Abstract
Background
Urgent recognition and treatment are needed in patients with acute coronary syndrome (ACS), however this may be difficult during the Coronavirus disease 2019 (COVID-19) pandemic with a national lock-down. We aimed to examine the incidence of ACS after national lock-down.
Methods
The Danish government announced national lock-down on March 11, 2020 and first phase of reopening was announced on April 6. Using Danish nationwide registries, we identified first-time ACS admissions in (1) January 1 to May 7, 2017-2019, and (2) January 1, 2020 to May 6, 2020. Incidence rates of ACS admissions per week for the 2017 to 2019 period and the 2020 period were computed and incidence rate ratios (IRR) were computed using Poisson regression analysis.
Results
The number of ACS admissions were 8,204 (34.6% female, median age 68.3 years) and 2,577 (34.0% female, median age 68.5 years) for the 2017 to 2019- and 2020 period, respectively. No significant differences in IRRs were identified for weeks 1 to 9 (January 1 to March 4) for 2020 compared with week 1 to 9 for 2017 to 2019. In 2020, significant lower IRRs were identified for week 10 (March 5 to 11) IRR = 0.71 (95% confidence intervals [CI]: 0.58 to 0.87), week 11 (12 to 18 March) IRR = 0.68 (0.56 to 0.84), and week 14 (April 2 to April 8) IRR = 0.79 (0.65 to 0.97). No significant differences in IRRs were identified for week 15 to 18 (April 9 to May 6). In subgroup analysis, we identified that the main result was driven by male patients, and patients ≥60 years.
Conclusions
During the COVID-19 pandemic with an established national lock-down we identified a significant decline around 30% in the incidence of ACS admissions. Along with the reopening of society, ACS admissions were stabilized at levels equal to previous years.
Abbreviations: ACS, acute coronary syndrome; AMI, acute myocardial infarction; CABG, coronary artery bypass grafting; CAG, coronary angiography; CI, confidence interval; COPD, chronic obstructive pulmonary disease; COVID-19, Coronavirus Disease 2019; ICD-10, International Classification of Disease 10; IRR, incidence rate ratio; NSTEMI, non-ST-elevation myocardial infarction; OHCA, out of hospital cardiac arrest; UA, Unstable angina; OR, odds ratio; PCI, percutaneous coronary intervention; PPV, positive predictive value; STEMI, ST-elevation myocardial infarction
Background
During the global Coronavirus disease 2019 (COVID-19) pandemic international efforts have been raised to contain spreading of the coronavirus and avoid collapsing of national healthcare systems due to high disease activity and extensive need for intensive care and respirator treatment. In Denmark, the first person confirmed COVID-19 positive was identified at February 27, 2020.1 Danish authorities announced national lock-down on March 11 by imposing closure of Danish borders, sending home all employees working in non-essential functions in the public sector, and closure of schools and daycare institutions. One week later on March 18, a ban of gatherings of more than 10 people was instated. As admissions and deaths related to COVID-19 stabilized, Danish authorities announced the first phase of reopening on April 6, 2020.
Acute coronary syndrome (ACS) may be triggered by physical, but also psychological stress2., 3., 4.—factors that currently are being put to the test during the global spread of the COVID-19. National health care systems are being reorganized and optimized for handling patients with COVID-19 and this may also impact patients with other diseases, including ACS. Prior studies have shown that there are several ways that such epidemics have influence on other parts of the society and might induce collateral damage in patients with ACS is feared.5
We set out to study the incidence of ACS after the national lock-down of Denmark and how ACS admission rates changed when the first phase of societal reopening was established.
Methods
Data sources
All citizens in Denmark are provided with a unique identifier and linkage of nationwide health care registries is therefore possible. For the present study the following registries were included: the Danish National Patient Registry, the Civil Population Registry, and the National Prescription Registry. The National Patient Registry holds information on every hospitalization in Denmark since 1977. One primary diagnosis code is provided for every hospital admission according to the International Classification of Disease 10. Every admission may be provided with up to several secondary diagnoses. The Civil Population Registry holds information of every Danish citizen regarding date of birth, date of death, sex, and migration status. The Prescription Registry holds information on every filled prescription from a Danish pharmacy. The registries are described in details previously.6., 7., 8. The Prescription Registry held information up until February 29, 2020.
Danish Health Care System during the COVID-19 pandemic
The Danish health care system is tax-payer funded and universal health care is provided with few exceptions (physiotherapist and dentist). On March 11, 2020, the Danish government introduced a national lock-down, sending home public employees, closing schools, and daycare institutions. On March 18 national borders were closed. The health care system was reorganized, out-patient visits were converted to telemedicine or cancelled whenever possible, elective none-vital procedures were cancelled or postponed, emergency rooms and intensive care units were upgraded. On April 6, 2020 the Danish government announced the first phase of a slowly reopening of society. Primary schools reopened at April 15, 2020 and small businesses reopened at April 20, 2020.
