Abstract
Introduction
Covid-19 pneumonia CT extent correlates well with outcome including mortality. However, CT is not widely available in many countries. This study aimed to explore the relationship between Covid-19 pneumonia CT extent and blood tests variations. The objective was to determine for the biological variables correlating with disease severity the cut-off values showing the best performance to predict the parenchymal extent of the pneumonia.
Methods
Bivariate correlations were calculated between biological variables and grade of disease extent on CT. Receiving Operating Characteristic curve analysis determined the best cutoffs for the strongest correlated biological variables. The performance of these variables to predict mild (<10%) or severe pneumonia (>50% of parenchyma involved) was evaluated.
Results
Correlations between biological variables and disease extent was evaluated in 168 patients included in this study. LDH, lymphocyte count and CRP showed the strongest correlations (with 0.67, −0.41 and 0.52 correlation coefficient, respectively). Patients were split into a training and a validation cohort according to their centers. If one variable was above/below the following cut-offs, LDH>380, CRP>80 or lymphocyte count <0.8G/L, severe pneumonia extent on CT was detected with 100% sensitivity. Values above/below all three thresholds were denoted in 73% of patients with severe pneumonia extent. The combination of LDH<220 and CRP<22 was associated with mild pneumonia extent (<10%) with specificity of 100%.
Discussion
LDH showed the strongest correlation with the extent of Covid-19 pneumonia on CT. Combined with CRP±lymphocyte count, it helps predicting parenchymal extent of the pneumonia when CT scan is not available.
Keywords: Coronavirus 2019 disease, CT-scan, Leukocytes
1. Introduction
The pandemic of Coronavirus disease 2019 (Covid-19) emerged in a noticeably short period of time, causing hundreds of thousands of deaths in the world. Numerous studies are currently being performed to understand the disease, find effective treatments, pending the development of a vaccine [1]. However, the underlying biological mechanisms of this viral infection are still not fully understood. Computed Tomography (CT)-scan has high sensitivity for Covid-19 pneumonia detection even though radiological signs might be delayed after symptoms onset, with up to 56% CT negativity in the first three days [2]. Sensitivity of CT-scan compared to RT-PCR may also be lower than previously thought [3]. Rigorous disinfection protocols of CT-scan and radiation doses limit the possibility of large scale CT-scanning [4]. Early chest CT might be used as diagnostic tool for containment of COVID-19 pandemic [5] but CT-scan is not widely available in many countries. Patients with mild respiratory symptoms are not necessarily referred for CT when they are diagnosed with SARS-CoV-2 infection. Previous studies demonstrated than extent of COVID-19 pneumonia on CT is related to patients’ outcome [6]. CT-scores of patients in Intensive Care Units (ICU) were significantly higher than those of discharged patients [7] Quantification of well aerated lung on CT were independent predictors of poor prognosis in COVID-19 [8]. Thus, it makes sense to predict the extent of CT lesions based on biological variables in resource-limited setting in order to facilitate hospitalization and close monitoring of patients with high extent. These patients could benefit from promising therapeutic possibilities, including anakinra [9], tocilizumab [10,11] or remdisivir [12]. However, the determinants of parenchymal extent on CT-scan are still investigated. Positive association between LDH level and severity of SARS-CoV-2 infection has been reported [13].
Thus, it would be of interest to find biological variables correlating with the extent of the pneumonia on CT, in order to have closer follow-up and/or early treatment of these patients. This study aimed to explore the relationship between CT-extent of Covid-19 pneumonia and blood tests variations. The goal was to determine the best cut-off values for biological variables correlating with CT-extent in order to predict parenchymal extent of the pneumonia based on these biological variables only.
2. Material and methods
Our local ethics committee approved this retrospective observational study (IRB AAA-2020-08026). Patients were recruited from four different hospitals (Cochin Hospital; Georges Pompidou European Hospital, Ambroise Paré Hospital; Raymond Poincaré Hospital, APHP) from emergency departments and departments of respiratory medicine between March 10th and April 10th, 2020. It was not appropriate or possible to involve patients or the public in the design, or conduct, or reporting, or dissemination plans of our research. Patients were included if they had a positive RT-PCR result, an available initial CT-scan and blood tests with at least LDH dosage.
