Abstract
Objectives
To evaluate whether the increase of temperature can influence the environmental endurance of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2).
Methods
Virus was inoculated on a plastic surface and harvested at predefined time-points in parallel at 20°C–25°C (room temperature; RT) and at 28°C (June temperature; JT). Samples were tested by TCID50 titres on Vero cells.
Results
Our results confirm that fomite transmission of the emerging SARS-CoV-2 is possible: the virus reserved its ability to infect cells for up to 84 hours at both RT and JT on a plastic surface, with TCID50 viral titres of 0.67 and 0.25 log10, respectively. At RT, an important reduction in the viral titre, from 4 log10 to 3 log10 TCID50, was observed during the first 24–36 hours. At JT, the same decay was observed more rapidly (between 8 and 12 hours), The rate of viral inactivation by D-value was 24.74 hours at RT and 12.21 hours at JT.
Conclusions
This remarkable difference between the two temperatures suggests that virus vitality can be influenced by the environmental temperature and that the hot season could reduce the probability of COVID-19 transmission.
Keywords: Coronavirus disease 2019, Infectious disease, Outbreak, Severe acute respiratory syndrome coronavirus 2, Temperature, Viral spread, Viral stability
Introduction
The coronavirus disease 2019 (COVID-19) pandemic has been caused by the enveloped betacoronavirus severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), transmitted from person to person through respiratory droplets and direct contact, and potentially by indirect contact through fomites [1].
Several studies have shown that viral spread could be influenced by climatic conditions as enveloped viruses tend to reduce their circulation in summer because of high temperature and solar radiation [2,3]. Indeed, the current spread of COVID-19 along the equator and tropics was shown to be significantly less [4], leading to the hypothesis that increase of temperature will influence the environmental endurance of SARS-CoV-2.
In an attempt to predict the epidemic dynamic of COVID-19 during the summer months, we tested the environmental stability of SARS-CoV-2 in parallel at room temperature (RT, 20°C–25°C) and at an average maximum temperature for June (JT) estimated at 28°C in Italy.
Methods
The strain BetaCov/Italy/CDG1/2020|EPI ISL 412973|2020-02-20 [5] was used to test the stability of SARS-CoV-2 on a plastic surface (polypropylene). This strain had an initial viral titre of 106.8 TCID50/mL, a comparable viral load to symptomatic, asymptomatic and minimally symptomatic patients [6].
The viral preparation was spotted in droplets of 10 μL on 24-well plates and allowed to dry for 30 minutes. Then, plates were incubated at both RT and JT for 7 days at relative humidity of 35%–45% (in an air-conditioned room). The virus was harvested at 0, 4, 8, 12, 24, 36, 48, 60, 72, 84 and 96 hours by adding 1 mL/well of Eagle's minimal essential medium (EMEM) + 2% fetal calf serum (FCS) and was quantified by end-point titration on Vero cells by TCID50 (dilution of virus at which 50% of the cell cultures are infected): 96-well plates were inoculated with two-fold dilutions of each viral sample (100 μL), and 22 000 cells/well in EMEM + 2% FCS were added (100 μL). Plates were left in the incubator at 37°C with 5% CO2 for 6 days and were checked daily to observe the cytopathic effect. The 50% end-point titres were determined using the Spearman–Karber method. Both experiments were conducted in three independent replicates and the limit of detection by the end-point technique was established as 1 log10. Ethical approval was not need for this study.
Viral titres of the daily collections at 0, 24, 48 and 72 hours at RT were also determined by plaque assay in Vero E6 cells. Briefly, 12-well plates were plated with Vero E6 cells (150 000/well in EMEM + 10% FCS) and inoculated with logarithmic dilutions of each sample. Plates were incubated for 1 hour at 37°C, and 4 mL/well of a medium containing 2% Gum Tragacanth + EMEM +2.5% FCS was added. After 5 days at 37°C with 5% CO2, titres were calculated using crystal violet dye in plaque-forming units per milliliter. All the experimental procedures were conducted under biosafety level 3 conditions.
To approximate a normal distribution, the viral titre of each well was log-transformed. Using standard deviation with a 95% confidence interval, the results mostly followed a normal distribution of a set value. The ratio of the standard deviation to the mean was investigated by calculating the coefficient of variance.
Results
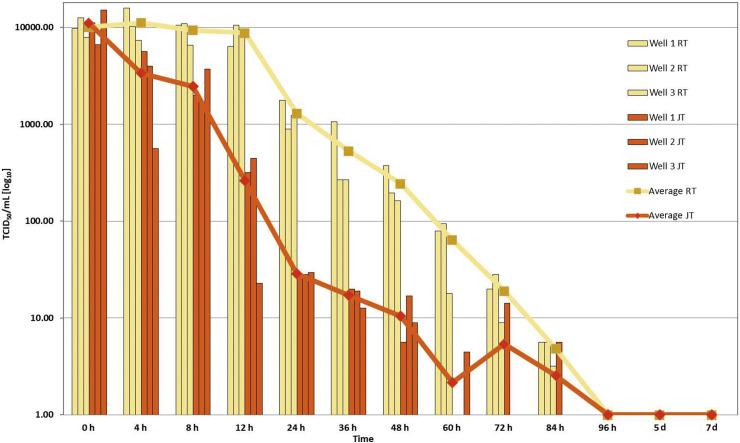
Analysis of data obtained by TCID50 titration showed that an important reduction in the viral titre, from 4 log10 to 3 log10 TCID50/mL of medium, was observed during the first 24–36 hours at RT (Fig. 1 ) with a D-value of 24.74 hours. This trend was confirmed by titration by plaque assay (see Supplementary material, Figs S1–S4 and Table S1).
