Abstract
Objective
Prior data suggest Emergency Department (ED) visits for many emergency conditions decreased during the initial COVID-19 surge. However, the pandemic's impact on the wide range of conditions seen in EDs, and the resources required for treating them, has been less studied. We sought to provide a comprehensive analysis of ED visits and associated resource utilization during the initial COVID-19 surge.
Methods
We performed a retrospective analysis from 5 hospitals in a large health system in Massachusetts, comparing ED encounters from 3/1/2020–4/30/2020 to identical weeks from the prior year. Data collected included demographics, ESI, diagnosis, consultations ordered, bedside procedures, and inpatient procedures within 48 h. We compared raw frequencies between time periods and calculated incidence rate ratios.
Results
ED volumes decreased by 30.9% in 2020 compared to 2019. Average acuity of ED presentations increased, while most non-COVID-19 diagnoses decreased. The number and incidence rate of all non-critical care ED procedures decreased, while the occurrence of intubations and central lines increased. Most subspecialty consultations decreased, including to psychiatry, trauma surgery, and cardiology. Most non-elective procedures related to ED encounters also decreased, including craniotomies and appendectomies.
Conclusion
Our health system experienced decreases in nearly all non-COVID-19 conditions presenting to EDs during the initial phase of the pandemic, including those requiring specialty consultation and urgent inpatient procedures. Findings have implications for both public health and health system planning.
1. Introduction
The COVID-19 pandemic has created numerous challenges for the United States health system. Among them was an initial surge of COVID-19 patients that overwhelmed emergency departments (EDs) in certain large cities, which garnered extensive media attention [1]. This was followed by widespread restrictions of public gatherings and mandated social distancing in many states. These measures appeared to slow the rate of new COVID-19 cases and helped to prevent further overcrowding of EDs and the overwhelming of other healthcare resources [2].
Simultaneously, concerns grew about patients delaying or altogether foregoing emergency medical care in this environment. An American College of Emergency Physicians (ACEP) survey conducted in April 2020 reported that 80% of patients had fears of contracting COVID-19 during a hypothetical visit to an ED, and 73% were concerned about placing unnecessary burden on the health system [3]. Nearly 60% of respondents also expressed concerns about not being able to have a visitor or guest present during their care in the ED. A number of studies have indeed shown decreased ED visits in the U.S. and other parts of the world during the COVID-19 surge, including reduced presentations of acute coronary syndromes and strokes [[4], [5], [6], [7], [8], [9], [10], [11]]. An additional study found evidence of increased rates of out-of-hospital cardiac arrests, likely due to delays in care [12].
While it is now understood that the initial surge in COVID-19 cases led to decreases in ED visits for most non-COVID-19 diseases, there has been less characterization of the impact of this decrease on ED physician activities and the utilization of ED and hospital resources. We therefore sought to analyze how COVID-19 impacted the overall pattern of ED presentations within our large health system, and how this affected rates of procedures performed both in the ED and during hospitalization, as well as the utilization of resources such as subspecialty consultations.
2. Methods
2.1. Study setting
This was an observational retrospective study of all ED patients from five hospitals in our health system in Eastern Massachusetts with a total annual ED visit volume of 340,000. The examined population included both children and adults in order to characterize the full range of ED visits. Two of the included hospitals are urban academic medical centers, which are both quaternary-care referral hospitals with level one trauma center, STEMI center, and comprehensive stroke center designations. The other three included hospitals are community hospitals; one is a level-three trauma center, STEMI center, and stroke center, while the other two are stroke centers.
2.2. Study design
We extracted data from our integrated electronic health record (EHR), which includes Epic, Verona, and WI, on all visits to the five hospitals within our health system between two comparative periods, an “early pandemic” period between March 1, 2020 to April 30, 2020, and a “baseline” period of the same weeks in the prior calendar year. Data was extracted using Structured Query Language (SQL) queries of the SQL data warehouse of our EHR, and no manual chart abstraction was performed. There was only manual review of several charts to confirm that each variable extracted accurately. For demographic data, we accounted for missing data differently for race, ethnic group, and language preference. If the patient's race was missing, we considered those data as null. For ethnic group we imputed missing data to “non-Hispanic,” and similarly for language preference we imputed missing data to “English-speaking,” as we found that these demographic fields were often documented by exception by the registration staff.
