Jacoby, 2014) and which are often associated with increased shame, have become not only standard but are advocated on official websites, such as the website of the WHO (https://www.who.int/emergencies/diseases/novel-coronavirus-2019/advice-for-public), and contamination fears have become real and well-founded. Moreover, due to panic shopping in the general population (e.g., stocking up on soaps, sanitizers, disinfectants), many patients with washing compulsions may be worried about or confronted with a lack of the cleaning products they need to perform their cleaning compulsions. Data from Italy supports the notion of the exacerbation of OCD symptoms due to the COVID-19 pandemic (Benatti et al., 2020; Prestia et al., 2020). Specifically, Benatti et al. (2020) have reported symptom worsening in approximately one third of their sample (N = 123), and Prestia et al. (2020) have showed that the presence of contamination symptoms before the first lockdown was associated with increased OCD symptom severity during the first lockdown in 2020 (N = 30).
In a consensus statement, the International College of Obsessive Compulsive Spectrum Disorders and the Obsessive-Compulsive Research Network of the European College of Neuropsychopharmacology have highlighted the necessity of adapting or even pausing treatment with exposure and response prevention (ERP) during the pandemic (Fineberg et al., 2020). Weighing the risks and benefits of treatment is certainly necessary as COVID-19 is highly contagious and ERP treatment for contamination-related OCD may involve, for example, touching highly frequented “public” surfaces without subsequent handwashing. According to current guidelines (e.g., the German Association for Psychiatry, Psychotherapy and Psychosomatics (DGPPN), Hohagen et al., 2015), however, ERP is an effective and recommended treatment for OCD, which also means that many people with OCD currently cannot start or continue ERP.
BesidesERP, dysfunctional beliefs are routinely targeted in cognitive-behavioral therapy (CBT; Clark, 2020) as they play a major role in the development and maintenance of OCD (Salkovskis, 1985). Of these, beliefs related to threats and positive beliefs about rituals may be relevant to the COVID-19 pandemic. Overestimation of threat refers to the overestimation of the likelihood of danger in general and of personal vulnerability to adverse events (Moritz and Pohl, 2009; Obsessive Compulsive Cognitions Working Group, 1997) and is more frequently found in people with OCD compared to, for example, people with panic disorder, pathological gambling (Anholt et al., 2004), or depression as well as nonclinical controls (Miegel, Jelinek, & Moritz, 2019). Positive beliefs about rituals (e.g., “I must perform rituals or I will never stop thinking about contamination"; McNicol & Wells, 2012, p. 331) form an essential part in the metacognitive model of OCD and have been shown to be associated with OCD symptoms (Solem, Myers, Fisher, Vogel, & Wells, 2010).
However, the pandemic may also strengthen functional beliefs if, for example, patients with OCD realize that their compulsions are exaggerated. Additionally, people with OCD (particularly those with washing compulsions) may also experience relief due to reduced stigmatization or other factors. Some patients may (paradoxically) even experience a sense of competence as a result of their functional beliefs and use of adaptive coping strategies (which have been highlighted by Moritz et al. (2018) using the Maladaptive and Adaptive Coping Styles Questionnaires (MAX)). So far, aspects sensitive to self-domains have primarily been studied to explain the occurrence of intrusions and thus are mostly related to “areas of life where the person lacks confidence” (p. 1, Abramovitch et al., 2020; Aardema & Wong, 2020; Doron, Kyrios, & Moulding, 2007). However, perceived competence, which is related to self-worth (Doron et al., 2007), may change over the course of the illness and even increase in some areas of life. People with C-OCD often have years of involvement and experience with topics such as “virus” and “disease,” particularly in the domain of “infection prevention.” Their former “problem” (having OCD) may even turn into a “virtue” (expertise) as people with C-OCD may give other people advice on how to, for example, best avoid contamination or clean their hands or maybe even shop for groceries.
First evidence on OCD during the start of the COVID-19 pandemic points to an increase of OCD in Italy (Benatti et al., 2020; Prestia et al., 2020). However, large sample sizes are lacking, and so are data for Germany. We thus aimed to fill this gap with the present study by investigating the influence of the COVID-19 pandemic on persons with OCD, in particular people with washing compulsions (‘washers’) in regard to change in symptom severity, the reasons for the change, and dysfunctional as well as functional beliefs during the COVID-19 pandemic. As no questionnaires were available at the start of the study and the pandemic was spreading quickly across Europe, we opted for the development of relevant exploratory questions by expert consensus.
2. Material and methods
2.1. Recruitment and procedure
Participants in Germany were recruited between March 23, 2020, and May 18, 2020. We aimed at recruiting a representative sample with manifest OCD in Germany. For this purpose, participants were recruited with the help of the German Society for Obsessive Compulsive Disorders (DGZ: Deutsche Gesellschaft Zwangserkrankungen e.V., www.zwaenge.de), which is a German nonprofit organization dedicated to helping people affected by OCD and their relatives to combat the disorder and to educate clinicians about effective treatment (Peters, 2009). Participants were also recruited through German psychiatric institutions treating patients with OCD as well as through an existing database of patients with OCD who had participated in previous studies and had consented to be contacted again.
During this time, Germany was largely under lockdown (e.g., restricted social contact), but the restrictions varied slightly among the German federal states (Steinmetz, Batzdorfer, & Bosnjak, 2020). For recruitment, a short statement on the aims of the study as well as an Internet link to an online survey was posted on the website of the DGZ or sent to potential participants via email who had given previous consent. The survey was carried out via the online platform Unipark/Questback® (Globalpark AG). At the beginning of the survey, electronic informed consent was obtained. Afterwards, demographic information (e.g., gender, age), medical history, and current severity of OCD and depression as well as change in symptoms since the beginning of the COVID-19 pandemic and patients’ reported reasons for the change as well as their dysfunctional and functional beliefs were assessed (see below for more details regarding questionnaires). Inclusion criteria were age between 18 and 80 years, a diagnosis of OCD in the past by a mental health professional (e.g., psychiatrist, psychotherapist, self-report), and completion of at least the Obsessive-Compulsive Inventory-Revised (OCI-R) and the first block of questions on OCD during the COVID-19 pandemic (reasons for increase or decrease in symptoms). Multiple logins from the same computer were precluded via “cookies.”
The research was conducted in accordance with the Declaration of Helsinki and was approved by the responsible ethics committee (LPEK-0131). Participants received a link to download a PDF manual on techniques to improve self-esteem as compensation for their participation.
2.2. Participants
In total 1,905 participants accessed the survey. Of these 1,289 only viewed the first page of the survey, 5 did not agree to informed consent, and 611 gave electronic informed consent. Of the latter, 214 participants were excluded due to inclusion and exclusion criteria (n = 140 did not answer the first block of questions on change in OCD symptomatology due to the COVID-19 pandemic, n = 61 did not report a verified OCD diagnosis by a mental health expert, n = 13 were not within the age range). Moreover, n = 3 participants were excluded due to a stereotypical pattern in their psychopathology ratings (i.e., the same value was entered throughout the psychopathology assessment). The final sample comprised 394 participants.
