Abstract
Study Design:
A retrospective review of clinical data and costs was performed for surgeries for adolescent idiopathic scoliosis (AIS) conducted from 2008 to 2017.
Objective:
Cost containment and healthcare value have become focal points in Japanese health care policy. The purpose of the study was to investigate trends over time in medical costs for surgery for AIS.
Methods:
A total of 83 patients underwent surgery for AIS from 2008 to 2017 at our hospital. Clinical data and length of stay were collected, and medical costs for surgery, local bone grafting, fees per day, and surgical instruments were evaluated.
Results:
There were slight year-by-year decreases in fees per day and decreases in costs of surgical instruments. The average length of stay was 16.4 days and gradually decreased over time. In contrast, scoliosis surgery costs increased about 1.6 times in 10 years from $9515 to $15 130.
Conclusion:
The trends for decreases in fees per day and prices for surgical instruments reflect recent government medical cost control policies. The cost for scoliosis surgery is also defined by the government, and the increase over 10 years may reflect the perspective of valuing effective and advanced surgeries. This study of cost trends of operative spinal intervention provides an assessment of surgical benefit and is likely to influence health care costs.
Keywords: trends, spine surgery, adolescent idiopathic scoliosis, medical costs, spinal instrumentation, health care costs
Introduction
Medical expenses in Japan have increased yearly from $353.9 billion in 2000 to over $495.5 billion in 2015.1 These increasing health care costs pose a significant challenge to the sustainability of the health care economy. Thus, efforts are required in current medical care to reduce expenses, such as shortening the length of hospital stay. In Japan, an all-inclusive payment system, a so-called “bundle payment,” was introduced in hospitals with specific functions in 2003. Since 2005, this method has been used in national hospitals, social insurance hospitals, and other centers. Generally, hospitalization costs in Japan include an all-inclusive payment (hospital administration fees per day, medical examination, medication, injection, diagnostic imaging) and an itemized payment (surgery, rehabilitation), with most costs determined by the government as official medical prices every two years. Cost containment and defining the value of health care provided to patients has become a focal point in Japanese health care policy.2-4 In this context, surgeons have responsibilities to society to limit costs related to spine surgery, and thus, more rigorous economic analyses of medicine and surgery are required.
Adolescent idiopathic scoliosis (AIS) is a 3-dimensional spinal deformity that results in physical and psychosocial impairment, including poor self-image, low self-esteem, and back pain.5-7 The primary goals of surgical treatment of AIS are to obtain curve correction, to prevent curve progression, and to achieve a balanced spine in the coronal and sagittal planes. Numerous studies have shown the clinical and radiographic benefits of spinal arthrodesis and instrumentation to treat progressive AIS.8-12 Surgical techniques for AIS continue to evolve, and surgical treatment has expanded greatly. Currently, posterior fixation with a pedicle screw is widely performed for AIS, since use of pedicle screws reduces the rate of revision surgery and improves radiographic and clinical outcomes.13 Blood salvage techniques and spinal cord monitoring are now also standard methods in surgery for AIS.14-18
These recent technological advances have added new procedures in surgery, with a resultant increase in medical costs. The cost-effectiveness of many spinal surgeries has been reported, but there has been less attention to the surgical costs themselves.19,20 In an effort to understand the value of operative management, we investigated operative resource utilization and the cost of treatment for AIS. There has been no previous report on the medical economics of AIS surgery in Japan. The purpose of this study was to evaluate the total treatment costs and medical bundle payments in spinal surgery for AIS and to investigate trends over time.
Materials and Methods
The subjects of the study were 83 patients (3 males, 80 females) who underwent surgery for AIS using a posterior only approach with pedicle screw instrumentation in a prone position with a one-stage procedure at our hospital from January 2008 to December 2017. Cases treated with anterior surgery, anterior and posterior combination surgery, or surgery for syndromic or congenital scoliosis were excluded.
The mean age at the time of surgery was 14.6 years (11-19 years). Preoperative motor status and comorbidities were not used as exclusion criteria. Demographic, radiographic, and surgical data were collected for each patient. Pre- and postoperative scoliosis was measured using the Cobb method. Curves were classified with the Lenke system.21 This study was approved by the ethical committee of our hospital.