The first case of COVID-19 thought to be the result of community spread in Massachusetts occurred on March 2nd, 2020. Cases increased thereafter, and an executive order mandating social distancing and the closure of non-essential businesses occurred on March 15 [13]. The volume of COVID-19 patients admitted to hospitals in our health system peaked in late April and had begun to decrease by April 30. March and April therefore accurately encompassed the period of the COVID-19 surge in our state. March 1, 2019 to April 30, 2019 was selected as the “baseline” comparison period to control for any seasonal variability in ED volumes.
This study was reviewed and deemed exempt by our Institutional Review Board.
2.3. Variables
For each ED encounter during the early pandemic and baseline period, we captured basic demographics, Emergency Severity Index (ESI), primary ED diagnosis, bedside procedures performed, subspecialty consults requested, and related procedures that occurred during the hospital stay after ED admission. ESI is not utilized in one of the academic centers and is therefore not recorded for that hospital. We also extracted the number of patients who tested positive for COVID-19 within the ED during the early pandemic period. Of note, this COVID-19 testing was conducted with Real Time PCR assays conducted in our own hospital's microbiology lab. The International Classification of Diseases, Tenth Edition (ICD-10) code of the primary ED diagnosis was mapped using Clinical Classifications Software Refined (CCSR) v2020.3, a software tool provided by the Agency for Healthcare Research and Quality (AHRQ) [14]. The CCSR is a standardized way to separate ICD-10 codes into clinical categories. In cases where one ICD-10 code could map to several clinical categories, the CCSR provides a default category.
Bedside procedures were identified by the presence of a distinct procedure note in the medical record related to the index visit, which is the standard method of documentation by ED providers. Bedside procedures documented within the full ED note or within a consultant's note were not identified. Consults were identified by the presence of a consult note or admission note within the same ED encounter. We identified inpatient procedure cases by extracting completed case records in the EHR that occurred within the same hospital encounter as the ED visit and within 48 h of admission from the ED.
2.4. Statistical analysis
Comparisons between categorical variables were performed using the chi-squared test, and comparisons of continuous variables were performed using an analysis of variance. For bedside procedures, consults, and operative procedures we calculated the percentage difference in the total number of occurrences between the two periods in order to characterize how the total number of each of these changed during the COVID-19 period. We also calculated incidence rate ratios with 95% confidence intervals in order to characterize changes in the proportion of case types seen during the COVID-19 period. Incidence rates were calculated as the number of the outcome of interest divided by the total ED visits in each period, reported as the frequency of the outcome per 100 ED visits. The incidence rate ratio (IRR) was calculated by dividing the incidence rate in the early pandemic period by the incidence rate in the baseline period for each outcome. Statistical analysis was performed in R (version 3.6.3, R Foundation).
3. Results
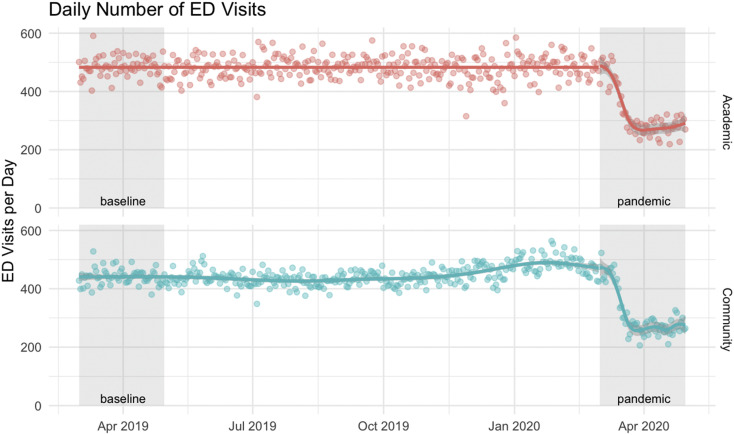
There were 38,966 ED visits across our health system in the “early pandemic” period of March and April of 2020, compared to 56,443 visits in the “baseline” period in 2019, a reduction of 30.9% (Fig. 1 ). During the early pandemic period there were 2585 unique patients that tested positive for COVID-19 in the ED. Overall, the population visiting EDs in the 2020 period was older on average (48.2 years vs. 45.3 years), had a lower percentage of women (50.1% vs. 53.7%), a higher percentage of non-white patients (34.8% vs 32%), and a higher percentage of patients preferring a language other than English (17.9% vs 15.9%) (see Table 1 ). The ED encounters in the early pandemic period had a higher average acuity level: a higher percentage of patients were ESI 1–3 (85.2% vs. 79.2%), a lower percentage of patients were discharged (59.5% vs. 64.5%), and a higher percentage of patients were admitted to the ICU (3.2% vs. 2.3%).