2.3. Assessment
The German version of the Obsessive–Compulsive Inventory-Revised (OCI-R; Foa et al., 2002; Gönner, Leonhart, & Ecker, 2008) was used to assess the severity of participants’ OCD. Studies have shown the inventory has good to excellent psychometric properties (Foa et al., 2002; Huppert et al., 2007), and its administration via the Internet has been shown to be equivalent to paper-and-pencil administration (Coles, Cook, & Blake, 2007). In addition to the total score, six subscales may be calculated: washing (items 5, 11, and 17), obsessing (items 6, 12, and 18), checking (items 2, 8, and 14), neutralizing (items 4, 10, and 16), hoarding (items 1, 7, and 13), and ordering (items 3, 9, and 15). Clinical benchmarks and norm values have recently been published for the English version of the OCI-R, with 0–15 points indicating mild, 16–27 points moderate, and 28–72 points severe OCD (Abramovitch, Abramowitz, Riemann, & McKay, 2020).
To assess severity of depression, we used the German version of the Patient Health Questionnaire (PHQ-9, Löwe, Kroenke, Herzog, & Gräfe, 2004). The PHQ-9 represents the depression module of the PHQ-D and uses 9 items rated on a 4-point Likert-scale (response options rated over the last two weeks: 0 = not at all, 1 = several days, 2 = more than half the days, 3 = nearly every day). Accordingly, scores range from 0 to 27. For the English version, Kroenke, Spitzer, and Williams (2001) have suggested that total scores of 5, 10, 15, and 20 points refer to mild, moderate, moderately severe, and severe depression, respectively. The questionnaire has good validity and reliability (Löwe et al., 2004; Martin, Rief, Klaiberg, & Braehler, 2006)
2.4. OCD in the COVID-19 pandemic
To assess consequences of the COVID-19 pandemic for people with OCD, we developed a new questionnaire. Items of the questionnaire were generated and based on consensus rating by five OCD experts and on previous questionnaires we developed. This was necessary as at the time of our study no such questionnaire existed. The questionnaire inquired about (1) demographic information, such as age and gender, as well as predominant OCD symptoms (obsessions, washing/cleaning, checking, symmetry/ordering, hoarding, and other); (2) reasons for the change in symptom severity (reduced mobility, availability of cleaning/hygiene products, economic factors, lack of availability of doctors/therapist, interpersonal conflicts) as rated on a 5-point Likert scale, with 1 = significantly increased to 5 = significantly decreased; (3) the change in OCD symptom severity (total, obsessions, compulsion, avoidance) as rated on a 5-point Likert scale, with 1 = significantly decreased to 5 = significantly increased (items largely corresponded to a scale used to quantify change during the COVID-10 pandemic in eating disorders, Schlegl, Maier, Meule, & Voderholzer, 2020; Schlegl, Meule, Favreau, & Voderholzer, 2020); (4) dysfunctional and functional beliefs associated with COVID-19 (for items, see Table 3) rated on a Likert scale ranging from 1 = does not apply at all to 5 = totally applies; (5) experience of self-competence associated with prevention of infection with COVID-19 (e.g., giving other people helpful hygiene tips; for items, see Table 4) rated on a Likert scale ranging from 1 = totally applies to 6 = does not apply at all. The allocation of beliefs as functional versus dysfunctional was determined by five experts on OCD as no suitable questionnaire was available at the time of assessment (see above). The items on dysfunctional beliefs were related to overestimation of threat (e.g., “My fears about the dangers in the world are confirmed”) and to positive beliefs about rituals (e.g., “Coronavirus is the result of people being very careless about hygiene”) and were adapted for the COVID-19 pandemic. The items on functional beliefs (e.g., “The threat associated with coronavirus makes me realize how exaggerated my compulsions are”) were related to items of the adaptive coping scale of the MAX (Moritz et al., 2018) but were also adapted for the COVID-19 pandemic.
Table 3.
Dysfunctional and Functional Beliefs Related to COVID-19 in Participants with OCD (n = 387), Rated on a 5-Point Likert Scale Ranging from 1 = Does not apply at all to 5 = Totally applies.
| Non-Washers (n = 167) |
Washers (n = 220) |
Group Comparison |
Total Sample (n = 387) (results for washers are in square brackets) |
||||
|---|---|---|---|---|---|---|---|
| Item | M | SD | M | SD | Cohen’s d [CI95%] | Statistics | Correlation with the change in severity of OCD |
| Other people are now realizing how dangerous viruses and germs are. | 2.59 | 1.22 | 3.54 | 1.33 | 0.74 [0.532–0.948] |
t(385) = 7.249, p < .001 |
r = .219, p < .001 [r = .194, p = .004] |
| Coronavirus is the result of people being very careless about hygiene. | 1.81 | 1.06 | 2.53 | 1.36 | 0.581 [0.376–0.786] |
t(384.7) = 5.894, p < .001 |
r = .180, p < .001 [r = .208, p = .002] |
| My fears about the dangers in the world are confirmed. | 2.47 | 1.30 | 3.04 | 1.40 | 0.42 [0.216–0.623] |
t(385) = 4.093, p < .001 |
r = .291, p < .001 [r = .320, p < .001] |
| The threat associated with coronavirus makes me realize how exaggerated my compulsions are. | 2.12 | 1.21 | 2.23 | 1.14 | 0.094 [−0.107–0.295] |
t(385) = 0.935, p = .350 |
r = −.060, p = .237 [r = −.191, p = .004] |
| Coronavirus does not frighten me as much as I thought it would. | 2.78 | 1.27 | 2.72 | 1.43 | −0.044 [−0.245–0.157] |
t(375.7) = 0.437, p = .663 |
r = −.310, p < .001 [r = −.355, p < .001] |
| Coronavirus frightens me less than other people around me. | 2.74 | 1.32 | 2.47 | 1.38 | −0.199 [−0.401–0.002] |
t(385) = 1.943, p = .053 |
r = −.260, p < .001 [r = −.333, p < .001] |
| The general panic about the coronavirus calms me down. | 2.14 | 1.34 | 2.29 | 1.34 | 0.112 [−0.089–0.131] |
t(385) = 1.040, p = .299 |
r = −.116, p = .022 [r =− .137, p = .042] |
| Coronavirus has also increased some of my other fears. | 3.17 | 1.48 | 3.31 | 1.44 | 0.096 [−0.105–0.297] |
t(385) = 0.907, p = .365 |
r = .364, p < .001 [r = .359, p < .001] |
| I believe that the coronavirus is unmanageable. | 2.32 | 1.15 | 2.65 | 1.15 | 0.287 [0.085–0.489] |
t(385) = 2.764, p = .006 |
r = .180, p < .001 [r = .245, p < .001] |
Table 4.