In all 83 cases, intraoperative brain-evoked muscle-action potentials (Br(E)-MsEPs) were recorded for spinal cord monitoring. Pedicle screws were inserted and polyethylene tape was simultaneously passed under the lamina. All vertebrae were held by pedicle screws or tapes. After local bone graft, rods bent into a good sagittal alignment were located on the concave side and correction was performed through a rotation maneuver. Ponte osteotomy was performed if required. Distraction was applied to the pedicle screws and the concave side of the curve was corrected. For the convex side, the rods were located in situ after local bone graft, and correction was performed by applying compression between the pedicle screws.22,23
A retrospective analysis of the AIS surgeries was performed using clinical data for fusion range, number of screws, screw density, operative time, estimated blood loss (EBL), length of hospital stay (LOS), and cost of hospitalization and surgical treatment of AIS over 10 years. Screw density was calculated as the total number of screws in the construct divided by the fusion range.24 Trends were examined for the costs for scoliosis surgery, local bone grafting, hospital administration fees per day, and surgical instruments, all of which are determined by the government every 2 years. Based on these data, the total treatment cost per patient per year was calculated.
Results
The preoperative characteristics of the patients are shown in Table 1. The Lenke types were 1 (n = 22), 2 (n = 15), 3 (n = 9), 4 (n = 4), 5 (n = 21), and 6 (n = 12). Preoperatively, the mean Cobb angle was 54.7° (43°-96°) and the manual traction Cobb angle was 24.3° (6°-73°). Surgery was performed in 22 cases in 2008-2009, 10 cases in 2010-2011, 19 cases in 2012-2013, 13 cases in 2014-2015, and 19 cases in 2016-2017. Postoperatively, the mean Cobb angle was 11.9° (1°-41°) and the correction rate was 75.3% (45.0%-97.6%). The average operation time was 287 minutes (159-606 minutes) and the average EBL was 776 mL (85-3300 mL). The average fusion range was 10.0 (6-15) levels, and was 9.8 levels in 2008-2009, 10.0 levels in 2010-2011, 9.6 levels in 2012-2013, 10.3 levels in 2014-2015, and 10.4 levels in 2016-2017. For instrumentation, 14.7 screws were used per patient in 2008-2009, 15.1 in 2010-2011, 14.1 in 2012-2013, 15.3 in 2014-2015, and 16.1 in 2016-2017. The mean screw density was 1.51 screws per fusion range, with a range of 1.47 to 1.59 screws (Table 2). The average LOS was 16.4 days (11 to 22 days). None of the patients had intra- or postoperative neurological sequelae. All patients received preoperative autologous blood donations and postoperative blood transfusion. There were no postoperative neurological deficits.
Table 1.
Demographic and Surgical Data (n = 83).a
| Item | Value |
|---|---|
| Demographic data | |
| Age (years) | 14.6 ± 2.2 |
| Female, n (%) | 80 (96) |
| Height (cm) | 154 ± 9.1 |
| Lenke classification, n (%) | |
| Type 1 | 22 (27) |
| Type 2 | 15 (18) |
| Type 3 | 9 (10) |
| Type 4 | 4 (5) |
| Type 5 | 21 (25) |
| Type 6 | 12 (14) |
| Preoperative Cobb angle (major curve) (deg) | 54.7 ± 14.5 |
| Preoperative traction Cobb angle (major curve) (deg) | 24.3 ± 10.1 |
| Procedural variables | |
| Operative time (min) | 287 ± 78 |
| Estimated blood loss (mL) | 776 ± 551 |
| Outcome | |
| Postoperative Cobb angle (deg) | 11.9 ± 7.5 |
| Correction rate (%) | 75.3 ± 12.4 |
| Length of stay (days) | 16.4 ± 2.2 |
a Data are shown as mean ± standard deviation or number (percentage).
Table 2.
Changes in Fusion Range, Number of Screws, and Screw Density Over Time.
| Year | Patients (n) | Fusion Range | Number of Screws | Screw Densitya |
|---|---|---|---|---|
| 2008-2009 | 22 | 9.8 | 14.7 | 1.50 |
| 2010-2011 | 10 | 10.0 | 15.1 | 1.51 |
| 2012-2013 | 19 | 9.6 | 14.1 | 1.47 |
| 2014-2015 | 13 | 10.3 | 15.3 | 1.49 |
| 2016-2017 | 19 | 10.4 | 16.1 | 1.59 |
| Total | 83 | 10.0 | 15.1 | 1.51 |
a Screw density is reported per vertebral level.