Demographics and biological variables including complete white blood cell and platelet counts, LDH, CRP and D-dimers were collected. These data were collected on the same day that the CT-scan.
CT-scan images were evaluated by a senior resident and a thoracic radiologist with 20 years of experience, in consensus. The extent of pneumonia was graded as follows: normal CT-scan (grade 0), minimal involvement with less than 10% of involved lung parenchyma (grade 1), moderate involvement (grade 2; approximately 10–25%); extended involvement (grade 3, 25–50%); severe involvement (grade 4; 50–75%); critical involvement (grade 5; >75%).
2.1. Correlation between CT-scan and biological variables
Bivariate correlations using Spearman's rank correlation coefficient were calculated between continuous biological variables and the ordinal variable of interest, CT-scan grade. A p-value<0.05 was considered as statistically significant. Weak correlation was defined as coefficient magnitude less than 0.4, moderate correlation as coefficients between 0.4 and 0.7 and strong correlation as coefficients >0.7.
2.2. Determination of cut-offs to predict CT-scan extent of the pneumonia
Consecutive patients were divided in 2 groups: a training cohort including patients from Cochin Hospital and Ambroise Paré Hospital and a cohort of validation with patients from Raymond Poincaré Hospital and Georges Pompidou European Hospital. The extent of pneumonia was evaluated as “LOW” (less than 10% of parenchymal involvement, grade 0 or 1), “INTERMEDIATE” (10–50% of parenchyma, grade 2 and 3) and “HIGH” (more than 50%, including grade 4 and 5). Variables with moderate to strong correlation coefficients were explored. Adequate cut-offs were determined using Receiving Operator Characteristic (ROC) curve analysis to differentiate “HIGH” extent of the pneumonia versus other patients (“LOW” and “INTERMEDIATE”) with high sensitivity (Se). Another ROC curve analysis was performed to differentiate “LOW” extent of the pneumonia from other patients (“INTERMEDIATE” and “HIGH”) with high specificity (Spe). We determined as useful variables those with Areas Under the Curve (AUC) of at least 0.75.