Self-Competence Associated with COVID-19 Infection Prevention (n = 253) Rated on a 6-Point Likert Scale Ranging from 1 = Totally applies to 6 = Does not apply at all.
|
Non-Washers (n = 154) |
Washers (n = 199) |
Statistics | ||||
|---|---|---|---|---|---|---|
| Item | M | SD | M | SD | Cohen’s d [CI95%] | t-test |
| Due to my OCD, I could give many people helpful tips in the context of COVID-19 | ||||||
|
4.46 | 1.72 | 2.58 | 1.77 | −1.075 [−1.3 to −0.85] |
t(351) = 9.992, p < .001 |
|
4.29d | 1.79 | 2.19e | 1.57 | −1.258 [−1.49 to −1.025] |
t(299.5) = 11.570, p < .001 |
|
4.29 | 1.74 | 2.14 | 1.64 | −1.276 [−1.507 to −1.046] |
t(351) = 11.877, p < .001 |
| In the context of COVID-19, I have given other people helpful hygiene tips. | 4.54 | 1.66 | 3.77 | 1.78 | −0.445 [−0.658 to −0.233] |
t(351) = 4.149, p < .001 |
| The reaction of the people to my tips was (n = 239) | ||||||
|
3.63b | 1.80 | 3.89c | 1.53 | 0.159 [−0.104 − 0.422] |
t(237) = 1.175, p = .241 |
|
5.20b | 1.60 | 4.41c | 1.82 | −0.454 [−0.719 to −0.188] |
t(237) = 3.391, p = .001 |
Notes. a rating scale ranged from 1 totally applies at all to 7 = does not apply at all; bn = 89; cn = 150; dn = 151; en = 194.
2.5. Strategy of data analysis
All analyses were conducted with IBM SPSS® Statistics version 26. To investigate responses (numbers as well as relative frequencies), we combined response categories. For each scale, the categories except for no change or the medium point on the scale were combined, for example, significantly increased and somewhat increased, significantly decreased and somewhat decreased, does not apply at all and does not apply, and applies and totally applies. Additionally, we calculated means (and standard deviations) separately for the responses of participants with and without washing-related OCD (group membership was based on the participants’ responses regarding their predominant OCD symptoms) and investigated group differences by calculating Student’s t tests. For effects sizes, Cohen’s ds were calculated.
3. Results
The final sample is described in Table 1 . According to norm values, OCD severity was moderate to severe (OCI-R score: M = 27.64, SD = 11.47), and severity of depression was moderate (PHQ-9: M = 12.41, SD = 6.61). At the beginning of the survey, participants indicated that the following symptoms were at the core of their OCD: obsessions (n = 261, 66.2 %), washing/cleaning (n = 223, 56.6 %), checking (n = 197, 50 %), symmetry/ordering (n = 62, 15.7 %), hoarding (n = 22, 5.6 %), and other (n = 83, 21.1 %). As planned, the sample was split into participants with and without washing or cleaning compulsions (washers, n = 223; non-washers, n = 171). For a description of the subsamples, see Table 1.
Table 1.
Demographics: Means (or Frequencies) and Standard Deviations (or Percentages) for the Total Sample and the Subsamples (Washers vs. Non-Washers).
| Total sample (N = 394) |
Non-Washers (n = 171) |
Washers (n = 223) |
|||||
|---|---|---|---|---|---|---|---|
| M/n | SD/% | M/n | SD/% | M/n | SD/% | Statistics | |
| Age | 37.76 | 12.14 | 38.20 | 12.92 | 37.43 | 11.52 | t(342.82) = 0.613, p = .540 |
| Gender (female/ male/ diverse) |
291/ 101/2 |
73.9/25.6/0.5 | 116/54/1 | 67.8/31.6/ 0.6 |
175/47/1 | 78.5/21.1/0.4 | Cramer-V = 0.120, p = .058 |
| Illness duration | 17.40 | 12.46 | 18.10 | 12.92 | 16.85 | 12.09 | t(391) = 0.982, p = .327 |
| Psychopathology | |||||||
| PHQ-9 | 12.41a | 6.61 | 11.39b | 6.84 | 13.17c | 6.34 | t(382) = 2.630, p = .009 |
| Washing (OCI-R) |
7.12 | 4.22 | 3.49 | 3.24 | 9.91 | 2.35 | t(297.34) = 21.852, p < .001 |
| Obsessing (OCI-R) |
6.95 | 3.26 | 7.32 | 3.33 | 6.68 | 3.19 | t(392) = 1.931, p = .054 |
| Hoarding (OCI-R) |
2.36 | 2.70 | 2.27 | 2.79 | 2.42 | 2.64 | t(392) = 0.555, p = .580 |
| Ordering (OCI-R) |
3.86 | 3.45 | 4.13 | 3.66 | 3.65 | 3.27 | t(392) = 1.370, p = .172 |
| Checking (OCI-R) |
4.88 | 3.57 | 5.03 | 3.72 | 4.77 | 3.46 | t(392) = 0.710, p = .478 |
| Neutralizing (OCI-R) | 2.46 | 3.08 | 2.56 | 3.09 | 2.39 | 3.09 | t(392 = 0.546, p = .586 |
| OCI-R total score | 27.64 | 11.47 | 24.80 | 11.39 | 29.82 | 11.06 | t(392) = 4.406, = p < .001 |
Note. OCI-R = Obsessive-Compulsive Inventory-Revised; PHQ-9 = Patient Health Questionnaire-9; an = 384; bn = 165; cn = 219.