Study population, outcome, follow-up
The study population comprised every Danish citizen in two periods: (1) A combined period of January 1, 2017 to May 7; 2017, January 1, 2018 to May 7, 2018; and January 1, 2019 to May 7, 2019, (2) January 1, 2020 to May 6, 2020. The total follow-up time had a maximum of 126 days for every period. Due to leap year in 2020, it was required that end dates differed between study periods. People were required to be alive and over 18 years at index (January 1, 2017-2020, respectively). People who had been admitted to hospital with ACS prior to index were excluded.
The primary outcome was first-time admission with ACS. The outcome was assessed from the National Patient Registry using the following diagnosis codes: I200 (unstable angina; UA), I210A, I211A, I214 (non-ST-elevation myocardial infarction; NSTEMI), I210B, I211B, I212, I213 (ST-elevation myocardial infarction; STEMI), and I219 (unspecified acute myocardial infarction [AMI]). The diagnosis codes of first-time UA, NSTEMI, and STEMI have been validated in the National Patient Registry with a positive predictive value of 88%, 92%, and 96%, respectively.9 For overall, first-time AMI, the diagnosis code (the International Classification of Disease-10: I21) has been validated with a positive predictive value of 97%.9 It was required that length of hospital stay was at least 24 hours, unless patients died within 24 hours of admission. Figure 1 shows a flow chart of the patient selection. Every person included in the study cohort was followed from date of entry until: ACS admission, date of death, or date of exit (May 7, 2017-2019, or May 6, 2020, respectively), whichever came first.
Figure 1.
Flow chart.
The figure shows the selection process for the study population.
Covariates
Demographic data (age and sex) were assessed from the Civil Population Registry. Comorbidities were registered from the National Patient Registry as an in-patient or out-patient, primary or secondary diagnosis code at any time prior to ACS admission. The following comorbidities were assessed: stroke, atrial fibrillation, peripheral vascular disease, heart failure, chronic renal failure, acute renal failure, diabetes, chronic obstructive pulmonary disease, dementia, liver disease, rheumatologic disease, or malignancy (Supplementary Table 1 presents specific codes). Concomitant pharmacotherapy was assessed from the Prescription Registry as a filled prescription within 1 year prior to ACS admission. Hypertension was defined from at least two antihypertensive filled prescriptions within 1 year of ACS admission as done previously.10 Coronary angiography (CAG), percutaneous coronary intervention (PCI), and coronary artery bypass grafting conducted during ACS admission was assessed and compared between study periods.
Statistics
Baseline characteristics for patients admitted to hospital with ACS were compared between study periods (1) January 1 to May 7, 2017-2019 (2) January 1, 2020 to May 6, 2020). Categorical variables are presented in counts and percentages and continuous variables are presented with a median and 25 and 75 percentiles. The number of ACS admissions was compared between study groups. For study period 1 (January 1 to May 7, 2017-2019), the average number of ACS admissions were computed for the comparison with study period 2 (January 1, 2020 to May 6, 2020) and difference in percentage was computed for the two study periods. The incidence rate of ACS admissions was computed for every week from index date in each study period. Incidence rates were computed with person years as the denominator and ACS admissions in the nominator. For the computation of the incidence rates the study cohort was split in bands of weeks (7 days) from index date. Incidence rate ratios (IRR) with 95% confidence interval [CI] were computed using a Poisson regression analysis for the comparison of every week for the two study periods. In a subgroup analysis, ACS admissions were grouped in (1) STEMI and (2) NSTEMI, UA, and AMI unspecified and IRR were computed for the two study periods. Further, in a subgroup analysis, we identified number of ACS admissions by age groups (<60 years and ≥60 years) and by sex for the two study periods.
For a detailed investigation of the period after national lock-down, two additional cohorts were investigated: (1) March 12 to May 6, 2017-2019, and (2) March 12, 2020 to May 6, 2020. Baseline characteristics were compared between cohorts and differences in ACS admissions were assessed. Further, incidence rates were computed by ACS subtype for the period after national lock-down and proportion of patients undergoing CAG, PCI, or coronary artery bypass grafting during ACS admission were reported along with 30-day mortality. For the lock-down period and the corresponding period in the 2017-2019 study cohort, 30-day mortality was examined for patients with ACS and compared between groups using a multivariable adjusted logistic regression analysis, including the following variables: sex, age, diabetes, hypertension, statin use, COPD, prior stroke, atrial fibrillation, heart failure, chronic renal failure. Results were presented with an odds ratio (OR). The level of statistical significance was P < .05. Data management and statistical analysis was conducted using SAS software 9.4 (SAS Institute, Inc., Cary, NC, USA) and the statistical software R version 3.5.0.11
Ethics
Registry-based studies from administrative data that are conducted for the sole purpose of statistics and scientific research do not require ethical approval or informed consent by law in Denmark. In accordance with the General Data Protection Regulation, the study is approved by the data responsible institute (the Capital Region of Denmark [approval number: P-2019-191]).
