Abstract
Glycemic control in type 1 diabetes mellitus (T1DM) remains a challenge for many, despite the availability of modern diabetes technology. While technologies have proven glycemic benefits and may reduce excess mortality in some populations, both mortality and complication rates remain significantly higher in T1DM than the general population. Diabetes technology can reduce some burdens of diabetes self-management, however, it may also increase anxiety, stress, and diabetes-related distress. Additional workload associated with diabetes technologies and the dominant focus on metabolic control may be at the expense of quality-of-life. Diabetes is associated with significantly increased risk of suicidal ideation, self-harm, and suicide. The risk increases for those with diabetes and comorbid mood disorder. For example, the prevalence of depression is significantly higher in people with diabetes than the general population, and thus, people with diabetes are at even higher risk of suicide. The Center for Disease Control and Prevention reported a 24% rise in US national suicide rates between 1999 and 2014, the highest in 30 years. In the United Kingdom, 6000 suicides occur annually. Rates of preventable self-injury mortality stand at 29.1 per 100 000 population. Individuals with diabetes have an increased risk of suicide, being three to four times more likely to attempt suicide than the general population. Furthermore, adolescents aged 15 to 19 are most likely to present at emergency departments for self-inflicted injuries (9.6 per 1000 visits), with accidents, alcohol-related injuries, and self-harm being the strongest risk factors for suicide, the second leading cause of death among 10 to 24 year olds. While we have developed tools to improve glycemic control, we must be cognizant that the psychological burden of chronic disease is a significant problem for this vulnerable population. It is crucial to determine the psychosocial and behavioral predictors to uptake and continued use of technology in order to aid the identification of those individuals most likely to realize benefits of any intervention as well as those individuals who may require more support to succeed with technology.
Keywords: diabetes, suicide, self-inflicted injury, self-harm
Background
Suicide and Self-inflicted Injury
Suicide is the leading cause of death among young people aged 20 to 34.1,2 In addition to depression, other risk factors include other psychiatric disorders, somatic diseases, past history of self-harm, family breakdown, violence, poor social conditions, poverty, imprisonment, unemployment, and social isolation.1 Men are more likely to commit suicide than women, with approximately three times as many men dying as a result of suicide compared to women.1 One reason mooted being that they are less likely to ask for help or talk about depressive or suicidal feelings.1 Talking about suicide remains highly stigmatized. The isolation that suicidal people feel can be reinforced by a judgmental approach in which their behavior is viewed as manipulative or selfish.3
The Center for Disease Control and Prevention reported in 2016 a 24% rise in the US national suicide rate between 1999 and 2014.4 Currently at a rate of 13 in 100 000 people, the US suicide rate is the the highest in 30 years.5 In the United Kingdom, almost 6000 suicides occurred in 2017 representing a small change on 2016 figures of 5965.6 Suicide risk for those with chronic health conditions is widely reported to be significantly higher than for people in the general population, with the risk in diabetes being approximately three to four times higher.7-9 In the general population, the intentional self-inflected injury presents two sides; it has a high in-hospital mortality, low mortality postdischarge, but then high recidivism rates. Thus, suicide risk increases following hospital discharge in psychiatric patients or those admitted for self-harm.10,11 The rates of self-harm and suicide could be underestimated in those with T1DM as each year large numbers of patients with diabetes present to emergency departments with hypoglycemic episodes of “unknown” etiology.12 It is possible that a significant proportion of them could be intentional overdoses.12 Data from one study of 160 cases of insulin overdose show that 90% were either suicidal or parasuicidal, whereas only 5% of cases were deemed accidental.12 Death certificates or International Classification of Diseases codes are used to determine causes of death; however, these may be unreliable in adult patients with T1DM.13
Diabetes and Self-inflicted Injury/Suicide
Glycemic control in T1DM remains a challenge for many, despite the availability of modern insulin analogs,14 the improving accuracy of glucose monitoring,15,16 and advances in diabetes technologies with the widening use of intensive insulin therapy. While new technologies have proven benefits in avoiding diabetes-related complications17 and may have reduced excess mortality in some populations,18 both mortality and complication rates remain significantly higher in T1DM when compared to the general population.19,20 Furthermore, the additional workload associated with diabetes technologies and the dominant focus on glycemic control, at the expense of quality of life, serves to increase the burden of diabetes for many.