3.1. Changes in OCD and reasons for the changes
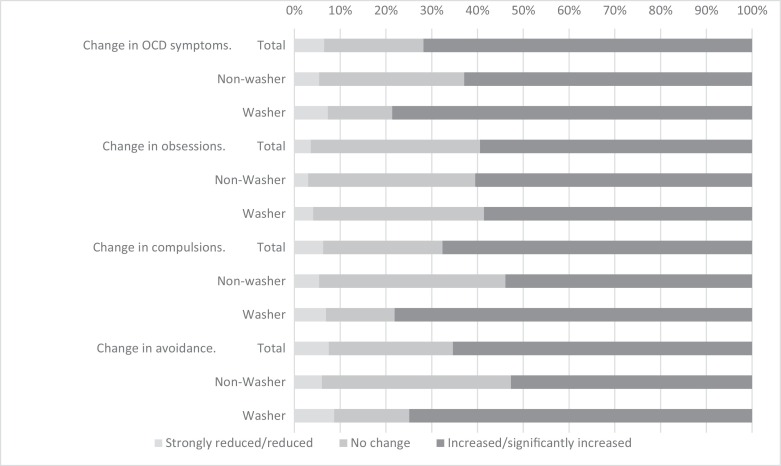
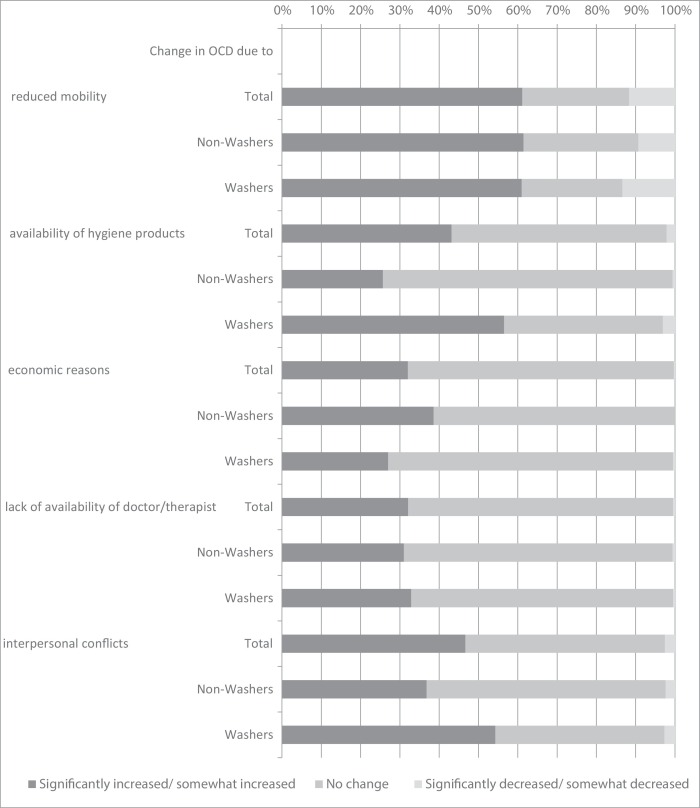
Changes in OCD symptoms due to the COVID-19 pandemic are displayed in Fig. 1 and the reasons for the changes as reported by the patients are given in the online Appendix (Fig. A ). The majority of participants (71.8 %) reported an increase in the severity of their OCD symptoms (see Fig. 1). Positive correlations occurred between the OCI-R total score and change in general OCD severity at small to medium magnitude (r = .268, p < .001), obsessions (r = .270, p < .001), compulsions (r = .304, p < .001), and avoidance (r = .208, p < .001). Participants primarily associated the increase with reduced mobility and interpersonal conflicts (see Fig. A, online Appendix). However, a minority experienced a decrease in symptoms (6.5 %), and 21.7 % reported no change in symptoms.
Fig. 1.
Reported Effects of the COVID-19 Pandemic in Obsessive-Compulsive Symptomatology for the Total Sample (n = 387), Washers (n = 220), and Non-Washers (n = 167).
Fig. A.
Changes in Obsessive-Compulsive Disorder and Reasons Given for the Changes in the Total Sample (N = 394), in Washers (n = 223), and in Non-Washers (n = 171).
When subsamples were compared, washers indicated a significantly greater increase in the severity of OCD symptoms with small to medium effect size, in particular regarding compulsions and avoidance behavior (but not obsessions) in comparison to non-washers. Washers and non-washers differed in the reasons they reported for the change in OCD symptom severity. Washers more than non-washers associated the availability of cleaning products and interpersonal conflicts with the increase in OCD symptoms with a medium effect, whereas non-washers associated the increase in OCD symptoms more with economic factors than washers did (see Table 2 ).
Table 2.
Comparison of Washers vs. Non-Washers Regarding Effects of the COVID-19 Pandemic on Obsessive-Compulsive Symptomatology and Reasons for the Change.
| Non-Washers (n = 171) |
Washers (n = 223) |
|||||
|---|---|---|---|---|---|---|
| Item | M | SD | M | SD | Cohen’s d [CI95%] | Statistics |
| Change in | ||||||
| OCD symptomsa | 3.78b | 0.86 | 4.00c | 0.93 | 0.244 [0.042 − 0.446] |
t(385) = 2.385, p = .018 |
| obsessionsa | 3.78b | 0.83 | 3.81c | 0.94 | 0.034 [−0.168 − 0.235] |
t(376.3) = 0.324, p = .746 |
| compulsionsa | 3.71b | 0.93 | 4.04c | 0.91 | 0.359 [0.156 − 0.562] |
t(353.4) = 3.523, p < .001 |
| avoidancea | 3.66b | 0.94 | 4.14c | 1.05 | 0.478 [0.274 − 0.682] |
t(385) = 4.571, p = .001 |
| Change in OCD due to | ||||||
| reduced mobilityd | 2.22 | 1.01 | 2.26 | 1.06 | 0.039 [−0.161 − 0.238] |
t(392) = 0.402, p = .689 |
| availability of cleaning/hygiene productsd | 2.68 | 0.60 | 2.20 | 0.89 | −0.617 [−0.821 to −0.413] |
t(385.9) = 6.485, p < .001 |
| economic factorsd | 2.49 | 0.71 | 2.67 | 0.61 | 0.275 [0.075 − 0.475] |
t(331.9) = 2.687, p = .008 |
| lack of availability of doctors/therapist d | 2.61 | 0.67 | 2.56 | 0.73 | −0.071 [−0.27 to −0.128] |
t(392) = 0.812, p = .417 |
| interpersonal conflictsd | 2.55 | 0.74 | 2.23 | 0.89 | −0.386 [−0.587 to −0.185] |
t(389.7) = 3.859, p < .001 |
Notes. a rated on a 5-point Likert scale with 1 = significantly decreased to 5 = significantly increased; bn = 167; cn = 220; d rated on a 5-point Likert scale with 1 = significantly increased to 5 = significantly decreased.
