Abstract
A 65-year-old man was followed for his coronary conditions using 320-multi detector row computed tomography (MDCT) for 30 months. He had soft plaque in the right coronary artery (RCA) [mean density of plaque was 22 hounsfield units (HU)]. His initial serum low-density lipoprotein cholesterol (LDL-C) was 72 mg/dL. After 30 months, his serum LDL-C was 26 mg/dL under 5.0 mg/day rosuvastatin and evolocumab 140 mg/2 weeks. MDCT showed a regression of the plaque in the RCA and the plaque density was 114 HU (intermediate plaque). In conclusion, intensive lipid-lowering therapy with evolocumab induced the regression and stabilization of coronary vulnerable plaque.
Keywords: myocardial infarction, PCSK9, evolocumab, plaque, multidetector row computed tomography
Introduction
Atherosclerotic plaque is usually considered to build up slowly. Some cases of a regression of plaque have been reported worldwide (1). Recently, lipid-lowering therapy using statins has been shown to reduce the risk of coronary artery disease and other complications (2). In addition, the addition of pro-protein convertase subtilisin/kexin type (PCSK) 9 inhibitors to existing statins was shown to suppress the onset of arteriosclerotic diseases (3).
Coronary artery plaque can be imaged non-invasively by multi detector row computed tomography (MDCT). MDCT has recently been recognized as an important resource for the evaluation of known or suspected coronary artery disease (CAD), especially for non-calcified lesions, and it can also be used to assess anomalies of the aorta, pulmonary artery, other vascular structures and cardiac chambers (4,5). We herein report a case of a regression and a change in the vulnerability of coronary plaque in the right coronary artery (RCA) after evolocumab treatment.
Case Report
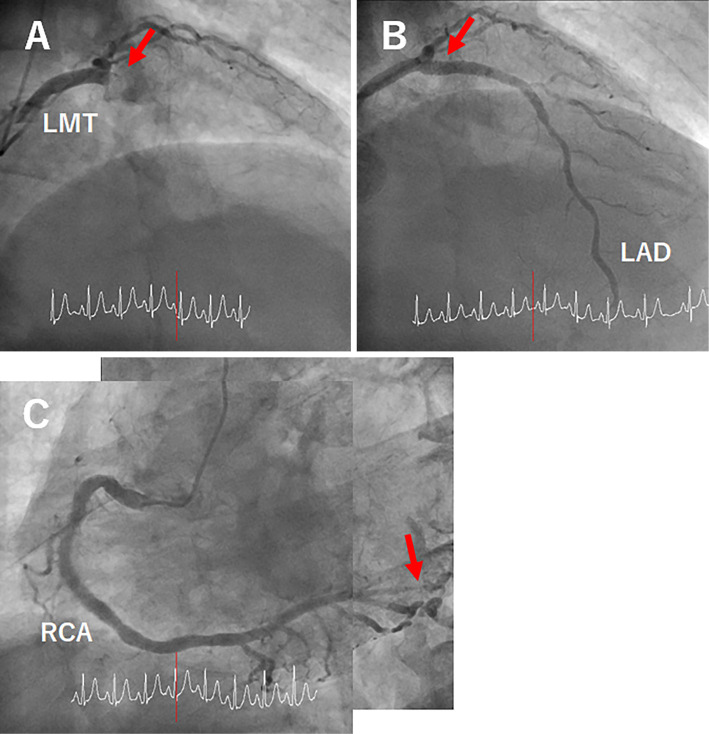
A 65-year-old man was brought to another emergency room complaining of sudden chest pain. He had never previously experienced chest pain. He had a history of dyslipidemia and diabetes mellitus (DM), but no history of hypertension. He was a past-smoker. With regard to the lipid profile, total cholesterol (TC) was 212 mg/dl, triglyceride (TG) was 87 mg/dL, high-density lipoprotein cholesterol (HDL-C) was 58 mg/dL, and low-density lipoprotein cholesterol (LDL-C) was 134 mg/dL. Coronary angiography showed significant focal occlusion of the left anterior descending artery (LAD) (Seg. 6) (Fig. 1A, B) and 90% stenosis of the RCA (Seg. 4 atrio-ventricular branch) (Fig. 1C). Since focal occlusion of the LAD was demonstrated and he was diagnosed to have acute myocardial infarction (AMI), antiplatelet therapy (aspirin 100 mg/day) and percutaneous coronary intervention (PCI) were administered. Clopidogrel 75 mg/day, rosuvastatin 2.5 mg/day, enalapril 2.5 mg/day, saxagliptin 5 mg/day and voglibose 0.9 mg/day were started after PCI.
