Abstract
Objectives:
The STOP-BANG questionnaire (snoring, tiredness, observed apneas, high blood pressure, body mass index, age, neck size, gender) was originally validated to screen for obstructive sleep apnea (OSA) in the surgical population. It has been validated in mixed populations of men and women. We aimed to evaluate its reliability for OSA screening of midlife women.
Study Design:
We retrospectively evaluated midlife women seen at the Women’s Health Clinic at Mayo Clinic in Rochester, Minnesota, who completed the STOP-BANG questionnaire and subsequently underwent diagnostic polysomnography (PSG) or home sleep apnea testing (HSAT).
Main Outcome Measures:
The questionnaire’s predictive ability was assessed with the apnea hypopnea index (AHI) measured at PSG and HSAT.
Results:
Because participants were female, the gender question response was consistently 0, making the mean (SD) STOP-BANG score low at 3 (1.2). The most sensitive item to detect any OSA and moderate to severe OSA through STOP-BANG was observed apneas; the most specific item to detect OSA and moderate to severe OSA was neck circumference exceeding 40 cm. A score of 3 or more had a sensitivity of 77% and a specificity of 45% to detect moderate to severe OSA. The area under the curve with the STOP-BANG score to predict moderate to severe OSA was 0.67 (95% CI, 0.51–0.84).
Conclusions:
Interpretation of the STOP-BANG questionnaire is nuanced for midlife women. Given the nature of its questions, a lower score may be predictive of more severe OSA in women, necessitating use of a lower threshold to trigger further testing.
Keywords: menopause, obstructive sleep apnea, STOP-BANG, women
Introduction
Obstructive sleep apnea (OSA) has historically been considered a disease of men [1, 2], with prevalence rates of 24% in young to middle-aged men compared with 9% in women of similar age [3, 4]. However, this discrepancy may be due to the underdiagnosis of OSA in women. The prevalence of OSA increases for women during perimenopause and menopause to 27% and 29%, respectively [5]. The marked increase in prevalence of OSA during the menopause transition may be due to the age-related increase in body mass index (BMI) [6–8]. In addition, it may be caused by structural changes in the airway or chemosensing mechanisms associated with the decline in endogenous sex steroids, including estradiol and progesterone [9].
OSA is associated with adverse cardiometabolic consequences, including hypertension [10], impaired glucose tolerance [11], stroke [12], and neurocognitive consequences including depression and cognitive impairment [13]. It is necessary to better understand its actual prevalence in midlife women and to develop reliable ways to screen women for this condition.
An estimated 93% of women with OSA are undiagnosed for OSA [14, 15], which perhaps reflects a difference in the clinical presentation of OSA for women compared with men [2, 16]. For example, women are 2 to 3 times less likely than men to report such classic symptoms of OSA as snoring, apneas, snorting, and gasping. Yet, women are more likely to report nonspecific symptoms like headache, fatigue, depression, anxiety, sleep onset insomnia, and sleep disruption [17]. Habitual snoring has been found to be less predictive of OSA for women than men [2]. It is conceivable that standard questionnaires used to screen for OSA in men (such as STOP-BANG [snoring, tiredness, observed apneas, high blood pressure, body mass index, age, neck size, gender]) may not be reliable for use in women.
The STOP-BANG questionnaire has been accepted widely as a convenient screening tool for OSA. However, it has not been validated specifically for use in women. The purpose of this study was to assess the reliability of the STOP-BANG questionnaire for OSA screening in midlife women.
Methods
Study Design and Population
This retrospective, cross-sectional study evaluated female patients seen in the Mayo Clinic Sleep Center and the Women’s Health Clinic (WHC) at Mayo Clinic in Rochester, Minnesota, between May 1, 2015, and December 31, 2018.
Women between the ages of 40 to 65 years were included when they had completed a STOP-BANG questionnaire (as part of a WHC visit) and subsequently had undergone polysomnography (PSG) or a home sleep apnea test (HSAT) during the specified period. All women seen in the Mayo Clinic WHC (a subspecialty clinic that provides consultative care to women with menopause or sexual health concerns) complete questionnaires, including the STOP-BANG questionnaire, that are contained in the Data Registry on Experiences of Aging, Menopause, and Sexuality (DREAMS). Women who received positive airway pressure (PAP) therapy at the time of PSG or HSAT were excluded from the study. The Mayo Clinic Institutional Review Board approved this study. All participants provided written informed consent for the use of their health records for research purposes.