3.2. Dysfunctional and functional beliefs associated with COVID-19
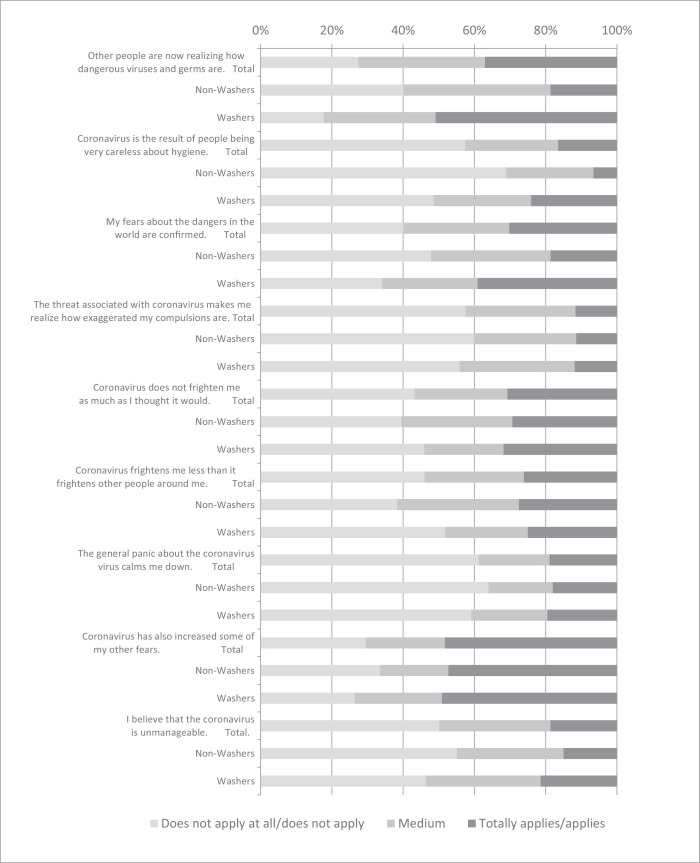
Participants’ dysfunctional and functional beliefs associated with COVID-19 are displayed in the online Appendix (Fig. B ). The statements “Corona has also increased some of my other fears” (48.32 %) and “Other people are now realizing how dangerous viruses and germs are” (36.95 %) received the highest endorsement by participants in the total sample. Importantly, washers agreed significantly more than non-washers with dysfunctional hygiene-related beliefs such as “Other people are now realizing how dangerous viruses and germs are,” “Coronavirus is the result of people being very careless about hygiene,” “My fears about the dangers in the world are confirmed,” and “I believe that the coronavirus is unmanageable.” Groups did not differ in functional beliefs associated with COVID-19, such as “The threat associated with coronavirus makes me realize how exaggerated my compulsions are,” “Coronavirus does not frighten me as much as I thought it would,” and “The general panic about the coronavirus calms me down” (see Table 3 ). As washers (M = 29.82, SD = 11.06) displayed a higher OCI-R total score than non-washers (M = 24.80, SD = 11.39, t(392) = 4.406, p < .001, see Table 1), we recalculated analyses with the OCI-R total score as a covariate, which did not change the results. Reported changes in OCD symptomatology during the COVID-19 pandemic correlated with dysfunctional beliefs in the total sample as well as in washers (see Table 3). Dysfunctional beliefs about hygiene were associated with an increase in OCD symptoms, whereas functional beliefs were associated with a decrease in symptoms. Most correlations were small to moderate in magnitude and stayed significant after correction for multiple testing (level of significance was reduced to p < 0.002, Bonferroni correction).
Fig. B.
Dysfunctional and Functional Beliefs Related to COVID-19 (n = 387) Rated on a 5-Point Likert Scale Ranging from 1 = Does not apply at all to 5 = Totally applies in the Total Sample (n = 387), in Washers (n = 220), and Non-Washers (n = 167).
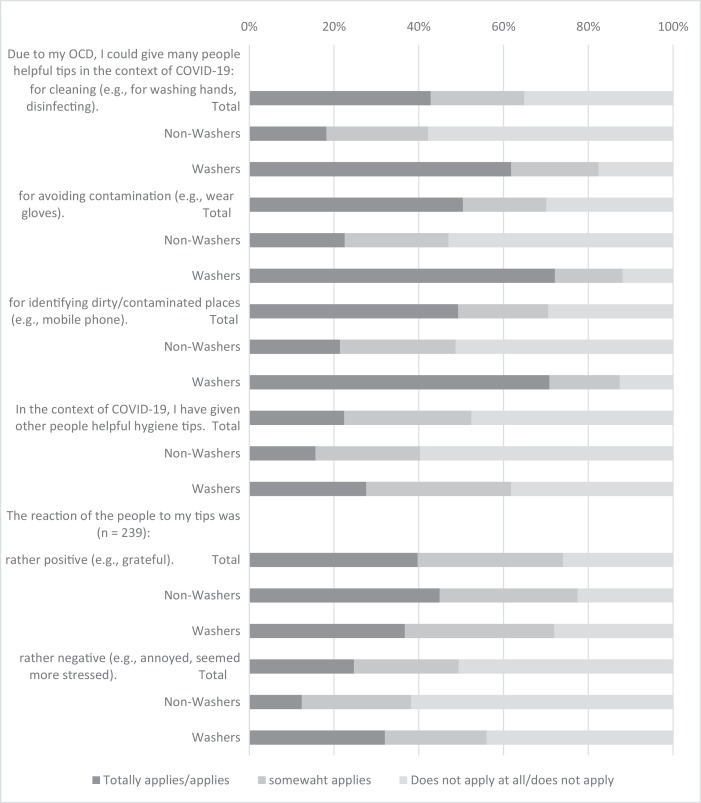
3.3. Self-Competence
Ratings regarding self-competence associated with prevention of infection with COVID-19 are displayed in Fig. 2 for the total sample as well as for washers and non-washers. Almost half of the participants (total sample) indicated that they could provide other people with helpful hygiene recommendations during the COVID-19 pandemic (infection prevention). This especially applied to washers, as indicated by large effect sizes (see Table 4 ). However, only 22.4 % of the total sample indicated that they had actually given other people advice, which again applied significantly more to washers with a medium effect size. Other people’s reactions to these recommendations included both positive feedback (39.7 %) and negative feedback (24.7 %), with washers receiving significantly more negative feedback than non-washers with a medium effect size (see Table 4). Again, results remained unchanged when the OCI-R total score was used as a covariate.
Fig. 2.
Self-Competence Associated with COVID-19 Infection Preventions (n = 253).
4. Discussion
The aim of the current study was to investigate changes in the severity of OCD symptoms during the COVID-19 pandemic in a large online sample. Due to the unique situation of people with washing compulsions (washers), whose thoughts and behaviors are often primarily concerned with infection prevention (long before as well as during the pandemic), we particularly wanted to assess whether washers were affected differently in comparison to non-washers. In summary, participants with OCD reported that the severity of their OCD symptoms increased due to the COVID-19 pandemic, and the negative effects were more pronounced in washers in comparison to non-washers.
In the total sample, 72 % of participants reported an increase in the severity of OCD. This increase in symptom severity was particularly true for washers in comparison to non-washers. Specifically, washers reported a larger increase than non-washers in compulsions and avoidance behavior but not in obsessions. It is possible that our questions regarding changes in OC symptoms were only rated with regard to pre-pandemic OCD and not with regard to change in OCD phenotype (e.g., the new occurrence of contamination-related symptoms in non-washers). Government recommendations for cleaning behavior and social distancing phenomenologically resemble compulsions and avoidance behavior. Accordingly, washers, but not non-washers, may have interpreted “COVID-19-related behaviors” as part of their pre-pandemic OCD-related symptoms. This would explain why pre-pandemic obsessions did not increase to a larger degree in washers. In total, however, about 60 % of the sample (washers and non-washers) indicated that their obsessions increased during the pandemic, which emphasizes the heightened distress experienced by both groups. Future studies should also address the occurrence of new contamination-related obsessions or compulsions in washers and any changes in OCD phenotypes (e.g., from non-washing to washing compulsions) as a result of the pandemic (see Benatti et al., 2020 for first evidence of an increase in new obsessions and compulsions).