A systematic review by Pompii et al21 reported that individuals with diabetes have an increased risk of suicide than the general population. In addition, diabetes is known to be associated with greater suicidal ideation.21 People with diabetes show greater hopelessness and greater rates of depression. This high suicide risk is present across ethnic diversities within diabetes, for example, African-American patients with T1DM are also reported to be three to four times more likely to attempt suicide than those without diabetes (13.3% vs 3.5%).22 In the general population, among suicide survivors, 7% eventually succeed, 23% reattempt with nonfatal consequences, and 70% never reattempt.23 In the United States, intentional self-harm (ISI) is the tenth leading cause of death. ISI includes both, suicidal and nonsuicidal self-injury such as cutting, burning, head banging, scratching, asphyxiation, poisoning, and self-hitting.24,25 There are also associated financial consequences, for example, there were 44 965 suicides in 2016 costing about $11.8 billion loss in productivity26,27 not counting the cost of emergency room visits for nonsuicidal intentional self-inflicted injury (ISI). Such incidents saw a dramatic increase between 2001 and 2016 of 42%.28
Statistics showed that there are 800 000 suicide deaths annually worldwide,29 half of them with prior ISI.30 Adolescents aged 15 to 19 are most likely to present at emergency departments for self-inflicted injuries (9.6 per 1000 visits),31 self-harm being one of the strongest risk factors for suicide, the second leading cause of death among 10 to 24 year olds. Risks of self-inflicted injury for those with chronic health conditions are significantly higher, with risk in diabetes approximately doubled.7-9 Compared with the unaffected individuals, those with type 1 diabetes had a higher standardized mortality ratio (SMR) relating to this outcome: in women, the SMR was 2.53 (95% CI 1.65-3.89), and in men, 1.80 (1.32-2.47).32
Ferro et al33 report that mood disorder moderates the association between chronic illness and suicidal thoughts (odds ratio = 1.89 [1.06-5.28]). For those without mood disorder, with or without chronic illness, the probability of reporting suicidal thoughts is low and stable. Among participants with both mood disorder and chronic illness, the probability of suicidal thoughts is significantly greater than those with mood disorder and no chronic illness. The authors call for attention to the need to address the problem of suicidal thoughts and behavior among vulnerable adolescents and young adults with a chronic illness.
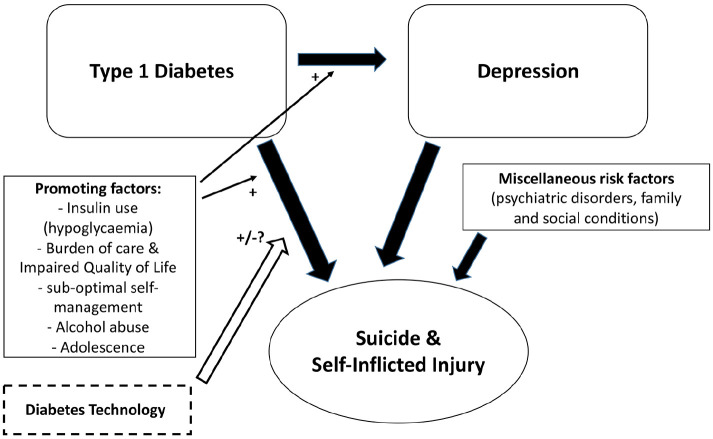
The relationship between suicide and diabetes is complex and multifaceted (Figure 1). Deaths related to diabetes including self-harm and suicide, like in the general population, are more prominent in decreased urbanization (ie, rural areas), high poverty, and lower health provider density.34 In the general population, depression is highly correlated with suicidal ideation35 and suicide attempt. In chronic diseases, suicidal risk increases with poor quality of life and general functioning, as well as the presence of chronic pain. Both depression and diabetes contribute to these features. Individuals with T1DM have significantly higher rates of depression than those without T1DM.36 In the general population, suicidal ideation is associated with negative outcomes such as distress, psychiatric comorbidity,35 and increased health service utilization.37 All of which are more common in people with diabetes. Among those with T1DM, suicidal ideation is associated with serious noncompliance with the medical regimen37; however, as in depression and diabetes, the direction of the relationship is unclear.