Fig. 1.
Daily number of ED visits over time across the five included hospitals, separated by academic and community hospitals.
Table 1.
Comparison of overall ED visit data between the two time periods
| Baseline n = 56,443 |
Pandemic n = 38,966 |
p | ||
|---|---|---|---|---|
| Age | Mean (SD) | 45.3 (24.8) | 48.2 (22.8) | <0.001 |
| Sex | Female | 30,337 (53.7) | 19,519 (50.1) | <0.001 |
| Male | 26,106 (46.3) | 19,447 (49.9) | ||
| Race | White | 37,412 (68.0) | 24,494 (65.2) | <0.001 |
| Black or African American | 7385 (13.4) | 5464 (14.5) | ||
| Two or more races or Other | 6380 (11.6) | 5135 (13.7) | ||
| Asian | 2186 (4.0) | 1337 (3.6) | ||
| Hispanic or Latino | 1525 (2.8) | 1011 (2.7) | ||
| American Indian or Alaskan Native | 112 (0.2) | 92 (0.2) | ||
| Native Hawaiian or Pacific Islander | 51 (0.1) | 41 (0.1) | ||
| Ethnic Group | Non-Hispanic | 54,855 (97.2) | 37,911 (97.3) | 0.337 |
| Hispanic | 1588 (2.8) | 1055 (2.7) | ||
| Primary Language | English | 47,909 (84.9) | 31,978 (82.1) | <0.001 |
| Other | 8534 (15.1) | 6988 (17.9) | ||
| Hospital Type | Academic | 29,549 (52.4) | 19,841 (50.9) | <0.001 |
| Community | 26,894 (47.6) | 19,125 (49.1) | ||
| ESI | ESI-1 (Immediate) | 539 (1.4) | 466 (1.8) | <0.001 |
| ESI-2 (Emergent) | 11,132 (29.5) | 8072 (31.2) | ||
| ESI-3 (Urgent) | 18,215 (48.3) | 13,497 (52.2) | ||
| ESI-4 (Less Urgent) | 7276 (19.3) | 3578 (13.8) | ||
| ESI-5 (Non-Urgent) | 574 (1.5) | 263 (1.0) | ||
| ED Length of Stay (min) | Mean (SD) | 359.9 (1107.2) | 336.0 (437.6) | <0.001 |
| ED Boarder Time (min) | Mean (SD) | 43.1 (131.7) | 20.8 (73.9) | <0.001 |
| ED Disposition | Discharge | 36,424 (64.5) | 23,179 (59.5) | <0.001 |
| Admit to Floor | 12,731 (22.6) | 10,906 (28.0) | ||
| Place in ED Observation | 3506 (6.2) | 1910 (4.9) | ||
| Admit to ICU | 1308 (2.3) | 1236 (3.2) | ||
| Outside Transfer | 1283 (2.3) | 925 (2.4) | ||
| LWBS, LWCT, AMA, and Other ⁎ | 1022 (1.8) | 691 (1.8) | ||
| Expired | 68 (0.1) | 79 (0.2) | ||
| Send to Labor and Delivery | 101 (0.2) | 40 (0.1) |
LWBS = Left Without Being Seen, LWCT = Left Without Completion of Treatment, AMA = Against Medical Advice.
The primary ED diagnosis mapped to CCSR categories demonstrated significant changes between the two study periods. The incidence rate ratio (IRR) of conditions that mapped to the Certain Infectious and Parasitic Diseases category was 3.16 (2.92–3.42 [95% Confidence Interval]) and Diseases of the Respiratory System was 1.31 (1.26–1.36), while most other disease categories decreased significantly both in incidence rates as well as total numbers (see Table 2 ). The IRR for Factors Influencing Health Status and Contact with Health Statuses was 2.37 (2.19–2.56), primarily because of the diagnoses of “suspected Covid-19 virus infection” (n = 773), “exposure to COVID-19” (n = 93), “encounters related to COVID-19 testing” (n = 20), and “advice given regarding COVID-19” (n = 20).
Table 2.