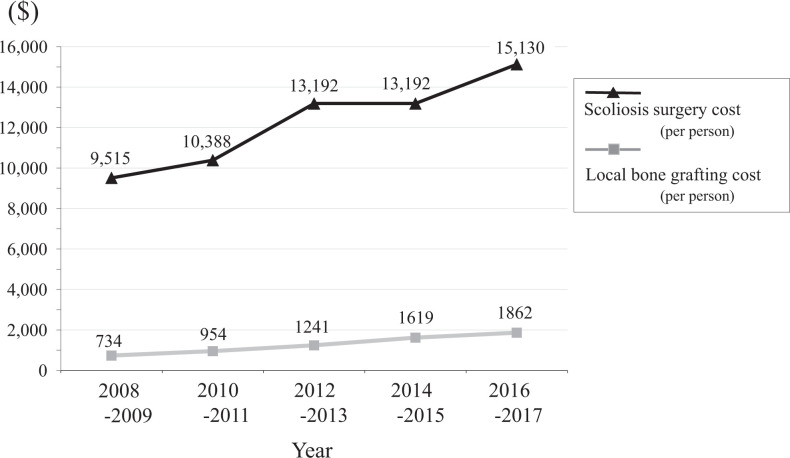
As medical costs are stipulated by the Ministry of Health, Labour and Welfare (MHLW), there were slight year-by-year decreases in hospital administration fees per day (Figure 1). There were also decreases in costs of surgical instruments such as screws, rods, and sublaminar wire (Figure 2), for which the reimbursement price is also defined by the government. LOS also gradually decreased over time (Figure 3). In contrast, scoliosis surgery costs, which are also determined by the MHLW, increased about 1.6 times in 10 years (from $9515 to $15 130) and the local bone grafting cost also increased (Figure 4). The proportion of the total cost occupied by surgical costs also increased over time (Figure 5). The surgical costs included those for implants, anesthesia, intraoperative spinal monitoring, blood transfusion, and intraoperative drugs. These costs increased over the study period, except for the reimbursement price of surgical instruments, which were included as part of the surgical cost.
Figure 1.
Trend in hospital administration fees per day over time.
Figure 2.
Trends in individual reimbursement prices for surgical instruments over time.
Figure 3.
Trends in length of stay over time.
Figure 4.
Trends in scoliosis surgery costs and local bone grafting costs per person, as defined by the Ministry of Health Labour and Welfare.
Figure 5.
Trends in total treatment costs and proportion occupied by surgical costs per person.
Discussion
The Diagnosis Procedure Combination (DPC) was introduced for “bundle payment” of medical expenses in Japan in 2003.25,26 The DPC was first used for acute inpatient medical care and was then introduced for hospitals with specific functions. By 2015, the DPC is used for about 55% of all general hospital beds in Japan.27 The DPC calculation determines an all-inclusive payment based on classification of the “diagnosed disease.” This is distinct from the “itemized payment”, for which the cost is calculated for each medical procedure. In general, based on the diagnosed disease determined by the MHLW, both the all-inclusive payment (injection, medication, treatment, examination, imaging diagnosis, hospitalization fee, etc) and the itemized payment (surgery, anesthesia, rehabilitation, etc) are included in the total cost. Thus, even if medications, injections, and diagnostic imaging are widely used, the all-inclusive payment does not change. However, surgery and rehabilitation expenses are calculated in an itemized manner.
There have been few previous studies of the cost of scoliosis surgery. In a retrospective review of hospital costs for surgical treatment of AIS, Kamerlink et al28 found that these costs ranged from $29 955 to $60 754, with the main contributors being implants used, intensive care unit stays, operating room time, and bone graft use. Correlations of general costs and surgery costs with reimbursement for primary surgical treatment of AIS showed that reimbursement was most closely linked with surgery costs.28 Bhat et al29 estimated an annual savings of US$11 to $20 million by changing from all pedicle screws to an alternating screw pattern, and Yang et al30 found a significant positive association between increased spending on implants per level fused and the % Cobb angle correction. However, no reports have examined the details of medical expenses determined by governments over time, such as the reimbursement price of surgical instruments and hospital administration fees.