Figure 1.
Coronary angiographic images before (A, C) and after percutaneous coronary intervention (PCI) (B). RCA: right coronary artery, LMT: left main coronary trunk artery, LAD: left anterior descending artery
We decided to follow his medical condition. His blood pressure was 108/73 mmHg without any laterality. His heart rate was 66 beats/min and regular. He had no cardiac murmur. An electrocardiogram showed a normal sinus rhythm and an abnormal Q wave in leads V1-2. A chest X-ray showed a normal cardiac silhouette (cardiothoracic ratio 41.1%). A transthoracic echocardiogram showed a left ventricular ejection fraction of 48.7% and anterior to anteroseptal severe hypokinesis. Further investigation was performed using 320-MDCT on an Aquilion ONE ViSION (Canon Medical Systems, Otawara, Japan) and a workstation (ZIO STATION, ZIO SOFT, Tokyo, Japan) (6). The volume-rendered and multi-planar reconstruction image showed the in-stent with mild stenosis in the LAD (Fig. 2A, B) and moderate stenosis of the RCA (Fig. 2C, D). A cross-sectional image showed moderate stenosis with vulnerable plaque (plaque size 1.87 mm2) in the RCA. The mean density of the plaque was 22 hounsfield units (HU), which indicated soft plaque (Fig. 2E). With regard to the lipid profile, TC, TG, HDL-C and LDL-C were 145 mg/dL, 43 mg/dL, 57 mg/dL and 72 mg/dL, respectively. Since the in-stent with mild stenosis in the LAD and moderate stenosis in the RCA was demonstrated, the dose of rosuvastatin was increased from 2.5 mg/day to 5.0 mg/day. Although we tried to add a higher dose of rosuvastatin, the patient complained of muscle pain.
Figure 2.
Multi detector row computed tomography (MDCT): Volume-rendered (A, C), multi- planar reconstructed (B, D) and cross-sectional images (E). RCA: right coronary artery, LAD: left anterior descending artery, LCX: left circumflex artery
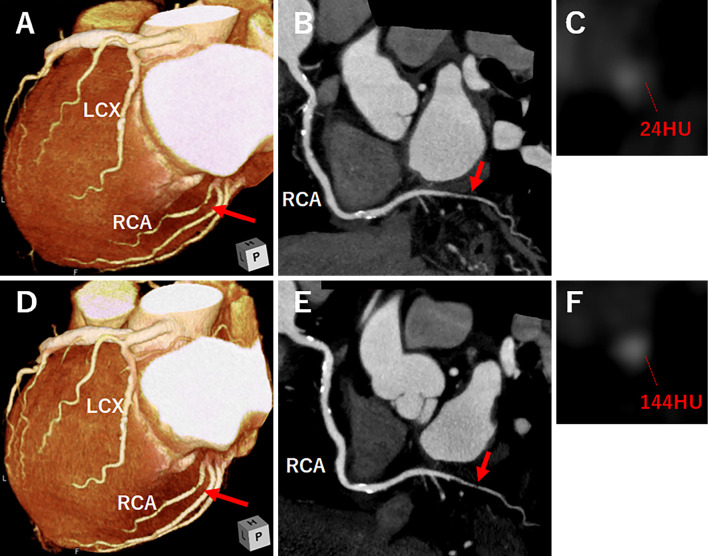
After 12 months, he had no symptoms and TC, TG, HDL-C and LDL-C were 142 mg/dL, 27 mg/dL, 64 mg/dL and 60 mg/dL, respectively. However, MDCT showed moderate stenosis and vulnerable plaque (plaque size 1.74 mm2), although the RCA showed a reduction in the lesion length. The mean density of the plaque was still 24 HU (Fig. 3A, B, C). Since focal stenosis of the RCA was demonstrated, evolocumab 140 mg/2 weeks was started with rosuvastatin 5.0 mg/day.
