Highlights
-
•
U.S. adults reduced physical activity during the early pandemic period.
-
•
Reductions in walking and steps were larger for low-income and Hispanic adults.
-
•
More vigorous physical activity was reported by those who were active at home.
-
•
More steps were recorded by those who were active in their neighborhoods.
Keywords: Vigorous activity, Moderate activity, Walking, Step counts, Income
Abstract
COVID-19 restrictions and social-distancing may inhibit adults from attaining recommended levels of physical activity. This study examined early impact of COVID-19 pandemic on physical activity in adults during the first two months of restrictions in the U.S. and how physical activity locations were associated with physical activity levels during this period. Adults (N = 268) completed an online survey between April 10-May 25, 2020. Participants reported minutes of vigorous, moderate, and walking physical activity for past 7 days (early-COVID-19) and for a typical week in February 2020 (pre-COVID-19). Adults reported locations (e.g., home/garage, parks/trails) were they were active over the past 7 days. Past 12-month step count data were extracted from participants’ personal smartphones. Participants (18–74 years old, 22% Hispanic/Latino, 81% female) showed reductions in vigorous (M diff = −66.9 min/week), moderate (M diff = −92.4 min/week), walking (M diff -70.8 min/week), and step counts (M diff = –2232 steps/day) from the pre- to early-COVID19 periods. Reductions in walking and steps were larger for low-income and Hispanic/Latino adults. During early-COVID19, more vigorous and moderate activity were reported by those who were active in their home/garage or driveway/yard, and more steps were recorded by those who were active on the roads in their neighborhood or at parks/trails. We observed a decline in adults’ physical activity during the first two months of the COVID-19 pandemic based on retrospective self-report and device-based measures. Although these restrictions were necessary to slow the spread of the virus, data indicate that there may be unintended consequences on health-related behaviors.
1. Introduction
COVID-19, the respiratory disease caused by the SARS-CoV-2 virus, has been declared a pandemic by the World Health Organization and a national emergency in the United States of America (U.S.). As of the date this article was written (Sep. 30, 2020), there were 7.25 million COVID-19 cases and 207,000 related deaths recoded by the U.S. Centers for Disease Control and Prevention (CDC COVID Data Tracker, 2020). In order to limit the spread of COVID-19, state governments in the U.S. issued “Shelter-in-place” or “Stay-at-home” orders starting between March 19 and April 3, 2020 (National Law Review, 2020). Although a few states rescinded or ended these orders in late April and early May, most states extended the expiration dates through May 15–May 29, 2020. “Shelter-in-place” and “Stay-at-home” orders vary in scope from state to state but generally require “non-essential” businesses to close their physical offices or storefronts and continue their operations remotely. These guidelines require residents to remain at home except when performing essential activities including purchasing groceries and seeking medical treatment. Residents were allowed to take walks in outdoor spaces as long as they maintained social distancing of at least 6 feet away from people not in their households. Federal, state, and local public parks, trails, and beaches were also closed in many jurisdictions starting mid-to-late March with some re-openings occurring in late April and early May, and most others in early to late June.
Despite the public health necessity of these social-distancing measures in order to slow the spread of COVID-19 and ensure that medical facilities have adequate resources to address needs, they may impose restrictions on individuals’ ability to engage in sufficient levels of physical activity in order to maintain health and prevent further disease. More than 70 million Americans regularly access gyms and fitness facilities (IHRSA, 2020), indicating that closure of these businesses may have a profound effect on physical activity behaviors. Furthermore, restricted access to public parks, trails, and beaches may eliminate low- and no-cost opportunities for outdoor physical activity. By limiting reasons to leave the house, incidental physical activity (e.g., during errands or chores) and active transportation (e.g., biking to work, walking to public transit) may decline dramatically. Preliminary data on the impact of COVID-19 restrictions suggests that physical activity among U.S. adults was reduced between 32% and 48% during the first week of April 2020 (Evidation Health, 2020, Meyer et al., 2020).
The overall goal of the current study was to investigate the early impact of the COVID-19 pandemic on activity levels among U.S. adults during the first two months that “Shelter-in-place” and “Stay-at-home” orders were in place. The primary objective was to determine whether physical activity significantly declined from the pre-COVID-19 period (February 1–29, 2020) to the early-COVID-19 period (April 3–May 25, 2020), and whether changes in physical activity levels differed by self-reported ethnicity (Hispanic/Latino vs. non-Hispanic/Latino) and household income. The secondary objective was to describe the locations of physical activity during the early-COVID-19 period and examine the extent to which physical activity locations were associated with physical activity levels during this same period. Given emerging evidence of the potential immune-protective effect of cardiorespiratory exercise against complications of COVID-19 (Halabchi et al., 2020) combined with concerns that temporary lapses in physical activity can extend to permanent disengagement with the behavior (Bélisle et al., 1987), understanding the early effects of the COVID-19 pandemic on physical activity levels in U.S. adults is an important public health issue.
2. Methods
2.1. Study design
The current study assessed the effects of the COVID-19 pandemic on physical activity among U.S. adults through a combination of cross-sectional and retrospective methods. An online survey, completed between April 10 and May 25, 2020, assessed early-COVID-19 and pre-COVID-19 levels of physical activity. Past 12-month stepping behavior was retrospectively captured through a built-in accelerometer application on participants’ personal smartphone devices.