Worsening of symptoms were primarily associated with the reduced mobility and interpersonal conflicts during the pandemic in the total sample. Washers and non-washers significantly differed in three of the five reasons associated with the changes in symptom severity. While reduced mobility and changes in health care (lack of availability of doctors/therapist) affected both groups to a similar degree, availability of cleaning products and interpersonal conflicts affected washers more negatively than non-washers. Surprisingly, non-washers associated economic factors more strongly with an increase in OCD severity than washers. An increased economic burden on the individual level may have caused heightened levels of distress and, in cases of distress intolerance (as postulated in OCD; e.g., Laposa, Collimore, Hawley, & Rector, 2015), may have also fostered hopelessness and worry, such as about the individual’s job situation, thus increasing psychopathology. As we did not ask participants about their yearly income or employment status, it is possible that subsamples differed in this regard (e.g., more non-washers than washers were working in businesses negatively affected by the pandemic or more washer than non-washers were receiving financial aid from the government, which was not reduced during the pandemic).
At the time of assessment, severity of OCD as assessed by the OCI-R was higher washers than in non-washers. As psychopathological data on the participants was not available before the outbreak of the pandemic, we do not know whether this difference represents a larger increase (as suggested for the increase in the prevalence of depression and anxiety by Li et al., 2020) in symptom severity in this subsample or whether they were already more affected by OCD before the pandemic.
Besides changes in the severity of OCD symptoms and the participants’ reasons for the changes, we also investigated dysfunctional and functional beliefs associated with COVID-19 in the sample. None of the beliefs was endorsed by more of 50 % of the total sample. However, washers agreed significantly more than non-washers with the hygiene-related dysfunctional beliefs (e.g., “Other people are now realizing how dangerous viruses and germs are,” “Coronavirus is the result of people being very careless about hygiene,” “My fears about the dangers in the world are confirmed,” “I believe that the coronavirus is unmanageable”). No differences between groups appeared for functional beliefs (“The threat associated with coronavirus makes me realize how exaggerated my compulsions are,” “Coronavirus does not frighten me as much as I thought it would,” and “The general panic about the coronavirus calms me down”), which were only endorsed by 31 % or less of the total sample. Still, higher agreement with hygiene-related dysfunctional beliefs was associated with an increase in OCD symptom severity, whereas higher agreement with functional beliefs was associated with a decrease in OCD symptom severity confirming the importance of beliefs in the maintenance of OCD (Salkovskis & McGuire, 2003). Other potential reasons for a decrease in OCD symptoms during the COVID-19 pandemic could be as decrease in experienced stigmatization and shame (e.g., due to measures taken for infection prevention, increased fear of contamination in the general population). However, this was not assessed in the present study.
Finally, most of the participants, particularly washers, endorsed that they could give helpful advice for infection prevention (e.g., regarding cleaning or avoiding contamination). However, only about half of the participants actually gave advice to other people. While only 40 % of the participants endorsed having received positive feedback, 25 % endorsed having received negative feedback as a result of their advice. Most importantly, washers indicated they had received more negative feedback compared to non-washers. This is clinically important as self-esteem is generally considered low in OCD (Ehntholt, Salkovskis, & Rimes, 1999; Husain et al., 2014) and has also been suggested as an important factor for change in CBT (Schwartz et al., 2017). Negative feedback in a domain where patients consider themselves experts may particularly affect their self-esteem and initiate or promote progression of symptoms.
While the study has certain strengths, such as the rather large sample size, data collection during the German lockdown, and strict inclusion and exclusion criteria (e.g., OCD diagnosis by a mental health professional), there are also some limitations that need to be discussed. First, we cannot exclude a selection bias. While the severity of OCD (OCI-R: M = 27.64, SD = 11.47) was at least as high as in other online studies on OCD (e.g., Hauschildt, Dar, Schröder, & Moritz, 2019; Herbst et al., 2014), significantly more women (74 %) than men participated in the currently study. Although OCD generally affects men and women equally, contamination-related OCD is more prevalent in women (American Psychiatric Association, 2014), and the percentage of women has previously been reported to be particularly high in online studies (during the COVID-19 pandemic, for example, 65 % were women in Qiu et al., 2020), potentially explaining the high participation of women in our study. While the choice of sampling method has previously been emphasized to estimate the change in prevalence of mental disorders during COVID-19 (Pierce et al., 2020), we would like to highlight that we did not estimate OCD prevalence in the current study. The aim of the study was to assess the effects of the COVID-19 pandemic on people with pre-pandemic OCD. To ensure high-quality data, we recruited a sample size of nearly 400 participants via diverse sources (such as clinics, patient associations, established databases) and used established psychopathological measures, and we also excluded participants with systematic response patterns. Still, it is likely that people who were particularly suffering during the COVID-19 pandemic were more likely to participate in the current study, potentially overestimating the effects. On the other hand, the effects might be underestimated as strongly affected people may not have been motivated to participate in the study. Longitudinal designs are necessary, using psychopathological data assessed before the outbreak of the pandemic, to fully confirm our interpretations.
Second, the assessment relied on self-report. This includes, for example, the participants’ assessment of their current symptom severity in OCD (OCI-R) and depression (PHQ-9), changes in OCD symptoms during the COVID-19 pandemic, and the declaration of an expert-confirmed OCD diagnosis. Although this is a limitation, it may have also increased study participation as OCD is highly associated with shame and is also called the “hidden” disorder (Hollander, 1997). To keep requirements for study participation to a minimum, this approach is essential to assess a representative OCD sample. Moreover, as no questionnaire on OCD during the COVID-19 pandemic existed at the time of our study, we developed new items in response to the speed of the outbreak in Europe and to allow us to quickly start the assessment. Items were carefully designed based on expert consensus and previously developed questionnaires, but we focused on the item level in the analyses rather than total scores. This highlights the exploratory nature of the study.
Third, we only assessed a limited number of reasons that participants associated with the changes in their OCD symptoms. Other reasons may have accounted for symptom change, and future studies would benefit from including an open question on reasons associated with the changes for exploratory purposes.
5. Conclusion
To our knowledge, this is the first German study to support the assumption that people with OCD (Fineberg et al., 2020; Fontenelle & Miguel, 2020), and in particular washers, are at risk of symptom increase during the COVID-19 pandemic. Our results underline the necessity of easily accessible and effective therapeutic interventions for this population to prevent potential long-term effects of the pandemic on this population.
6. Ethical standards
The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national and institutional committees on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008.
7. Financial support
This research received no specific grant from any funding agency, commercial or not-for-profit sectors.
Conflicts of interest
None.
Acknowledgements
We would like to thank Stella Schmotz to help setting up the online assessment.