STOP-BANG Questionnaire
The STOP-BANG questionnaire is an OSA screening tool of 8 questions with a self-reported yes or no answer to snoring, tired, observed apneas, high blood pressure, BMI (>35 kg/m2), age older than 50 years, neck size of 40 cm or greater, and gender (male sex). A positive response scores 1 point, and each negative response scores 0. Conventional OSA risk classification is 0 to 2 points, low risk; 3 or 4 points, intermediate risk; and 5 or greater points, high risk.
OSA Diagnosis and Severity
The diagnostic apnea hypopnea index (AHI) for PSG and the respiratory event index (REI) for HSAT were used to classify patients as no apnea (AHI/REI <5); mild OSA (AHI/REI, 5–14); moderate OSA (AHI/REI, 15–29); or severe OSA (AHI/REI ≥30). The STOP-BANG scores of participants were compared with the AHI or REI results obtained from their PSG or HSAT, respectively.
Data Collection and Statistics
Basic demographic data were obtained from DREAMS, including age and BMI. Health records were reviewed for information about medication use, including hormone therapy and PAP therapy. The descriptive statistics used for patient characteristics were median (interquartile range) or mean (SD) for continuous variables and frequency and percentage for categorical variables. Because this was a descriptive study that used existing registry data, a power calculation was not performed.
To evaluate the ability of the STOP-BANG questionnaire to distinguish OSA from non-OSA, multiple 2×2 contingency tables were constructed to calculate sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV) for each STOP-BANG question and each score cutoff. OSA outcomes of interest were any OSA (AHI >5), moderate-to-severe OSA (AHI >15), and severe OSA (AHI >30). Logistic regression was used to generate the area under the curve (AUC) to assess the diagnostic ability of the continuous STOP-BANG score. An AUC estimate of 0.7 to 0.8 was considered acceptable, and 0.8 to 0.9, excellent. Statistical analyses were performed with software (SAS version 9.4; SAS Institute Inc).
Results
Of the women who met the age criteria and completed the STOP-BANG questionnaire during their WHC consultation, 66 subsequently had a PSG (93%) or HSAT (7%) for evaluation of an abnormal screening overnight oximetry during the specified period and were included in the study. Table 1 summarizes the demographic and clinical characteristics.
Table 1.
Patient Demographic and Clinical Characteristics
| Variable | Valuea (N=66) |
|---|---|
| Age, mean (SD), y | 54 (6) |
| BMI, mean (SD), kg/m2 | 33.3 (7.5) |
| AHI, median (IQR) | 8 (3–13) |
| Severity of OSA | |
| None | 24 (36.4) |
| Mild | 28 (42.4) |
| Moderate | 8 (12.1) |
| Severe | 6 (9.1) |
| Positive response on STOP-BANG questions | |
| 1) Snoring | 41 (62.1) |
| 2) Tiredness or sleepy | 50 (75.8) |
| 3) Observed apneas | 14 (21.2) |
| 4) High blood pressure | 15 (22.7) |
| 5) BMI >35 | 26 (39.4) |
| 6) Age >50 y | 46 (69.7) |
| 7) Neck size >40 cmb | 11 (17) |
| 8) Male sex | 0 (0) |
Abbreviations: AHI, apnea-hypopnea index; BMI, body mass index; IQR, interquartile range; OSA, obstructive sleep apnea; STOP-BANG, snoring, tiredness, observed apneas, high blood pressure, body mass index, age, neck size, and gender.
Categorical variables are reported as number (percentage) of patients.
Neck circumference was available for 56 patients
The maximum response score in the STOP-BANG questionnaire was 6 (Table 1) because the response for the question about gender was consistently 0. In addition, neck circumference was not available for 10 women, but the results did not change after its exclusion from the analysis. Of our cohort, 30% were younger than 50 years. The mean (SD) STOP-BANG score was 3 (1.2). On the basis of STOP-BANG scores, 23 women (35%) were classified as low risk, 19 (29%) as intermediate risk, and 24 (36%) as high risk for OSA. On the basis of the AHI and REI obtained with PSG or HSAT, 24 women (36%) did not have OSA. By comparison, 28 women (43%) had mild; 8 (12%) had moderate, and 6 (9%) had severe OSA. Among women with an AHI or REI greater than 15 (moderate-to-severe OSA), results of the STOP-BANG questionnaire classified 3 (21%) as low risk; 5 (36%), intermediate risk; and 6 (43%), high risk. Of the 6 women with AHI or REI greater than 30 (ie, severe OSA), the results classified 1 as low risk; 1, intermediate risk; and 4, high risk.
Sensitivity, specificity, PPV, and NPV were calculated for each question of the STOP-BANG questionnaire (Table 2). The most sensitive question to detect any OSA (AHI >5) and moderate-to-severe OSA (AHI >15) was observed apneas. The most specific question was the presence of a neck size greater than 40 cm, and it was followed by the presence of tiredness. For severe OSA (AHI >30), no question had a good sensitivity, but presence of a neck circumference greater than 40 cm was specific for it.