Results
A total of 4,470,461; 4,504,949; 4,534,612; and 4,554,923 people from the Danish population were identified at January 1, 2017, 2018, 2019 and 2020, respectively. For the 2017-2019 period, we identified that 8,204 patients were admitted with first-time ACS (STEMI: 26.4%, NSTEMI: 36.9%, UA: 14.7%, and AMI unspecified: 22.0%), while the corresponding numbers for the 2020-study period were 2,577 patients (STEMI: 29.9%, NSTEMI: 40.3%, UA: 12.9%, and AMI unspecified: 16.9%). We identified that 57.7% and 55.8% of the ACS patients underwent PCI for the 2017 to 2019- and 2020 period, respectively. Table 1 shows baseline characteristics for ACS patients for the two study periods and, overall, no differences were seen in sex, age, or comorbidities.
Table 1.
Baseline characteristics for patients admitted with ACS
| January 1 to May 7, 2017-2019 |
January 1 to May 6, 2020 |
|||
|---|---|---|---|---|
| N | (%) | N | (%) | |
| Number | 8,204 | (100) | 2,577 | (100) |
| Age (years), median (IQR) | 68.3 (58.0-77.3) | 68.5 (58.1-77.3) | ||
| Female | 2,838 | (34.6) | 876 | (34.0) |
| Comorbidities | ||||
| Stroke | 478 | (5.8) | 137 | (5.3) |
| Atrial flutter/fibrillation | 660 | (8.0) | 231 | (9.0) |
| Peripheral vascular disease | 347 | (4.2) | 91 | (3.5) |
| Heart failure | 451 | (5.5) | 146 | (5.7) |
| Chronic renal failure | 440 | (5.4) | 128 | (5.0) |
| Diabetes | 1,077 | (13.1) | 328 | (12.7) |
| COPD | 603 | (7.4) | 172 | (6.7) |
| Liver disease | 173 | (2.1) | 57 | (2.2) |
| Rheumatologic disease | 452 | (5.5) | 150 | (5.8) |
| Malignancy | 1,118 | (13.6) | 334 | (13.0) |
| Medication | ||||
| Beta blockade | 1,688 | (20.6) | 479 | (18.6) |
| Ca-channel blocker | 1,846 | (22.5) | 643 | (25.0) |
| RASi | 2,966 | (36.2) | 987 | (38.3) |
| Loop-diuretics | 928 | (11.3) | 248 | (9.6) |
| Statin | 2,446 | (29.8) | 883 | (34.3) |
| ASA | 1,651 | (20.1) | 486 | (18.9) |
| ADPi | 645 | (7.9) | 229 | (8.9) |
| OAC | 761 | (9.3) | 243 | (9.4) |
| Hypertension | 2,892 | (35.3) | 892 | (34.6) |
ACS, acute coronary syndrome; IQR, interquartile range; COPD, chronic obstructive pulmonary disease; RASi, renin-angiotensis system inhibitor; ASA, aspirin; ADPi, adenosine-di-phosphate inhibitor; OAC, oral anticoagulant therapy.