Orthopedic surgery, and especially spinal surgery, is an implant-intensive specialty, which contributes significantly to the total cost of care. Surgeons are constantly trying to improve operative care and often recognize potentially useful adaptations in techniques or implants. Market forces are likely to continue to affect the cost of implants, and collaborative efforts among industry, individual hospitals, and institutions are needed to help curtail rising costs. In the setting of rapid and unsustainable increases in costs of care, surgeons and hospitals need to work in alignment to be aware of costs and to consider the impact of implant costs on the overall value of care. In Europe and America, competitive group pricing is a common strategy used to reduce the cost per implant.31-33 In contrast, Japan has used public health insurance since 1961, under which all people receive equal medical treatment, and reimbursements for medical materials and medical costs have been calculated by the MHLW every two years. In particular, there is no variability in the cost of surgical implants between hospitals and manufacturers in Japan, and the total medical costs that can be billed to a patient do not differ among hospitals.
In our series, trends for a slight decrease in costs such as hospital fees per day and a substantial decrease in reimbursement prices for surgical instruments reflect recent medical cost control policies of the government. However, the cost for scoliosis surgery defined by the MHLW increased by about 1.6 times in 10 years, and the proportion of surgical costs in the total treatment cost also increased. These changes may reflect the viewpoint of the MHLW in valuing advanced surgical procedures with good outcomes under current economic conditions. An investigation of the cost trends of operative spinal intervention provides a useful assessment of the treatment benefit and is likely to influence health care costs.
The average LOS in our series was 16 days, which is longer than that in most countries, in which most patients are discharged from hospital in less than 1 week. Our patients were admitted a few days before surgery for whole body screening, and hospital discharge occurred after removal of the wound suture and confirming the wound condition at about 10 days after surgery. Thus, our LOS was significantly longer than the standard LOS worldwide. There were no neurological deficits before surgery and no cases with motor deficit after surgery; therefore, the rehabilitation period was short and there was no increase in postoperative rehabilitation costs.
There are several limitations in this study. Relatively few surgeries were included because our facility is a national university hospital. In particular, the analysis focused only on AIS conducted with a posterior approach over a short period of 10 years, and with examination of hospitalization costs only, without considering outpatient clinical practice. Also, the medical costs used in the study are the total costs during hospitalization, and there is a large gap from the amount paid by the patient, who pays only a bed fee and a meal fee due to preferential treatment of pediatric patients in Japan. However, although it is difficult to investigate individual details in comprehensive medical care, this study is the first report of Japanese medical cost variability in AIS, and it may reflect the current medical economy in Japan, as the fastest aging society worldwide. Also, in a longitudinal study in one hospital, variation of confounding factors such as operating room protocols, surgical instrumentation, evolving surgical and anesthetic techniques, differences in trainee skill level, and postoperative pain regimens and rehabilitation protocols are likely to be small. Therefore, this study provides a unique contribution to the clinical experience of management of AIS.
Conclusion
This investigation of the medical costs involved in AIS surgery revealed a trend that reflects the problem of medical economics. In Japan, universal insurance is available for all people and the self-payment amount is low. Medical expenditures in Japan have increased significantly with aging, and about half of all medical expenses are paid from sources other than insurance premiums, since about half of the national budget revenue is from government bond issuance. Reduced all-inclusive payments, such as hospital administration fees per day, and a substantial decline in reimbursement prices for surgical instruments reflect recent medical cost control policies in Japan. In contrast, itemized costs related to surgery are increasing with technological advances. These competing trends provide a challenge for the health care economy, and spine surgeons need to understand medical costs, including those for surgeries. Our study of cost trends in operative spinal intervention provides an assessment of surgical benefit and is likely to influence health care costs.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Shiro Imagama, MD  https://orcid.org/0000-0003-1721-9626
https://orcid.org/0000-0003-1721-9626
References
- 1. Ministry of Health, Labour and Welfare. Outline of welfare and labor in 2017 [in Japanese]. https://www.mhlw.go.jp/wp/hakusyo/kousei/17/dl/all.pdf. Accessed October 16, 2019.