Table 2.
Predictive Parameters of the STOP-BANG Questions for Any, Moderate-to-Severe, and Severe OSA
| OSA per STOP-BANGa Question | Value, Median (IQR) | |||
|---|---|---|---|---|
| Sensitivity | Specificity | PPV | NPV | |
| Any OSA (AHI >5) | ||||
| S | 0.26 (0.13–0.43) | 0.46 (0.28–0.66) | 0.40 (0.21–0.61) | 0.32 (0.18–0.48) |
| T | 0.34 (0.20–0.51) | 0.89 (0.72–0.98) | 0.81 (0.54–0.96) | 0.50 (0.36–0.64) |
| O | 0.82 (0.66–0.92) | 0.25 (0.11–0.45) | 0.60 (0.45–0.73) | 0.50 (0.23–0.77) |
| P | 0.74 (0.57–0.87) | 0.18 (0.06–0.37) | 0.55 (0.40–0.69) | 0.33 (0.12–0.62) |
| B | 0.61 (0.43–0.76) | 0.39 (0.22–0.59) | 0.57 (0.41–0.73) | 0.42 (0.23–0.63) |
| A | 0.21 (0.10–0.37) | 0.57 (0.37–0.76) | 0.40 (0.19–0.64) | 0.35 (0.21–0.50) |
| N | 0.26 (0.12–0.43) | 0.93 (0.76–0.99) | 0.82 (0.48–0.98) | 0.49 (0.35–0.63) |
| Moderate-to-severe OSA (AHI >15) | ||||
| S | 0.15 (0.02–0.45) | 0.57 (0.42–0.70) | 0.08 (0.01–0.26) | 0.73 (0.57–0.86) |
| T | 0.15 (0.02–0.45) | 0.74 (0.60–0.85) | 0.12 (0.02–0.38) | 0.78 (0.64–0.88) |
| O | 0.85 (0.55–0.98) | 0.23 (0.12–0.36) | 0.21 (0.11–0.35) | 0.86 (0.57–0.98) |
| P | 0.62 (0.32–0.86) | 0.19 (0.09–0.32) | 0.16 (0.07–0.29) | 0.67 (0.38–0.88) |
| B | 0.54 (0.25–0.81) | 0.38 (0.25–0.52) | 0.17 (0.07–0.33) | 0.77 (0.56–0.91) |
| A | 0.23 (0.05–0.54) | 0.68 (0.54–0.80) | 0.15 (0.03–0.38) | 0.78 (0.64–0.89) |
| N | 0.42 (0.15–0.72) | 0.88 (0.76–0.95) | 0.45 (0.17–0.77) | 0.86 (0.74–0.94) |
| Severe OSA (AHI >30) | ||||
| S | 0.17 (0.00–0.64) | 0.60 (0.47–0.72) | 0.04 (0.00–0.20) | 0.88 (0.74–0.96) |
| T | 0.17 (0.00–0.64) | 0.75 (0.62–0.85) | 0.06 (0.00–0.30) | 0.90 (0.78–0.97) |
| O | 0.67 (0.22–0.96) | 0.20 (0.11–0.32) | 0.08 (0.02–0.19) | 0.86 (0.57–0.98) |
| P | 0.67 (0.22–0.96) | 0.22 (0.12–0.34) | 0.08 (0.02–0.19) | 0.87 (0.60–0.98) |
| B | 0.50 (0.12–0.88) | 0.38 (0.26–0.52) | 0.07 (0.02–0.20) | 0.88 (0.70–0.98) |
| A | 0.17 (0.00–0.64) | 0.68 (0.55–0.80) | 0.05 (0.00–0.25) | 0.89 (0.76–0.96) |
| N | 0.60 (0.15–0.95) | 0.86 (0.74–0.94) | 0.27 (0.06–0.61) | 0.96 (0.87–1.00) |
Abbreviations: AHI, apnea-hypopnea index; IQR, interquartile range; NPV, negative predictive value; OSA, obstructive sleep apnea; PPV, positive predictive value; STOP-BANG, snoring, tiredness, observed apneas, high blood pressure, body mass index, age, neck sizes, gender.
Neck size available for 56 study participants. Gender question response was 0 for all participants because all were women.
