Abstract
Background
Severe acute respiratory syndrome corona virus 2 (SARS- CoV-2) is known as COVID 19 seems to be one of the most contagious and dangerous infection in children and adults. According to first adult studies association of gastrointestinal (GI) symptoms with COVID 19 infection was as high as 79% (1).But later study showed lower association around 18% (2).As the pandemic of COVID 19 is going on, different clinical presentation of disease especially in children are well appeared. In addition atypical presentations may confuse and mislead physician to do different diagnostic procedures and interventions. We report a 6 years and half old boy with diarrhea, abdominal pain with first diagnosis acute abdomen due to acute appendicitis. At last diagnosis of pneumatosis intestinalis due to enterocolitis was confirmed.
Case presentation
A 6 years and half old boy with severe abdominal pain admitted in emergency ward. He had history of fever, nine days of diarrhea and recurrent vomiting. The abdominal pain was severe with moderate tenderness in right lower quadrant. He admitted in pediatric surgery ward after surgical consultation for rolling out acute appendicitis. The results of first lab studies were shown leucopenia, lymphopenia and COVID 19 PCR was positive. During admission the cough has increased and abdominal distention has evolved. Vomiting was intractable and feeding was impossible. Pneumatosis intestinalis in ascending colon and dilatation in colon caliber were detected abdominal. Miliary like pattern in lung has reported in chest CT. Stool exam results revealed loss of protein in high amount in spite of normal pancreatic and enterocyte function. The calprotectin was high and implied high inflammation in large intestine. With all above data necrotizing enterocolitis management was started. After 14 days patients had good appetite and feeding slowly introduced. All symptoms resolved with exception of cough. Albumin and other electrolytes remained stable. The patient discharged without morbidity.
Conclusion
COVID 19 infection has many different and mysterious presentations. GI manifestations are among important, common presentations. The acute abdomen like presentation with different complications like pneumatosis intestinalis, protein losing enteropathy are not common but knowledge about these presentations assist physician to be aware and make decision accurately.
Keywords: COVID 19, Children, Pneumatosis intestinalis, Protein losing enteropathy, Acute abdomen, “Case report”
1. Background
Severe acute respiratory syndrome corona virus 2 (SARS- CoV-2) is known as COVID 19 seems to be one of the most contagious and dangerous infection in children and adults. As the pandemic of COVID 19 is going on, different clinical presentation of disease especially in children are well appeared. We know after respiratory signs and symptoms, gastrointestinal (GI) manifestations are the most common in children and adults. The fecal mucosal transmission is one of the well known routes of infection. The virus shedding in the stool has been continued even when the virus is not found in respiratory tract anymore. According to adult studies association of GI symptoms with COVID 19 infection may imply worse prognosis. In addition atypical presentations may confuse and mislead physician to do different diagnostic procedures and interventions. We report a 6 years and half old boy with diarrhea, abdominal pain and later diagnosis of enterocolitis.
2. Case presentation
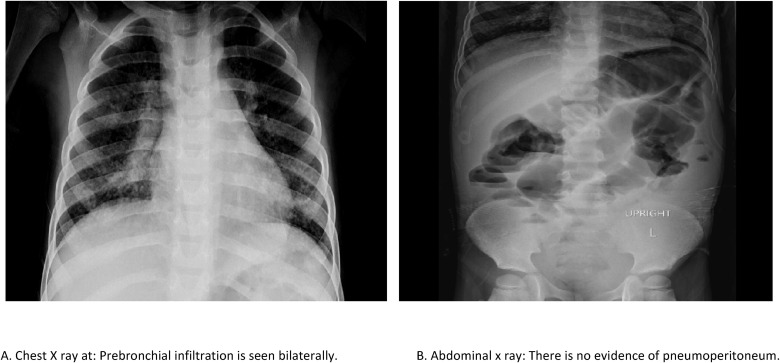
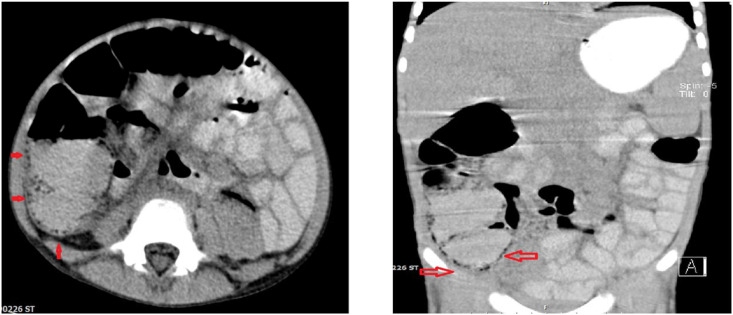
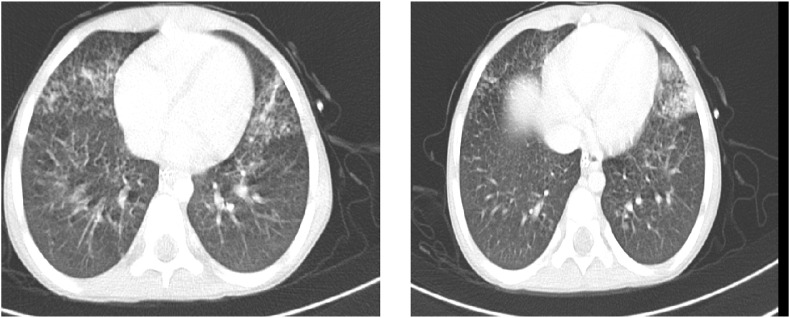