SPSS software (version 24,Chicago, IL,USA) was used for statistical analysis.
3. Results
A total of 393 patients were eligible in the 4 university hospitals. Of them, 225 were excluded because LDH levels were lacking. Consequently, 168 patients with a mean age of 64.7 years (STD = 15.7; range = [23–97]), 109 men and 59 women were included in this study (Table 1 ). All patients had available LDH and CRP results. D-dimers were available for 85 patients and complete white blood count for 110 patients.
Table 1.
Clinical characteristics and CT-score of included patients; STD = standard deviation.
| Numbers (Proportion) | Confidence Intervals | |
|---|---|---|
| Characteristics | ||
| Patients | 168 | |
| Age (mean) | 64.8 years | STD = 15.7 years |
| Sex (males) | 109 (64.8%) | [57.1%; 72%] |
| Onset to CT-scan | 6.7 days | STD = 3.7 days |
| CT-score | ||
| 0 | 6 (3.6%) | [1.5%–8%] |
| 1 | 20 (11.9%) | [7.6%–18.0%] |
| 2 | 44 (26.2%) | [19.9%–33.6%] |
| 3 | 61 (36.3%) | [29.1%–44.1%] |
| 4 | 24 (14.3%) | [9.5%–20.7%] |
| 5 | 13 (7.7%) | [4.4%–13.1%] |
| Outcomes | ||
| Intubation | 42 (25.0%) | [18.8%–32.4%] |
| Death | 27 (16.1%) | [11%–22.7%] |
3.1. Correlation between CT-scan and biological variables
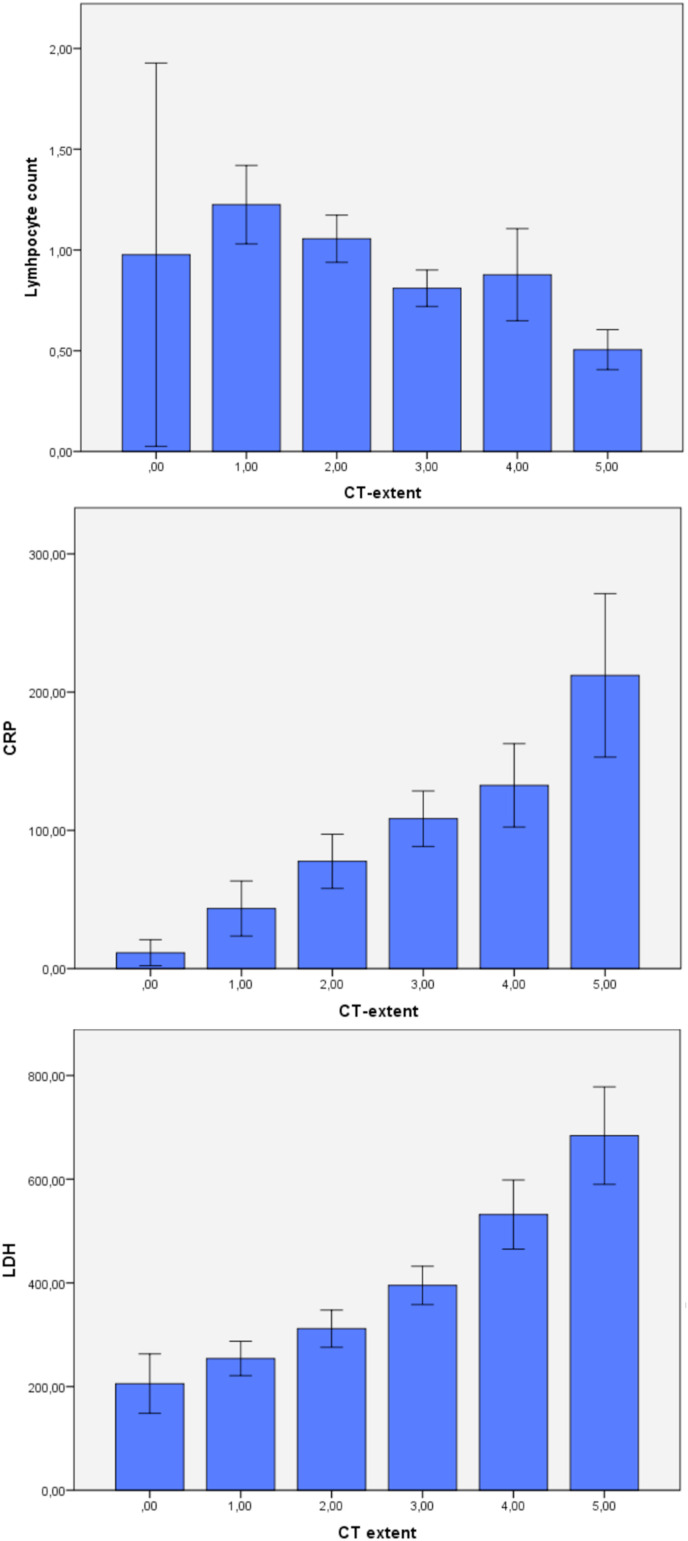
Of the 168 patients, the biological variables significantly correlating with CT-scan extent were lymphocyte, eosinophil, basophil, monocyte and neutrophil counts, LDH and CRP (Table 1). LDH, lymphocyte count, CRP showed moderate correlations (with 0.67, −0.41 and 0.52 correlation coefficient, respectively), with decreased lymphocyte count and increased CRP and LDH correlating with more severe involvement (Fig. 1 ). Eosinophil, basophil, monocyte, neutrophil counts were only weakly correlated (Table 2 ). Platelet count and D-dimers were not correlated to the extent of pneumonia.
Fig. 1.
Correlation between CT-extent and lymphocyte count (0 = absent; 1 = minimal; 2 = moderate; 3 = extended; 4 = severe; 5 = critical), CRP and LDH
Table 2.