For a STOP-BANG score of 3 or greater, the sensitivity for moderate-to-severe OSA (AHI/REI >15) was 77%, with a poor specificity of 45% (Table 3). As the STOP-BANG score cutoff increased from 3, the sensitivity for detecting moderate-to-severe OSA decreased but the specificity increased. For detection of severe OSA (AHI/REI >30), a STOP-BANG score of 4 or higher had slightly better predictability. However, at higher score cutoffs, sensitivity again decreased but specificity increased. The AUC of the STOP-BANG score for prediction of moderate-to-severe OSA was 0.67 (95% CI, 0.51–0.84) (Figure). The AUC of the STOP-BANG score for prediction of severe OSA was more favorable at 0.70 (95% CI, 0.41–0.99).
Table 3.
Predictive Parameters of STOP-BANG Questionnaire Score for Identification of Patients With OSA
| STOP-BANG Score for OSA | Value, Median (IQR) | |||
|---|---|---|---|---|
| Sensitivity | Specificity | PPV | NPV | |
| Any (AHI >5) | ||||
| ≥3 | 0.66 (0.49–0.80) | 0.50 (0.31–0.69) | 0.62 (0.47–0.79) | 0.52 (0.32–0.70) |
| ≥4 | 0.47 (0.31–0.64) | 0.71 (0.51–0.87) | 0.69 (0.48–0.86) | 0.50 (0.34–0.66) |
| ≥5 | 0.13 (0.04–0.28) | 0.93 (0.76–0.99) | 0.71 (0.29–0.96) | 0.44 (0.31–0.58) |
| Moderate-to-severe (AHI >15) | ||||
| ≥3 | 0.77 (0.46–0.95) | 0.45 (0.32–0.60) | 0.26 (0.13–0.42) | 0.89 (0.71–0.98) |
| ≥4 | 0.54 (0.25–0.81) | 0.64 (0.50–0.77) | 0.27 (0.12–0.48) | 0.85 (0.70–0.94) |
| ≥5 | 0.31 (0.09–0.61) | 0.94 (0.84–0.99) | 0.57 (0.18–0.90) | 0.85 (0.73–0.93) |
| Severe (AHI >30) | ||||
| ≥3 | 0.67 (0.22–0.96) | 0.42 (0.29–0.55) | 0.10 (0.03–0.24) | 0.93 (0.76–0.99) |
| ≥4 | 0.67 (0.22–0.96) | 0.63 (0.50–0.75) | 0.15 (0.04–0.35) | 0.95 (0.83–0.99) |
| ≥5 | 0.50 (0.12–0.88) | 0.93 (0.84–0.98) | 0.43 (0.10–0.82) | 0.95 (0.86–0.99) |
Abbreviations: AHI, apnea-hypopnea index; IQR, interquartile range; NPV, negative predictive value; OSA, obstructive sleep apnea; PPV, positive predictive value; STOP-BANG, snoring, tiredness, observed apneas, high blood pressure, body mass index, age, neck sizes, gender.
Figure.
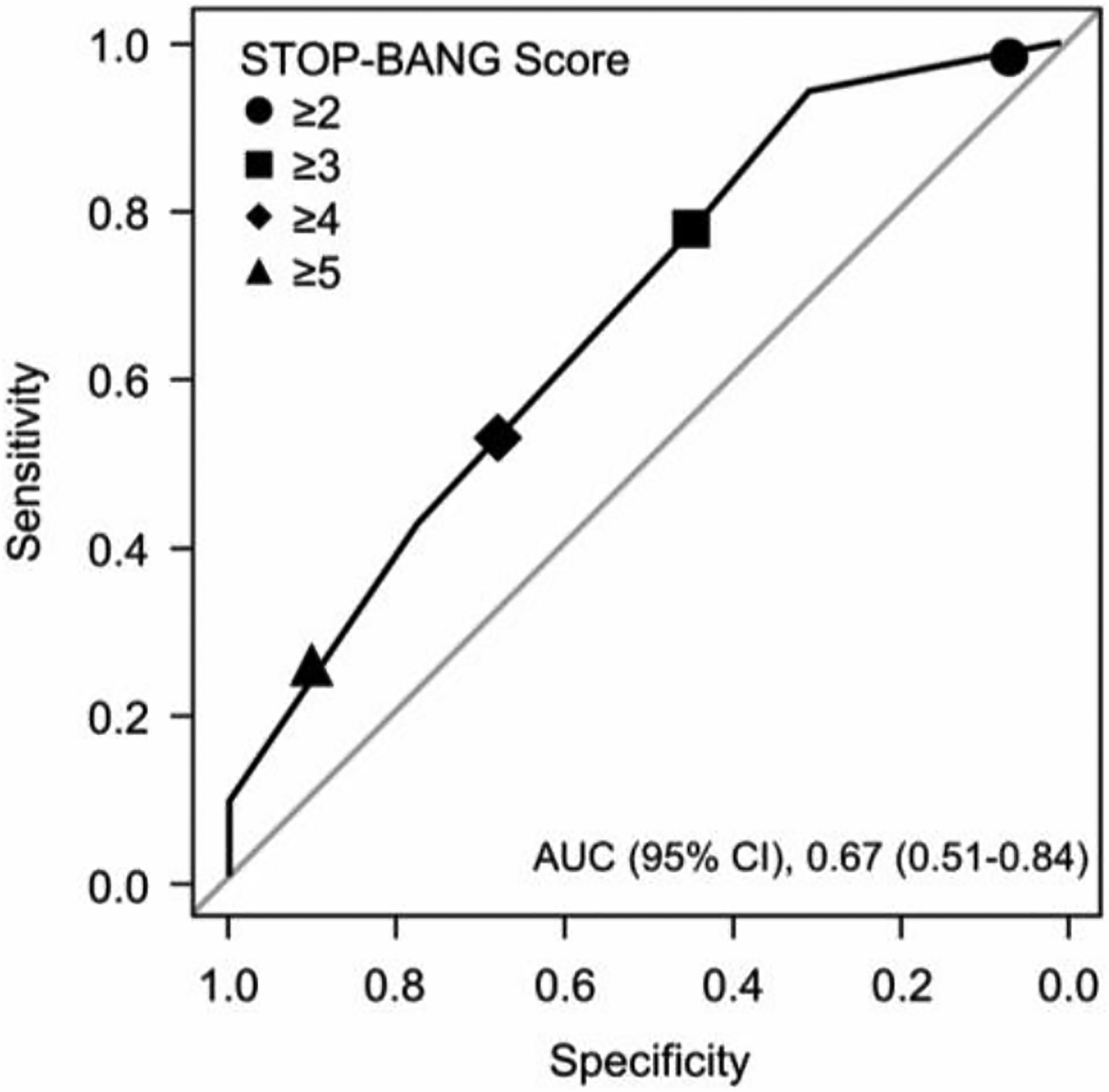
Receiver Operating Characteristic Curve of STOP-BANG Questionnaire Scores to Predict Moderate-to-Severe Obstructive Sleep Apnea of Midlife Women. AUC indicates area under the curve; STOP-BANG, snoring, tiredness, observed apneas, high blood pressure, body mass index, age, neck size, gender.
Discussion
At first glance, the results of the present study indicate that the STOP-BANG questionnaire has a lower sensitivity and specificity for detection of moderate-to-severe OSA in women than reported previously (sensitivity, 77% vs 83%; specificity, 45% vs 56%) [18]. However, of importance is recognition of the potential reasons for this outcome and the distinct nuances in the interpretation of this score for women.