Figure 3.
Multi detector row computed tomography (MDCT): volume-rendered (A), multi-planar reconstructed (B) and cross-sectional images (C) after 12 months, and volume-rendered (D), multi-planar reconstructed (E) and cross-sectional images (F) after 30 months. RCA: right coronary artery, LAD: left anterior descending artery, LCX: left circumflex artery
After 30 months, TC, TG, HDL-C and LDL-C were 105 mg/dL, 33 mg/dL, 62 mg/dL and 26 mg/dL, respectively. MDCT showed mild stenosis and a regression of the plaque (plaque size 0.81 mm2) in the RCA. The mean density of the plaque was 114 HU, which indicated intermediate plaque (Fig. 3D-F) (Table).
Table.
Time Courses of Plaque and Lipid Profile.
Discussion
This patient represents a case of the regression and stabilization of coronary plaque in the RCA after intensive lipid-lowering therapy using evolocumab.
Patients in need of secondary prevention who have a medical history of CAD should be managed with a target of less than 100 mg/dL of LDL-C. In addition, patients with familial cholesterolemia (FH) and acute coronary syndrome (ACS) should be considered for strict management with a target of less than 70 mg/dL of LDL-C, especially high-risk patients with atherosclerotic diseases. Patients with DM are also considered to have a high risk of recurrence, and management according to FH and ACS should be considered (7). In this patient with DM who had a medical history of ACS in need of secondary prevention, management with a target LDL-C of less than 70 mg/dL was appropriate. After 12 months, although the LDL-C level was 60 mg/dL, MDCT showed moderate stenosis and vulnerable plaque. As a result, this patient was considered to require more intensive lipid-lowering therapy.
In the ESTABLISH study (8,9), JAPAN-ACS study (10) and PRECISE- intravascular ultrasound (IVUS) study (11), intensive LDL-C-lowering therapy using statins with or without ezetimibe for ACS was shown to be effective for suppressing plaque progression. In addition, a meta-analysis of clinical trials using IVUS showed that DM was an independent risk factor in patients who developed coronary plaque despite treatment to reduce LDL-C below 70 mg/dL (12). Strict LDL-C-lowering therapy is important for patients with CAD complicated with DM. Complications by DM was a negative risk factor for plaque regression in a sub-analysis in JAPAN-ACS (13). Since our case had other coronary risk factors, including DM and DL with coronary soft plaque, we thought that lipid-lowering therapy might not be significant. Thus, a target LDL-C of less than 70 mg/dL was not sufficient for regression and stabilization of coronary vulnerable plaque, indicating that a lower target might be better (11). Therefore, we decided to use evolocumab. The FOURIER study examined cardiovascular outcomes under evolocumab (average 2.2 years). After 48 weeks, LDL-C decreased 59% in the evolocumab group compared to that in the placebo group. The median value decreased from 90 mg/dL to 30 mg/dL. In addition, the incidence of major endpoints in the evolocumab group was significantly reduced compared to that in the placebo group (14). The study showed the potential for reducing cardiovascular risk by statin with PCSK9 inhibitor. The European Society of Cardiology (ESC)/European Atherosclerosis Society (EAS) guidelines recommend an LDL-C reduction of ≥50% from baseline and an LDL-C goal of <70 mg/dL for patients at high risk (15). In this case, since evolocumab reduced LDL-C by 50% or more (from LDL-C 60 mg/dL to 26 mg/dL), a remarkable regression and stabilization of coronary vulnerable plaque could be achieved.