Correlations between CT-extent and biological variables (white blood cell count, platelets, CRP, D-dimers, LDH) using Spearman's coefficient; Lympho = lymphocytes; Eosino = eosinophils; Baso = Basophils; Mono = Monocytes; Neutro = Neutrophils.
| Lympho | Eosino | Baso | Neutro | Mono | CRP | Platelets | D-dimers | LDH | |
|---|---|---|---|---|---|---|---|---|---|
| Absent | 0.98 | 0.05 | 0.03 | 4.50 | 0.66 | 11.5 | 219.0 | 1229 | 206 |
| Minimal | 1.23 | 0.09 | 0.02 | 4.84 | 0.56 | 43.5 | 242.0 | 1015 | 254 |
| Moderate | 1.06 | 0.04 | 0.02 | 4.58 | 0.56 | 77.6 | 206.6 | 2166 | 312 |
| Extended | 0.81 | 0.01 | 0.01 | 5.61 | 0.45 | 108.4 | 196.8 | 4694 | 395 |
| Severe | 0.88 | 0.02 | 0.02 | 6.50 | 0.40 | 132.6 | 234.9 | 1151 | 532 |
| Critical | 0.51 | 0.02 | 0.01 | 8.06 | 0.46 | 212.1 | 251.8 | 2535 | 684 |
| Coeff | −0.41 | −0.32 | −0.22 | 0.38 | −0.25 | 0.52 | 0.08 | 0.19 | 0.67 |
| p-value | <10−3 | 0.001 | 0.02 | <10−3 | 0.008 | <10−3 | 0.39 | 0.08 | <10−3 |
3.2. Determination of cut-offs to predict CT-scan extent of the pneumonia
98 patients were included in the training cohort and 70 in the validation cohort.
In the training cohort, 11 patients had “LOW” CT-extent (<10%), 51 patients had “INTERMEDIATE” CT-scan extent (10–50%) and 26 “HIGH” CT-extent (>50%).
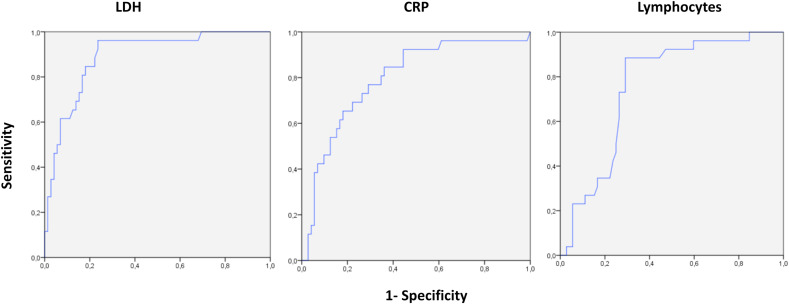
First, ROC curve analysis was performed to differentiate “HIGH” CT-extent from other patients (<50% CT-extent) (Fig. 2 ). Lymphocytes <0.8G/L (Se = 0.89; Spe = 0.71, AUC = 0.76), CRP>80 (Se = 0.85; Spe = 0.63, AUC = 0.79), and LDH>380 (Se = 0.96; Spe = 0.74, AUC = 0.89) were determined as the best cut-offs to differentiate these 2 groups.
Fig. 2.
ROC curve analysis of LDH, CRP and Lymphocytes to differentiate “HIGH” (>50%) CT-extent of COvid-19 pneumonia from other patients (“INTERMEDIATE” and “LOW”, <50%).