2.2. Recruitment and participants
A convenience sampling strategy, focused on recruiting general populations of adults living in the U.S. during the COVID-19 pandemic, was utilized. To minimize in-person interactions, potential respondents were electronically invited through various social media platforms (e.g., Facebook, Twitter, Reddit, LinkedIn) and university-based email list servs of students, faculty, and staff. Inclusion criteria were as follows: 18 years or older, able to speak and read English, live in the U.S., and own and regularly use an Android or iPhone smartphone that they are willing to use to complete app-based surveys for the duration of the study. Exclusion criteria were as follows: enrolled in another study related to physical activity behaviors, including studies monitoring physical activity, intervening on physical activity, or examining the effects of wearable fitness trackers. Once eligibility was determined, individuals agreed to participate through an online anonymous information sheet that described the study procedures, risks, and benefits. The Institutional Review Board of the University of Southern California determined that the study procedures presented no more than minimal risk and approved it as exempt from full review.
2.3. Procedures
Participants completed the survey in English through an online survey platform between April 10 and May 25, 2020, which cover the first one to two months after most U.S. states issued “Shelter-in-place” or “Stay-in-home” orders. The survey took approximately 30 min to complete. Participants had the option to complete it either on their mobile phone, tablet, or desktop device. Upon completion of the survey, participants were eligible to be entered into a lottery to win one of ten $50 gift cards.
2.4. Measures
Self-reported physical activity. Participants completed the International Physical Activity Questionnaire Short Form (IPAQ-SF) (Bauman et al., 2009) twice in the survey. The IPAQ is one of the most widely used report-based physical activity instruments and has demonstrated acceptable reliability and validity across a range of populations (Brown et al., 2004, Ekelund et al., 2006). The first time, the instructions asked individuals to “Think about the time you spent being physically active during a typical week in February 2020 (BEFORE THE COVID-19 PANDEMIC),” which represented the pre-COVID-19 period. The second time, the instructions asked individuals to “Think about the time you typically spent being physically active in the last 7 days PRIOR TO TODAY.” Since the survey was completed between April 10 and May 25, 2020, which covers the first 1–2 months after most U.S. states issued “Shelter-in-place” or “Stay-in-home” orders, this second IPAQ administration represented the early-CVOID-19 period. During both times, participants reported on levels of vigorous intensity activity, moderate intensity activity, and walking activity. For all three types of physical activity, individuals reported the number of days per week that they performed the targeted activity for at least 10 min at a time. They then reported how much time they usually spent on one of those days doing the targeted physical activity. Data were cleaned following the IPAQ scoring protocol (Forde, 2020). Duration values were censored to a maximum of 180 min per day to reduce the effect of possibly spurious outliers.
Device-based physical activity. Stepping behavior for the past 12 months was retrospectively captured using the built-in accelerometer from participants’ personal smartphones. Modern smartphones include a three-axis gyroscope and accelerometer that capture body movements. The iOS (Apple, Inc) operating system comes with default accelerometer application that continuously counts steps taken by the user. Information about the underlying algorithm used by each application to count steps was not available. Previous studies have demonstrated that smartphones are valid tools for step counting in different age groups and across a range of walking and running conditions (Höchsmann et al., 2018). At the end of the online survey, iOS users were asked to upload a screenshot of the automatically generated bar graph of their past year steps-by-month from their Apple Health app. Compatible steps data were not available from users of Android smartphones. To extract these data, research staff uploaded screenshots to WebPlotDigitizer (WebPlotDigitizer, 2020) where the length of Y axis on the bar graph was measured and calibrated. Average steps by month was calculated rounded to the nearest whole number based on the length of the bar and were exported. Screenshots were excluded from extraction if an incorrect screenshot was uploaded (i.e. average miles by month) (n = 21) or the quality of the screenshot was too poor to extract (n = 6). The pre- and early-COVID-19 periods were represented by step count data extracted from Feb 2020 and April 2020, respectively.
Physical activity locations. Participants were asked whether they were currently physically active for at least 30 min per week. If so, they were asked to indicate where (i.e., the types of locations in which) they did physical activity over the past 7 days, with instructions to choose all that apply from the following options: inside my home or garage, in my yard or driveway, on the sidewalks and roads in my neighborhood, on the sidewalks and roads outside my neighborhood, gym or fitness center, at a park or trail, and at an outdoor sports facility (e.g., basketball/tennis court, baseball diamond).
Demographics. Participants self-reported their biological sex at birth (male vs. female), age (later categorized as 18–39 years, 40–59 years, and 60 + years), race, ethnicity (Hispanic/Latino vs. non-Hispanic/Latino), education level, and annual household income (later categorized as less than $27,000, $27,000–$59,999, $60,000–$99,999, $100,000 or more). Participants also reported their height (inches) and weight (pounds). Height was converted to meters, and weight was converted to kilograms. Body mass index (BMI; kg/m2) was calculated, and weight status categories were created (underweight is 18.5 kg/m2, normal weight is ≥18.5 kg/m2 and <25 kg/m2, overweight is ≥25 kg/m2 and <30, obese is ≥30 kg/m2).