Comparison of ACS admissions, 2017-2019 vs 2020
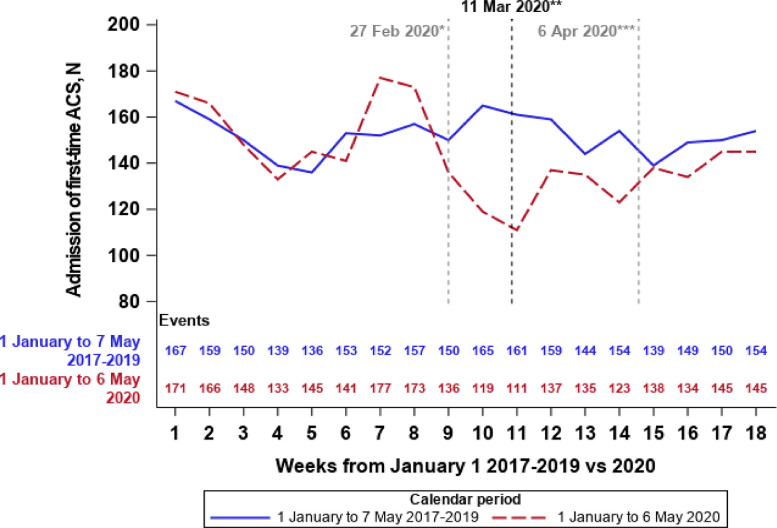
Overall, a 5.8% decline in ACS admissions were seen in the 2020 period as compared with the average of the 2017-2019 period. For subgroups of STEMI, NSTEMI, UA, and AMI unspecified, the difference in percentages in 2020 was +6.7%, +2.9%, −17.2%, and −27.7% as compared with the average of the corresponding subgroups for the 2017-2019 study period. Number of ACS admissions is depicted in Figure 2 . A decline in incidence rate of ACS was identified from weeks 9 to 18 (February 27 to May 6) in 2020 as compared with week 9 to 18 (February 27 to May 7) 2017-2019 with an overall incidence rate in week 9 to 18 in 2020 at 1.52 ACS cases/1,000 PY (95% CI: 1.44 to 1.60) as compared to 1.77 ACS cases /1,000 PY (1.72 to 1.82) for week 9 to 18 in 2017-2019 The overall incidence rate for week 1 to 8 in 2020 was 1.80/1,000 PY (95% CI: 1.70-1.90) as compared to 1.76 ACS cases/1,000 PY (95% CI: 1.70 to 1.81) for week 1 to 8 for 2017-2019. Person years and events with corresponding incidence rates and 95% CI are shown in Table 2 . In a regression analysis we identified a significant decline of ACS admissions with an IRR = 0.71 (95% CI: 0.58 to 0.87) for week 10 (March 5 to March 11), IRR = 0.68 (95% CI: 0.56 to 0.84) for week 11 (March 12 to March 18), and IRR = 0.79 (95% CI: 0.65 to 0.97) for week 14 (April 2 to April 8) in 2020 as compared with corresponding weeks in 2017-2019 (Figure 3 ). Reopening of society was announced on April 6 and for week 15-18 (April 9 to May 6) no difference between study periods were identified, Figure 3. In a subgroup analysis the IRR was examined for patients with STEMI for week 1 to 18 for the 2020 study period and no significant difference were found when compared with week 1 to 18 2017-2019, Supplementary Figure 1. The main result was mostly driven by patients with NSTEMI, UA, and AMI unspecified, Supplementary Figure 2. In subgroup analyses of age groups and sex, we identified that the main result was driven by male patients ≥60 years of age, Supplementary Figure 3.
Figure 2.
Number of ACS admissions.
The figure shows the average number of first-time ACS admissions from January 1 to May 7, 2017-2019 and January 1 to May 6, 2020 per week. ACS, acute coronary syndrome.
*First case of COVID-19 in Denmark.
**Announcement of national lock-down.
***Announcement of first phase of societal reopening.
Table 2.
Incidence rate of ACS admissions per week in 2017-2019 and 2020
| January 1 to May 7, 2017-2019 |
January 1 to May 6, 2020 |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Week | Events | Person years | IR per 1,000 PY | 95% CI | Events | Person years | IR per 1,000 PY | 95% CI | ||
| 1 | 500 | 258,890 | 1.93 | 1.77 | 2.11 | 171 | 87,285 | 1.96 | 1.69 | 2.28 |
| 2 | 477 | 258,825 | 1.84 | 1.68 | 2.02 | 166 | 87,263 | 1.90 | 1.63 | 2.21 |
| 3 | 449 | 258,761 | 1.74 | 1.58 | 1.90 | 148 | 87,242 | 1.70 | 1.44 | 1.99 |
| 4 | 416 | 258,698 | 1.61 | 1.46 | 1.77 | 133 | 87,223 | 1.52 | 1.29 | 1.81 |
| 5 | 407 | 258,634 | 1.57 | 1.43 | 1.73 | 145 | 87,202 | 1.66 | 1.41 | 1.96 |
| 6 | 458 | 258,566 | 1.77 | 1.62 | 1.94 | 141 | 87,181 | 1.62 | 1.37 | 1.91 |
| 7 | 455 | 258,499 | 1.76 | 1.61 | 1.93 | 177 | 87,160 | 2.03 | 1.75 | 2.35 |
| 8 | 470 | 258,430 | 1.82 | 1.66 | 1.99 | 173 | 87,140 | 1.99 | 1.71 | 2.30 |
| 9 | 449 | 258,362 | 1.74 | 1.58 | 1.91 | 136 | 87,120 | 1.56 | 1.32 | 1.85 |
| 10 | 494 | 258,294 | 1.91 | 1.75 | 2.09 | 119 | 87,100 | 1.37 | 1.14 | 1.64 |
| 11 | 482 | 258,229 | 1.87 | 1.71 | 2.04 | 111 | 87,080 | 1.27 | 1.06 | 1.54 |
| 12 | 477 | 258,162 | 1.85 | 1.69 | 2.02 | 137 | 87,059 | 1.57 | 1.33 | 1.86 |
| 13 | 432 | 258,098 | 1.67 | 1.52 | 1.84 | 135 | 87,038 | 1.55 | 1.31 | 1.84 |
| 14 | 461 | 258,036 | 1.79 | 1.63 | 1.96 | 123 | 87,016 | 1.41 | 1.18 | 1.69 |
| 15 | 417 | 257,975 | 1.62 | 1.47 | 1.78 | 138 | 86,995 | 1.59 | 1.34 | 1.87 |
| 16 | 448 | 257,915 | 1.74 | 1.58 | 1.91 | 134 | 86,973 | 1.54 | 1.30 | 1.82 |
| 17 | 451 | 257,857 | 1.75 | 1.59 | 1.92 | 145 | 86,953 | 1.67 | 1.42 | 1.96 |
| 18 | 461 | 257,798 | 1.79 | 1.63 | 1.96 | 145 | 86,932 | 1.67 | 1.42 | 1.96 |
ACS, acute coronary syndrome; IR, incidence rate; PY, person years; CI, confidence interval.