Figure 1.
Complexity of relationship between type 1 diabetes, depression, and suicide/self-injury.
In response to the 2017 US Preventive Services Task Force recommendation for routine depression screening, Myers et al38 argued that people with diabetes should be screened for suicidal ideation in the presence of a mood disorder as suicide could be more “easily achieved” due to the access of this population to potential lethal medication such as insulin. Those with T1DM must adapt to age-related life transitions, while also dealing with the demands of diabetes and these stressors may have long-term consequences on depression and overall wellbeing.38 This can be most difficult in the adolescent period, where normal physical and psychological development occur and greater diabetes distress and depression are seen.39,40 Adolescents and young adults with T1DM have 61% higher odds of reporting suicidal thoughts than those without diabetes.36 The risk for suicide attempts is highest soon after young people are diagnosed with chronic illness. Such suicidal ideation has been identified as one of the strongest predictors of suicide behaviors and completion.41 The 2012 National Strategy for Suicide Prevention promotes healthcare settings as one of the most promising and critical environments to implement suicide prevention practices.42
In suicide victims with T1DM, insulin as a suicide method covered half of the self-poisoning cases (mostly male), while the proportion in those with type 2 diabetes mellitus (T2DM) was 13%.7 This perhaps reflects the availability of such a potentially lethal drug as insulin to different cohorts. Alcohol further increases the risk of hypoglycemia in the multifactorial process of suicide among diabetes patients. Alcohol was a factor in 24.5% of victims with T2DM being under the influence of alcohol when they died, compared to 44.4% in type 1 diabetes and 46.6% of those without diabetes (P = .007).43 The authors recommended that physicians who treat diabetes patients should evaluate co-occurring depression and substance abuse, both of which are major risk factors of suicide. Self-poisoning, especially with insulin, was the most common method of suicide among those with type 1 diabetes. In one study,44 victims with T1DM suffered more commonly from depression (44.4%) than those with T2DM (23.5%) or those without diabetes (19.9%) (P = .006) and chose self-poisoning as their suicide method (48.1% vs 31.4% and 18.0%, respectively, P ≤ .001).
It is further noted in the literature that during adolescence, insulin omission and suboptimal diabetes care can be seen as a form of self-inflicted injuries. Suicidal ideations caused by depressive state due to diabetes and self-inflicted injury or suicide can also be underreported at this age.37 Risks are increased for adolescents with diabetes as access to insulin makes the adolescent population with diabetes more vulnerable than the general teenager population that may suffer the same mood disorders that accompany this stage of life.45
Diabetes and Technologies
The use of diabetes technologies to support self-management has increased rapidly, particularly among pediatric population. The 2016 to 2017 National Paediatric Diabetes Audit of children and young people in England and Wales reports 32.2% pump use among this population.46 This contains considerable variability, with 45.7% of 0 to 4 year olds using pumps compared to only 27% of 15 to 19 year olds. Notwithstanding, these numbers reflect a rapid increase in pump use among children and young people from 8% in 2011. The usage numbers for adults with T1DM have grown more slowly with 15.6% use in 2016 to 2017, up from less than 2% use in 2011.47 In the United States, in T1D Exchange Registry, insulin pump use increased from 57% to 63% and CGM use increased from 7% to 30% from 2010 to 2018, respectively.48 There are no official figures for continuous glucose monitor use, however, it is estimated that approximately 10% of people with T1DM use this technology in the United Kingdom currently. The use of flash glucose monitoring is increasing, driven in part by a campaign to force all commissioning groups to provide this technology for free as part of National Health Service provision. Abbott reported in January 2019 that there are 200 000 users of the FreeStyle Libre system in the United States, with a further 800 000 users globally.49
Despite the advancement of technologies and reliable measures of diabetes distress, there remains no routine intervention in clinical care to alleviate distress and improve quality of life.50 The psychosocial sequelae of diabetes have been recognized in a number of UK and international guidelines that have set out the standards of care that people with diabetes should expect; however, there remains a gulf in the provision of psychological care, with widespread evidence of poor service despite clinical need.51 Structured education programs have been developed and tested in a systematic manner, widely shown to be cost-effective but implementation remains challenging with availability and uptake poor.52 Diabetes and its treatment contribution can be burdensome and it is interesting to note that suicides occur in people using diabetes technologies as well as those who do not. It has long been argued that treatments as well as disease can negatively impact quality of life and it would appear that diabetes technologies are no different.