Comparison of incidence of primary ED diagnosis by CCSR diagnosis categories between periods. N represents the raw number of cases in each period. The difference % compares the raw number of cases between the baseline and early pandemic periods. Incidence is the number of a given case-type per 100 ED encounters. IRR = Incidence Rate Ratio, which is the ratio of incidences between the two periods. Note that the confidence intervals refer only to the IRR, and do not relate to the change in total number of cases in a given category
| CCSR Diagnosis Category | Baseline |
Pandemic |
Comparison |
|||
|---|---|---|---|---|---|---|
| n | Incidence* | n | incidence | difference (%) | IRR (95% CI) | |
| Symptoms, Signs and Abnormal Clinical and Laboratory Findings, Not Elsewhere Classified | 12,246 | 21.70 | 9309 | 23.89 | −24.0 | 1.1 (1.07–1.13) |
| Injury, Poisoning and Certain Other Consequences of External Causes | 7749 | 13.73 | 3854 | 9.89 | −50.3 | 0.72 (0.69–0.75) |
| Diseases of the Circulatory System | 5282 | 9.36 | 3323 | 8.53 | −37.1 | 0.91 (0.87–0.95) |
| Diseases of the Respiratory System | 4950 | 8.77 | 4354 | 11.17 | −12.0 | 1.27 (1.22–1.32) |
| Diseases of the Musculoskeletal System and Connective Tissue | 4100 | 7.26 | 1867 | 4.79 | −54.5 | 0.66 (0.62–0.7) |
| Diseases of the Digestive System | 4020 | 7.12 | 2369 | 6.08 | −41.1 | 0.85 (0.81–0.89) |
| Mental, Behavioral and Neurodevelopmental Disorders | 3892 | 6.90 | 2913 | 7.48 | −25.2 | 1.08 (1.03–1.13) |
| Diseases of the Genitourinary System | 2740 | 4.85 | 1552 | 3.98 | −43.4 | 0.82 (0.77–0.87) |
| Diseases of the Nervous System | 2257 | 4.00 | 1297 | 3.33 | −42.5 | 0.83 (0.78–0.89) |
| Diseases of the Skin and Subcutaneous Tissue | 1469 | 2.60 | 845 | 2.17 | −42.5 | 0.83 (0.76–0.9) |
| Factors Influencing Health Status and Contact with Health Services | 1008 | 1.79 | 1609 | 4.13 | +59.6 | 2.31 (2.14–2.5) |
| Certain Infectious and Parasitic Diseases | 922 | 1.63 | 1944 | 4.99 | +110.8 | 3.05 (2.82–3.3) |
| Endocrine, Nutritional and Metabolic Diseases | 903 | 1.60 | 568 | 1.46 | −37.1 | 0.91 (0.82–1.01) |
| Diseases of the Ear and Mastoid Process | 676 | 1.20 | 212 | 0.54 | −68.6 | 0.45 (0.39–0.53) |
| Neoplasms | 644 | 1.14 | 456 | 1.17 | −29.2 | 1.03 (0.91–1.16) |
| Pregnancy, Childbirth and the Puerperium | 553 | 0.98 | 349 | 0.90 | −36.9 | 0.91 (0.8–1.04) |
| Diseases of the Eye and Adnexa | 508 | 0.90 | 231 | 0.59 | −54.5 | 0.66 (0.56–0.77) |
| Diseases of the Blood and Blood Forming Organs and Certain Disorders Involving the Immune Mechanism | 378 | 0.67 | 344 | 0.88 | −9.0 | 1.32 (1.14–1.53) |
| Certain Conditions Originating in the Perinatal Period | 31 | 0.05 | 17 | 0.04 | −45.2 | 0.79 (0.44–1.43) |
| Congenital Malformations, Deformations and Chromosomal Abnormalities | 31 | 0.05 | 12 | 0.03 | −61.3 | 0.56 (0.29–1.09) |
The total number of most ED bedside procedures decreased in the early pandemic period compared with the baseline period, including every low to mid-acuity procedure. This included laceration repairs (34% decrease), orthopedic injury treatments (44% decrease), and lumbar punctures (46% decrease) (see Table 3 ). Critical care procedures occurred more frequently in the early pandemic period, including endotracheal intubations (118% increase), arterial lines (36% increase), and central lines (45% increase). The IRR of ED patients requiring a critical care procedure also increased, with an IRR of 3.18 (2.66–3.8) for endotracheal intubation.
Table 3.