Figure 3.
Incidence rate ratio of ACS admission in 2020 vs 2017-2019
The figure shows the incidence rate ratios per week (1 to 18) in 2020 as compared with week 1 to 18 in 2017-2019. ACS, acute coronary syndrome.
*First case of COVID-19 in Denmark.
**Announcement of national lock-down.
***Announcement of first phase of societal reopening.
The 30-day mortality was 7.0% and 5.8% for ACS patients in the 2017 to 2019- and 2020 study period, respectively (crude analysis, P = .04). In adjusted analysis, no significant difference was found in 30-day mortality, OR = 0.85 (95% CI: 0.70 to 1.03 for patients in 2020 as compared with 2017-2019.
After national lock-down in 2020
An average of 1,186 ACS admissions were identified from March 12 to May 6, 2017-2019 as compared with 1,048 ACS admissions from March 12 to May 6, 2020 (11.6% decline). We identified that 59.2% and 54.1% of the ACS patients underwent PCI during ACS admission for the 2017 to 2019- and 2020 period, respectively. For subgroups of STEMI, NSTEMI, UA, and AMI unspecified, differences of −6.6%, −1.0%, −25.1%, and −29.6% were identified, respectively, for 2020 as compared with the average of 2017-2019. We identified a lower proportion of patients undergoing CAG and PCI during admission for all sub types of ACS (Table 3 ). Overall, no difference in baseline characteristics was identified for ACS patients for the two periods (Supplementary Table 2). The 30-day mortality was 6.6% and 6.7% for ACS patients in the 2017 to 2019- and 2020 study period, respectively. In adjusted analysis, no significant difference was found in 30-day mortality, OR = 1.03 (95% CI: 0.77 to 1.37) for patients in 2020 as compared with 2017-2019. No significant difference in 30-day mortality was found between study periods for the different sub types, STEMI P = .74, NSTEMI P = .58, UA P = .71, and AMI unspecified P = .12 (Table 3).
Table 3.
Incidence, management, and 30-day mortality by sub type of ACS
| March 12 to May 6, 2017-2019 |
March 12 to May 6, 2020 |
|||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| IR* | 95% CI | CAG (%) | PCI (%) | CABG (%) | 30-day mortality (%) | IR* | 95% CI | CAG (%) | PCI (%) | CABG (%) | 30-day mortality (%) | |
| STEMI | 0.49 | 0.46-0.52 | 95.4 | 88.8 | 1.5 | 8.4 | 0.45 | 0.40-0.50 | 85.4 | 79.2 | 3.6 | 7.8 |
| NSTEMI | 0.62 | 0.59-0.66 | 84.8 | 52.2 | 6.5 | 3.9 | 0.62 | 0.57-0.69 | 77.0 | 46.7 | 6.1 | 3.3 |
| UA | 0.26 | 0.24-0.28 | 77.7 | 34.6 | 8.5 | 1.1 | 0.19 | 0.16-0.23 | 71.2 | 30.3 | 8.3 | 0.8 |
| AMI unspecified | 0.38 | 0.36-0.41 | 70.1 | 49.6 | 6.1 | 12.6 | 0.27 | 0.23-0.31 | 62.1 | 46.2 | 3.3 | 17.0 |
ACS, acute coronary syndrome; IR, incidence rate; CI, confidence interval; CAG, coronary angiography; PCI, percutaneous coronary intervention; CABG, coronary artery bypass grafting; STEMI, ST-elevation myocardial infarction; NSTEMI, non-ST-elevation myocardial infarction; UA, unstable angina pectoris; AMI, acute myocardial infarction.
per 1,000 person years.