Appendix A
Label not found for Float ElementLabel not found for Float Element Label not found for Float ElementLabel not found for Float Element
References
- Aardema F., Wong S.F. Feared possible selves in cognitive-behavioral theory: An analysis of its historical and empirical context, and introduction of a working model. Journal of Obsessive-Compulsive and Related Disorders. 2020;24:100479. doi: 10.1016/j.jocrd.2019.100479. [DOI] [Google Scholar]
- Abramovitch A., Abramowitz J., Riemann B., McKay D. Severity benchmarks and contemporary clinical norms for the Obsessive-Compulsive Inventory-Revised (OCI-R) Journal of Obsessive-compulsive and elated disorders. 2020;27(July):100557. doi: 10.1016/j.jocrd.2020.100557. [DOI] [Google Scholar]
- Abramowitz J.S., Jacoby R.J. Obsessive-compulsive disorder in the DSM-5. Clinical Psychology Science and Practice. 2014;21(3):221–235. doi: 10.1111/cpsp.12076. [DOI] [Google Scholar]
- American Psychiatric Association . In: Diagnostisches und statistisches manual psychischer störungen - DSM-5 [diagnostic and statistical manual of mental dsisorders - DSM-5] Falkai P., Wittchen H.-U., editors. Hogrefe Verlag; 2014. [Google Scholar]
- Anholt G.E., Emmelkamp P.M.G., Cath D.C., van Oppen P., Nelissen H., Smit J.H. Do patients with OCD and pathological gambling have similar dysfunctional cognitions? Behaviour Research and Therapy. 2004;42(5):529–537. doi: 10.1016/S0005-7967(03)00159-1. [DOI] [PubMed] [Google Scholar]
- Benatti B., Albert U., Maina G., Fiorillo A., Celebre L., Girone N. What happened to patients with obsessive compulsive disorder during the COVID-19 pandemic? A multicentre report from tertiary clinics in northern Italy. Frontiers in Psychiatry. 2020;11(July):1–5. doi: 10.3389/fpsyt.2020.00720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clark D.A. Cognitive-behavioral therapy for OCD and its subtypes. 2nd ed. The Guilford Press; 2020. [Google Scholar]
- Coles M.E., Cook L.M., Blake T.R. Assessing obsessive compulsive symptoms and cognitions on the internet: Evidence for the comparability of paper and Internet administration. Behaviour Research and Therapy. 2007;45(9):2232–2240. doi: 10.1016/j.brat.2006.12.009. [DOI] [PubMed] [Google Scholar]
- Doron G., Kyrios M., Moulding R. Sensitive domains of self-concept in obsessive-compulsive disorder (OCD): Further evidence for a multidimensional model of OCD. Journal of Anxiety Disorders. 2007;21(3):433–444. doi: 10.1016/j.janxdis.2006.05.008. [DOI] [PubMed] [Google Scholar]
- Ehntholt K.A., Salkovskis P.M., Rimes K.A. Obsessive–compulsive disorder, anxiety disorders, and self-esteem: An exploratory study. Behaviour Research and Therapy. 1999;37(8):771–781. doi: 10.1016/S0005-7967(98)00177-6. [DOI] [PubMed] [Google Scholar]
- Fineberg N.A., Van Ameringen M., Drummond L., Hollander E., Stein D.J., Geller D. How to manage obsessive-compulsive disorder (OCD) under COVID-19: A clinician’s guide from the International College of Obsessive Compulsive Spectrum Disorders (ICOCS) and the Obsessive-Compulsive and Related Disorders Research Network (OCRN) of the European College of Neuropsychopharmacology. Comprehensive Psychiatry. 2020;100(January):1521740. doi: 10.1016/j.comppsych.2020.152174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Foa E.B., Huppert J.D., Leiberg S., Langner R., Kichic R., Hajcak G. The Obsessive-Compulsive Inventory: Development and validation of a short version. Psychological Assessment. 2002;14(4):485–496. doi: 10.1037//1040-3590.14.4.485. [DOI] [PubMed] [Google Scholar]
- Fontenelle L.F., Miguel E.C. The impact of COVID-19 in the diagnosis and treatment of obsessive-compulsive disorder. Depression and Anxiety. 2020:510–511. doi: 10.1002/da.23037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gönner S., Leonhart R., Ecker W. The Obsessive-Compulsive Inventory-Revised (OCI-R): Validation of the German version in a sample of patients with OCD, anxiety disorders, and depressive disorders. Journal of Anxiety Disorders. 2008;22(4):734–749. doi: 10.1016/j.janxdis.2007.07.007. [DOI] [PubMed] [Google Scholar]
- Hauschildt M., Dar R., Schröder J., Moritz S. Congruence and discrepancy between self-rated and clinician-rated symptom severity on the Yale–Brown Obsessive-Compulsive Scale (Y-BOCS) before and after a low-intensity intervention. Psychiatry Research. 2019;273:595–602. doi: 10.1016/j.psychres.2019.01.092. [DOI] [PubMed] [Google Scholar]
- Herbst N., Voderholzer U., Thiel N., Schaub R., Knaevelsrud C., Stracke S. No talking, just writing! Efficacy of an internet-based cognitive behavioral therapy with exposure and response prevention in obsessive compulsive disorder. Psychotherapy and Psychosomatics. 2014;83(3):165–175. doi: 10.1159/000357570. [DOI] [PubMed] [Google Scholar]
- Hohagen F., Wahl-Kordon A., Lotz-Rambaldi W., Muche-Borowski C., editors. S3-Leitlinie Zwangsstörungen [S3 guidelines obsessive-compulsive disorder] Springer; 2015. [Google Scholar]
- Hollander E. Obsessive-compulsive disorder: The hidden epidemic. The Journal of Clinical Psychiatry. 1997;58(Suppl 12):3–6. [PubMed] [Google Scholar]
- Huppert J.D., Walther M.R., Hajcak G., Yadin E., Foa E.B., Simpson H.B. The OCI-R: Validation of the subscales in a clinical sample. Journal of Anxiety Disorders. 2007;21(3):394–406. doi: 10.1016/j.janxdis.2006.05.006. [DOI] [PubMed] [Google Scholar]
- Husain N., Chaudhry I., Raza-ur-Rehman, Ahmed G.R. Self-esteem and obsessive compulsive disorder. Journal of the Pakistan Medical Association. 2014;64(1):64–68. http://www. ncbi. nlm. nih. gov/pubmed/24605716 [PubMed] [Google Scholar]
- Kroenke K., Spitzer R.L., Williams J.B.W. The PHQ-9. Journal of General Internal Medicine. 2001;16:605–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Laposa J.M., Collimore K.C., Hawley L.L., Rector N.A. Distress tolerance in OCD and anxiety disorders, and its relationship with anxiety sensitivity and intolerance of uncertainty. Journal of Anxiety Disorders. 2015;33:8–14. doi: 10.1016/j.janxdis.2015.04.003. [DOI] [PubMed] [Google Scholar]