MDCT has been previously used to diagnose atherosclerotic plaque (16,17). It has been reported that the mean density of soft plaque was 14±26 HU (-14 to +47HU), that of intermediate plaque was 91±21 HU (61 to 112 HU), and that of calcified plaque was 419±194 HU (126 to 736 HU) (18). In this case, the mean density of plaque by MDCT before treatment was 22 HU. The total volume of soft plaque in three vessels of coronary arteries was 1.74 mm3, and coronary artery calcification score was 316 arbitrary units (AU).
This plaque was classified as soft plaque, which is prone to ACS and more vulnerable to rupture (19). After 30 months of evolocumab, the mean density of plaque by MDCT increased to 114 HU, which is considered to be intermediate plaque. The total volume of soft plaque in three vessels of coronary arteries was 1.22 mm3, and coronary artery calcification score was 350 AU. The decrease in the total volume and the increase in the density indicated that plaque vulnerability had thus stabilized after treatment. In the GLAGOV study (20), the effect of evolocumab on coronary atherosclerotic plaque progression in patients receiving the optimal dose of statin therapy was examined by IVUS at baseline and 78 weeks. This study revealed that treatment with evolocumab significantly reduced the percent atheroma volume. MDCT may thus become a useful tool for studying the courses of the size and vulnerability of coronary plaque, and the effect of intensive lipid-lowering therapy (21).
Conclusions
Intensive lipid-lowering therapy with evolocumab induced the regression and stabilization of coronary vulnerable plaque. Non-invasive MDCT is a useful tool for diagnosing CAD, and for evaluating the size and properties of coronary plaque.
The authors state that they have no Conflict of Interest (COI).
References
- 1.Jensen LO, Thayssen P, Pedersen KE, Stender S, Haghfelt T. Regression of coronary atherosclerosis by simvastatin: a serial intravascular ultrasound study. Circulation 110: 265-270, 2004. [DOI] [PubMed] [Google Scholar]
- 2.LaRosa JC, Grundry SM, Waters DD, et al. Intensive lipid lowering with atorvastatin in patients with stable coronary disease. N Engl J Med 352: 1425-1435, 2005. [DOI] [PubMed] [Google Scholar]
- 3.Wiegand P, McCombs JS, Wang JJ. Factors of hyperlipidemia medication adherence in a nationwide health plan. Am J Manag Care 18: 193-199, 2012. [PubMed] [Google Scholar]
- 4.Achenbach S, Moselewski F, Ropers D, et al. Detection of calcified and noncalcified coronary atherosclerotic plaque by contrast-enhanced, submillimeter multidetector spiral computed tomography: a segment-based comparison with intravascular ultrasound. Circulation 109: 14-17, 2004. [DOI] [PubMed] [Google Scholar]
- 5.Budoff MJ, Cohen MC, Carcia MJ, et al. ACCF/AHA clinical competence statement on cardiac imaging with computed tomography and magnetic resonance. Circulation 112: 598-617, 2005. [DOI] [PubMed] [Google Scholar]
- 6.Mitsutake R, Miura S, Kawamura A, Saku K. Are metabolic factors associated with coronary artery stenosis on MDCT? Circ J 73: 132-138, 2009. [DOI] [PubMed] [Google Scholar]
- 7.Japan Atherosclerosis Society (JAS) Guidelines for Prevention of Atherosclerotic Cardiovascular Diseases. 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Okazaki S, Yokoyama T, Miyauchi K, et al. Early statin treatment in patients with acute coronary syndrome: demonstration of the beneficial effect on atherosclerotic lesions by serial volumetric intravascular ultrasound analysis during half a year after coronary event: the ESTABLISH study. Circulation 110: 1061-1068, 2004. [DOI] [PubMed] [Google Scholar]