The STOP-BANG questionnaire was created to screen for OSA in the surgical population [2]. When compared with other sleep questionnaires, including Berlin, STOP (snoring, tired, observed apneas, and high blood pressure), and Epworth Sleepiness Scale, the STOP-BANG was found to have the highest reliability [19, 20]. The questionnaire has been widely adopted and validated in different populations [21–24]. During the initial validation of the STOP-BANG questionnaire, Chung et al [18] reported that by adding BMI, age, neck circumference, and gender to the STOP scoring studied initially, the sensitivity to predict an AHI greater than 5 increased from 65.6% to 83.6 %, an AHI greater than 15 increased from 74.3% to 92.69%, and an AHI greater than 30 increased from 79.5% to 100%. However, the STOP-BANG questionnaire has not been developed as a sex-specific screening tool.
In the present study, some factors may have resulted in the lower sensitivity. All participants were women and thus scored 0 on the gender question, which automatically lowered the score. Neck circumference was not available for all participants. In previous validation studies of STOP-BANG that included women, the women were underrepresented, thus biasing the results toward the majority of male participants. One study that segregated the questionnaire in accordance with sex found that STOP-BANG had good performance in identifying women with OSA; however, the age range was broad and the sample size small [23]. A reasonable speculation is that lower scores on the STOP-BANG questionnaire are significant for women. Perhaps a lower threshold should be used to trigger more testing for OSA of women. Further study is needed to establish appropriate thresholds in this regard.
New approaches have been proposed in the past few years to increase the specificity of the STOP-BANG questionnaire [25, 26]. Mou et al [26] suggested an alternative, sex-specific scoring to improve predictive performance of STOP-BANG. They found that lowering the BMI to 30 kg/m2 and increasing the neck circumference to 43 cm improved the screening utility for both sexes at any level of OSA. Consistent with their findings, the results of the present study suggest that lowering the BMI would identify more women with sleep apnea. With a BMI cutoff of 30 kg/m2, the sensitivity for diagnosis of any OSA increased to 68%, with a specificity of 54%, PPV of 67%, and NPV of 56% for any OSA. For the diagnosis of severe OSA, sensitivity was 83%; specificity, 43%; PPV, 13%; and NPV, 96%. Other studies have validated the STOP-BANG questionnaire for specific mixed populations in which the BMI tended to be lower, but the percentage of women in those studies was only 11% to 40% [18, 27]. In addition, many women do not know their neck circumference, so this question does not have universal utility unless the neck circumference is measured at the clinic appointment.