Psychological and Behavioral Factors
In addition to patients’ perceptions rooted in their previous experience, unrealistic expectations of technologies may lead to disappointment and discontinuation of the device. General “tech savviness” can also play a role in acceptance in that those more familiar and comfortable with technology may be more willing to trust the system. Furthermore, the time and effort required to invest in building device-related skills, trust, and acceptance may be underestimated (and often is), as these range from technical handling to integrating the system information into one’s diabetes self-management and everyday living without intrusive disruptions.
Therefore, psychological and behavioral factors play a critical role in the acceptance of diabetes technologies and the trust users put in them. It is crucial to determine the psychosocial and behavioral predictors to uptake and continued use of technology in order to aid the identification of those individuals most likely to realize benefits of any intervention as well as those individuals who may require more support to succeed with technology. Additional individual user characteristics (eg, diabetes belief systems and self-management skills) may be predictive of technology acceptance, trust, use, and benefit. At present, little is known about psychological, behavioral, and social factors that contribute to diabetes technology adoption and successful use.
While the psychological burden of diabetes may lead to the increased risk of depression, it does not fully account for it. Some common risk factors (low socioeconomic status, irregular sleep patterns, lack of physical activity, and poor diet) may play an important role in activating common physiological pathways (stress and inflammation systems) that promote and reinforce diabetes and depression.
MRI scanning of the brains of people with type 1 diabetes has shown that prefrontal glutamate-glutamine-gamma-aminobutyric acid levels are higher than in healthy control subjects, and these levels correlate with mild depressive symptoms.53 Decreased treatment adherence in patients with T1DM may reflect impairments in decision-making and underlying associated deficits in working memory and executive functioning.54
Beyond depression, diabetes and suicidal risk may share pathways that may participate in their co-occurrence. First, cognitive impairments (particularly decision making) reported in diabetes have also been shown in individuals without diabetes having a past history of suicide attempt independent of depression.55 Second, certain factors (low socioeconomic status, irregular sleep patterns, and lack of physical activity) may play an important role in activating common physiological pathways (stress and inflammation systems) that reinforce diabetes and depression.56 Third, growing evidence shows the specific involvement of HPA axis impairment and inflammation in suicidal vulnerability. For example, C-reactive protein levels are increased in suicide attempters independent of sociodemographic factors and presence of chronic diseases.57
Pompili et al reported that diabetes is associated with an increased risk of suicide, independently from the severity of depressive condition, and that a perceived poor quality of life was related to low self-efficacy, high hopelessness, and suicidality.58 Indeed, a hopeless feeling regarding the illness might be associated with risk of suicide attempts, and also with neglect of health care and lack of motivation to adhere to medical instructions.59
Factors related to personality and individual differences are of interest because they are affected by the environment, and affect cognition and emotion, and because some common features seem as well to represent both vulnerability traits of suicidal behavior as to influence the course of the diabetes. For instance, individual differences in self-regulatory capacity (eg, executive function and emotion regulation skills) are associated with diabetes management during late adolescence60,61 and may affect both self- and social-regulation processes. Otherwise, recent psychological models of suicidal behavior emphasize the role of hopelessness, impulsivity, perfectionism, problem-solving ability, cognitive rigidity, and belongingness and burdensomeness.62
Thus, further research is needed to identify factors predicting depression and suicide, comparing biological (inflammation), cognitive and psychological (family and individual), and environmental (particularly sensitivity to social adversity) risk factors in large population-based prospective cohorts of patients with type 1 diabetes who would be, or would not be, candidate for new diabetes technologies. One may hypothesize that people who would receive such technologies may be an enriched population in risk factors of suicidal behavior, common to poor management of diabetes. In this case, personalized psychological and social management should be implemented in association with diabetes technologies.