A 6 years and half old boy with severe abdominal pain admitted in emergency ward. He had history of fever, nine days of diarrhea and recurrent vomiting. He had three outpatient visits and got oral rehydration solution (ORS) and ondansetrone. The abdominal pain was severe with moderate tenderness in right lower quadrant. He admitted in pediatric surgery ward after surgical consultation for rolling out acute appendicitis. Since close observation in pediatric surgery ward the patient had scattered cough and fever was 38.5 °C. According to the consultation of pediatric infectious service chest X ray and nasopharyngeal COVID 19 PCR test were performed. The results of first lab and radiologic studies were shown in Table 1 and Fig. 1 . The first results have shown leucopenia, lymphopenia and COVID 19 PCR was positive. The first abdominal ultrasound showed distended gall bladder and sludge and normal appendix. Abdominal X ray was unremarkable. The patient has referred to COVID 19 ward. During admission the cough has increased and abdominal distention has evolved. Vomiting was intractable and feeding was impossible. According to GI consult abdominal and pelvic CT was performed in addition to spiral chest CT. The results have shown in Fig. 2, Fig. 3 . New lab tests have shown hypoalbuminemia, hypocalcaemia, hypophasphatemia and hypomagnesaemia. Mild elevation of AST and lipase were seen. Pneumatosis intestinalis in ascending colon and dilatation in colon caliber were detected. Miliary like pattern in lung has reported and investigations about immune deficiency, fungal infection and TB were recommended. Stool exam results revealed loss of protein in high amount in spite of normal pancreatic and enterocyte function. The calprotectin was high and implied high inflammation in large intestine. With all above data necrotizing enterocolitis management was started. The patient was NPO for 14 days. Parenteral nutrition with correction of electrolyte imbalances was advocated. Wide spectrum intravenous antibiotics (ceftazidime 150 mg/kg/d + metronidazole 30 mg/kg/d for 14 days) were administered. The culture results from blood, urine and stool were all negative. Toxin A and B for C. difficile were negative. The general condition had improved slowly and the vomiting resolved at day of 10. Fever subsided at 12 days from admission. After 14 days patients had good appetite and feeding slowly introduced. All symptoms resolved with exception of cough. Albumin and other electrolytes remained stable. The patient discharged without morbidity.
Table 1.
Lab data.
| Lab test | Admission time | Hospitalization Time | Discharge Time |
|---|---|---|---|
| WBC (103/micl) | 3100 | 2300 | 5200 |
| Neutrophil | 64 | 65 | 60 |
| Lymphocyte | 26 | 24 | 35 |
| Hemoglobin (g/dl) | 11.8 | 11.7 | 11.8 |
| MCV (fl) | 77 | 75 | 76 |
| Platelet (103/micL) | 215 | 194 | 218 |
| ESR (mm/hr) | 18 | 20 | 5 |
| CRP (mg/dl) | 30 | 78 | 7 |
| AST (U/L) | 27 | 110 | 78 |
| ALT (U/L) | 20 | 11 | 10 |
| ALP (U/L) | 218 | 201 | 107 |
| GGT (U/L) | – | 54 | – |
| ALB (g/dl) | – | 1.3 | 3.7 |
| Total Protein (g/dl) | – | 5.5 | 6.1 |
| Globulin (g/dl) | – | 3.2 | 2.4 |
| Amyl (U/L) | – | 13 | – |
| Lipase (U/L) | – | 130 | 45 |
| Triglyceride (mg/dl) | – | 131 | – |
| Cholestrol (mg/dl) | – | 63 | – |
| LDH (IU/L) | – | 545 | – |
| PT (sec)/INR | – | 13/1 | 13/1 |
| PTT (sec) | – | 35 | 34 |
| Calcium (mg/dl) | – | 6.4 | 8.6 |
| Phosphorus (mg/dl) | – | 3 | 3.8 |
| Magnesium (mg/dl) | – | 1.5 | 2.7 |
| BUN (mg/dl) | – | 12.8 | 7 |
| Cr (mg/dl) | – | 0.5 | 0.4 |
| Stool WBC | – | 1–3 | – |
| Stool RBC | – | 2–4 | – |
| Stool mucus | – | 2+ | – |
| Stool fat | – | + | – |
| Stool Sudan III | – | <30 | – |
| Stool trypsin activity | – | 1/128 | – |
| Stool fecal elastase 1 (micro gr/gr) | – | 280 | – |
| Stool alpha 1 antitrypsin (micro gr/gr) | – | 2160 | – |
| Stool calprotectin | – | 1115 | – |
| Stool culture | – | Neg | – |
| Stool toxin A and B for C.diffcile | – | Neg | – |
Fig. 1.