BMI and neck circumference may not be the only clinical variables that affect the reliability of the questionnaire because of differences in the overall clinical presentation of OSA for women compared with men. For example, after adjustment for age, BMI, and AHI, men with OSA are more likely to report snoring (odds ratio [OR] 4.06; P<.001), habitual snoring or loud snoring (OR 2.34, P<.001; OR 2.14, P<.001) and apneas (OR 2.44, P<.001) than women [28]. In contrast, women are more likely to have tiredness (OR 0.57; P<.001), sleep-onset insomnia (OR 0.59; P<.004), and morning headaches (OR 0.32; P<.001).
In the present study, among the questions related to loud snoring, tiredness, and witnessed apnea, most of the women reported tiredness (75.8%) and loud snoring (62.1%), with witnessed apneas (21.2%). Witnessed apnea was the most sensitive question to identify women with moderate-to-severe OSA (sensitivity 85%), but it had low specificity (23%). The ability to have witnessed apnea may be a limiting criterion for midlife women who live alone (ie, no one observes them asleep). Additionally, women usually attend clinical appointments alone, which also makes this question difficult to answer [29].
Although the STOP-BANG questionnaire has been described as a practical screening tool for OSA, its interpretation for women is more nuanced. A lower overall score may be predictive of more severe OSA for women than for men. Women also are less likely to know their neck circumference, therefore requiring a neck measurement that adds time to assessments made in primary care clinics.
Limitations
The present study is limited because of its retrospective design and small sample size due to the low percentage of women who are referred for OSA testing and diagnosis. The proportion of women with moderate-to-severe OSA was low in this study. In addition, 13 of the 66 participants were taking hormone therapy at the time of PSG, which could have influenced the PSG and STOP-BANG questionnaire results. However, the small number limits subgroup analysis. These results need to be confirmed in a larger study. Finally, menopausal status was not consistently reported in our cohort. Therefore, a separate analysis comparing premenopausal women with postmenopausal women could not be performed.
Conclusion
The commonly used STOP-BANG questionnaire may not be as sensitive for OSA screening of women, particularly women with mild disease. Nevertheless, the tool is still useful for prediction of moderate-to-severe disease. Further study is needed to validate this questionnaire for women, with specific attention to establishment of appropriate thresholds to trigger confirmatory testing for OSA of women. Of importance, improvement in OSA diagnosis for midlife women is needed so appropriate therapeutic approaches can be initiated to reduce the long-term adverse health consequences of untreated sleep apnea.
Highlights.
The STOP-BANG questionnaire is a screening tool for obstructive sleep apnea (OSA).
Sex differences exist in the physiologic factors, symptoms, and severity of obstructive sleep apnea.
The STOP-BANG questionnaire for screening for obstructive sleep apnea has not been validated in women.
This screening questionnaire for obstructive sleep apnea needs different interpretation in women than men.
Funding
Dr. Kapoor and Dr. Miller's time was partly supported by the NIA grant U54 AG044170.
Abbreviations
- AHI
apnea hypopnea index
- AUC
area under the curve
- BMI
body mass index
- DREAMS
Data Registry on Experiences of Aging, Menopause, and Sexuality
- HSAT
home sleep apnea test
- NPV
negative predictive value
- OR
odds ratio
- OSA
obstructive sleep apnea
- PAP
positive airway pressure
- PPV
positive predictive value
- PSG
polysomnography
- REI
respiratory event index
- STOP-BANG
snoring, tiredness, observed apneas, high blood pressure, body mass index, age, neck size, gender
- WHC
Women’s Health Clinic
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Presented at the Sleep 2018 Annual Meeting, Baltimore, Maryland, June 2–6, 2018.
Conflicts of interest: All authors have read and approved the final version of this manuscript. The authors listed above certify that they have no affiliations with or involvement in any organization or entity with any financial interest (such as honoraria; educational grants; participation in speakers’ bureaus; membership, employment, consultancies, stock ownership, or other equity interest; and expert testimony or patent-licensing arrangements), or nonfinancial interest (such as personal or professional relationships, affiliations, knowledge or beliefs) in the subject matter or materials discussed in this manuscript.