2.5. Statistical analyses
Prior to data analyses, variables were screened for violations of statistical assumptions (e.g., normality, linearity). All four physical activity variables (i.e., vigorous intensity, moderate intensity, walking, and step counts) were positively skewed and thus subjected to cube root transformations. A preliminary set of paired t-tests examined within-subject effects of time (pre-COVID-19 vs. early-COVID-19]) on vigorous intensity, moderate intensity, walking, and step counts. Mixed model repeated-measures analysis of variance (ANOVA) procedure examined the between-subject effects of self-reported ethnicity and annual household income on the within-subject difference in physical activity the two time points (i.e., Time [WS] × Ethnicity [BS] and Time [WS] × Income [BS] after controlling for the main effects and interactions with time for age, sex, and weight status. These confounders were selected due to population-based evidence in adults showing that physical activity declines with age, is lower among women, and inversely associated with adiposity (Hawkins et al., 2009, Wanner et al., 2016). To examine whether the likelihood of engaging in physical activity at the various locations also differed by self-reported ethnicity, logistic regressions were conducted with ethnicity and the covariates entered simultaneously and each location (yes vs. no) as the dependent variables in separate models controlling for the covariates listed above. Lastly, multiple linear regression analyses tested the associations of performing physical activity in various locations (e.g., home/garage, driveway/yard, roads in one’s neighborhood) (yes vs. no) with vigorous intensity, moderate intensity, walking, and step counts during the early-COVID-19 period after adjusting for the covariates listed above.
Post-hoc statistical power analyses using G*Power (Faul et al., 2007) indicated that analytic sample sizes of 250 (i.e., relevant to the full analytic sample) and 136 (i.e., relevant to the subsample with smartphone accelerometer data) are able to detect small effect sizes (η2 = 0.011–0.015) and (η2 = 0.020–0.029), respectively, with β = 0.80, α = 0.05, and correlation among measures of r = 0.3 in a repeated measures ANOVA testing a BS × WS interaction with two to four groups (BS) (i.e., Hispanic/Latino vs. non-Hispanic/Latino, annual household income categories) and two repeated measures (WS) (i.e., pre-COVID-19 vs. early-COVID-19). In multiple linear regression analyses, sample sizes of 248 (i.e., relevant to the full analytic dataset) and 140 (i.e., relevant to the subsample with smartphone accelerometer data) are able to detect small effect sizes (f2 = 0.032) and (f 2 = 0.057), respectively, with β = 0.80, α = 0.05, and up to 11 predictor variables in the model.
3. Results
3.1. Data availability and demographic characteristics
A total of 530 individuals expressed interest in the study and completed the screening questions. Of this number, a total of 496 individuals were eligible after completing the screener, and 430 individuals consented for the study. Cases were removed that had not yet started (n = 19) or not yet completed the survey (n = 80) at the time of data analysis. Of the n = 331 remaining, 63 cases with missing data on one or more of the demographic covariates were removed, leaving an analytic sample size of 268. Table 1 shows the descriptive statistics for the demographic characteristics of the analytic sample. Approximately 58% of participants resided in California, but the sample included residents of 31 U.S. states and the District of Columbia. Participants ranged in age from 18 to 74 years old with an average age of 33.96 (SD = 12.2) years. A majority of participants were younger and female. Approximately 22% of the sample identified as Hispanic/Latino, which is somewhat higher than the rate in the general U.S. population (18.5%) according to recent census data (Bergman et al., 2017). Smartphone-recorded daily step counts were available for a subsample of n = 143 individuals. Chi-square tests showed that the subsample with available step count data was younger (p < .001) than the excluded sample without smartphone step count data.
Table 1.
Descriptive Statistics for Sample on Demographic Characteristics.
| Variable | n (%) |
|---|---|
| Age Group | |
| 18–39 years | 207 (77.2) |
| 40–59 years | 46 (17.2) |
| ≥60 years | 15 (5.6) |
| Sex | |
| Male | 52 (19.5) |
| Female | 215 (80.5) |
| Ethnicity | |
| Hispanic/Latino | 58 (21.6) |
| Non-Hispanic/Latino | 210 (78.4) |
| Race | |
| White/Caucasian | 182 (67.9) |
| Black/African-American | 9 (3.4) |
| Asian | 34 (12.7) |
| Other/Don’t know/Prefer not to answer | 25 (9.3) |
| Mixed | 18 (6.7) |
| Annual Household Income | |
| Less than $27,000 | 36 (13.4) |
| $27,000–$59,999 | 70 (26.1) |
| $60,000–$99,999 | 48 (17.9) |
| $100,000 or more | 114 (42.5) |
| Education | |
| High school graduate | 6 (2.2) |
| Some college | 20 (7.5) |
| College graduate | 102 (38.1) |
| Some graduate school | 140 (52.2) |
| Weight Categories | |
| Underweight | 7 (2.6) |
| Normal weight | 143 (53.4) |
| Overweight | 79 (29.5) |
| Obese | 39 (14.6) |
N = 268.
3.2. Change in physical activity from the Pre- to Early-COVID-19 periods
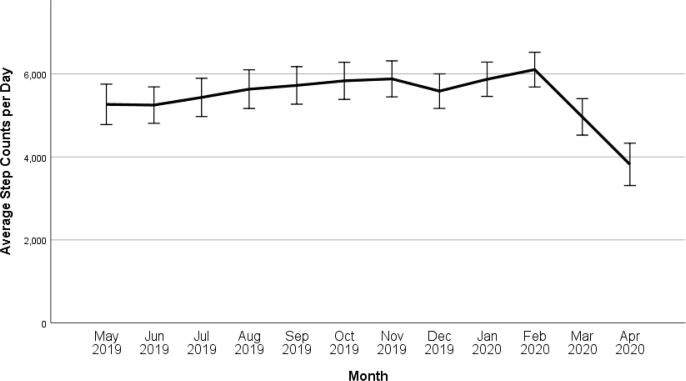
Descriptive statistics for vigorous, moderate, and walking physical activity per week as well as steps per day for the pre-COVID-19 (February 2020) and early-COVID-19 (April-May 2020) periods are shown in Table 2. Unadjusted paired t-tests indicated significant reductions in vigorous intensity, Mdiff = −66.9 min/week (35.1% decrease), t(267) = 6.30, p < .001, moderate intensity, Mdiff = −92.4 min/week (45.7% decrease), t(263) = 6.30, p < .001, walking, Mdiff = −70.8 min/week (20.7% decrease), t(264) = 4.62, p < .001, and steps, Mdiff = –2232.4 steps/day (36.3% decrease), t(142) = 10.02, p < .001 during the early-COVID 19 period as compared to the pre-COVID-19 period. Available past 12-month smartphone-based step count data show that average daily steps remained steady between May 2019 and February 2020, with an observed decrease of about 2,000 steps per day across March and April 2020 (See Fig. 1).