- Li J., Yang Z., Qiu H., Wang Y., Jian L., Ji J. Anxiety and depression among general population in China at the peak of the COVID‐19 epidemic. World Psychiatry : Official Journal of the World Psychiatric Association (WPA) 2020;19(2):249–250. doi: 10.1002/wps.20758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Löwe B., Kroenke K., Herzog W., Gräfe K. Measuring depression outcome with a brief self-report instrument: Sensitivity to change of the Patient Health Questionnaire (PHQ-9) Journal of Affective Disorders. 2004;81:61–66. doi: 10.1016/S0165-0327(03)00198-8. [DOI] [PubMed] [Google Scholar]
- Martin A., Rief W., Klaiberg A., Braehler E. Validity of the brief patient health questionnaire mood scale (PHQ-9) in the general population. General Hospital Psychiatry. 2006;28:71–77. doi: 10.1016/j.genhosppsych.2005.07.003. [DOI] [PubMed] [Google Scholar]
- McNicol K., Wells A. Metacognition and obsessive-compulsive symptoms: The contribution of thought-fusion beliefs and beliefs about rituals. International Journal of Cognitive Therapy. 2012;5(3):330–340. doi: 10.1521/ijct.2012.5.3.330. [DOI] [Google Scholar]
- Miegel F., Jelinek L., Moritz S. Dysfunctional beliefs in patients with obsessive-compulsive disorder and depression as assessed with the Beliefs Questionnaire (BQ) Psychiatry Research. 2019;272(5):265–274. doi: 10.1016/j.psychres.2018.12.070. [DOI] [PubMed] [Google Scholar]
- Moritz S., Pohl R.F. Biased processing of threat-related information rather than knowledge deficits contributes to overestimation of threat in obsessive-compulsive disorder. Behavior Modification. 2009;33(6):763–777. doi: 10.1177/0145445509344217. [DOI] [PubMed] [Google Scholar]
- Moritz S., Fink J., Miegel F., Nitsche K., Kraft V., Tonn P. Obsessive–compulsive disorder is characterized by a lack of adaptive coping rather than an excess of maladaptive coping. Cognitive Therapy and Research. 2018;42(5):650–660. doi: 10.1007/s10608-018-9902-0. [DOI] [Google Scholar]
- Obsessive Compulsive Cognitions Working Group Cognitive assessment of obsessive[HYPHEN]compulsive disorder. Behaviour Research and Therapy. 1997;35:667–681. doi: 10.1016/S0005-7967(97)00017-X. [DOI] [PubMed] [Google Scholar]
- Ornell F., Moura H.F., Scherer J.N., Pechansky F., Kessler F.H.P., von Diemen L. The COVID-19 pandemic and its impact on substance use: Implications for prevention and treatment. Psychiatry Research. 2020;289 doi: 10.1016/j.psychres.2020.113096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peters A. Hilfe zur Selbsthilfe – Die Deutsche Gesellschaft Zwangserkrankungen e. V. stellt sich vor [Help for self-help - The German Society for Obsessive Compulsive Disorders introduces itself] Notfall & Hausarztmedizin. 2009;35(02):e1–e4. doi: 10.1055/s-0029-1213751. [DOI] [Google Scholar]
- Pfefferbaum B., North C.S. Mental health and the Covid-19 pandemic. The New England Journal of Medicine. 2020 doi: 10.1056/NEJMp2008017. NEJMp2008017. [DOI] [PubMed] [Google Scholar]
- Pierce M., McManus S., Jessop C., John A., Hotopf M., Ford T. Says who? The significance of sampling in mental health surveys during COVID-19. The Lancet Psychiatry. 2020 doi: 10.1016/S2215-0366(20)30237-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prestia D., Pozza A., Olcese M., Escelsior A., Dettore D., Amore Mario. The impact of the COVID-19 pandemic on patients with OCD: Effects of contamination symptoms and remission state before the quarantine in a preliminary naturalistic study. Psychiatry Research. 2020;291 doi: 10.1016/j.psychres.2020.113213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qiu J., Shen B., Zhao M., Wang Z., Xie B., Xu Y. A nationwide survey of psychological distress among Chinese people in the COVID-19 epidemic: Implications and policy recommendations. General Psychiatry. 2020;33(2) doi: 10.1136/gpsych-2020-100213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salkovskis P.M. Obsessional-compulsive problems: A cognitive-behavioural analysis. Behaviour Research and Therapy. 1985;23(5):571–583. doi: 10.1016/0005-7967(85)90105-6. [DOI] [PubMed] [Google Scholar]
- Salkovskis P.M., McGuire J. Cognitive-behavioural theory of OCD. In: Menzies R.G., De Silva P., editors. Obsessive-compulsive disorder: Theory, research and treatment. Wiley; 2003. [Google Scholar]
- Schlegl S., Maier J., Meule A., Voderholzer U. Eating disorders in times of the COVID‐19 pandemic - Results from an online survey of patients with anorexia nervosa. The International Journal of Eating Disorders. 2020 doi: 10.1002/eat.23374. eat.23374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schlegl S., Meule A., Favreau M., Voderholzer U. Bulimia nervosa in times of the COVID-19 pandemic - Results from an online survey of former inpatients. European Eating Disorders Review. 2020 doi: 10.1002/erv.2773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schwartz C., Hilbert S., Schubert C., Schlegl S., Freyer T., Löwe B. Change factors in the process of cognitive-behavioural therapy for obsessive-compulsive disorder. Clinical Psychology & Psychotherapy. 2017;24(3):785–792. doi: 10.1002/cpp.2045. [DOI] [PubMed] [Google Scholar]
- Solem S., Myers S.G., Fisher P.L., Vogel P.A., Wells A. An empirical test of the metacognitive model of obsessive-compulsive symptoms: Replication and extension. Journal of Anxiety Disorders. 2010;24(1):79–86. doi: 10.1016/j.janxdis.2009.08.009. [DOI] [PubMed] [Google Scholar]
- Steinmetz H., Batzdorfer V., Bosnjak M. The ZPID lockdown measures dataset. ZPID Science Information Online. 2020;20(1) doi: 10.23668/psycharchives.3019. [DOI] [Google Scholar]
- Touyz S., Lacey H., Hay P. Eating disorders in the time of COVID-19. Journal of Eating Disorders. 2020;8(1):19. doi: 10.1186/s40337-020-00295-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- WHO . 2020. Mental health and psychosocial considerations during the COVID-19 outbreak. 18th March 2020.https://www.who.int/docs/default-source/coronaviruse/mental-health-considerations.pdf?sfvrsn=6d3578af_2 [Google Scholar]
- Yao H., Chen J.-H., Xu Y.-F. Patients with mental health disorders in the COVID-19 epidemic. The Lancet Psychiatry. 2020;7(4):e21. doi: 10.1016/S2215-0366(20)30090-0. [DOI] [PMC free article] [PubMed] [Google Scholar]