Latin America became the epicenter of the coronavirus disease 2019 (COVID-19) pandemic. Although the United States still leads the world in the number of diagnosed cases (6,204,000) and reported deaths (187,000), as of September 5, 2020, Brazil (4,092,000 cases and 123,500 deaths) was second behind the United States in both infections and deaths.1 The leading affected countries contributing in both infections and deaths, respectively, are Peru (n = 683,700 and n = 29,680); Chile (n = 420,400 and n = 11,500); Mexico (n = 629,400 and n = 67,300); Colombia (n = 658,450 and n = 21,100); Ecuador (n = 118,045 and n = 6700); Argentina (n = 451,100 and n = 9400); and Bolivia (n = 119,500 and n = 5300). In this study, we describe the clinical characteristics, mortality, and symptoms of the confirmed COVID-19 cases officially registered by countries that make pertinent information publicly available, with special emphasis on gastrointestinal symptoms (GI) and comorbidities in relation to disease outcome.
Methods
We analyzed data from severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2)–positive patients evaluated at health care centers and hospitals in 8 Latin American countries (Brazil, Peru, Mexico, Argentina, Colombia, Venezuela, Ecuador, and Bolivia) between March 1 and July 30, 2020. These countries comprise a population that exceeds 519 million. Demographics, comorbidities, and clinical symptoms were collected. The total cohort consisted of 728,282 patients. Common symptoms and comorbidities were combined and evaluated by weighted analysis methods. Correlation coefficients were calculated together with regression analysis to establish associations between comorbidities and lethality. The effect of symptoms was reported using weighted analysis. SPSS software (IBM Corp) was used for this analysis.
Results
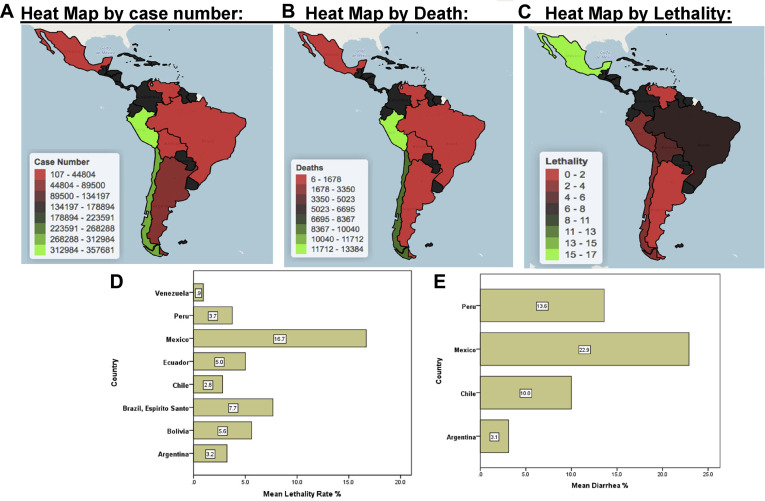
A total of 728,282 patients tested positive for COVID-19 across all 8 Latin American countries. Of these patients, 52.6% were female. Mean age was 48.4 years. Peru had the oldest cohort (mean age, 56.8 years) and highest rate of female patients (56.8%), and Chile had the youngest cohort (mean age, 39 years). Venezuela had the highest male prevalence (56.7%). The most common symptoms were cough (60.1%; Bolivia had the highest rate with 78%), fatigue or tiredness (52.0%), sore throat (50.3%), and fever (44.2%). Bolivia had fever as the top symptom (83.3%). GI symptoms, including diarrhea (highest in Mexico with 22.9%) (Figure 1 ), nausea, vomiting, and abdominal pain, were not associated with higher mortality. The collective death toll was 25,008 patients (3.4%). Hypertension was among the top comorbidities (12.1%), followed by diabetes (8.3%) and obesity (4.5%). In multivariable analyses, the leading and significant comorbidities were hypertension (r = 0.83; P = .02), diabetes (r = 0.91; P = .01), and obesity (r = 0.86; P = .03). Asthma (r = 0.37; P = .54) and increasing age (r = 0.13; P = .81) were not independently associated with higher mortality. Lethality was highest in Mexico (16.6%) and lowest in Venezuela (0.9%) among the analyzed cohorts (Figure 1).
Figure 1.
Latin America heatmap for case number (A), death (B), and lethality rate (C), and comparison of mean lethality rate (D) and diarrhea prevalence (E) in selected studies from different countries.
Discussion
Our study revealed that COVID-19 manifests differently among the various regions of Latin America. These differences are important to consider because their impact can influence management, treatment, and prevention strategies. The most common symptoms are dry cough, fatigue, sore throat, and fever. The most common comorbidities are obesity, hypertension, and diabetes. This contrasts with what was reported by Maechler et al2 (common symptoms were fatigue, myalgia, and cough, and top comorbidities were chronic lung disease and chronic heart disease). In addition, these symptoms and comorbidities did not distribute similarly among the 8 nations studied. Mexico and Chile followed a similar profile for comorbidities.