Table 2.
Descriptive Statistics for Self-reported and Device-based Physical Activity Variables.
| Pre-COVID-19 (Feb. 2020) |
Early-COVID-19(April-May 2020) |
|||||
|---|---|---|---|---|---|---|
| n | Mean (SD) | Median | n | Mean (SD) | Median | |
| Vigorous (min/week) | 268 | 190.7 (211.2) | 120.0 | 268 | 123.9 (171.4) | 60.0 |
| Moderate (min/week) | 265 | 202.4 (271.9) | 120.0 | 266 | 111.0 (172.5) | 60.0 |
| Walking (min/week) | 266 | 341.9 (339.8) | 210.0 | 267 | 244.1 (280.8) | 140.0 |
| Steps (counts/day) | 149 | 6153.2 (2805.9) | 5998.0 | 143 | 3920.8 (3344.5) | 3058.0 |
Self-reported minutes of vigorous, moderate, and walking physical activity per week were assessed by the short-form International Physical Activity Questionnaire (IPAQ). Device-based step counts per day were assessed by the on-board accelerometer in participants’ personal smartphones. Median values are presented due to positive skew.
Fig. 1.
Average steps (counts/day) for the past 12 months (May 2019-April 2020) with 95% confidence intervals for study participants. Step data extracted from personal smartphone accelerometer tracking app on iOS and Android.
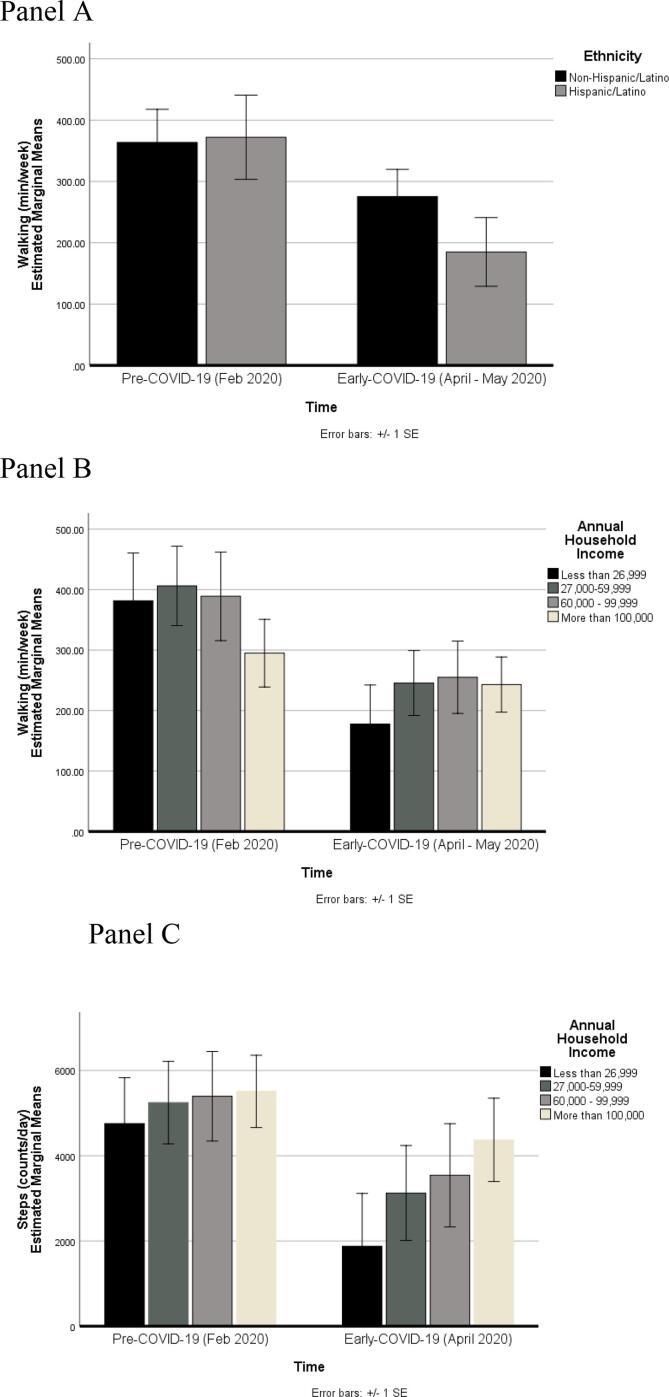
Results for the models examining changes in physical activity between the pre-COVID-19 and early-COVID-19 periods by self-reported ethnicity and annual household income are shown in Table 3. After controlling for the covariates in the model, changes in reported vigorous and moderate intensity physical activity did not differ by ethnicity or annual household income (See Table 3). However, there were significant Time (WS) × Ethnicity (BS) and Time (WS) × Income (BS) interactions for walking, indicating that the size of the change in minutes of walking physical activity per week differed by ethnicity (Hispanic/Latino vs. non-Hispanic/Latino) and annual household income. Fig. 2 (Panel A) shows that Hispanic adults reported a greater decrease in walking physical activity minutes per week as compared to non-Hispanic adults. Also, adults with annual household incomes between $27,00–$59,999 reported a greater decrease in walking physical activity minutes per week as compared to adults with annual household incomes greater than or equal to $100,000 (see Fig. 2, Panel B). The significant Time (WS) × Income (BS) interaction for step counts per day in Table 3 shows that after controlling for the effects of the covariates in the model, changes in recorded steps per day between the pre-COVID-19 and early-COVID-19 periods differed by annual household income. Adults with annual household incomes between $27,000–$59,999 showed a greater decrease in steps per day as compared to adults with annual household incomes greater than or equal to $100,000 (see Fig. 2, Panel C).