Comparison of the incidence of ED bedside procedures performed between periods, with comparisons of raw numbers and incidence rate ratios. Occurrence of a procedure was identified by presence of a procedure note within the ED encounter
| ED Bedside Procedure | Baseline |
Pandemic |
Comparison |
|||
|---|---|---|---|---|---|---|
| n | incidence * | n | incidence * | difference (%) | IRR (95% CI) | |
| Laceration Repair | 1263 | 2.24 | 837 | 2.15 | −33.7 | 0.96 (0.88–1.05) |
| Incision and Drainage | 340 | 0.60 | 213 | 0.55 | −37.4 | 0.91 (0.77–1.08) |
| Orthopedic Injury Treatment | 269 | 0.48 | 151 | 0.39 | −43.9 | 0.81 (0.66–0.99) |
| Endotracheal Intubation | 177 | 0.31 | 386 | 0.99 | +118.1 | 3.16 (2.64–3.78) |
| Arterial Line | 111 | 0.20 | 151 | 0.39 | +36.0 | 1.97 (1.54–2.52) |
| Central Line | 98 | 0.17 | 142 | 0.36 | +44.9 | 2.1 (1.62–2.72) |
| Lumbar Puncture | 93 | 0.16 | 50 | 0.13 | −46.2 | 0.78 (0.55–1.1) |
| Foreign Body Removal | 90 | 0.16 | 52 | 0.13 | −42.2 | 0.84 (0.6–1.18) |
| Arthrocentesis | 73 | 0.13 | 31 | 0.08 | −57.5 | 0.62 (0.41–0.94) |
| Nerve Block | 57 | 0.10 | 32 | 0.08 | −43.9 | 0.81 (0.53–1.25) |
| Epistaxis Control | 56 | 0.10 | 34 | 0.09 | −39.3 | 0.88 (0.57–1.35) |
| Ear Cerumen Removal | 54 | 0.10 | 17 | 0.04 | −68.5 | 0.46 (0.27–0.79) |
| Paracentesis | 40 | 0.07 | 27 | 0.07 | −32.5 | 0.98 (0.6–1.6) |
| Gastric Intubation | 38 | 0.07 | 156 | 0.40 | +310.5 | 5.95 (4.17–8.48) |
| Electrical Cardioversion | 19 | 0.03 | 14 | 0.04 | −26.3 | 1.07 (0.54–2.13) |
| Chest Tube | 11 | 0.02 | 13 | 0.03 | +18.2 | 1.71 (0.77–3.82) |
| Intraosseous Line | 11 | 0.02 | 21 | 0.05 | +90.9 | 2.77 (1.34–5.75) |
The total number of consultations ordered for ED patients during the early pandemic period decreased for every subspecialty measured except infectious disease, which increased by 53% (see Table 4 ). Trauma surgery consultations decreased by 19%, psychiatry consultations decreased by 21%, cardiology consultations decreased by 35%, and ENT/Ophthalmology consultations decreased by 51%. The proportional rate of consultations in comparison to total ED volumes remained largely unchanged for most specialties, other than an increase in infectious disease (IRR of 2.29 (2.14–2.45)) and a decrease in ophthalmology/ENT (IRR 0.71 (0.61–0.82)).
Table 4.
Comparison of the incidence of subspecialty consultations from the ED between periods, with comparisons of raw numbers and incidence rate ratios. Occurrence of a consultation was identified by the presence of a consultation note during the index admission from the ED.
| Consulting Service | Baseline |
Pandemic |
Comparison |
|||
|---|---|---|---|---|---|---|
| n | Incidence* | n | incidence | difference (%) | IRR (95% CI) | |
| General Surgery and Subspecialties | 3145 | 5.57 | 2374 | 6.09 | −24.5 | 1.09 (1.03–1.15) |
| Psychiatry | 2433 | 4.31 | 1925 | 4.94 | −20.9 | 1.15 (1.08–1.22) |
| Neurology | 2262 | 4.01 | 1483 | 3.81 | −34.4 | 0.95 (0.89–1.01) |
| Cardiology | 2131 | 3.78 | 1376 | 3.53 | −35.4 | 0.94 (0.88–1.01) |
| Gastroenterology | 1504 | 2.66 | 1065 | 2.73 | −29.2 | 1.03 (0.95–1.11) |
| Orthopedic Surgery | 1470 | 2.60 | 966 | 2.48 | −34.3 | 0.95 (0.88–1.03) |
| Infectious Disease | 1330 | 2.36 | 2037 | 5.23 | +53.2 | 2.22 (2.07–2.38) |
| Neurosurgery | 801 | 1.42 | 551 | 1.41 | −31.2 | 1 (0.9–1.11) |
| Urology | 779 | 1.38 | 530 | 1.36 | −32.0 | 0.99 (0.89–1.11) |
| Obstetrics and Gynecology | 657 | 1.16 | 395 | 1.01 | −39.9 | 0.87 (0.77–0.99) |
| ENT and Ophthalmology | 539 | 0.95 | 265 | 0.68 | −50.8 | 0.71 (0.61–0.82) |
| Trauma Surgery | 288 | 0.51 | 232 | 0.60 | −19.4 | 1.17 (0.98–1.39) |
The total number of every inpatient procedure we measured that was performed on patients admitted from EDs decreased in the early pandemic period compared with the baseline, with the exception of exploratory laparotomy, which increased by 14.3% (see Table 5 ). Cardiac catheterizations decreased by 28%, appendectomies decreased by 21.5%, craniotomies decreased by 29%, and fracture reduction and fixations decreased by 29%. Most of these procedures decreased in proportion to total volume reductions with incidence rate ratios approximating 1.0, with few exceptions.
