Abstract
The universal phenomenon of blood clotting is well known to be protective in external cellular/ tissue injury. However, the emergence of unusual thrombotic presentations in COVID-19 patients is the real concern. Interaction of the spike glycoprotein with ACE2 receptor present in the host cell surface mediates the entry of SARS-CoV-2 causing COVID-19 infection. New clinical findings of SARS-CoV-2 pathogenesis are coming out every day, and one such mystery is the formation of mysterious blood clots in the various tissues and organs of COVID-19 patients, which needs critical attention. To address this issue, we hypothesis that, high ACE2 expression in the endothelium of blood vessels facilitates the high-affinity binding of SARS-CoV-2 using spike protein, causing infection and internal injury inside the vascular wall of blood vessels. This viral associated injury may directly/indirectly initiate activation of coagulation and clotting cascades forming internal blood clots. However, the presence of these clots is undesirable as they are responsible for thrombosis and need to be treated with anti-thrombotic intervention.
Background
Coronavirus Disease (COVID-19), since its emergence from Wuhan province, China in December 2019, now spreading to 213 countries worldwide, forcing the World health organization to declare this outbreak a global pandemic on 11 March 2020 [1]. COVID-19 is caused by highly infectious, severe acute respiratory syndrome coronavirus (SARS-CoV-2), infecting more than 36 million individuals, with 1,060,563 reported deaths as of 8 October 2020 [2]. The understanding of this novel virus and disease evolves sequentially in the past seven months. Initially, thought to transmit by droplets or aerosols causing fever as classical clinical symptoms, mainly in old age or immunocompromised individuals. However, the dynamics of COVID-19 keeps on evolving with the emergence of different SARS-CoV-2 strains. Evidence of airborne mode of SARS-CoV-2 transmission [3], asymptomatic clinical presentations along with extra-pulmonary manifestations [4] are the real concern.
SARS-CoV-2 is a single-stranded, positive-sense RNA virus having envelope, glycoprotein, and spike protein. Being a respiratory virus, SARS-CoV-2 enters inside the human body and infect the lungs as a primary and predominant organ [5]. The entry is mediated by the binding of the receptor-binding domain (RBD) of the S1 subunit of the viral spike protein with the host angiotensin-converting enzyme 2, (ACE2) receptor primarily expressed in the type II pneumocytes, serving as a viral reservoir [6], [7]. Usually, COVID-19 presented with fever, sore throat, dry cough, and shortness of breath as common clinical manifestations [8], however asymptomatic cases are also being reported which are more critical to diagnose. ACE2 is also found to be expressed in the oral, nasal mucosa, epithelial cells of lungs, kidney, and heart, enterocytes of the small intestine, and in the endothelial cells of blood vessels [9]. The SARS-COV-2 associated extra-pulmonary manifestations are encephalitis, rashes on the skin, meningitis, conjunctivitis, acute hepatic, and renal injury.
Surprisingly, autopsies of COVID-19 patients have revealed clots in the small vessels of the lungs, heart, liver, and kidney which are responsible for strokes and heart attacks [10]. More than 33% of critical COVID-19 patients’ are reported with critically high levels of blood clotting or elevated levels of D-dimer [11]. The development of these mysterious clots causing coagulation abnormalities and thrombosis is the real concern and needs to be addressed. So, we hypothesis the possible mechanism for the formation of the vascular blood clots in COVID-19 patients.
Origin of hypothesis
The hypothesis for the formation of blood clots in the vessels is retrieved from the classical concept of blood clotting. The mechanism of blood clotting is like a two-edged sword, wherein the case of severe external injury, clotting is very crucial for preventing the blood loss, whereas, in the case of internal blood vessels injury, it, unfortunately, leads to the formation of blood clots, causing vascular blockades and thrombosis, expanding to every organ leading to severe and fatal outcomes.
The above concept is substantiated by the following three facts:
-
)a)
Recognition of ACE2 receptor-expressing endothelial cells of the blood vessels by spike protein of SRAS-CoV-2.
-
)b)
Direct injury to the endothelial cell by SARS-CoV-2 infection resulting in vascular damage.
-
)c)
Indirect damage due to immune-mediated cytokine release syndrome (CRS) causing inflammation and cell death.
To protect the direct and/or indirect damage caused by SARS-CoV-2 to endothelial cells lining the blood vessels, host innate defensive mechanism of blood clotting activates, recruiting the activated platelets at the injury site to form a clot which although reduce the damage but negatively may lead to obstruction of blood vessels and vasoconstriction causing more damage.