Table 3.
Mixed Model Repeated-Measures Analysis of Variance (ANOVA) Examining the Effects of Time (pre-COVID-19 [Feb. 2020] vs. early-COVID-19 [April-May 2020]) on Self-reported and Device-based Physical Activity by Ethnicity and Income.
| Variable | Vigorous (min/week) |
Moderate (min/week) |
Walking (min/week) |
Steps (counts/day) |
||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| df | F | p | η2 | df | F | p | η2 | df | F | p | η2 | df | F | p | η2 | |
| Time (WS) | 1259 | 10.602 | 0.001 | 0.040 | 1255 | 16.686 | 0.000 | 0.062 | 1266 | 9.247 | 0.003 | 0.035 | 1132 | 5.716 | 0.018 | 0.042 |
| Hispanic (BS) | 1259 | 1.410 | 0.236 | 0.005 | 1255 | 0.109 | 0.742 | 0.000 | 1266 | 3.655 | 0.057 | 0.014 | 1132 | 1.291 | 0.258 | 0.010 |
| Income (BS) | 3259 | 2.335 | 0.074 | 0.027 | 3255 | 0.631 | 0.596 | 0.007 | 3266 | 0.844 | 0.471 | 0.010 | 3132 | 3.017 | 0.032 | 0.064 |
| Time (WS) × Hispanic (BS) | 1259 | 1.071 | 0.302 | 0.004 | 1255 | 0.694 | 0.405 | 0.003 | 1266 | 4.289 | 0.039 | 0.017 | 1132 | 0.129 | 0.720 | 0.001 |
| Time (WS) × Income (BS) | 3259 | 0.617 | 0.604 | 0.007 | 3255 | 1.203 | 0.309 | 0.014 | 3266 | 2.935 | 0.034 | 0.034 | 3132 | 3.075 | 0.030 | 0.065 |
n = 268 for vigorous, n = 264 for moderate, n = 265 for walking, and n = 143 for steps. η2 = effect size (partial eta squared). WS = within-subject effect. BS = between-subject effect. Self-reported minutes of vigorous, moderate, and walking physical activity per week were assessed by the short-form International Physical Activity Questionnaire (IPAQ). Device-based step counts per day were assessed by the on-board accelerometer in participants’ personal smartphones. Vigorous, moderate, walking, and steps were cube root transformed to adjust for positive skew. Hispanic/Latino (vs. non-Hispanic/Latino), and annual household income ($12,500–$26,999, $27,000–$59,999, $60,000–$99,999, more than $100,000). All models adjust for the main effects and interactions of age (18–39 years, 40–59 years, and 60+ years), sex (male vs/ female), and weight status (underweight is <18.5 kg/m2, normal weight is ≥18.5 kg/m2 and <25 kg/m2, overweight is ≥25 kg/m2 and <30, obese is ≥30 kg/m2) with Time.
Fig. 2.
Panel A: Effects of time (pre-COVID-19 [Feb. 2020] vs. early-COVID-19 [April-May 2020]) on minutes of walking physical activity per week by ethnicity (Hispanic/Latino n = 57, non-Hispanic/Latino n = 208). Estimated marginal means are presented for raw (untransformed) data adjusting for sex, age, weight status, and annual household income. n = 265. Panel B: Effects of time (pre-COVID-19 [Feb. 2020] vs. early-COVID-19 [April-May 2020]) on minutes of walking per week by annual household income (n = 36 for <$27,000, n = 70 for $27,000–$59,999, n = 48 for $60,000–$99,999, n = 111 for ≥$100,000). Estimated marginal means are presented for raw (untransformed) data adjusting for sex, age, weight status, ethnicity. n = 265. Panel C: Effects of time (pre-COVID-19 [Feb. 2020] vs. early-COVID-19 [April 2020]) on smartphone accelerometer-derived steps per day by annual household income (n = 23 for <$27,000, n = 38 for $27,000–$59,999, n = 23 for $60,000–$99,999, n = 59 for ≥$100,000). Estimated marginal means are presented for raw (untransformed) data adjusting for sex, age, weight status, and ethnicity. n = 143.