Conflict of interest
Stephanie S. Faubion is a consultant for AMAG Pharmaceutical, Inc; Mithra Pharmaceuticals; and Proctor & Gamble.
All other authors declare that they have no conflict of interest.
Ethical approval
The Mayo Clinic Institutional Review Board approved this study. All participants provided written informed consent for the use of their health records for research purposes.
Research data (data sharing and collaboration)
There are no linked research data sets for this paper. Additional details can be sought by contacting the corresponding author, Ekta Kapoor, MBBS (kapoor.ekta@mayo.edu). Deidentified participant data that underlie the reported results in this article (ie, text, tables, and figures) can be made available beginning at 9 months and ending at 36 months after article publication for individual participant data meta-analysis, if the proposed use has been approved by an independent review committee. Proposals should be directed Ekta Kapoor, MBBS (kapoor.ekta@mayo.edu). To gain access, data requestors will need to sign a data access agreement.
References
- [1].Block AJ, Boysen PG, Wynne JW, Hunt LA, Sleep apnea, hypopnea and oxygen desaturation in normal subjects: a strong male predominance, N Engl J Med 300(10) (1979) 513–7. [DOI] [PubMed] [Google Scholar]
- [2].Young T, Hutton R, Finn L, Badr S, Palta M, The gender bias in sleep apnea diagnosis: are women missed because they have different symptoms?, Arch Intern Med 156(21) (1996) 2445–51. [PubMed] [Google Scholar]
- [3].Young T, Palta M, Dempsey J, Skatrud J, Weber S, Badr S, The occurrence of sleep-disordered breathing among middle-aged adults, N Engl J Med 328(17) (1993) 1230–5. [DOI] [PubMed] [Google Scholar]
- [4].Lozo T, Komnenov D, Badr MS, Mateika JH, Sex differences in sleep disordered breathing in adults, Respir Physiol Neurobiol 245 (2017) 65–75. [DOI] [PubMed] [Google Scholar]
- [5].Young T, Finn L, Austin D, Peterson A, Menopausal status and sleep-disordered breathing in the Wisconsin Sleep Cohort Study, Am J Respir Crit Care Med 167(9) (2003) 1181–5. [DOI] [PubMed] [Google Scholar]
- [6].Unal Y, Ozturk DA, Tosun K, Kutlu G, Association between obstructive sleep apnea syndrome and waist-to-height ratio, Sleep Breath 23(2) (2019) 523–529. [DOI] [PubMed] [Google Scholar]
- [7].Naufel MF, Frange C, Andersen ML, Girao M, Tufik S, Beraldi Ribeiro E, Hachul H, Association between obesity and sleep disorders in postmenopausal women, Menopause 25(2) (2018) 139–144. [DOI] [PubMed] [Google Scholar]
- [8].Correa KM, Bittencourt LR, Tufik S, Hachul H, [Frequency of sleep disturbances in overweight/obese postmenopausal women], Rev Bras Ginecol Obstet 36(2) (2014) 90–6. [PubMed] [Google Scholar]
- [9].Lin CM, Davidson TM, Ancoli-Israel S, Gender differences in obstructive sleep apnea and treatment implications, Sleep Med Rev 12(6) (2008) 481–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Torres G, Sanchez-de-la-Torre M, Barbe F, Relationship between OSA and hypertension, Chest 148(3) (2015) 824–832. [DOI] [PubMed] [Google Scholar]
- [11].Nagayoshi M, Punjabi NM, Selvin E, Pankow JS, Shahar E, Iso H, Folsom AR, Lutsey PL, Obstructive sleep apnea and incident type 2 diabetes, Sleep Med 25 (2016) 156–161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Yaggi HK, Concato J, Kernan WN, Lichtman JH, Brass LM, Mohsenin V, Obstructive sleep apnea as a risk factor for stroke and death, N Engl J Med 353(19) (2005) 2034–41. [DOI] [PubMed] [Google Scholar]
- [13].Blackwell T, Yaffe K, Laffan A, Redline S, Ancoli-Israel S, Ensrud KE, Song Y, Stone KL, Osteoporotic G Fractures in Men Study, Associations between sleep-disordered breathing, nocturnal hypoxemia, and subsequent cognitive decline in older community-dwelling men: the Osteoporotic Fractures in Men Sleep Study, J Am Geriatr Soc 63(3) (2015) 453–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Huang T, Lin BM, Markt SC, Stampfer MJ, Laden F, Hu FB, Tworoger SS, Redline S, Sex differences in the associations of obstructive sleep apnoea with epidemiological factors, Eur Respir J 51(3) (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Young T, Evans L, Finn L, Palta M, Estimation of the clinically diagnosed proportion of sleep apnea syndrome in middle-aged men and women, Sleep 20(9) (1997) 705–6. [DOI] [PubMed] [Google Scholar]