With the evolution of diabetes technology, type 1 diabetes management in the 21st century is becoming ever more patient-centered. Personalized, ongoing education, as well as psychological and social support, can be delivered through telemedicine, mobile apps, and online modules.63,64
Support Opportunities
If appropriate and timely help and emotional support is offered to people who are experiencing deep unhappiness and distress, this can reduce the risk self-harm. An empathic approach and being open to understanding suicide and suicidal ideation can help those at risk by letting them know that it is okay for them to share. As such, the prevention of suicide is not the exclusive responsibility of any one sector of society. Healthcare professionals, as well as family members or friends, can all play a part in recognizing and reducing the risks. Constructively challenging personal assumptions regarding self-harm and suicidal behaviors and showing care and respect for those individuals at risk of suicide can provide opportunities to share feelings and help prevent such events. It is argued that suicide is recognized as a major public health issue more prevalent in the diabetes population and that studies reducing rate of self-injury (suicide) attempts should be given high priority.
Conclusion
Despite all advances in diabetes care in recent years, diabetes burden still impacts lives for people living with diabetes. Developing screening strategies for self-harm and suicide to identify patients with diabetes at risk and provide prompt referral and evaluation of these to a certified psychologist or psychiatrist is essential. Data from diabetes technologies may be a tool for identifying those at risk.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iDs: Katharine D. Barnard-Kelly  https://orcid.org/0000-0002-3888-3123
https://orcid.org/0000-0002-3888-3123
Diana Naranjo  https://orcid.org/0000-0001-8039-0616
https://orcid.org/0000-0001-8039-0616
Halis K. Akturk  https://orcid.org/0000-0003-4518-5179
https://orcid.org/0000-0003-4518-5179
Eric Renard  https://orcid.org/0000-0002-3407-7263
https://orcid.org/0000-0002-3407-7263
References
- 1. Office for National Statistics (2017). Suicides in the UK: 2016 Registrations. https://www.ons.gov.uk/peoplepopulationandcommunity/birthsdeathsandmarri. . . Accessed January 10, 2019.
- 2. Centers for Disease Control and Prevention. Preventing Suicide. CDC 24/7: Saving Lives, Protecting People. https://www.cdc.gov/violenceprevention/suicide/fastfact.html. Accessed July 30, 2019.
- 3. Batterham P, Calear A, Christensen H. The stigma of suicide scale. Crisis. 2013;34(1):13-21. [DOI] [PubMed] [Google Scholar]
- 4. Curtin SC, Warner M, Hedegaard H. Increase in Suicide in the United States 1999-2014. Hyattsville, MD: National Center for Health Statistics CDC; 2016. [Google Scholar]
- 5. Ahmedani BK, Peterson EL, Yong Hu, et al. Major physical health conditions and risk of suicide. Am J Prev Med. 2017;53(3):308-315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Mental Health Foundation. Thousands of people in the UK end their lives by suicide each year. Suicide, September 2018. www.mentalhealth.org.uk/a-to-z/s/suicide. Accessed December 28, 2018.
- 7. Lofman S, Hakko H, Mainio A, Timonen M, Rasanen P. Characteristics of suicide among diabetes patients: a population based study of suicide victims in Northern Finland. J Psychosom Res. 2012;73(4):268-271. [DOI] [PubMed] [Google Scholar]
- 8. Pompii M, Forte A, Lester D, et al. Suicide risk in type 1 diabetes mellitus: a systematic review. J Psychosom Res. 2014;76(5):352-360. [DOI] [PubMed] [Google Scholar]
- 9. Fuller-Thomson E, Sawyer J-L. Lifetime prevalence of suicidal ideation in a representative sample of Canadians with type 1 diabetes. Diabetes Res Clin Pract. 2009;83(1):e9-e11. [DOI] [PubMed] [Google Scholar]
- 10. Townsend E. Time to take self-harm in young people seriously. Lancet Psy. 2019;6(4):279-280. [DOI] [PubMed] [Google Scholar]