Discussion
This nationwide study examined the incidence of ACS during national lock-down due to the COVID-19 pandemic. The main finding was that the incidence of ACS admissions was significantly reduced with approximately 30% around the announcement of national lock-down as compared with a corresponding period from 2017 to 2019. At the end of the 2020 study period, ACS admissions stabilized at a level seen 2017-2019. In subgroup analysis, we identified that the main result was driven by male patients, and patients ≥60 years.
Data from the US, including nine high-volume cardiac catherization laboratories, suggested a 38% reduction in STEMI systems activation during the COVID-19 pandemic in the US.12 Data from Northern Italy and Austria also suggest a decline in ACS admissions of around 30% during the COVID-19 outbreak as compared with similar period the previous year.13., 14., 15. From Northern Italy, another study has been published showing an increment in out-of-hospital cardiac arrest (OHCA) during the COVID-19 outbreak as compared with previous year.16 No causal link can be made between the two observational studies from Northern Italy showing a decline in ACS admissions and an increment of OHCA, however the data are worrisome. Further, a multicenter study from tertiary centers in the US found a decline at 43.4% of hospitalizations for acute cardiovascular conditions.17 Our data supplement current knowledge with nationwide data suggesting a decrease in the incidence of ACS admissions around the announcement of nationwide lock-down during the COVID-19 pandemic in Denmark. Further, our data, not only describe a decline in admissions but also a decline in CAGs and PCIs along all subtypes of ACS. No clear explanation can be provided for this finding. Speculatively, a higher degree of type 2 AMIs could explain this finding, however from the registries used it was not able to differentiate by type of AMI. The national lock-down in Denmark was announced on March 11, 2020, however from our data a decline in ACS admissions was seen from February 27, 2020 (week 9). We can only speculate on this finding, however awareness in the Danish population of health care systems pushed to the limits in other countries may have led to patients not seeking medical help and fear of virus contraction by contact to the health care system. Further, our data showed that with the slowly reopening of Denmark from April 6, 2020, admission rates of ACS have returned towards previous years. This finding may suggest that care is especially needed in patients with ACS around the time of national lock-down and that admission rates normalize when reopening is initiated. This finding may be useful for health care planners and policy makers if a new pandemic or new COVID-19 wave appears. We found no significant reduction in STEMI admissions, however a trend towards a decline in the lock-down period could be interpreted from our results and wide confidence intervals in this subgroup suggest a potential type II-error. In part, patients classified as AMI unspecified may have been patients with STEMI, however we were not able to assess this category in further detail, which is a limitation to the present study. In additional subgroup analyses, we identified that the main result was driven by male patients and patients ≥ 60 years of age. Speculatively and in general terms, male patients may have a tendency to seek medical help less often than female patients. For patients ≥ 60 years, a high concern of contracting COVID-19 when seeking medical help may explain the decline in ACS admissions for this patient group. The Danish health care system has been vastly reorganized at the beginning of the pandemic. Outpatient visits were cancelled or changed to telemedicine if possible and nonvital elective procedures were cancelled, while resources were allocated for emergency rooms and intensive care units. A reorganization of this caliber may have had consequences for the urgent recognition and treatment of patients with ACS. Other health care systems pushed to the limits by the COVID-19 crisis have also seen a decline in ACS admission rates and allocation of health care resources for the treatment of COVID-19 may have jeopardized the care for patients with ACS.13 , 14 On the other hand, the government and health care authorities have announced that the health care system only should be consulted on urgent matters. Although well-indicated, some patients with chest pain may have abstained from consulting a physician out of fear from contracting COVID-19 or a feeling of overloading a health care system already on its knees.18 This is inappropriate from a patient point of view, a health care point of view and a new public health crisis might emerge beyond the COVID-19 crisis.
Hence, our findings may be partly explained by both system and patient related factors and we cannot clearly distinguish these from each other.
Little variations were seen in the characteristics of patients admitted with ACS in the lock-down period as compared with previous years. Overall, risk factors for ischemic heart disease were frequent in the population with no difference between groups. Hypothetically, one could have expected that patients with few comorbidities were more present during the lock-down period in order to navigate in a health care system with resources allocated to COVID-19 wards, however this was not seen from the data presented in this study.
Strengths and limitations
The main strength of our study is the large, unselected sample size from a nationwide cohort. The Danish nationwide health care registries provide a unique opportunity for the investigation of a national lock-down during the COVID-19 pandemic with detailed descriptions on ACS management and mortality.