The virus enters into the peripheral blood causing viremia and gets transmitted to the different organs such as the heart, kidney, gastrointestinal tract resulting in multiple organ failure. As it is evident that blood clots were observed in both live and dead COVID-19 patients, so it is out most interesting to decode the mystery.
Hypothesis statement
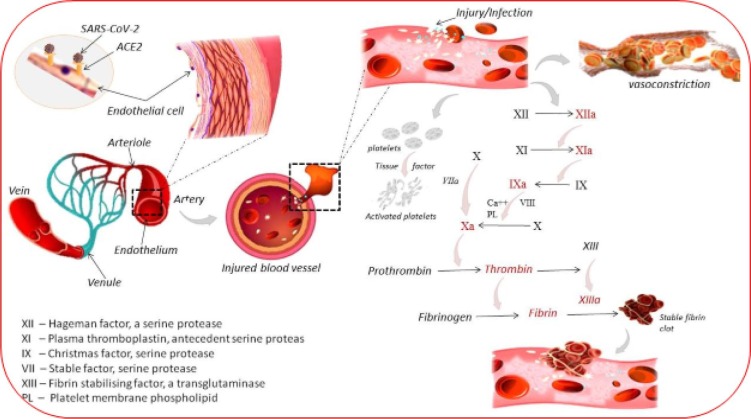
Considering the above facts and recent unusual reports, a hypothesis develops for the blood clots formation in the COVID-19 patients (Fig. 1 ), states that “Due to an internal injury in the endothelium of blood vessels, either directly by SARS-CoV-2 infection (co-expression and binding of the spike protein with the ACE2) or my virus-mediated inflammatory immune response, may result in vasoconstriction and the activation of coagulation and blood clotting pathways, resulting in the formation of blood clots”.
Fig. 1.
Schematic representation showing the mechanism of clot formation in the blood vessels when the endothelial cells rich in ACE2 receptors are targeted by SARS-CoV-2 and resulted in the internal blood vessel injury, resulting in the cascade of blood clot formation.
Theoretical evaluation and validation
During COVID-19 infection, SARS-CoV-2 enters into the systemic circulation and binds with the ACE2 expressing endothelial cells (endothelium) lining the blood vessels. Binding facilitates the virus internalization, causing infection and injury in the vascular wall of blood vessels. The vascular injury might result in vasoconstriction, which may further reduce the blood flow at the site of injury. Also, injury to endothelial cells reduces the expression of fibrinolytic heparin and thrombomodulin. Conversely, high expression and secretion of the Von Willebrand factor enhance the aggregation of platelets at the site of injury in blood vessels and activate the coagulation cascade for the formation of blood clots.
Immediately within a few seconds of endothelial cells injury in a blood vessel, platelets along with collagen, recruit at the injury site to swell and aggregate. Soon the coagulation is initiated and fibrin strands begin to intersperse among the wound to form a complete platelet plug. Viruses like Dengue and Herpes simplex virus (HSV) are known to infect endothelial and circulating blood cells, activating coagulation cascade by promoting tissue factor [12]. Interestingly, lysis of fibrin known as fibrinolysis by fibrinolytic molecule plasminogen and plasmin proved to induce deleterious inflammation and defective fibrin clot formation in Influenza A viruses (IAV) [13]. In addition to viral stimulation, binding of an extracellular proteolytic enzyme known as urokinase-type plasminogen activator (uPA) with its receptor, uPAR is crucial for the activation of plasminogen to plasmin as reported in various malignancies [14]. Detrimental inflammation in the endothelial cells may initiate the cascade of cytokine release and subsequently leads to the blood vessel injury.
Similarly, the SARS-CoV-2 induced vascular trauma/injury, activates the platelets exposed endothelium or collagen following the intrinsic pathway. Following the injury to blood vessels, near-by platelets stick to the vascular proteins, get degranulated, releasing prothrombin activator, serotonin, adenosine diphosphate (ADP), and thromboxane A2 for further activation of platelets. The mechanism for the formation of clots in the blood vessels may start sequentially by 12 clotting factors, i.e. activating the factor XII, converting prothrombin to thrombin and later fibrinogen to long and insoluble fibrin which may entangle with platelets by covalent cross-linking, forming a stable interlocking fibrous network of a fibrin clot at the site of injury. This may slow down the blood flow, but platelets in the clot begin to shrink to initiate the wound healing process with intrinsic and extrinsic coagulation pathways. However, the upregulation of the expression of fibrinogen subunits FGA, FGB, and FGG also plays a very significant role in the formation of the clot. Various thrombotic complications and coagulation abnormalities are associated with COVID-19 like sepsis-induced coagulopathy (SIC), disseminated intravascular coagulation (DIC), venous thromboembolism (VTE), pulmonary embolism (PE), micro-thrombosis, microvascular thrombosis, and thrombotic micro-angiopathy. Intense endothelial inflammation may be the involved mechanism leading to microvascular thrombosis as suggested in lung pathology contributing to ARDS [15]. SIC is hypercoagulability, characterized by elevated fibrinogen and D-dimer levels causing endothelial dysfunction, micro-thrombosis, and stroke [16].