- 2. Cutler D, Wikler E, Basch P. Reducing administrative costs and improving the health care system. N Engl J Med. 2012;367:1875–1878. [DOI] [PubMed] [Google Scholar]
- 3. Oberlander J. Unfinished journey—a century of health care reform in the United States. N Engl J Med. 2012;367:585–590. [DOI] [PubMed] [Google Scholar]
- 4. Orszag PR, Emanuel EJ. Health care reform and cost control. N Engl J Med. 2010;363:601–603. [DOI] [PubMed] [Google Scholar]
- 5. Ramirez N, Johnston CE, Browne RH. The prevalence of back pain in children who have idiopathic scoliosis. J Bone Joint Surg Am. 1997;79:364–368. [DOI] [PubMed] [Google Scholar]
- 6. Smith PL, Donaldson S, Hedden D, et al. Parents’ and patients’ perceptions of postoperative appearance in adolescent idiopathic scoliosis. Spine (Phila Pa 1976). 2006;31:2367–2374. [DOI] [PubMed] [Google Scholar]
- 7. Asher M, Lai SM, Burton D, Manna B. The influence of spine and trunk deformity on preoperative idiopathic scoliosis patients’ health-related quality of life questionnaire responses. Spine (Phila Pa 1976). 2004;29:861–868. [DOI] [PubMed] [Google Scholar]
- 8. Luque ER. Segmental spinal instrumentation for correction of scoliosis. Clin Orthop Relat Res. 1982;(163):192–198. [PubMed] [Google Scholar]
- 9. Danielsson AJ, Wiklund I, Pehrsson K, Nachemson AL. Health-related quality of life in patients with adolescent idiopathic scoliosis: a matched follow-up at least 20 years after treatment with brace or surgery. Eur Spine J. 2001;10:278–288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Helenius I, Remes V, Yrjönen T, et al. Harrington and Cotrel-Dubousset instrumentation in adolescent idiopathic scoliosis. Long-term functional and radiographic outcomes. J Bone Joint Surg Am. 2003;85:2303–2309. [DOI] [PubMed] [Google Scholar]
- 11. Lenke LG, Bridwell KH, Blanke K, Baldus C, Weston J. Radiographic results of arthrodesis with Cotrel-Dubousset instrumentation for the treatment of adolescent idiopathic scoliosis. A five to ten-year follow-up study. J Bone Joint Surg Am. 1998;80:807–814. [DOI] [PubMed] [Google Scholar]
- 12. Bjerkreim I, Steen H, Brox JI. Idiopathic scoliosis treated with Cotrel-Dubousset instrumentation: evaluation 10 years after surgery. Spine (Phila Pa 1976). 2007;32:2103–2110. [DOI] [PubMed] [Google Scholar]
- 13. Kuklo TR, Potter BK, Lenke LG, et al. Surgical revision rates of hooks versus hybrid versus screws versus combined anteroposterior spinal fusion for adolescent idiopathic scoliosis. Spine (Phila Pa 1976). 2007;32:2258–2264. [DOI] [PubMed] [Google Scholar]
- 14. Ho C, Sucato DJ, Richards BS. Risk factors for the development of delayed infections following posterior spinal fusion and instrumentation in adolescent idiopathic scoliosis patients. Spine (Phila Pa 1976). 2007;32:2272–2277. [DOI] [PubMed] [Google Scholar]
- 15. Ridgeway S, Tai C, Alton P, Barnardo P, Harrison DJ. Pre-donated autologous blood transfusion in scoliosis surgery. J Bone Joint Surg Br. 2003;85:1032–1036. [DOI] [PubMed] [Google Scholar]
- 16. Copley LA, Richards BS, Safavi FZ, Newton PO. Hemodilution as a method to reduce transfusion requirements in adolescent spine fusion surgery. Spine (Phila Pa 1976). 1999;24:219–224. [DOI] [PubMed] [Google Scholar]
- 17. Neilipovitz DT, Murto K, Hall L, Barrowman NJ, Splinter WM. A randomized trial of tranexamic acid to reduce blood transfusion for scoliosis surgery. Anesth Analg. 2001;93:82–87. [DOI] [PubMed] [Google Scholar]
- 18. Schwartz DM, Auerbach JD, Dormans JP, et al. Neurophysiological detection of impending spinal cord injury during scoliosis surgery. J Bone Joint Surg Am. 2007;89:2440–2449. [DOI] [PubMed] [Google Scholar]