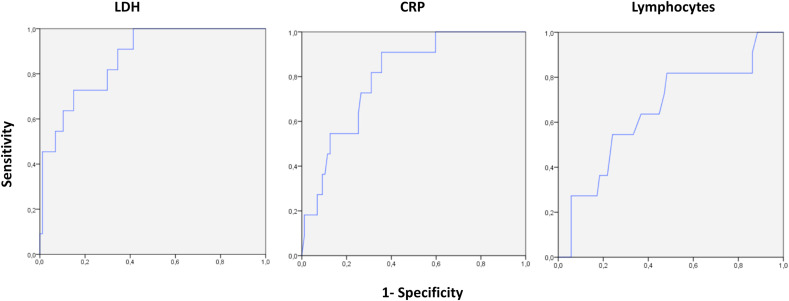
Then, a second ROC curve analysis (Fig. 3 ) was performed to differentiate “LOW” CT-extent from other patients (>10% CT-extent). The best cut-offs were CRP<22 (Se = 0.36; Spe = 0.91, AUC = 0.80) and LDH<220 (Se = 0.55; Spe = 0.92, AUC = 0.87). Lymphocyte count exhibited only moderate performance to differentiate these 2 groups with AUC = 0.65 and was therefore not used.
Fig. 3.
ROC curve analysis of LDH, CRP and Lymphocytes to differentiate “LOW” (<10%) CT-extent of COvid-19 pneumonia from other patients (“INTERMEDIATE” and “HIGH”, >10%).
In the validation cohort, 15 patients had “LOW” involvement, 47 “INTERMEDIATE” extent and 11 “HIGH” extent. The AUC to differentiate “HIGH” parenchymal extent from others was 0.82 with 100% of sensitivity if at least one of the 3 variables was above (CRP>80 and LDH>380) or below (lymphocytes<0.8G/L) the cut-offs and 100% of Negative Predictive Value (NPV) when none of these variables were above or below the cutoffs (19/62 patients). Eight of the 11 patients (73%) with >50% parenchymal extent on CT had all 3 variables above/below the thresholds.
The AUC to differentiate “LOW” parenchymal extent from others was of 0.75 with 100% of specificity when CRP was <22 and LDH<220 (for 6 of the 15 patients [40%] with normal CT-scan or grade 1).
4. Discussion
We found that LDH was the biological parameter showing the strongest correlation with Covid-19 pneumonia CT extent, while lymphocyte count and CRP were also moderately correlated. Lymphocytes <0.8G/L, CRP>80 and LDH>380 were useful to suspect severe pneumonia with at least 50% of CT-extent (grade 4 or 5). Furthermore, CRP<22 and LDH<220 were useful to predict mild parenchyma extent (<10%, grade 0 or 1). We tried to differentiate patients that might have mild CT involvement or normal CT and those with high CT-extent as previous literature suggest that patient with lower parenchymal involvement have better prognosis [14]. Therefore, biological variables can capture those patients that need closer monitoring versus those that are less at risk of severe pneumonia. This could be useful in countries with limited access to CT-scan and to ease the burden on imaging facilities during the ongoing pandemic. Diagnostic strategy combining RT-PCR and these biological values could for example help choosing patients which might benefit the most from CT-scan. Thus, these two thresholds can aid in decision making ability to allocate the resources in appropriate manner.
A previous study from J Wu et al. reported weak or moderate correlations between pulmonary infiltration index and lymphocyte count, monocyte count, CRP, PCT and clinical variables in 80 patients [15], but the correlation with LDH was not evaluated in this study. Other studies presented low lymphocyte count as a risk factor for disease progression in 17 patients [16] and CRP as a predictor of severe form of COVID-19 pneumonia in 27 patients [17]. COVID 19 pneumonia can lead to Acute Respiratory Distress Syndrome (ARDS) which is characterized by relatively preserved compliance but higher frequency of thrombotic events [18]. D-dimers are elevated in case of pulmonary embolism in COVID-19 patients [19] but increased d-dimer level (greater than 1 μg/mL) has also been already identified as a risk factor for poor outcome, but this dosage was only available for a minority of our patients [20]. LDH, an enzyme that catalyzes the conversion of lactate in pyruvate is increased in case of important tissue damage, e.g. in pneumocystis pneumonia [21]. Therefore, LDH could also be an interesting biological marker of Covid-19 pneumonia. LDH has been positively associated with Covid-19 severity in previous studies [13]. Our study confirms the association between LDH levels and parenchymal extent of the pneumonia. This could help understand the pathophysiological biological variations occurring in severe forms of pneumonia caused by SARS-CoV-2 infection.