3.3. Locations of physical activity during the Early-COVID-19 period
A total of 236 participants indicated that they were currently physically active for at least 30 min per week, and thus provided physical activity location data. During the early-COVID-19 period, the greatest proportion of physical activity was reported at home or in one’s garage (75.0%), followed by on the sidewalks or roads in one’s neighborhood (69.9%), at a park or trail (27.1%), on the sidewalks or roads outside one’s neighborhood (19.9%), in one’s yard or driveway (19.9%), gym or fitness center (5.1%), and outdoor sports facility (1.3%). Demographic differences in the likelihood of engaging in physical activity in the top three locations (i.e., home/garage, in neighborhood, park/trail) were examined. Individuals who had annual household incomes of $27,000–$59,999 (OR = 2.92, 95% CI = [1.13–7.63]), $60,000–$99,999 (OR = 2.79, 95% CI = [1.01, 7.71]), or more than $100,000 (OR = 5.47, 95% CI = [2.11, −14.18]) than were more likely to engage in physical activity on sidewalks and roads in their neighborhoods than individuals whose annual household incomes were less than $27,000, after adjusting for age, sex, weight status, and ethnicity. Neither ethnicity nor annual household income were associated with the likelihood of engaging in physical activity at home/in garage or on at a park/trail.
Results of the analyses examining associations of vigorous, moderate, walking, and step counts during the early-COVID-19 period with various locations that physical activity had been performed are shown in Table 4. Performing physical activity in one’s home/garage or driveway/yard was associated with more vigorous and moderate intensity physical activity after adjusting for age, sex, weight status, ethnicity, and income. Also, a greater number of steps per day during the early-COVID-19 period was recorded for individuals who performed physical activity on the roads in their neighborhood and at parks/trails. None of the measured locations of physical activity were associated with walking physical activity.
Table 4.
Multiple Linear Regression Analysis for Self-reported and Device-based Physical Activity During the early-COVID-19 (April-May 2020) Period as a Function of Past 7-day Physical Activity Locations.
| Physical Activity Location | Vigorous (min/week) |
Moderate (min/week) |
Walking (min/week) |
Steps (counts/day) |
||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| β | SE | p | ΔR2 | β | SE | p | ΔR2 | β | SE | p | ΔR2 | β | SE | p | ΔR2 | |
| Home/Garage | 1.579 | 0.436 | <0.001 | 0.056 | 1.333 | 0.410 | 0.001 | 0.040 | 0.079 | 0.382 | 0.836 | <0.001 | −0.374 | 0.934 | 0.689 | 0.011 |
| Driveway/Yard | 1.136 | 0.464 | 0.015 | 0.025 | 1.201 | 0.440 | 0.007 | 0.029 | 0.124 | 0.410 | 0.763 | <0.001 | 1.142 | 0.924 | 0.219 | 0.006 |
| Roads in Neighborhood | −0.203 | 0.409 | 0.619 | <0.001 | 0.102 | 0.387 | 0.793 | 0.001 | 0.508 | 0.361 | 0.161 | 0.010 | 2.081 | 0.804 | 0.011 | 0.062 |
| Roads outside Neighborhood | 0.875 | 0.467 | 0.063 | 0.017 | 0.296 | 0.445 | 0.507 | 0.030 | 0.472 | 0.410 | 0.250 | 0.008 | 1.207 | 0.947 | 0.205 | 0.028 |
| Gym/Fitness Center | −0.004 | 0.847 | 0.996 | <0.001 | 1.081 | 0.797 | 0.177 | 0.008 | −0.405 | 0.743 | 0.587 | 0.001 | 1.955 | 1.755 | 0.268 | 0.010 |
| Park/Trail | 0.315 | 0.420 | 0.454 | 0.002 | 0.301 | 0.396 | 0.448 | 0.002 | 0.336 | 0.369 | 0.363 | 0.003 | 1.781 | 0.846 | 0.038 | 0.029 |
n = 235 for vigorous, n = 233 for moderate, n = 234 for walking, and n = 124 for steps. SE = standard error. ΔR2 = change in r-squared value. Self-reported minutes of vigorous, moderate, and walking physical activity per week were assessed by the short-form International Physical Activity Questionnaire (IPAQ). Device-based step counts per day were assessed by the on-board accelerometer in participants’ personal smartphones. Vigorous, moderate, walking, and steps were cube root transformed to adjust for positive skew. Physical activity locations (i.e., where physical activity occurred in past 7 days) coded 1 = yes and 0 = no. Participants who reported less 30 min physical activity per week did not receive past 7-day physical activity questions (n = 32). All models adjust for age (18–39 years, 40–59 years, and 60+ years), sex (male vs. female), weight status (underweight is <18.5 kg/m2, normal weight is ≥18.5 kg/m2 and <25 kg/m2, overweight is ≥25 kg/m2 and <30, obese is ≥30 kg/m2), ethnicity (Hispanic/Latino vs. non-Hispanic/Latino), and annual household income ($12,500–$26,999, $27,000–$59,999, $60,000–$99,999, more than $100,000).
4. Discussion
This study examined the early effects of the COVID-19 pandemic on physical activity locations and behavior among adults living in the U.S. Overall, physical activity levels declined during the early-COVID-19 period. Observed changes for self-reported physical activity ranged from a 21% decrease for walking to an almost 46% decrease for moderate intensity. These values are similar in size to percent changes in the range of 32%–48% found for overall physical activity on recent self-report surveys of U.S. adults for the late March to early April period (Meyer et al., 2020). Previous data from wearable activity tracking devices collected during the same time frame have found smaller decreases in physical activity levels ranging from 7% to 12% (Fitbit, 2020, Withings, 2020). Data from European countries such as France and Switzerland suggest similar trends with declines in vigorous physical activity and commuting-based physical activity during the same time frame (Cheval et al., 2020).
The positive association between performing physical activity at a home location and higher levels of moderate/vigorous activity suggests that individuals may attempt to replace closed gyms and fitness centers with online/streaming fitness classes or available equipment at home. Results showing that step counts are positively associated with walking in one’s neighborhood and parks, suggests that neighborhood- or park-based walking may be a viable option for maintaining physical activity over the course of an extended pandemic.