Our study has some limitations. First, the ACS diagnosis was defined from diagnosis codes and data from electrocardiogram, troponin levels, and coronary angiography were not available. Our data provide knowledge on first-time ACS admissions and not total ACS admissions. Second, from the registries used, we were not able to identify patients with a delayed entry into the health care system and patients with missed STEMI were not assessable. Third, although fluctuations in ACS admission between weeks may be by chance, the changes over time was statistically significant, suggesting that the changes were related to the COVID-19 national lock-down in Denmark. Fourth, prescribed medication was only available up until February 29, 2020, hence we may have underestimated the use of medication in patients admitted with ACS in the most recent time period investigated. Fifth, no data on causes of death were obtained and we were not able to investigate the overall ACS mortality in the calendar periods studied. Sixth, data on ethnicity of included patients were not available. Seventh, patients categorized as AMI unspecified may have withhold patients with either STEMI or NSTEMI and the results of the sub group analysis by type of ACS must be seen in this light.
In conclusion, from nationwide data during a national lock-down due to the COVID-19 pandemic, we identified a significant decrease in ACS admissions with around 30%. Along with the reopening of society, ACS admissions were stabilized at levels equal to previous years. Subgroup analyses showed that the main result mainly was driven by male patients, ≥60 years of age. In a global health crisis as the one we face right now we are obliged to secure timely and appropriate treatment of all diseases—not solely COVID-19. Herein lies the information of patients to contact health care providers if symptoms occur.
Footnotes
Disclosure: None of the authors report conflicts of interest.
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.ahj.2020.11.004.
Appendix. Supplementary materials
Supplementary Figure 1. Incidence rate ratio of STEMI admission in 2020\elsamp #x202F;vs 2017-2019.
Supplementary Figure 1. The figure shows the incidence rate ratios per week (1 to 18) in 2020 as compared with week 1 to 18 in 2017-2019. STEMI: ST-elevation myocardial infarction.
*First case of COVID-19 in Denmark.
**Announcement of national lock-down.
***Announcement of first phase of societal reopening.
Supplementary Figure 2. Incidence rate ratio of non-STEMI admission in 2020\elsamp #x202F;vs 2017-2019.
Supplementary Figure 2. The figure shows the incidence rate ratios per week (1 to 18) in 2020 as compared with week 1 to 18 in 2017-2019. Non-STEMI: non-ST-elevation myocardial infarction, including non-STEMI, unstable angina, and myocardial infarction unspecified.
*First case of COVID-19 in Denmark.
**Announcement of national lock-down.
***Announcement of first phase of societal reopening.
Supplementary Figure 3. The figure shows the average number of first-time ACS admissions from January 1 to May 7, 2017-2019 and January 1 to May 6, 2020 per week. Panel A: Female patients, Panel B: Male patients, Panel C \elsamp #x003C;60 years of age, Panel D: \elsamp #x2265;60 years of age.
ACS: acute coronary syndrome.
*First case of COVID-19 in Denmark.
**Announcement of national lock-down.
***Announcement of first phase of societal reopening.
References
- 1.Statens Serum Institut. Første dansker testet positive for COVID-19 [Internet]. [cited April 15, 2020]. Available from: https://www.ssi.dk/aktuelt/nyheder/2020/02_27_foerste-tilfaelde-af-ny-coronavirus-i-dk 2020.
- 2.Wilbert-Lampen U., Leistner D., Greven S. Cardiovascular events during world cup soccer. N Engl J Med. 2008;358:475–483. doi: 10.1056/NEJMoa0707427. Jan 31. [DOI] [PubMed] [Google Scholar]
- 3.Mittleman M.A., Maclure M., Tofler G.H. Triggering of acute myocardial infarction by heavy physical exertion – protection against triggering by regular exertion. N Engl J Med. 1993;329:1677–1683. doi: 10.1056/NEJM199312023292301. Dec 2. [DOI] [PubMed] [Google Scholar]
- 4.Möller J., Hallqvist J., Diderichsen F. Do episodes of anger trigger myocardial infarction? a case-crossover analysis in the Stockholm Heart Epidemiology Program (SHEEP) Psychosom Med. 1999;61:842–849. doi: 10.1097/00006842-199911000-00019. Nov. [DOI] [PubMed] [Google Scholar]