- 11. Large MM, Chung DT, Davidson M, Weiser M, Ryan CJ. In-patient suicide: selection of people at risk, failure of protection and the possibility of causation. Br J Psychiatry Open. 2017;3(3):102-105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Russell KS, Stevens JR, Stern TA. Insulin overdose among patients with diabetes: a readily available means of suicide. Prim Care Companion J Clin Psychiatry. 2009;11(5):258-262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Muhlhauser I, Sawicki PT, Blank M, Overmann H, Richter B, Berger M. Reliability of causes of death in persons with type 1 diabetes. Diabetologia 2002;45 (11):1490-1497. [DOI] [PubMed] [Google Scholar]
- 14. Hirsch IB. Insulin analogues. N Engl J Med. 2005;352(2):174-183. [DOI] [PubMed] [Google Scholar]
- 15. Klonoff DC, Prahalad P. Performance of cleared blood glucose monitors. J Diabetes Sci Technol. 2015;9(4):895-910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Castle JR, Jacobs PG. Nonadjunctive use of continuous glucose monitoring for diabetes treatment decisions. J Diabetes Sci Technol. 2016;10(5):1169-1173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Diabetes Control and Complications Trial. Intensive diabetes treatment and cardiovascular disease in patients with type 1 diabetes. N Engl J Med. 2005;2005(353):2643-2653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Secrest AM, Becker DJ, Kelsey SF, LaPorte RE, Orchard TJ. All-cause mortality trends in a large population-based cohort with long-standing childhood-onset type 1 diabetes. Diabetes Care. 2010;33(12):2573-2579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Lind M, Svensson AM, Kosiborod M, et al. Glycemic control and excess mortality in type 1 diabetes. N Engl J Med. 2014;371(21):1972-1982. [DOI] [PubMed] [Google Scholar]
- 20. Nishimura R, LaPorte RE, Dorman JS, et al. Mortality trends in type 1 diabetes. Diabetes Care. 2001;24(5):823-827. [DOI] [PubMed] [Google Scholar]
- 21. Pompii M, Forte A, Lester D, et al. Suicide risk in type 1 diabetes mellitus: a systematic review. J Psychosom Res. 2014;76(5):352-360. [DOI] [PubMed] [Google Scholar]
- 22. Roy A, Roy M, Janal M. Suicide attempts and ideation in African-American type 1 diabetic patients. Psychiatry Res. 2010;179(1):53-56. [DOI] [PubMed] [Google Scholar]
- 23. Owens D, Horrocks J, House A. Fatal and non-fatal repetition of self-harm. Systemic review. Br J Psychiatry. 2002;181:193-199. [DOI] [PubMed] [Google Scholar]
- 24. Cipriano A, Cella S, Cotrufo P. Nonsuicidal self-injury: a systemic review. Front Psychol. 2017;8:1946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Hedegaard H, Schoenbaum M, Claassen C, Crosby A, Holland K, Proescholdbell S. Issues in developing a surveillance case definition for nonfatal suicide attempt and intentional self-harm using International Classification of Diseases, Tenth Revision, Clinical Modification (ICD-10-CM) coded data. National Health Statistic Reports; no 108. Hyattsville, MD: National Center for Health Statistics; 2018. https://www.cdc.gov/nchs/data/nhsr/nhsr108.pdf [PubMed] [Google Scholar]
- 26. Xu J, Murphy SL, Kochanek MA, Bastian B, Arias E; Deaths: Final Data for 2016. National Vital Statistics Reports; vol. 67, no 5 Hyattsville, MD: National Center for Health Statistics; 2018. https://www.cdc.gov/nchs/data/nvsr/nvsr67/nvsr67_05.pdf [PubMed] [Google Scholar]
- 27. Goldsmith K, Pellmar TC, Kleinman AM, Bunney WE. Reducing Suicide: A National Imperative. Washington, DC: The National Academies Press; 2002. https://www.nap.edu/catalog/10398/reducing-suicide-a-national-imperative [PubMed] [Google Scholar]
- 28. Stone DM, Simon TR, Fowler KA, et al. Vital signs: trends in state suicide rates — United States, 1999–2016 and circumstances contributing to suicide — 27 states, 2015. MMWR Morb Mortal Wkly Rep. 2018;67(22):617-624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. World Health Organization. Preventing Suicide: A Global Imperative. https://www.who.int/mental_health/suicide-prevention/world_report_2014/en/. Accessed 19 November 2019.