Admission time A. Chest X ray at: Prebronchial infiltration is seen bilaterally. B. Abdominal x ray: There is no evidence of pneumoperitoneum.
Fig. 2.
Spiral abdominal and pelvic CT with and without IV contrast: A. Pneumatosis intestinalis is noted (red arrows) in ascending colon with dilated colon caliber. Transverse colon diameter was measured 50 mms. B. Multifocal small bowel loops intussusceptum are noted as a transient finding. Prominent paraaortic lymph nodes up to 8 mms are seen. Mild splenomegaly is seen. (For interpretation of the references to colour in this figure legend, the reader is referred to the Web version of this article.)
Fig. 3.
Chest CT with IV contrast: A B. A, B Peribronchial thickening and subsegmental consolidation in bilateral paracardiac is also noted. Bilateral hilar lymph nodes are prominent. Miliary pattern in bilateral upper lobes are seen.
3. Discussion
GI system involvement is well known in COVID 19 infection. There are many angiotensin converting enzyme 2(ACE 2) receptors in small intestine especially in ileum and colon. In addition cholangiocytes and pancreatic cells have these receptors. Protein S of COVID 19 attaches to the receptors and transmembrane protease serine 2 (TMPRSS2) help to detach from cell membrane [[3], [4], [5]]. This mechanism makes the GI system one of the easy route of entry for viruses. One in four children has GI manifestations. The most common manifestations are diarrhea, vomiting and abdominal pain [2]. Loss of appetite and weight loss are other common complications [1]. According to Xiong et al. children with fever or age lower than 2 years of old had more GI symptoms. In addition virus can be found in stool in the same amount between children with GI symptoms and without GI symptoms [6].
As the pandemic of COVID 19 is going on, different clinical presentation of disease especially in children are well appeared. In our patient severe abdominal pain and right lower quadrant tenderness without respiratory symptoms has lead patient to surgery ward. The acute appendicitis was first suspected diagnosis. Acute appendicitis like presentation associated with COVID 19 infection has been reported in literature especially in children. For the first time Calinescu et al. have reported four children with severe abdominal pain with guarding and tenderness [7]. The focus of pain was in right lower quadrant. Clinical diagnoses of all four were perforated acute appendicitis. Abdominal CT was the modality that has provided more information. All patients had conservative management with antibiotics and anticoagulants. Tullie et al. has reported six children with Asian or black ethnicity with severe abdominal pain and acute appendicitis like presentation. The courses of illness in all six patients were severe but fortunately no one has passed away [8]. The authors remind us about atypical presentations of COVID 19 with abdominal pain and appendicitis like presentation and recommend imaging studies and screening of COVID 19 infection in this group of patients. Suwanwongse and Shabarek has reported 18 years old female with severe abdominal pain, nausea, vomiting but without respiratory symptoms [9]. The lab findings were suggestive of COVID 19 infection despite abdominal ultrasound which was suggestive of acute appendicitis. Positive PCR for COVID 19 infection and normal CT help the physician to make correct decision. Ekbatani et al. has reported 2 cases with severe abdominal pain and recurrent vomiting and ultrasound findings in favor of acute appendicitis. Abdominal CT incidentally showed lower lung involvement with COVID 19 infection. After management of infection children discharged without surgical intervention [10].There are several case reports about acute appendicitis like presentation and acute surgical abdomen in adults [[11], [12], [13], [14]]. We conclude that COVID 19 infection may present with severe acute abdominal pain and mimic acute appendicitis. Thus during pandemic of COVID 19 surgeons should consider this infection and use radiologic studies beside clinical examination.