- 9.Dohi T, Miyauchi K, Okazaki S, et al. Early intensive statin treatment for six months improves long-term clinical outcomes in patients with acute coronary syndrome (Extended-ESTABLISH trial): a follow-up study. Atherosclerosis 210: 497-502, 2010. [DOI] [PubMed] [Google Scholar]
- 10.Hiro T, Kimura T, Morimoto T, et al. ; JAPAN-ACS Investigators. Effect of intensive statin therapy on regression of coronary atherosclerosis in patients with acute coronary syndrome: a multicenter randomized trial evaluated by volumetric intravascular ultrasound using pitavastatin versus atorvastatin (JAPANACS [Japan assessment of pitavastatin and atorvastatin in acute coronary syndrome] study). J Am Coll Cardiol 54: 293-302, 2009. [DOI] [PubMed] [Google Scholar]
- 11.Tsujita K, Sugiyama S, Sumida H, et al. ; PRESISE-IVUS Investigators. Impact of dual lipid-lowering strategy with ezetimibe and atorvastatin on coronary plaque regression in patients with percutaneous coronary intervention: the multicenter randomized controlled PRECISE-IWS trial. J Am coil Cardiol 66: 495-507, 2015. [DOI] [PubMed] [Google Scholar]
- 12.Bayturan O, Kapadia S, Nicholls SJ, et al. Clinical predictors of plaque progression despite very low levels of low-density lipoprotein cholesterol. J Am Coll Cardiol 55: 2736-2742, 2010. [DOI] [PubMed] [Google Scholar]
- 13.Hiro T, Kimura T, Morimoto T, et al. ; JAPAN-ACS Investigators. Diabetes mellitus is a major negative determinant of coronary plaque regression during statin therapy in patients with acute coronary syndrome-serial intravascular ultrasound observations from the Japan Assessment of Pitavastatin and Atorvastatin in Acute Coronary Syndrome Trial (the JAPAN-ACS Trial). Circ J 74: 1165-1174, 2010. [DOI] [PubMed] [Google Scholar]
- 14.Giugliano RP, Pedersen TR, Park JG, et al. ; FOURIER Investigators. Clinical efficacy and safety of achieving very low LDL-cholesterol concentrations with the PCSK9 inhibitor evolocumab: a prespecified secondary analysis of the FOURIER trial. Lancet 390: 1962-1971, 2017. [DOI] [PubMed] [Google Scholar]
- 15.European Society of Cardiology (ESC)/European Atherosclerosis Society (EAS) guidelines for the management of dyslipidemias: lipid modification to reduce cardiovascular risk. 2019. [Google Scholar]
- 16.Mitsutake R, Miura S, Okamura K, Niimura H, Kawamura A, Saku K. Successful intensive lipid-lowering therapy using atorvastatin stabilizes coronary artery plaque as assessed by multi-detector row computed tomography. Intern Med 46: 859-863, 2007. [DOI] [PubMed] [Google Scholar]
- 17.Johnson KM, Dowe DA, Catanzano TM, Brink JA. Regression of coronary atherosclerotic plaque as shown by CT arteriography. AJR Am Roentgenol 187: W241, 2006. [DOI] [PubMed] [Google Scholar]
- 18.Schoenhangen P, Ziada KM, Kapadia SR, Crowe TD, Nissen SE, Tuzcu EM. Extent and direction of arterial remodeling in stable versus unstable coronary syndromes: an intravascular ultrasound study. Circulation 101: 598-603, 2000. [DOI] [PubMed] [Google Scholar]
- 19.Schroeder S, Kopp AF, Baumbach A, et al. Noninvasive detection and evaluation of atherosclerotic coronary plaque with multislice computed tomography. J Am Coll Cardiol 37: 1430-1435, 2001. [DOI] [PubMed] [Google Scholar]
- 20.Nicholls SJ, Puri R, Anderson T, et al. Effect of evolocumab on progression of coronary disease in statin-treated patients: the GLAGOV randomized clinical trial. JAMA 316: 2373-2384, 2016. [DOI] [PubMed] [Google Scholar]
- 21.Taylor S, Shaw LJ, Fayad Z, et al. Tracking atherosclerosis regression: a clinical tool in preventive cardiology. Atherosclerosis 180: 1-10, 2005. [DOI] [PubMed] [Google Scholar]