Table 5.
Comparison of the incidence of inpatient procedures associated with the ED encounter between periods, with comparisons of raw numbers and incidence rate ratios. Inpatient procedures include those performed in the cardiac catheterization lab, endoscopy suite, interventional radiology suite, or the operating room. A procedure was considered associated with an ED encounter if it occurred within 48 h of admission from the ED.
| Inpatient Procedure | Baseline |
Pandemic |
Comparison |
|||
|---|---|---|---|---|---|---|
| n | Incidence* | n | incidence | difference (%) | IRR (95% CI) | |
| Endoscopy | 686 | 1.22 | 367 | 0.94 | −46.5 | 0.77 (0.68–0.87) |
| Fracture Reduction and Fixation | 265 | 0.47 | 188 | 0.48 | −29.1 | 1.03 (0.85–1.24) |
| Appendectomy | 191 | 0.34 | 150 | 0.38 | −21.5 | 1.14 (0.92–1.41) |
| Cardiac Catheterization | 147 | 0.26 | 106 | 0.27 | −27.9 | 1.04 (0.81–1.34) |
| Debridement | 134 | 0.24 | 89 | 0.23 | −33.6 | 0.96 (0.73–1.26) |
| Cholecystectomy | 121 | 0.21 | 94 | 0.24 | −22.3 | 1.13 (0.86–1.48) |
| Cystoscopy or Ureteral Stent Placement | 105 | 0.19 | 88 | 0.23 | −16.2 | 1.21 (0.91–1.61) |
| Exploratory Laparotomy | 77 | 0.14 | 88 | 0.23 | +14.3 | 1.66 (1.22–2.25) |
| Incision and Drainage | 55 | 0.10 | 36 | 0.09 | −34.5 | 0.95 (0.62–1.45) |
| Craniotomy | 55 | 0.10 | 39 | 0.10 | −29.1 | 1.03 (0.68–1.55) |
4. Discussion
Consistent with prior studies, we observed a substantial decrease in ED visits during 8 weeks of the early COVID-19 surge in March and April of 2020 compared to identical weeks in 2019. The average level of acuity for ED presentations was higher during the 2020 period, which was accompanied by an increase in the number of ED critical care procedures performed and a decrease in the number of low acuity ED procedures performed. While ED critical care procedures increased, however, most urgent inpatient procedures decreased. The lower numbers of cardiac catheterizations and appendectomies may have been influenced by a preference for conservative approaches by proceduralists in the COVID-19 era [15], but there also do seem to be “missing cases” as other studies have observed [12]. Accompanying the decrease in cases was a mostly proportional decline in subspecialty consultations, except for a marked proportional rise in infectious disease consultations as a result of COVID-19. One exception to the decrease in procedures was an increase in laparotomies performed during the early pandemic period compared to the baseline period. There have been reports suggesting mesenteric ischemia requiring surgery as a thromboembolic complication of COVID-19 [16,17], and delayed presentations of surgical conditions such as appendicitis or cholecystitis could also have led to more laparotomies for peritonitis; this finding and the underlying explanations merit future study.
Some portion of the overall decreased procedures performed may be explained by lifestyle changes outside of the hospital during the COVID-19 pandemic, including decreased injuries requiring laceration repair or orthopedic fracture reduction. It is also certainly possible that some portion of care usually provided in the ED was occurring in other settings, such as through telemedicine consultations. As others have noted [10], however, it is unlikely that all of the declines observed can be attributed to a decrease in actual incidence of disease or a shift in care settings, particularly for the more severe disease states requiring procedures. Our findings therefore echo others' concerns that some patients avoided care for emergency conditions that likely warranted expedient care during the COVID-19 surge.