Fig. 1.
Relation between viral titre (determined by 50% end-point titration; TCID50) and time of collection in logarithmic scale. Average viral titres in samples collected at either room temperature (RT) or June temperature (JT) are plotted as a function of time-points after infection.
At JT, the same decay was observed more rapidly (between 8 and 12 hours), indicating that viral infectivity can be influenced by higher temperature with a D-value of 12.21 hours.
This decay trend continued until 84 hours, showing a remarkable difference between the two temperatures. In both the experimental conditions, the virus was no longer detectable at 96 hours.
Discussion
The present study confirms that fomite transmission of the emerging SARS-CoV-2 is possible [7], because the virus remained viable on plastic surfaces for up to 84 hours at both RT and JT. In both experimental conditions, the virus was not detectable at 96 hours. End-point titration showed that the virus infectivity on a plastic surface rapidly declined during the first 24–36 hours at RT and there was a remarkable difference between the two temperatures.
Contaminated surfaces are reported to be significant vectors in the transmission of infections and survival of viruses on a variety of fomites has been demonstrated for other coronaviruses, influenza viruses, paramyxoviruses, poxviruses and retroviruses [[8], [9], [10]].
The results of this study support the hypothesis that during the hot season the increase of temperature may influence the environmental endurance of SARS-CoV-2 and reduce the probability of virus transmission. The main limitation of this study is the small number of temperatures tested, which does not allow accurate evaluation of the influence of environmental temperature on virus stability. Moreover, we cannot establish at what times and temperatures viral transmission is no longer possible because we do not know the minimum infectious dose of SARS-CoV-2.
In conclusion, the increase of temperature observed in summer may influence the environmental endurance of SARS-CoV-2 but this does not influence the need to maintain social distancing measures.
Transparency declaration
The authors declare no competing interests.
Funding
No external funding was received.
Authors' contributions
MF conceived and designed the study; MF, BM and MA performed the experiments; MF, BM and NL analysed the data; MF and BM wrote the manuscript, and NL and RG critically revised the manuscript.
COVID-19 study group
In addition to the authors, the COVID-19 Study Group consisted of: Eleonora Benedetti, Concetta Fabiani, Stefano Fiore, Maedeh Kojouri, Paola Bucci, Emilio D'Ugo and Silvia Gioacchini.
Acknowledgements
The authors wish to thank Dr Paola Stefanelli for providing the virus SARS-CoV-2 BetaCov/Italy/CDG1/2020|EPI ISL 412973|2020-02-20 and Alessia Caratelli, Ambrogio Carlei, Marina Sbattella and Eugenio Sorrentino for their technical support.
Editor: Laurent Kaiser
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.cmi.2020.10.034.
Contributor Information
COVID-19 Study Group:
Benedetti Eleonora, Fabiani Concetta, Fiore Stefano, Kojouri Maedeh, Bucci Paola, D'Ugo Emilio, and Gioacchini Silvia
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- 1.World Health Organization . WHO Scientific brief; Geneva: 2020. Modes of transmission of virus causing COVID-19: implications for IPC precaution recommendations. WHO. [Google Scholar]
- 2.Price R.H.M., Graham C., Ramalingam S. Association between viral seasonality and meteorological factors. Sci Rep. 2019;9:929. doi: 10.1038/s41598-018-37481-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gundy P.M., Gerba C.P., Pepper I.L. Survival of coronaviruses in water and wastewater. Food Environ Virol. 2009;1:10. [Google Scholar]
- 4.Dong E., Du H., Gardner L. An interactive web-based dashboard to track COVID-19 in real time. Lancet Infect Dis. 2020 doi: 10.1016/S1473-3099(20)30120-1. https://coronavirus.jhu.edu/map.html [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Stefanelli P., Faggioni G., Lo Presti A., Fiore S., Marchi A., Benedetti E. On behalf of ISS COVID-19 study group. Whole genome and phylogenetic analysis of two SARS-CoV-2 strains isolated in Italy in January and February 2020: additional clues on multiple introductions and further circulation in Europe. Euro Surveill. 2020;25:2000305. doi: 10.2807/1560-7917.ES.2020.25.13.2000305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Zheng S., Fan J., Yu F., Feng B., Lou B., Zou Q. Viral load dynamics and disease severity in patients infected with SARS-CoV-2 in Zhejiang province, China, January–March 2020: retrospective cohort study. BMJ. 2020;369:m1443. doi: 10.1136/bmj.m1443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Van Doremalen N., Bushmaker T., Morris D.H., Holbrook M.G., Gamble A., Williamson B.N. Aerosol and surface stability of SARS-CoV-2 as compared with SARS-CoV-1. N Engl J Med. 2020;382:1564–1567. doi: 10.1056/NEJMc2004973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hall C.B., Douglas R.G., Geiman J.M. Possible transmission by fomites of respiratory syncytial virus. J Infect Dis. 1980;141:98–102. doi: 10.1093/infdis/141.1.98. [DOI] [PubMed] [Google Scholar]
- 9.Pirtle E.C., Beran G.W. Virus survival in the environment. OIE Rev Sci Techn. 1991;10:733–748. doi: 10.20506/rst.10.3.570. [DOI] [PubMed] [Google Scholar]
- 10.Aboubakr H.A., Sharafeldin T.A., Goyal S.M. Stability of SARS-CoV-2 and other coronaviruses in the environment and on common touch surfaces and the influence of climatic conditions: a review. Transbound Emerg Dis. 2020 doi: 10.1111/tbed.13707. ePub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.