Additionally, vasoconstriction has an inverse relation with ACE2. During systemic infection, the ACE2 expressed blood vessels’ endothelial cells, might attach to the viral spike protein resulting in the unavailability of ACE2. Renin-angiotensin-aldosterone system (RAAS) may drive the formation of micro-thrombin in COVID-19 patients stimulating Angiotensin II (Ag II) to induce tissue factor (TF) and plasminogen activator inhibitor-1 (PAI-1) expression by endothelial cells. Ag II acts on the CNS to increase vasopressin production which causes vasoconstriction. Depletion of ACE2 by SARS-CoV-2, PAI-1/tPA imbalance, and a hyper-coagulable state may favor tissue injury and stroke [17]. This may explain the unresolved mystery of unresolved fibrin deposits in the alveoli of patients with general ARDS [18].
ACE2 converts Ag II to Ag (1–7), protecting endothelial cell function and prevent early atherosclerosis which can be caused by a clot in the blood vessels [19]. Profound hypoxemia in the pulmonary capillaries may result in the activation of hypoxia-inducible factors (HIFs) resulting in inducing or inhibition of TF and PAI-1 respectively, and vasoconstriction thereby promoting vascular occlusion [20], [21], [22].
The deposition of the C56-9 component of the complement system in the damaged vessel results in micro thrombosis as an anti-phospholipid syndrome [23]. Neutrophil extracellular traps (NET) are associated with elevated levels of histones, activating increased thrombin production [24]. In a study including 362 closed COVID-19 cases from Italy, high mortality attributed to pulmonary embolism (PE) and pulmonary thrombosis with VTE and ischemic stroke as primary and DIC as a secondary outcome. Thromboembolic events occurred in 28 (7.7%) cases, with VTE in 16 (36%), PE in 10 (33%) and, DIC in 8 (2.2%) patients [25]. High-risk coagulation abnormalities are associated with an elevated concentration of D-dimer and a reduction in platelet count [11]. Thrombotic microangiopathy in the lungs autopsies showing aggregates of CD4 around thrombosed small vessels and are significantly associated with hemorrhage. [26]. VTE may develop via immunologic activation of intravascular and platelet-releases thrombin. Severe derangement of hemostasis, accompanied by reduced platelet count and fibrinogen, may explain the events of venous thromboembolism supporting hypercoagulability in COVID-19 positive patients [27]. Incidence of VT increase between 25% and 49% in severe COVID-19 patients, with pulmonary embolism being the most common thrombotic complication [28], [29]. Microvascular thrombotic complications are indicative of a strong interaction between the SARS-CoV-2 and coagulation. More than 80% of lung autopsies reported platelet–fibrin thrombi, especially in the small pulmonary vasculature [30]. The presence of antiphospholipid antibodies is a serious complication causing thrombotic stroke in young patients [31].
SO, in COVID-19 patients, the SARS-CoV-2 mediated endothelial inflammation, thrombin generation, platelet, and leukocyte recruitment, complement activation, and the initiation of innate and adaptive immune responses, forming clots, culminate in immunothrombosis, ultimately resulting in thrombotic complications, stroke, and finally death.
Discussion & conclusion
Based on the literature and clinical observation of mysterious clots reported in the COVID-19 patients, expression of ACE2 in the endothelium of blood vessels, blood clotting pathways, interaction of the SARS-CoV-2 spike protein with host ACE2, the pathogenesis of SARS-CoV-2, and the role of ACE2 in RAS, we can hypothesize and end with the conclusion that the mysterious clots reported in the COVID-19 patients may be due to the binding of the spike protein of SARS-CoV-2 with the ACE2 receptor expressed in the endothelial cells of blood vessels which may cause, vasoconstriction and activation of the intrinsic pathway of coagulation and eventually results in the formation of blood clots.