In addition to public health implications, our findings may be important for future hospital and ED operations planning. It would appear that fewer inpatient procedural, but more critical care resources were required to support emergency care needs during the surge. EDs can likely reduce resources devoted to low and mid-acuity cases as well as most bedside procedures during such times, but must have the personnel and equipment required to perform more critical care interventions. At a time of financial stress like the early COVID-19 pandemic, being able to predict supply and equipment needs in this way is crucial. In contrast to ED procedures, the decrease in consultation requests and inpatient procedures was relatively evenly distributed across specialties; while ENT and ophthalmology did see the largest proportional decrease, even neurosurgery and trauma surgery witnessed substantial consultation reductions. The patterns observed may help to inform the allocation of operating room resources and surgical staff in similar future scenarios, which may be particularly important at a time when staff are being redeployed to new roles.
A challenging question does arise from the decreases that have been observed in emergency health care utilization, including procedures and consultations: what proportion of the care avoided by patients was actually needed? It has been well-documented that some visits to EDs are likely unnecessary and may add little value from a health system perspective [18]. However, we also know it can be difficult for patients to predict when they truly require an emergency department evaluation or not [19]. Our data may raise concerns about patients having foregone needed care, but we cannot assess the ultimate consequences of the patterns observed. Future studies might productively leverage the decreased healthcare utilization seen during COVID-19 as a natural experiment to examine the impact of ED visits, hospitalizations, and procedures on a variety of health outcomes.
5. Limitations
This was a retrospective study that utilized aggregated electronic health record (EHR) data and is therefore subject to potential data inconsistencies within the EHR. Our analysis also only includes data from within our health system and not every hospital in Eastern Massachusetts. While the combined catchment areas of the included hospitals are quite broad, it is possible that during the COVID-19 pandemic period patients chose to avoid the quaternary academic centers within our system and go to smaller community hospitals closer to home. We did find similar decreases in ED visit volumes between our academic and community sites, but we could not examine visits outside of our system.
It is also likely that the number of positive COVID-19 tests at the included hospitals represents an undercount of total COVID-19 cases seen, both because the PCR test is not fully sensitive, and because some discharged patients may not have received COVID-19 testing. The true number of COVID-19 patients seen is therefore likely higher than we report.
Finally, we were not able to assess whether the decreases in ED visits seen were accompanied by increases in certain types of outpatient care, perhaps reflecting a shift in healthcare demand rather than an absence of demand. Further work to understand whether patients who avoided EDs sought care elsewhere, or went without care altogether, would be valuable.
6. Conclusion
In a large health system in Massachusetts, we observed a decrease in ED visits, procedures, and consultations associated with a wide range of emergency conditions during the COVID-19 pandemic. The only diagnoses, procedures, and consultations that increased were those pertaining to COVID-19 patients. While further study is needed, these data support concerns that patients were reluctant to seek emergency care for non-COVID-19 conditions during the surge. These data may help inform decisions regarding the allocation of resources by health systems during any future COVID-19 surges.
Contributions
JJB, BAW, and SD developed the paper concept and drafted the manuscript. DM completed the data extraction. SD created the tables and figures. BJY, DFMB, and ASR provided critical revisions of the manuscript for important intellectual content.
Prior presentations
None.
Financial support
None.
Declaration of Competing Interest
JJB, BAW, DM, BJY, DFMB, ASR, and SD report no conflicts of interest.
Acknowledgments
None.