- 30. Cooper J, Kapur N, Webb R, et al. Suicide after deliberate self-harm: a 4-year cohort study. Am J Psychiatry. 2005;162(2):297-303. [DOI] [PubMed] [Google Scholar]
- 31. Mercado MC, Holland K, Leemis RW, et al. Trends in emergency department visits for nonfatal self-inflicted injuries among youth aged 10-24 years in the United States, 2001-2015. JAMA. 2017;318(19):1931-1933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Huxley RR, Peters SA, Mishra GD, Woodward M. Risk of all-cause mortality and vascular events in women versus men with type 1 diabetes: a systematic review and meta-analysis. Lancet Diabetes Endocrinol. 2015;3(3):198-206. [DOI] [PubMed] [Google Scholar]
- 33. Ferro MA, Rhodes AE, Kimber M, et al. Suicidal behaviour among adolescents and young adults with self-reported chronic illness. Can J Psychiatry. 2017;62(12):845-853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. El-Menyar A, Mekkodathil A, Al-Thani H. Traumatic injuries in patients with diabetes mellitus. J Emerg Trauma Shock. 2016;9(2):64-72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Godney RD. Suicidal ideation in a random community sample: attributable risk due to depression and psychosocial and traumatic events. Aust N Z J Psychiatry. 2000;34(1):98. [DOI] [PubMed] [Google Scholar]
- 36. Barnard K, Skinner T, Pevelar R. The prevalence of co-morbid depression in adults with type 1 diabetes: systematic literature review. Diabet Med. 2006;23(4):445-448. [DOI] [PubMed] [Google Scholar]
- 37. Goldston DB. Suicidal ideation and behavior and noncompliance with the medical regimen among diabetic adolescents. J Am Acad Child Adolesc Psychiatry. 1997;36(11):1528. [DOI] [PubMed] [Google Scholar]
- 38. Myers AK, Triverdi MH. Death by insulin: management of self-harm and suicide in diabetes managements. Curr Diabetes Rev. 2017;13(3):251-262. [DOI] [PubMed] [Google Scholar]
- 39. Haggar V, Hendriekx C, Sturt J, Skinner T, Speight J. Diabetes distress among adolescents with type 1 diabetes: a systematic review. Curr Diab Rep. 2016;16(1):9. [DOI] [PubMed] [Google Scholar]
- 40. Hood K, Huestis S, Maher A, Butler D, Volkening L, Laffel L. Depressive symptoms in children and adolescents with type 1 diabetes. Diabetes Care. 2006;29(6):1389-1389. [DOI] [PubMed] [Google Scholar]
- 41. Nielson B. Attempted suicide in Denmark. IV. A five-year follow-up. Acta Psychiatrica Scandinavica. 1990;81(3):250. [DOI] [PubMed] [Google Scholar]
- 42. Ahmedani BK, Vannoy S. National pathways for suicide prevention and health services research. Am J Prev Med. 2014;47(3 suppl 2):S222-S228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Niskanen L, Partonen T, Auvinen A, Haukka J. Excess mortality in Finnish diabetic subjects due to alcohol, accidents and suicide: a nationwide study. Eur J Endocrinol. 2018;179(5):299-306. [DOI] [PubMed] [Google Scholar]
- 44. Rockett IRH, Caine ED, Connery HS, Greenfield SF. Mortality in the United States from self-injury surpasses diabetes: a prevention imperative.2019;25(4):331-333. Inj Prev. doi: 10.1136/injuryprev-2018-042889. [DOI] [PubMed] [Google Scholar]
- 45. Goldston DB, Kovacs M, Ho VY, Parrone PL, Stiffler LJ. Suicidal ideation and suicide attempts among youth with insulin-dependent diabetes mellitus. Am Acad Child Adolesc Psychiatry. 1994;33(2):240-246. [DOI] [PubMed] [Google Scholar]
- 46. Rockett IRH, Caine ED, Connery HS, Greenfield SF. Mortality in the United States from self-injury surpasses diabetes: a prevention imperative. Inj Prev. 2019;25(4):331-333. [DOI] [PubMed] [Google Scholar]
- 47. National Diabetes Audit Report 1 – Findings and Recommendations 2016-2017. https://digital.nhs.uk/data-and-information/publications/statistical/national-diabetes-audit/national-diabetes-audit-report-1-findings-and-recommendations-2016-17. Accessed August 7, 2019.