These markers of severity could also help predicting disease worsening, which might occur after 7–10 days of evolution [22]. Elevated PCT, creatinine, amino transferase, cardiac troponin and D-dimers were also described as risk factors of critical Covid-19 infection [23].
Chest X-ray is an interesting tool when CT-scan is not available, in particular for critically-ill patients that cannot be moved [24]. However, determining the extent of Covid-19 pneumonia on X-ray is limited since the sensitivity for ground-glass opacity is imperfect. Recently published works studied the use of artificial intelligence as a tool to increase X-ray diagnostic and prognostic power, which is a great support especially in places where CT is not readily available [25,26].
Our study presents several limitations. First, almost all included patients had available blood tests including LDH because they were hospitalized, with 25% of them being intubated and 16% having fatal outcome. Our results might not be reproducible for outpatients with less severe symptoms. However, hospitalized patients are those who are more likely to develop severe forms of the disease. The estimation of disease extent on CT was based on visual assessment and not quantified using automated methods, which is prone to interobserver variability, this is the reason why it was evaluated by an experienced chest radiologist in our study. Even though the pandemic has affected a large number of individuals, we could only include 168 patients having complete blood cell count and LDH dosage in addition to CT, due to the retrospective design of our study and lack of standardization of biological tests during the first wave of the pandemic. Thus, our results need to be prospectively validated on a larger series.
In conclusion, LDH, CRP and lymphocyte count could be useful to predict disease extent severity when CT is not available. This could help selection of patients requiring closer follow-up and/or early specific treatment when available.
Funding
None.
CRediT authorship contribution statement
Mickael Tordjman: Conceptualization, Methodology, Investigation, Formal analysis, Writing - original draft. Ahmed Mekki: Conceptualization, Methodology, Investigation, Writing - original draft. Rahul D. Mali: Formal analysis, Writing - original draft. Hippolyte Monnier: Methodology, Investigation. Sophie Neveu: Investigation. Guillaume Chassagnon: Visualization, Investigation. Fadila Mihoubi: Visualization, Investigation. Nicolas Carlier: Methodology, Resources. Jonathan Marey: Methodology, Resources. Laure Fournier: Methodology, Resources, Investigation. Robert-Yves Carlier: Methodology, Resources, Investigation. Jean-Luc Drapé: Conceptualization, Methodology, Investigation, Supervision. Marie-Pierre Revel: Conceptualization, Project administration, Methodology, Supervision, Writing - review & editing.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
References
- 1.Baden L.R., Rubin E.J. Covid-19 — the search for effective therapy. N. Engl. J. Med. 2020 doi: 10.1056/NEJMe2005477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bernheim A., Mei X., Huang M., Yang Y., Fayad Z.A., Zhang N., Diao K., Lin B., Zhu X., Li K., Li S., Shan H., Jacobi A., Chung M. Chest CT findings in coronavirus disease-19 (COVID-19): relationship to duration of infection. Radiology. 2020:200463. doi: 10.1148/radiol.2020200463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Waller J.V., Allen I.E., Lin K.K., Diaz M.J., Henry T.S., Hope M.D. The limited sensitivity of chest computed tomography relative to reverse transcription polymerase chain reaction for severe acute respiratory syndrome coronavirus-2 infection: a systematic review on COVID-19 diagnostics. Invest. Radiol. 