Results suggest that decreases in self-reported walking and device-based step counts were larger for individuals from lower-income households. Additionally, adults identifying as Hispanic/Latino demonstrated larger decreases in walking during this period. COVID-19-based restrictions and closures may have eliminated of transport- and occupational-based walking among members of these groups who previously traveled to work by walking or public transportation, or who previously engaged in walking while at work due to the nature of their job position. Location data during the early-COVID-19 period indicate that individuals from lower income households were less likely to report engaging in physical activity on the sidewalks and roads in their neighborhood. Streets in lower income neighborhoods may have poorer sidewalk availability and quality, greater traffic volume, or higher crime, which can deter leisure walking (Silfee et al., 2016). Findings observed here suggest that disparate impacts of the COVID-19 pandemic on lower income and ethnic minority groups reach beyond viral exposures and mortality (Garg, 2020), and extend into health-related behaviors that may have long-lasting consequences for other chronic diseases.
Strengths of the study included the timeliness of the survey during the early-COVID-19 period (April–May 2020), the collection of retrospective data to capture the period prior to the pandemic, and the use of standardized self-report and device-based physical activity measures. However, there were some limitations. The use of a retrospective self-report measures to assess pre-COVID-19 levels of vigorous, moderate, and walking physical activity could have introduced various reporting errors and biases. Also, individuals may not carry their smartphones with them at all times, leading to potential underestimation of physical activity through the device-based measure. Furthermore, this study did not use an objective GPS-based measure of environmental contexts of physical activity, which would enhance the reliability and validity. Additionally, the sample largely consisted of younger adults who were female, college graduates, and came from from middle-to-higher income households. Thus, findings may be not generalizable to a representative sample of U.S. adults.
5. Conclusions
In summary, we observed a decline in adults’ physical activity during the first two months of the COVID-19 pandemic based on retrospective self-report and device-based measures. Although “Shelter-in-Place” and “Stay-at-Home” orders issued by states were necessary in order to slow the spread of the virus and allow healthcare facilities to build capacity, there may be unintended consequences on other health-related behaviors such as physical activity. Disparate impacts of the COVID-19 pandemic on the physical activity levels of potentially vulnerable sub-groups, including individuals who are low income or Hispanic/Latino, underscore the need for population-specific physical activity programs and policies over the next several months to years as the pandemic continues.
Funding source
This study was funded in part by National Institutes of Health grants R01HL119255 and U01HL146327.
CRediT authorship contribution statement
Genevieve F. Dunton: Conceptualization, Formal analysis, Funding acquisition, Investigation, Methodology, Writing - original draft, Writing - review & editing. Shirlene D. Wang: Conceptualization, Data curation, Methodology, Project administration, Writing - review & editing. Bridgette Do: Conceptualization, Data curation, Investigation, Methodology, Project administration, Writing - review & editing. Jimikaye Courtney: Conceptualization, Data curation, Investigation, Methodology, Writing - review & editing.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgements
This study was funded by National Institutes of Health grants R01HL119255 and U01HL146327. We would like to thank Amy Nguyen for her assistance with participant recruitment and data collection. We would also like to thank Kayla Nuss for helping design the baseline physical activity survey.
References
- Meyer J, McDowell, C., Lansing, J., Brower, C., Smith, L., Tully, M., & Herring, M. Changes in physical activity and sedentary behaviour due to the COVID-19 outbreak and associations with mental health in 3,052 US adults. Cambridge Open Engage, 2020. doi: 10.33774/coe-2020-h0b8g[published Online First: Epub Date]|.
- Forde C. Scoring the International Physical Activity Questionnaire (IPAQ). Secondary Scoring the International Physical Activity Questionnaire (IPAQ) Trinity College Dubliin. 2020 https://ugc.futurelearn.com/uploads/files/bc/c5/bcc53b14-ec1e-4d90-88e3-1568682f32ae/IPAQ_PDF.pdf [Google Scholar]
- Garg, S, 2020. Hospitalization rates and characteristics of patients hospitalized with laboratory-confirmed coronavirus disease 2019—COVID-NET, 14 States, March 1–30, 2020.. Morbidity and mortality weekly report, 69. [DOI] [PMC free article] [PubMed]
- Halabchi F., Ahmadinejad Z., Selk-Ghaffari M. COVID-19 epidemic: exercise or not to exercise; that is the question! Asian. J. Sports Med. 2020 [Google Scholar]
- Bélisle M., Roskies E., Lévesque J.-M. Improving adherence to physical activity. Health Psychol. 1987;6(2):159. doi: 10.1037//0278-6133.6.2.159. [DOI] [PubMed] [Google Scholar]
- Bauman A., Ainsworth B.E., Bull F. Progress and pitfalls in the use of the International Physical Activity Questionnaire (IPAQ) for adult physical activity surveillance. J. Phys. Activity Health. 2009;6(s1):S5–S8. doi: 10.1123/jpah.6.s1.s5. [DOI] [PubMed] [Google Scholar]