CRediT authorship contribution statement
Saurav Biswas: Conceptualization, Data curation, Investigation, Methodology, Writing - original draft. Vikram Thakur: Conceptualization. Writing - original draft, Data curation, Investigation, Methodology, Resources, Software. Parneet Kaur: Writing - review & editing. Azhar Khan: Formal analysis, Investigation Validation, Visualization. Saurabh Kulshrestha: Validation, Visualization, Funding acquisition, Investigation, Project administration. Pradeep Kumar: Conceptualization, Writing - review & editing, Formal analysis, Investigation, Validation, Visualization, Resources, Supervision.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgment
Special thanks to Prof. Prem Kumar Khosla, Vice-Chancellor, Shoolini University, Solan for providing financial support and necessary facilities.
References
- 1.Cucinotta D., Vanelli M. ‘WHO declares COVID-19 a pandemic’, Acta Biomedica. Mattioli. 2020;1885:157–160. doi: 10.23750/abm.v91i1.9397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Worldometer (2020) ‘Coronavirus Cases’, Worldometer, pp. 1–22. doi: 10.1101/2020.01.23.20018549V2.
- 3.Klompas M., Baker M.A., Rhee C. Airborne Transmission of SARS-CoV-2: Theoretical Considerations and Available Evidence. JAMA - Journal of the American Medical Association. American Medical Association. 2020:441–442. doi: 10.1001/jama.2020.12458. [DOI] [PubMed] [Google Scholar]
- 4.Gupta A. ‘Extrapulmonary manifestations of COVID-19’, Nature Medicine. Nature Research. 2020:1017–1032. doi: 10.1038/s41591-020-0968-3. [DOI] [PubMed] [Google Scholar]
- 5.Jain A. ‘COVID-19 and lung pathology’, Indian Journal of Pathology and Microbiology. Wolters Kluwer Medknow Publications. 2020;63(2):171. doi: 10.4103/IJPM.IJPM_280_20. [DOI] [PubMed] [Google Scholar]
- 6.Hoffmann M. SARS-CoV-2 Cell Entry Depends on ACE2 and TMPRSS2 and Is Blocked by a Clinically Proven Protease Inhibitor. Cell. Cell Press. 2020;181(2):271–280.e8. doi: 10.1016/j.cell.2020.02.052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lin L. ‘Hypothesis for potential pathogenesis of SARS-CoV-2 infection–a review of immune changes in patients with viral pneumonia’, Emerging Microbes and Infections. Taylor and Francis Ltd. 2020:727–732. doi: 10.1080/22221751.2020.1746199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kakodkar P., Kaka N., Baig M. A Comprehensive Literature Review on the Clinical Presentation, and Management of the Pandemic Coronavirus Disease 2019 (COVID-19) Cureus. Cureus, Inc. 2020;12(4) doi: 10.7759/cureus.7560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hamming I. Tissue distribution of ACE2 protein, the functional receptor for SARS coronavirus. A first step in understanding SARS pathogenesis. Journal of Pathology. 2004;203(2):631–637. doi: 10.1002/path.1570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Tang N. ‘Abnormal coagulation parameters are associated with poor prognosis in patients with novel coronavirus pneumonia’, Journal of Thrombosis and Haemostasis. Blackwell Publishing Ltd. 2020;18(4):844–847. doi: 10.1111/jth.14768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Levi M. Coagulation abnormalities and thrombosis in patients with COVID-19. The Lancet Haematology. Elsevier Ltd. 2020:e438–e440. doi: 10.1016/S2352-3026(20)30145-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Antoniak S., MacKman N. Multiple roles of the coagulation protease cascade during virus infection. Blood. American Society of Hematology. 2014;123(17):2605–2613. doi: 10.1182/blood-2013-09-526277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Berri F. ‘Plasminogen Controls Inflammation and Pathogenesis of Influenza Virus Infections via Fibrinolysis’, PLoS Pathogens. Edited by A. Pekosz. Public Library of Science. 2013;9(3) doi: 10.1371/journal.ppat.1003229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mahmood N., Mihalcioiu C., Rabbani S.A. Multifaceted role of the urokinase-type plasminogen activator (uPA) and its receptor (uPAR): Diagnostic, prognostic, and therapeutic applications. Front Oncol. Frontiers Media S.A. 2018:24. doi: 10.3389/fonc.2018.00024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wang J. ‘Tissue plasminogen activator (tPA) treatment for COVID-19 associated acute respiratory distress syndrome (ARDS): A case series’, Journal of Thrombosis and Haemostasis. Blackwell Publishing Ltd. 2020;18(7):1752–1755. doi: 10.1111/jth.14828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Iba T. Diagnosis and management of sepsis-induced coagulopathy and disseminated intravascular coagulation. J Thromb Haemost. 2019;17(11):1989–1994. doi: 10.1111/jth.14578. Blackwell Publishing Ltd. [DOI] [PubMed] [Google Scholar]