References
- 1.Ouyang H. None of Us Will Ever Be the Same; New York Times: 2020 Apr 14. I’m an ER doctor in New York. [Google Scholar]
- 2.Center for Disease Control Coronavirus Disease 2019: Cases in the US. Centers for Disease Control and Prevention. 2020. https://www.cdc.gov/coronavirus/2019-ncov/cases-updates/cases-in-us.html [accessed May 30, 2020]
- 3.American College of Emergency Physicians Public Poll: Emergency Care Concerns Amidst COVID-19. 2020. https://www.emergencyphysicians.org/article/covid19/public-poll-emergency-care-concerns-amidst-covid-19 [accessed May 30, 2020]
- 4.Bullrich M.B., Fridman S., Mandzia J.L., Mai L.M., Khaw A., Gonzalez J.C., et al. COVID-19: Stroke Admissions, Emergency Department Visits, and Prevention Clinic Referrals. Canadian Journal of Neurological Sciences. 2020;47(5):693–696. doi: 10.1017/cjn.2020.101. 1–0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Morelli N., Rota E., Terracciano C., Immovilli P., Spallazzi M., Colombi D., et al. The baffling case of ischemic stroke disappearance from the casualty department in the COVID-19 era. Eur Neurol. 2020 Apr;14:1. doi: 10.1159/000507666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Garcia S., Albaghdadi M.S., Meraj P.M., Schmidt C., Garberich R., Jaffer F.A., et al. Reduction in ST-segment elevation cardiac catheterization laboratory activations in the United States during COVID-19 pandemic. J Am Coll Cardiol. 2020 Apr;10 doi: 10.1016/j.jacc.2020.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kansagra A.P., Goyal M.S., Hamilton S., Albers G.W. Collateral effect of Covid-19 on stroke evaluation in the United States. New England Journal of Medicine. 2020 May;8 doi: 10.1056/NEJMc2014816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Solomon M.D., McNulty E.J., Rana J.S., Leong T.K., Lee C., Sung S.H., et al. The Covid-19 pandemic and the incidence of acute myocardial infarction. New England Journal of Medicine. 2020 May;19 doi: 10.1056/NEJMc2015630. [DOI] [PubMed] [Google Scholar]
- 9.Kim H.S., Cruz D.S., Conrardy M.J., Gandhi K.R., Seltzer J.A., Loftus T.M., et al. Emergency department visits for serious diagnoses during the COVID-19 pandemic. Acad Emerg Med. 2020 Sep;27(9):910–913. doi: 10.1111/acem.14099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Westgard B.C., Morgan M.W., Vazquez-Benitez G., Erickson L.O., Zwank M.D. An analysis of changes in emergency department visits after a state declaration during the time of COVID-19. Ann Emerg Med. 2020 Jun;11 doi: 10.1016/j.annemergmed.2020.06.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Jeffery M.M., D’Onofrio G., Paek H., Platts-Mills T.F., Soares W.E., Hoppe J.A., et al. Trends in emergency department visits and hospital admissions in health care systems in 5 states in the first months of the COVID-19 pandemic in the US. JAMA Intern Med. 2020 Aug;3 doi: 10.1001/jamainternmed.2020.3288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wong L.E., Hawkins J.E., Murrell K.L. Where are all the patients? Addressing Covid-19 fear to encourage sick patients to seek emergency care. NEJM Catalyst Innovations in Care Delivery. 2020 May;14 [Google Scholar]
- 13.Commonwealth of Massachusetts COVID-19 State of Emergency. 2020. https://www.mass.gov/info-details/covid-19-state-of-emergency [accessed May 30, 2020]
- 14.Healthcare Cost and Utilization Project (HCUP) Clinical Classification Software Refined for ICD-10 CM Diagnoses. 2020. www.hcup-us.ahrq.gov/toolssoftware/ccsr/ccs_refined.jsp [accessed May 30, 2020]
- 15.Daniels M.J., Cohen M.G., Bavry A.A., Kumbhani D.J. 2020 Apr 13. Reperfusion of STEMI in the COVID-19 era-business as usual? Circulation. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bhayana R., Som A., Li M.D., Carey D.E., Anderson M.A., Blake M.A., et al. Abdominal imaging findings in COVID-19: preliminary observations. Radiology. 2020 May;11:201908. doi: 10.1148/radiol.2020201908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Parry A.H., Wani A.H., Yaseen M. Acute mesenteric ischemia in severe coronavirus-19 (COVID-19): possible mechanisms and diagnostic pathway. Acad Radiol. 2020 Aug 1;27(8):1190. doi: 10.1016/j.acra.2020.05.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Uscher-Pines L., Pines J., Kellermann A., Gillen E., Mehrotra A. Emergency department visits for nonurgent conditions: systematic literature review. Am J Manag Care. 2013 Jan 1;19(1):47–59. [PMC free article] [PubMed] [Google Scholar]
- 19.Coster J.E., Turner J.K., Bradbury D., Cantrell A. Why do people choose emergency and urgent care services? A rapid review utilizing a systematic literature search and narrative synthesis. Acad Emerg Med. 2017 Sep;24(9):1137–1149. doi: 10.1111/acem.13220. [DOI] [PMC free article] [PubMed] [Google Scholar]