- Brown W., Trost S., Bauman A., Mummery K., Owen N. Test-retest reliability of four physical activity measures used in population surveys. J. Sci. Med. Sport. 2004;7(2):205–215. doi: 10.1016/s1440-2440(04)80010-0. [DOI] [PubMed] [Google Scholar]
- Ekelund U., Sepp H., Brage S. Criterion-related validity of the last 7-day, short form of the International Physical Activity Questionnaire in Swedish adults. Public Health Nutr. 2006;9(2):258–265. doi: 10.1079/phn2005840. [DOI] [PubMed] [Google Scholar]
- Höchsmann C., Knaier R., Eymann J., Hintermann J., Infanger D., Schmidt-Trucksäss A. Validity of activity trackers, smartphones, and phone applications to measure steps in various walking conditions. Scand. J. Med. Sci. Sports. 2018;28(7):1818–1827. doi: 10.1111/sms.13074. [DOI] [PubMed] [Google Scholar]
- Hawkins M.S., Storti K.L., Richardson C.R. Objectively measured physical activity of USA adults by sex, age, and racial/ethnic groups: a cross-sectional study. Int. J. Behav. Nutr. Phys. Activity. 2009;6(1):1–7. doi: 10.1186/1479-5868-6-31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wanner M., Martin B.W., Autenrieth C.S. Associations between domains of physical activity, sitting time, and different measures of overweight and obesity. Prev. Med. Rep. 2016;3:177–184. doi: 10.1016/j.pmedr.2016.01.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Faul F., Erdfelder E., Lang A.-G., Buchner A. G* Power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav. Res. Methods. 2007;39(2):175–191. doi: 10.3758/bf03193146. [DOI] [PubMed] [Google Scholar]
- Bergman, K., Sarkar, P., O'Connor, T.G., Modi, N., Glover, V., 2007. Maternal stress during pregnancy predicts cognitive ability and fearfulness in infancy. J. Am. Acad. Child Adolescent Psychiatry 46(11), 1454–1463 doi: 10.1097/chi.0b013e31814a62f6[published Online First: Epub Date]|. [DOI] [PubMed]
- Cheval, B., Sivaramakrishnan, H., Maltagliati, S., et al., 2020. Relationships Between Changes in Self-reported Physical Activity and Sedentary Behaviours and Health During the Coronavirus (COVID-19) Pandemic in France and Switzerland. [DOI] [PubMed]
- https://automeris.io/WebPlotDigitizer. (Accessed 16 Nov 2020).
- Silfee V.J., Rosal M.C., Sreedhara M., Lora V., Lemon S.C. Neighborhood environment correlates of physical activity and sedentary behavior among Latino adults in Massachusetts. BMC public health. 2016;16(1):966. doi: 10.1186/s12889-016-3650-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- https://www.cdc.gov/coronavirus/2019-ncov/cases-updates/summary.html. 2020. (Accessed 16 November 2020).
- https://blog.withings.com/2020/05/01/data-quarantine-isnt-making-us-gain-weight-or-slow-down/. 2020. (Accessed 16 November 2020).
- https://blog.fitbit.com/covid-19-global-activity/. 2020. (Accessed 16 November 2020).
- https://www.natlawreview.com/article/covid-19-us-state-policy-report-october-27-november-2-2020. 2020. (Accessed 16 November 2020).
- https://www.ihrsa.org/about/media-center/press-releases/latest-data-shows-u-s-health-club-industry-serves-70-2-million/. 2018. (Accessed 16 November 2020).
- https://evidation.com/news/covid-19-pulse-first-data-evidation. 2020. (Accessed 16 November 2020).
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
A total of 530 individuals expressed interest in the study and completed the screening questions. Of this number, a total of 496 individuals were eligible after completing the screener, and 430 individuals consented for the study. Cases were removed that had not yet started (n = 19) or not yet completed the survey (n = 80) at the time of data analysis. Of the n = 331 remaining, 63 cases with missing data on one or more of the demographic covariates were removed, leaving an analytic sample size of 268. Table 1 shows the descriptive statistics for the demographic characteristics of the analytic sample. Approximately 58% of participants resided in California, but the sample included residents of 31 U.S. states and the District of Columbia. Participants ranged in age from 18 to 74 years old with an average age of 33.96 (SD = 12.2) years. A majority of participants were younger and female. Approximately 22% of the sample identified as Hispanic/Latino, which is somewhat higher than the rate in the general U.S. population (18.5%) according to recent census data (Bergman et al., 2017). Smartphone-recorded daily step counts were available for a subsample of n = 143 individuals. Chi-square tests showed that the subsample with available step count data was younger (p < .001) than the excluded sample without smartphone step count data.
Table 1.
Descriptive Statistics for Sample on Demographic Characteristics.
| Variable | n (%) |
|---|---|
| Age Group | |
| 18–39 years | 207 (77.2) |
| 40–59 years | 46 (17.2) |
| ≥60 years | 15 (5.6) |
| Sex | |
| Male | 52 (19.5) |
| Female | 215 (80.5) |
| Ethnicity | |
| Hispanic/Latino | 58 (21.6) |
| Non-Hispanic/Latino | 210 (78.4) |
| Race | |
| White/Caucasian | 182 (67.9) |
| Black/African-American | 9 (3.4) |
| Asian | 34 (12.7) |
| Other/Don’t know/Prefer not to answer | 25 (9.3) |
| Mixed | 18 (6.7) |
| Annual Household Income | |
| Less than $27,000 | 36 (13.4) |
| $27,000–$59,999 | 70 (26.1) |
| $60,000–$99,999 | 48 (17.9) |
| $100,000 or more | 114 (42.5) |
| Education | |
| High school graduate | 6 (2.2) |
| Some college | 20 (7.5) |
| College graduate | 102 (38.1) |
| Some graduate school | 140 (52.2) |
| Weight Categories | |
| Underweight | 7 (2.6) |
| Normal weight | 143 (53.4) |
| Overweight | 79 (29.5) |
| Obese | 39 (14.6) |
N = 268.