The prevalence of diarrhea was much higher than reported previously.3 This is probably because a higher prevalence of diarrhea in Latin American populations existed before the SARS-CoV-2 outbreak.4 The cumulative lethality in Latin America is 3.4%, close to that reported worldwide.1 We understand that this lethality rate might be inflated compared with the actual risk of death because the people most likely to get tested for COVID-19 are those with severe symptoms, not asymptomatic or mild symptoms. Results of analysis of the impact of the top comorbidities on lethality found that obesity, hypertension, and diabetes were highly correlated with lethality.
Another pertinent element to emphasize is that the prevalence of tuberculosis in our study was >1.2%. There is a well-known high prevalence of tuberculosis in the region and use of bacille Calmette-Guerin vaccination in Latin America. Many studies reported a potential effect of the bacille Calmette-Guerin vaccine in providing heterologous protection5 against other infections, like that from SARS-CoV-2. Although the role of the bacille Calmette-Guerin vaccine is still debated, future large and well-designed comparative studies might reveal whether it played any role in the pandemic’s outcomes in Latin America.
Some of the observed differences between countries have to do with pandemic management and data availability. Venezuela, for example, showed the least lethality, which might be explained by free access to health care system and the fact that the treatment protocol includes hospitalizing every reported positive case.6 This is in contrast to other countries, such as Mexico, where only patients with severe disease are hospitalized and there is less access to advanced care available for the general population.7
Although the mechanisms of GI manifestations elicited by SARS-CoV-2 are still unknown, it is clear that angiotensin receptor 2 expression in the esophagus and small and large intestines plays a role. Angiotensin receptor 2 was reported to be co-expressed with TMPRSS2, which is needed for cleavage of the spike protein and facilitation of the virus entry into the host GI system, aggravating systemic effects of the virus and elevating rates of transmission. Although millions of patients have been discharged and tested negative in their nasopharyngeal specimens, a sizable portion still tested positive in their stools.8 This group of patients should be the focus of the next stringent monitoring methods, as they are likely to play a role in the dissemination and recurrence of the disease. It will also be worth monitoring whether SARS-CoV-2 persistence in the GI system will impact overall GI system functions.
In conclusion, approximately 10.5%–53% of patients with COVID-19 have GI manifestations. Differential clinical symptoms were associated with COVID-19 in Latin American countries. Metabolic syndrome components were the main comorbidities associated with poor outcomes. Country-specific management and prevention plans are needed.
Acknowledgments
CRediT Authorship Contributions
Hassan Ashktorab, PhD (Conceptualization: Lead; Supervision: Lead; Writing – original draft: Lead).
Antonio Pizuorno, MD (Data curation: Equal).
Gholamreza Oskrochi, PhD (Formal analysis: Lead).
Nora Alma Fierro González, MD, PhD (Data curation: Equal; Resources: Equal).
Zaki A. Sherif, PhD (Writing – review & editing: Equal).
Hassan Brim, PhD (Writing – review & editing: Equal).
Footnotes
Conflicts of interest The authors disclose no conflicts.
Funding This project was supported in part by the National Institute on Minority Health and Health Disparities of the National Institutes of Health under award G12MD007597. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript. Data used for this study were anonymized.
References
- 1.Johns Hopkins University. Available at: https://coronavirus.jhu.edu/map.html. Accessed December 9, 2021.
- 2.Maechler F. Clin Microbiol Infect. 2020;26: 1685.e7–1685.e12. [Google Scholar]
- 3.Sultan S. Gastroenterology. 2020;159:320–334.e27. doi: 10.1053/j.gastro.2020.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kane E.M. Rev Panam Salud Publica. 2004;16:371–377. doi: 10.1590/s1020-49892004001200002. [DOI] [PubMed] [Google Scholar]
- 5.Redelman-Sidi G. Nat Rev Urol. 2020;17:316–317. doi: 10.1038/s41585-020-0325-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Venezuela Ministry of Popular Power Popular for Health. Available at: https://docs.bvsalud.org/biblioref/2020/09/1118413/art2-daniel-sanchez-y-otros.pdf. Revised June 15, 2020. Accessed December 11, 2021.
- 7.Mexican Institute of Social Security. Available at: http://educacionensalud.imss.gob.mx/es/system/files/Algoritmos_interinos_COVID19_CTEC.pdf. Accessed July, 25, 2020.
- 8.Gu J. Gastroenterology. 2020;158:1518–1519. doi: 10.1053/j.gastro.2020.02.054. [DOI] [PMC free article] [PubMed] [Google Scholar]