2020 doi: 10.1097/RLI.0000000000000700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Nakajima K., Kato H., Yamashiro T., Izumi T., Takeuchi I., Nakajima H., Utsunomiya D. COVID-19 pneumonia: infection control protocol inside computed tomography suites. Jpn. J. Radiol. 2020 doi: 10.1007/s11604-020-00948-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Amalou A., Türkbey B., Sanford T., Harmon S., Türkbey E.B., Xu S., An P., Carrafiello G., Cariati M., Patella F., Obinata H., Mori H., Sun K., Spiro D.J., Suh R., Amalou H., Wood B.J. Targeted early chest CT in COVID-19 outbreaks as diagnostic tool for containment of the pandemic-A multinational opinion. Diagn Interv Radiol. 2020;26:292–295. doi: 10.5152/dir.2020.20231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Liu Z., Jin C., Wu C.C., Liang T., Zhao H., Wang Y., Wang Z., Li F., Zhou J., Cai S., Zeng L., Yang J. Association between initial chest CT or clinical features and clinical course in patients with coronavirus disease 2019 pneumonia. Korean J. Radiol. 2020;21:736–745. doi: 10.3348/kjr.2020.0171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chen H.J., Qiu J., Wu B., Huang T., Gao Y., Wang Z.P., Chen Y., Chen F. Early chest CT features of patients with 2019 novel coronavirus (COVID-19) pneumonia: relationship to diagnosis and prognosis. Eur. Radiol. 2020 doi: 10.1007/s00330-020-06978-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Colombi D., Bodini F.C., Petrini M., Maffi G., Morelli N., Milanese G., Silva M., Sverzellati N., Michieletti E. Well-aerated lung on admitting chest CT to predict adverse outcome in COVID-19 pneumonia. Radiology. 2020 doi: 10.1148/radiol.2020201433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Huet T., Beaussier H., Voisin O., Jouveshomme S., Dauriat G., Lazareth I., Sacco E., Naccache J.-M., Bézie Y., Laplanche S., Berre A.L., Pavec J.L., Salmeron S., Emmerich J., Mourad J.-J., Chatellier G., Hayem G. Anakinra for severe forms of COVID-19: a cohort study. The Lancet Rheumatology. 2020 doi: 10.1016/S2665-9913(20)30164-8. 0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Xu X., Han M., Li T., Sun W., Wang D., Fu B., Zhou Y., Zheng X., Yang Y., Li X., Zhang X., Pan A., Wei H. Effective treatment of severe COVID-19 patients with tocilizumab. Proc. Natl. Acad. Sci. Unit. States Am. 2020;117:10970–10975. doi: 10.1073/pnas.2005615117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Cellina M., Orsi M., Bombaci F., Sala M., Marino P., Oliva G. Favorable changes of CT findings in a patient with COVID-19 pneumonia after treatment with tocilizumab. Diagnostic and Interventional Imaging. 2020;101:323–324. doi: 10.1016/j.diii.2020.03.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Goldman J.D., Lye D.C.B., Hui D.S., Marks K.M., Bruno R., Montejano R., Spinner C.D., Galli M., Ahn M.-Y., Nahass R.G., Chen Y.-S., SenGupta D., Hyland R.H., Osinusi A.O., Cao H., Blair C., Wei X., Gaggar A., Brainard D.M., Towner W.J., Muñoz J., Mullane K.M., Marty F.M., Tashima K.T., Diaz G., Subramanian A. Remdesivir for 5 or 10 Days in patients with severe covid-19. N. Engl. J. Med. 2020 doi: 10.1056/NEJMoa2015301. 0, null. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Deng X., Liu B., Li J., Zhang J., Zhao Y., Xu K. Blood biochemical characteristics of patients with coronavirus disease 2019 (COVID-19): a systemic review and meta-analysis. Clin. Chem. Lab. Med. 2020;1 doi: 10.1515/cclm-2020-0338. [DOI] [PubMed] [Google Scholar]
- 14.Francone M., Iafrate F., Masci G.M., Coco S., Cilia F., Manganaro L., Panebianco V., Andreoli C., Colaiacomo M.C., Zingaropoli M.A., Ciardi M.R., Mastroianni C.M., Pugliese F., Alessandri F., Turriziani O., Ricci P., Catalano C. Chest CT score in COVID-19 patients: correlation with disease severity and short-term prognosis. Eur. Radiol. 2020 doi: 10.1007/s00330-020-07033-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wu J., Wu X., Zeng W., Guo D., Fang Z., Chen L., Huang H., Li C. Chest CT findings in patients with coronavirus disease 2019 and its relationship with clinical features. Invest. Radiol. 2020;55:257–261. doi: 10.1097/RLI.0000000000000670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Zhou Y., Zhang Z., Tian J., Xiong S. Risk factors associated with disease progression in a cohort of patients infected with the 2019 novel coronavirus. Ann. Palliat. Med. 2020;9:428–436. doi: 10.21037/apm.2020.03.26. [DOI] [PubMed] [Google Scholar]