- 17.Hess D.C., Eldahshan W., Rutkowski E. COVID-19-Related Stroke. Translational Stroke Research. 2020:322–325. doi: 10.1007/s12975-020-00818-9. Springer. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Vaughan D.E., Lazos S.A., Tong K. ‘Angiotensin II Regulates the Expression of Plasminogen Activator Inhibitor-1 in Cultured Endothelial Cells: A Potential Link between the Renin-Angiotensin System and Thrombosis’, Journal of Clinical Investigation. The American Society for Clinical Investigation. 1995;95(3):995–1001. doi: 10.1172/JCI117809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Zhang Y.H. ACE2 and Ang-(1–7) protect endothelial cell function and prevent early atherosclerosis by inhibiting inflammatory response. Inflamm Res. Birkhauser Verlag AG. 2015;64(3–4):253–260. doi: 10.1007/s00011-015-0805-1. [DOI] [PubMed] [Google Scholar]
- 20.Yan, S. F. et al. (1999) ‘Hypoxia/hypoxemia-induced activation of the procoagulant pathways and the pathogenesis of ischemia-associated thrombosis’, Arteriosclerosis, Thrombosis, and Vascular Biology. Lippincott Williams and Wilkins, pp. 2029–2035. doi: 10.1161/01.ATV.19.9.2029. [DOI] [PubMed]
- 21.Gupta N., Zhao Y.Y., Evans C.E. The stimulation of thrombosis by hypoxia. Thromb Res. Elsevier Ltd. 2019:77–83. doi: 10.1016/j.thromres.2019.07.013. [DOI] [PubMed] [Google Scholar]
- 22.Grimmer B., Kuebler W.M. The endothelium in hypoxic pulmonary vasoconstriction. J Appl Physiol. American Physiological Society. 2017:1635–1646. doi: 10.1152/japplphysiol.00120.2017. [DOI] [PubMed] [Google Scholar]
- 23.Magro, C. et al. (2020) ‘Complement associated microvascular injury and thrombosis in the pathogenesis of severe COVID-19 infection: A report of five cases’, Translational Research. Mosby Inc., 220, pp. 1–13. doi: 10.1016/j.trsl.2020.04.007. [DOI] [PMC free article] [PubMed]
- 24.Barnes, B. J. et al. (2020) ‘Targeting potential drivers of COVID-19: Neutrophil extracellular traps’, Journal of Experimental Medicine. Rockefeller University Press. doi: 10.1084/jem.20200652. [DOI] [PMC free article] [PubMed]
- 25.Lodigiani C. ‘Venous and arterial thromboembolic complications in COVID-19 patients admitted to an academic hospital in Milan, Italy’, Thrombosis Research. Elsevier Ltd. 2020;191:9–14. doi: 10.1016/j.thromres.2020.04.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Fox, S. et al. (2020) ‘Pulmonary and Cardiac Pathology in Covid-19: The First Autopsy Series from New Orleans’, medRxiv. Cold Spring Harbor Laboratory Press, p. 2020.04.06.20050575. doi: 10.1101/2020.04.06.20050575.
- 27.Panigada M. ‘Hypercoagulability of COVID-19 patients in intensive care unit: A report of thromboelastography findings and other parameters of hemostasis’, Journal of Thrombosis and Haemostasis. Blackwell Publishing Ltd. 2020;18(7):1738–1742. doi: 10.1111/jth.14850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Cui S. ‘Prevalence of venous thromboembolism in patients with severe novel coronavirus pneumonia’, Journal of Thrombosis and Haemostasis. Blackwell Publishing Ltd. 2020;18(6):1421–1424. doi: 10.1111/jth.14830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Klok F.A. ‘Confirmation of the high cumulative incidence of thrombotic complications in critically ill ICU patients with COVID-19: An updated analysis. Thrombosis Research Elsevier Ltd. 2020;191:148–150. doi: 10.1016/j.thromres.2020.04.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Carsana L. Pulmonary Post-Mortem Findings in a Large Series of COVID-19 Cases from Northern Italy. SSRN Electronic Journal. 2020 doi: 10.1101/2020.04.19.20054262. Cold Spring Harbor Laboratory Press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Zhang Y. Coagulopathy and Antiphospholipid Antibodies in Patients with Covid-19. N Engl J Med Massachussetts Medical Society. 2020;382(17) doi: 10.1056/NEJMc2007575. [DOI] [PMC free article] [PubMed] [Google Scholar]