The results of abdominal CT were pneumatosis intestinalis in ascending colon, colon dilatation and recurrent small bowel intussusceptions were seen. Cai et al. [15] and Moazzam [16] et al. both have reported cases with intussusception. Unfortunately one of cases died because of multi organ failure. In our case it was transient phenomenon and according to radiologist opinion no intervention was needed.
Our patient with recurrent vomiting, abdominal distention and pneumatosis intestinalis diagnosed as necrotizing enterocolitis. Two weeks of NPO with wide spectrum antibiotic and supportive TPN has improved the condition of patient. Two cases of pneumatosis intestinalis were reported in literature in association with COVID 19 infection but in adult. Lakshmanan et al. [17] reported 72 years old male with diffuse abdominal pain, abdominal distention and fever who was admitted in hospital. Abdominal CT showed ascending colon pneumatosis intestinalis and dilatation of sigmoid and rectum. No operation was needed and supportive management was the only treatment for GI complications. 44 years old man was reported by Meini et al. [18] who was hospitalized for respiratory symptoms of COVID 19 infection. Later after improvement of respiratory symptoms incidentally they have noticed about pneumatosis intestinalis in cecum and right colon. Patient had no GI symptom. Patient was discharged without sequel. Pneumatosis intestinalis has lots of reason. GI disease like inflammatory bowel disease, ischemic bowel disease, obstructive bowel disease and post upper and lower endoscopy are some of them. In addition other disorder as obstructive lung disease, medication as corticosteroid and post surgery is other reasons. Between infections CMV and HIV are capable of producing pneumatosis intestinalis [18]. When the patient has no symptoms, under observation and supportive therapy is sufficient management. But in patients with clinical manifestations more intense therapy and close observation is necessary. Pneumatosis intestinalis may change to pneumoperitoneum and bowel perforation [18].
As far as we know protein losing enteropathy due to COVID 19 infection was not reported yet. In our patient stool alfa 1 antitrypsin was very high and liver and kidney function were normal. Post infection protein losing enteropathy was mentioned due to rotavirus, CMV, shigella and C.dificcile. Post infection protein losing enteropathy may be severe but usually transient [19].
The most common findings in chest CT of patients with COVID 19 infection are ground-glass opacities and consolidations [20]. Miliary like lesions were found in our patient. Our radiologist has recommended investigations about tuberculosis, fungal infection and immunodeficiency. All other studies were normal and no other diagnoses were found.
Another important point about our patient was high stool calprotectin. According to study by Grabherr et al. [14] in patients with COVID 19 infection, high calprotectin was detected in patients with stopped diarrhea and patients with ongoing diarrhea in comparison with patients without diarrhea at all. This is definitely important in patient with inflammatory bowel disease in whom differentiation of COVID 19 infection from disease exacerbation may be difficult.
4. Conclusion
COVID 19 infection has many different and mysterious presentations. GI manifestations are among important, common presentations. The acute abdomen like presentation is not common but may sometimes challenging presentation for pediatrician and pediatric surgeon. Other different complications like intussusception, pneumatosis intestinalis and protein losing enteropathy are rare but knowledge about these presentations assist physician to be aware and make decision accurately.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgements
‘Not Applicable’.
Abbreviation
- Angiotensin converting enzyme 2
ACE 2
- Nothing per os
NPO
- Oral rehydration solution
ORS
- Severe acute respiratory syndrome corona virus 2
SARS- CoV-2, COVID 19
- Total parenteral nutrition
TPN
- Transmembrane protease serine 2
TMPRSS2
Ethics approval, consent to participate or consent for publication
This study was approved by ethics committee of Shahid Beheshti University of Medical Sciences. Written informed consent was obtained from the children's parents (father) for the publication of this case report, including any data contained within.
Authors contributions
RP: Major contributor in writing the manuscript. Pediatric gastroenterologist who managed patient in GI ward.
KA: Professor who managed children in COVID 19 infection ward.
RTS: Professor who managed children in COVID 19 infection ward.
MK: Radiologist who diagnosed pneumatosis intestinalis.
SAK: Minor contributor in writing the manuscript. Pediatric gastroenterologist who managed patient in GI ward.
TG: Pediatric resident who managed children. Minor contributor in writing the manuscript.
Funding
“No funding was obtained for this study”.
Availability of data and materials
All data generated during this study are included in this publication [and its supplementary information files].