- 17.Tan C., Huang Y., Shi F., Tan K., Ma Q., Chen Y., Jiang X., Li X. C-reactive protein correlates with computed tomographic findings and predicts severe COVID-19 early. J. Med. Virol. 2020 doi: 10.1002/jmv.25871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Grasselli G., Tonetti T., Protti A., Langer T., Girardis M., Bellani G., Laffey J., Carrafiello G., Carsana L., Rizzuto C., Zanella A., Scaravilli V., Pizzilli G., Grieco D.L., Di Meglio L., de Pascale G., Lanza E., Monteduro F., Zompatori M., Filippini C., Locatelli F., Cecconi M., Fumagalli R., Nava S., Vincent J.-L., Antonelli M., Slutsky A.S., Pesenti A., Ranieri V.M., collaborators Pathophysiology of COVID-19-associated acute respiratory distress syndrome: a multicentre prospective observational study. Lancet Respir Med. 2020 doi: 10.1016/S2213-2600(20)30370-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bompard F., Monnier H., Saab I., Tordjman M., Abdoul H., Fournier L., Sanchez O., Lorut C., Chassagnon G., Revel M. Pulmonary embolism in patients with Covid-19 pneumonia. Eur. Respir. J. 2020 doi: 10.1183/13993003.01365-2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Zhou F., Yu T., Du R., Fan G., Liu Y., Liu Z., Xiang J., Wang Y., Song B., Gu X., Guan L., Wei Y., Li H., Wu X., Xu J., Tu S., Zhang Y., Chen H., Cao B. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395:1054–1062. doi: 10.1016/S0140-6736(20)30566-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Boldt M.J., Bai T.R. Utility of lactate dehydrogenase vs radiographic severity in the differential diagnosis of Pneumocystis carinii pneumonia. Chest. 1997;111:1187–1192. doi: 10.1378/chest.111.5.1187. [DOI] [PubMed] [Google Scholar]
- 22.Li K., Chen D., Chen S., Feng Y., Chang C., Wang Z., Wang N., Zhen G. Predictors of fatality including radiographic findings in adults with COVID-19. Respir. Res. 2020;21:146. doi: 10.1186/s12931-020-01411-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Zheng Z., Peng F., Xu B., Zhao J., Liu H., Peng J., Li Q., Jiang C., Zhou Y., Liu S., Ye C., Zhang P., Xing Y., Guo H., Tang W. Risk factors of critical & mortal COVID-19 cases: a systematic literature review and meta-analysis. J. Infect. 2020 doi: 10.1016/j.jinf.2020.04.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.de Barry O., Obadia I., El Hajjam M., Carlier R.-Y. Chest-X-ray is a mainstay for follow-up in critically ill patients with covid-19 induced pneumonia. Eur. J. Radiol. 2020;129:109075. doi: 10.1016/j.ejrad.2020.109075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Blain M., T Kassin M., Varble N., Wang X., Xu Z., Xu D., Carrafiello G., Vespro V., Stellato E., Ierardi A.M., Di Meglio L., D Suh R., Walker S.A., Xu S., H Sanford T., Turkbey E.B., Harmon S., Turkbey B., J Wood B. Determination of disease severity in COVID-19 patients using deep learning in chest X-ray images. Diagn Interv Radiol. 2020 doi: 10.5152/dir.2020.20205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Mushtaq J., Pennella R., Lavalle S., Colarieti A., Steidler S., Martinenghi C.M.A., Palumbo D., Esposito A., Rovere-Querini P., Tresoldi M., Landoni G., Ciceri F., Zangrillo A., De Cobelli F. Initial chest radiographs and artificial intelligence (AI) predict clinical outcomes in COVID-19 patients: analysis of 697 Italian patients. Eur. Radiol. 2020 doi: 10.1007/s00330-020-07269-8. [DOI] [PMC free article] [PubMed] [Google Scholar]