- 48. Foster NC, Beck RW, Miller KM, et al. State of type 1 diabetes management and outcomes from the T1D exchange in 2016-2018. Diabetes Technol Ther. 2019;21(2):66-72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Morgan JP. 37th Annual J.P. Morgan Healthcare Conference; January 7–10, 2019; San Francisco, California, JPMorgan Chase & Co. [Google Scholar]
- 50. Naranjo D, Tanenbaum ML, Iturralde E, Hood KK. Diabetes technology: uptake, outcomes, barriers, and the intersection with distress. J Diabetes Sci Technol. 2016;10(4):852-858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Barnard KD, Lloyd CE, Dyson PA, et al. Kaleidoscope model of diabetes care: time for a rethink? Diabetic Med. 2014;31(5):522-530. [DOI] [PubMed] [Google Scholar]
- 52. Kovacs BK, Nicolucci A, Holt RIG, et al. Second diabetes attitudes, wishes, and needs (DAWN2) study: cross-national benchmarking indicators for family members living with people with diabetes. Diabet Med. 2013;30(7):778-788. [DOI] [PubMed] [Google Scholar]
- 53. Lyoo IK, Yoon SJ, Musen G, et al. Altered prefrontal glutamate-glutamine-gamma-aminobutyric acid levels and relation to low cognitive performance and depressive symptoms in type 1 diabetes mellitus. Arch Gen Psychiatry. 2009;66(8):878-887. [DOI] [PubMed] [Google Scholar]
- 54. Rustad JK, Musselman DL, Skyler JS, et al. Decision-making in diabetes mellitus type 1. J Neuropsychiatry Clin Neurosci. 2013;25(1):40-50. [DOI] [PubMed] [Google Scholar]
- 55. Jollant F, Bellivier F, Leboyer M, et al. Impaired decision making in suicide attempters. Am J Psychiatry. 2005;162(2):304-310. [DOI] [PubMed] [Google Scholar]
- 56. Agardh E, Allebeck P, Hallqvist J, Moradi T, Sidorchuk A. Type 2 diabetes incidence and socio-economic position: a systematic review and meta-analysis. Int J Epidemiol. 2011;40(3):804-818. [DOI] [PubMed] [Google Scholar]
- 57. Moulton CD, Pickup JC, Ismail K. The link between depression and diabetes: the search for shared mechanisms. Lancet Diabetes Endocrinol. 2015;3(6):461-471. [DOI] [PubMed] [Google Scholar]
- 58. Pompili M, Lester D, Innamorati M, et al. Quality of life and suicide risk in patients with diabetes mellitus. Psychosomatics. 2009;50(1):16-23. [DOI] [PubMed] [Google Scholar]
- 59. Radobuljac MD, Bratina NU, Battelino T, Tomori M. Lifetime prevalence of suicidal and self-injurious behaviors in a representative cohort of Slovenian adolescents with type1 diabetes. Pediatr Diabetes. 2009;10(7):424-431. [DOI] [PubMed] [Google Scholar]
- 60. Berg CA, Wiebe DJ, Suchy Y, et al. Individual differences and day-to-day fluctuations in perceived self-regulation associated with daily adherence in late adolescents with type 1 diabetes. J Pediatr Psychol. 2014;39(9):1038-1048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Suchy Y, Turner SL, Queen TL, et al. The relation of questionnaire and performance-based measures of executive functioning with type 1 diabetes outcomes among late adolescents. Health Psychol. 2016;35(7):661-669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. O’Connor RC, Nock MK. The psychology of suicidal behaviour. Lancet Psychiatry. 2014;1(1):73-85. [DOI] [PubMed] [Google Scholar]
- 63. Prahalad P, Tanenbaum M, Hood K, Maahs DM. Diabetes technology: improving care, improving patient-reported outcomes and preventing complications in young people with Type 1 diabetes. Diabet Med. 2018;35(4):419-429. [DOI] [PubMed] [Google Scholar]
- 64. Peis I, M Olmos P, Vera-Varela C, et al. Deep sequential models for suicidal ideation from multiple source data. IEEE J Biomed Health Inform. 2019;23(6):2286-2293. doi: 10.1109/JBHI.2019.2919270. [DOI] [PubMed] [Google Scholar]