- 19. Fritzell P, Hägg O, Jonsson D, Nordwall A; Swedish Lumbar Spine Study Group. Cost-effectiveness of lumbar fusion and nonsurgical treatment for chronic low back pain in the Swedish Lumbar Spine Study: a multicenter, randomized, controlled trial from the Swedish Lumbar Spine Study Group. Spine (Phila Pa 1976). 2004;29:421–434. [DOI] [PubMed] [Google Scholar]
- 20. Kuntz KM, Snider RK, Weinstein JN, Pope MH, Katz JN. Cost-effectiveness of fusion with and without instrumentation for patient with degenerative spondylolisthesis and spinal stenosis. Spine (Phila Pa 1976). 2000;25:1132–1139. [DOI] [PubMed] [Google Scholar]
- 21. Lenke LG, Betz RR, Harms J, et al. Adolescent idiopathic scoliosis: a new classification to determine extent of spinal arthrodesis. J Bone Joint Surg Am. 2001;83:1169–1181. [PubMed] [Google Scholar]
- 22. Imagama S, Ito Z, Wakao N, et al. Posterior surgery for adolescent idiopathic scoliosis with pedicle screws and ultra-high molecular weight polyethylene tape: achieving the ideal thoracic kyphosis. Clin Spine Surg. 2016;29:E376–E383. [DOI] [PubMed] [Google Scholar]
- 23. Kobayashi K, Imagama S, Ito Z, et al. Transcranial motor evoked potential waveform changes in corrective fusion for adolescent idiopathic scoliosis. J Neurosurg Pediatr. 2017;19:108–115. [DOI] [PubMed] [Google Scholar]
- 24. Tannous OO, Banagan KE, Belin EJ, et al. Low-density pedicle screw constructs for adolescent idiopathic scoliosis: evaluation of effectiveness and cost. Global Spine J. 2018;8:114–120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Cromwell J, Dayhoff DA, Thoumaian AH. Cost savings and physician responses to global bundled payments for Medicare heart bypass surgery. Health Care Financ Rev. 1997;19:41–57. [PMC free article] [PubMed] [Google Scholar]
- 26. Satin DJ, Miles J. Performance-based bundled payments: potential benefits and burdens. Minn Med. 2009;92:33–35. [PubMed] [Google Scholar]
- 27. Ministry of Health, Labour and Welfare. Outline of medical treatment fee revision in 2012 [in Japanese]. https://www.mhlw.go.jp/stf/shingi/2r9852000002909e-att/2r985200000290dw.pdf. Accessed October 16, 2019.
- 28. Kamerlink JR, Quirno M, Auerbach JD, et al. Hospital cost analysis of adolescent idiopathic scoliosis correction surgery in 125 consecutive cases. J Bone Joint Surg Am. 2010;92:1097–1104. [DOI] [PubMed] [Google Scholar]
- 29. Bhat SB, Rendon N, Drummond DS, et al. Cost analysis of implants for surgical correction of scoliosis: implications of construct design. Poster presented at the American Academy of Orthopaedic Surgeons (AAOS) 2012 Annual Meeting; February 7-11, 2012; San Francisco, CA. [Google Scholar]
- 30. Yang S, Jones-Quaidoo SM, Eager M, et al. Right adolescent idiopathic thoracic curve (Lenke 1 A and B): does cost of instrumentation and implant density improve radiographic and cosmetic parameters? Eur Spine J. 2011;20:1039–1047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Paulus MC, Kalantar SB, Radcliff K. Cost and value of spinal deformity surgery. Spine (Phila Pa 1976). 2014;39:388–393. [DOI] [PubMed] [Google Scholar]
- 32. Pahlavan S, Berven S, Bederman SS. Variation in costs of spinal implants in united states academic medical centers. Spine (Phila Pa 1976). 2016;41:515–521. [DOI] [PubMed] [Google Scholar]
- 33. Larson AN, Polly DW, Jr, Ackerman SJ, et al. Minimize Implants Maximize Outcomes Study Group. What would be the annual cost savings if fewer screws were used in adolescent idiopathic scoliosis treatment in the US? J Neurosurg Spine. 2016;24:116–123. [DOI] [PubMed] [Google Scholar]