- 5.Schull M.J., Stukel T.A., Vermeulen M.J. Effect of widespread restrictions on the use of hospital services during an outbreak of severe acute respiratory syndrome. Can Med Assoc J. 2007;176:1827–1832. doi: 10.1503/cmaj.061174. Jun 19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Schmidt M., Schmidt S.A., Sandegaard J.L. The Danish National Patient Registry: a review of content, data quality, and research potential. Clin Epidemiol. 2015;7:449–490. doi: 10.2147/CLEP.S91125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Schmidt M., Pedersen L., Sørensen H.T. The Danish Civil Registration System as a tool in epidemiology. Eur J Epidemiol. 2014;29:541–549. doi: 10.1007/s10654-014-9930-3. Aug. [DOI] [PubMed] [Google Scholar]
- 8.Kildemoes H.W., Sørensen H.T., Hallas J. The Danish National Prescription Registry. Scand J Public Health. 2011;39(7 Suppl):38–41. doi: 10.1177/1403494810394717. Jul. [DOI] [PubMed] [Google Scholar]
- 9.Sundbøll J., Adelborg K., Munch T. Positive predictive value of cardiovascular diagnoses in the Danish National Patient Registry: a validation study. BMJ Open. 2016;6 doi: 10.1136/bmjopen-2016-012832. Nov 18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Olesen J.B., Lip G.Y.H., Hansen M.L. Validation of risk stratification schemes for predicting stroke and thromboembolism in patients with atrial fibrillation: nationwide cohort study. BMJ. 2011;342(jan31 1):d124. doi: 10.1136/bmj.d124. Jan 31d124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.R Core Team . R Foundation for Statistical Computing; Vienna, Austria: 2018. R: A Language and Environment for Statistical Computing.https://www.R-project.org/ URL. [Google Scholar]
- 12.Garcia S., Albaghdadi M.S., Meraj P.M. Reduction in ST-segment elevation cardiac catheterization laboratory activations in the United States during COVID-19 Pandemic. J Am Coll Cardiol. 2020;75(22):2871–2872. doi: 10.1016/j.jacc.2020.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Metzler B., Siostrzonek P., Binder R.K. Decline of acute coronary syndrome admissions in Austria since the outbreak of COVID-19: the pandemic response causes cardiac collateral damage. Eur Heart J. 2020;41:1852–1853. doi: 10.1093/eurheartj/ehaa314. May 14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.De Filippo O., D'Ascenzo F., Angelini F. Reduced rate of hospital admissions for ACS during Covid-19 Outbreak in Northern Italy. N Engl J Med. 2020;383(1):88–89. doi: 10.1056/NEJMc2009166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Salvatore DR, Carmen S, Cristina B, et al. Reduction of hospitalizations for myocardial infarction in Italy in the COVID-19 era. European Heart Journal [Internet]. 2020 [cited 2020 Jun 4];Epub ahead of print. Available from: http://fdslive.oup.com/www.oup.com/pdf/production_in_progress.pdf 2020.
- 16.Baldi E., Sechi G.M., Mare C. Out-of-hospital cardiac arrest during the Covid-19 outbreak in Italy. N Engl J Med. 2020;383(5):496–498. doi: 10.1056/NEJMc2010418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bhatt A.S., Moscone A., McElrath E.E. Fewer Hospitalizations for Acute Cardiovascular Conditions During the COVID-19 Pandemic. J Am Coll Cardiol. 2020;76(3):280–288. doi: 10.1016/j.jacc.2020.05.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Michael Walter. Cardiologists urge heart attack, stroke patients not to delay medical attention over COVID-19 fears [Internet]. Cardiovascular business. [cited April 15, 2020]. Available from: https://www.cardiovascularbusiness.com/topics/acute-coronary-syndrome/cardiologists-heart-attack-stroke-delay-coronavirus-covid-19 2020
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Figure 1. Incidence rate ratio of STEMI admission in 2020\elsamp #x202F;vs 2017-2019.
Supplementary Figure 1. The figure shows the incidence rate ratios per week (1 to 18) in 2020 as compared with week 1 to 18 in 2017-2019. STEMI: ST-elevation myocardial infarction.
*First case of COVID-19 in Denmark.
**Announcement of national lock-down.
***Announcement of first phase of societal reopening.
Supplementary Figure 2. Incidence rate ratio of non-STEMI admission in 2020\elsamp #x202F;vs 2017-2019.
Supplementary Figure 2. The figure shows the incidence rate ratios per week (1 to 18) in 2020 as compared with week 1 to 18 in 2017-2019. Non-STEMI: non-ST-elevation myocardial infarction, including non-STEMI, unstable angina, and myocardial infarction unspecified.
*First case of COVID-19 in Denmark.
**Announcement of national lock-down.
***Announcement of first phase of societal reopening.
Supplementary Figure 3. The figure shows the average number of first-time ACS admissions from January 1 to May 7, 2017-2019 and January 1 to May 6, 2020 per week. Panel A: Female patients, Panel B: Male patients, Panel C \elsamp #x003C;60 years of age, Panel D: \elsamp #x2265;60 years of age.
ACS: acute coronary syndrome.
*First case of COVID-19 in Denmark.
**Announcement of national lock-down.
***Announcement of first phase of societal reopening.