- [16].Ye L, Pien GW, Weaver TE, Gender differences in the clinical manifestation of obstructive sleep apnea, Sleep Med 10(10) (2009) 1075–84. [DOI] [PubMed] [Google Scholar]
- [17].Shepertycky MR, Banno K, Kryger MH, Differences between men and women in the clinical presentation of patients diagnosed with obstructive sleep apnea syndrome, Sleep 28(3) (2005) 309–14. [PubMed] [Google Scholar]
- [18].Chung F, Yegneswaran B, Liao P, Chung SA, Vairavanathan S, Islam S, Khajehdehi A, Shapiro CM, STOP questionnaire: a tool to screen patients for obstructive sleep apnea, Anesthesiology 108(5) (2008) 812–21. [DOI] [PubMed] [Google Scholar]
- [19].Chiu HY, Chen PY, Chuang LP, Chen NH, Tu YK, Hsieh YJ, Wang YC, Guilleminault C, Diagnostic accuracy of the Berlin questionnaire, STOP-BANG, STOP, and Epworth sleepiness scale in detecting obstructive sleep apnea: a bivariate meta-analysis, Sleep Med Rev 36 (2017) 57–70. [DOI] [PubMed] [Google Scholar]
- [20].Pataka A, Daskalopoulou E, Kalamaras G, Fekete Passa K, Argyropoulou P, Evaluation of five different questionnaires for assessing sleep apnea syndrome in a sleep clinic, Sleep Med 15(7) (2014) 776–81. [DOI] [PubMed] [Google Scholar]
- [21].Alam A, Chengappa KN, Ghinassi F, Screening for obstructive sleep apnea among individuals with severe mental illness at a primary care clinic, Gen Hosp Psychiatry 34(6) (2012) 660–4. [DOI] [PubMed] [Google Scholar]
- [22].Chung F, Yang Y, Liao P, Predictive performance of the STOP-BANG score for identifying obstructive sleep apnea in obese patients, Obes Surg 23(12) (2013) 2050–7. [DOI] [PubMed] [Google Scholar]
- [23].Cruces-Artero C, Herves-Beloso C, Martin-Miguel V, Hernaiz-Valero S, Lago-Deibe FI, Montero-Gumucio M, Orge-Amoedo M, Roca-Pardinas J, Claveria A, [Diagnostic accuracy of STOP-BANG questionnaire on moderate sleep apnoea in primary care], Gac Sanit 33(5) (2019) 421–426. [DOI] [PubMed] [Google Scholar]
- [24].Nagappa M, Liao P, Wong J, Auckley D, Ramachandran SK, Memtsoudis S, Mokhlesi B, Chung F, Validation of the STOP-BANG questionnaire as a screening tool for obstructive sleep apnea among different populations: a systematic review and meta-analysis, PLoS One 10(12) (2015) e0143697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Chung F, Abdullah HR, Liao P, STOP-BANG questionnaire: a practical approach to screen for obstructive sleep apnea, Chest 149(3) (2016) 631–8. [DOI] [PubMed] [Google Scholar]
- [26].Mou J, Pflugeisen BM, Crick BA, Amoroso PJ, Harmon KT, Tarnoczy SF, Shirley Ho S, Mebust KA, The discriminative power of STOP-BANG as a screening tool for suspected obstructive sleep apnea in clinically referred patients: considering gender differences, Sleep Breath 23(1) (2019) 65–75. [DOI] [PubMed] [Google Scholar]
- [27].Nunes FS, Danzi-Soares NJ, Genta PR, Drager LF, Cesar LA, Lorenzi-Filho G, Critical evaluation of screening questionnaires for obstructive sleep apnea in patients undergoing coronary artery bypass grafting and abdominal surgery, Sleep Breath 19(1) (2015) 115–22. [DOI] [PubMed] [Google Scholar]
- [28].Nigro CA, Dibur E, Borsini E, Malnis S, Ernst G, Bledel I, Gonzalez S, Arce A, Nogueira F, The influence of gender on symptoms associated with obstructive sleep apnea, Sleep Breath 22(3) (2018) 683–693. [DOI] [PubMed] [Google Scholar]
- [29].Quintana-Gallego E, Carmona-Bernal C, Capote F, Sanchez-Armengol A, Botebol-Benhamou G, Polo-Padillo J, Castillo-Gomez J, Gender differences in obstructive sleep apnea syndrome: a clinical study of 1166 patients, Respir Med 98(10) (2004) 984–9. [DOI] [PubMed] [Google Scholar]