References
- 1.Tian Y., Rong L., Nian W. Review article: gastrointestinal features in COVID-19 and the possibility of faecal transmission. Aliment Pharmacol Ther. 2020;51:843–851. doi: 10.1111/apt.15731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Akobeng AK, Grafton-Clarke C, Abdelgadir I, et al Gastrointestinal manifestations of COVID-19 in children: a systematic review and meta-analysis. Frontline Gastroenterology Epub ahead of print: August 6, 2020. doi:10.1136/flgastro-2020-101529. [DOI] [PMC free article] [PubMed]
- 3.Hoffmann M., Kleine-Weber H., Schroeder S. SARS-CoV-2 cell entry depends on ACE2 and TMPRSS2 and is blocked by a clinically proven protease inhibitor. Cell. 2020;181:271–280. doi: 10.1016/j.cell.2020.02.052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hashimoto T., Perlot T., Rehman A. ACE2 links amino acid malnutrition to microbial ecology and intestinal inflammation. Nature. 2012;487:477–481. doi: 10.1038/nature11228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mandal A, Konala VM, Adapa S et al Gastrointestinal manifestations in COVID-19 Infection and its practical applications. Cureus 12(6): e8750. DOI 10.7759/cureus.8750. [DOI] [PMC free article] [PubMed]
- 6.Xiong X, Wong KK, Chi S, et al Comparative study of the clinical characteristics and epidemiological trend of 244 COVID-19 infected children with or without GI symptoms. Gut Epub ahead of print: 14 may 2020. doi:10.1136/gutjnl-2020-321486. [DOI] [PubMed]
- 7.Calinescu A.M., Vidal I., Grazioli S. 2020. Beware of too aggressive approach in children with acute abdomen during COVID-19 outbreak: ann Surg. publish ahead of print 10.1097/SLA.0000000000004100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Tullie L., Ford K., Bisharat M. Gastrointestinal features in children with COVID-19: an observation of varied presentation in eight children. Lancet. 2020;4:e19–20. doi: 10.1016/S2352-4642(20)30165-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Suwanwongse K, Shabarek N. Pseudo-Appendicitis in an adolescent with COVID-19: Cureus 12(7): e9394. DOI 10.7759/cureus.9394. [DOI] [PMC free article] [PubMed]
- 10.Ekbatani M.S., Hassani S.A., Tahernia L. Atypical and novel presentations of Coronavirus Disease 2019: a case series of three children. Br J Biomed Sci. 2020 doi: 10.1080/09674845.2020.1785102. [DOI] [PubMed] [Google Scholar]
- 11.Saeed U., Sellevoll H.B., Young V.S., Sandbaek G., Glomsaker T., Mala T. Covid-19 may present with acute abdominal pain. Br J Surg. 2020;107:186–187. doi: 10.1002/bjs.11674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gahide G., Frandon J., Vendrell J.F. COVID-19 patients presenting with afebrile acute abdominal pain. Clin Med. 2020;20:e4–e6. doi: 10.7861/clinmed.2020-0150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ahmed A.O.E., Badawi M., Ahmed K., Mohamed M.F.H. Case report: COVID-19 masquerading as an acute surgical abdomen [Epub ahead of print] Am J Trop Med Hyg. 2020 doi: 10.4269/ajtmh.20-0559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Effenberger M, Grabherr F, Mayr L, et al Faecal calprotectin indicates intestinal inflammation in COVID-19. Gut Epub ahead of print: 13 April 2020. doi:10.1136/gutjnl-2020-321388. [DOI] [PMC free article] [PubMed]
- 15.Cai X., Ma Y., Li S., Chen Y., Rong Z., Li W. Clinical characteristics of 5 COVID-19 cases with non-respiratory symptoms as the first manifestation in children. Front Pediatr. 2020;8:1–9. doi: 10.3389/fped.2020.00258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Moazzam Z., Salim A., Ashraf A. Intussusception in an infant as a manifestation of COVID-19. JPS case reports. 2020;59:101533. doi: 10.1016/j.epsc.2020.101533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lakshmanan S., Toubia N. Pneumatosis intestinalis in COVID-19. Clin Gastroenterol Hepatol. 2020 May 30 doi: 10.1016/j.cgh.2020.05.048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Meini S., Zini C., Passaleva M.T. Pneumatosis intestinalis in COVID-19 BMJ open. Gastroenterology. 2020;7 doi: 10.1136/bmjgast-2020-000434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Braamskamp M.J., Dolman K.M., Tabbers M.M. Clinical practice. Protein‐losing enteropathy in children. Eur J Pediatr. 2010;169:1179–1185. doi: 10.1007/s00431-010-1235-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Li X., Zeng W., Li X. CT imaging changes of corona virus disease 2019 (COVID-19): a multi-center study in Southwest China. J Transl Med. 2020;18:154. doi: 10.1186/s12967-020-02324-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data generated during this study are included in this publication [and its supplementary information files].