Abstract
Background
Public health measures were instituted to reduce COVID-19 spread. A decrease in total emergency department volume followed, but the impact on injury is unknown. With lockdown and social distancing potentially increasing domicile discord, we hypothesized that intentional injury increased during COVID-19, driven primarily by an increase in penetrating trauma.
Study Design
A retrospective review of acute adult patient care in an urban Level I trauma center assessed injury patterns. Presenting patient characteristics and diagnoses from 6 weeks pre to 10 weeks post statewide stay-at-home orders (March 16, 2020) were compared, as well as with 2015-2019. Subsets were defined by intentionality (intentional vs nonintentional) and mechanism of injury (blunt vs penetrating). Fisher exact and Wilcoxon tests were used to compare proportions and means.
Results
There were 357 trauma patients that presented pre stay-at-home order and 480 that presented post stay-at-home order. Pre and post groups demonstrated differences in sex (35.6% vs 27.9% female; p = 0.02), age (47.4 ± 22.1 years vs 42 ± 20.3 years; p = 0.009), and race (1.4% vs 2.3% Asian; 63.3% vs 68.3% Black; 30.5% vs 22.3% White; and 4.8% vs 7.1% other; p = 0.03). Post stay-at-home order mechanism of injury revealed more intentional injury (p = 0.0008). Decreases in nonintentional trauma after adoption of social isolation paralleled declines in daily emergency department visits. Compared with earlier years, 2020 demonstrated a significantly greater proportion of intentional violent injury during the peripandemic months, especially from firearms.
Conclusions
Unprecedented social isolation policies to address COVID-19 were associated with increased intentional injury, especially gun violence. Meanwhile, emergency department and nonintentional trauma visits decreased. Pandemic-related public health measures should embrace intentional injury prevention and management strategies.
Abbreviations and Acronyms: ED, emergency department; ISS, Injury Severity Score; IVT, intentional or violent trauma; MOI, mechanism of injury; MVC, motor vehicle crash; NIT, nonintentional trauma; PPMC, Penn Presbyterian Medical Center; SAHO, stay-at-home order
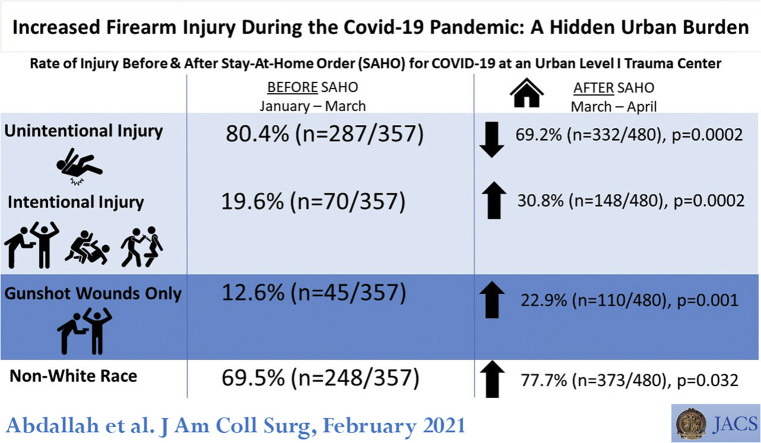
Graphical abstract
Continuing Medical Education Credit Information.
Accreditation: The American College of Surgeons is accredited by the Accreditation Council for Continuing Medical Education (ACCME) to provide continuing medical education for physicians.
AMA PRA Category 1 CreditsTM: The American College of Surgeons designates this journal-based CME activity for a maximum of 1 AMA PRA Category 1 Credit™. Physicians should claim only the credit commensurate with the extent of their participation in the activity.
Of the AMA PRA Category 1 Credits™ listed above, a maximum of 1 credits meet the requirement for Self-Assessment.
In October 2019, reports began emerging from Wuhan, China about a novel coronavirus that could result in severe respiratory failure. It was not until late February 2020 to early March 2020 that the gravity of this situation became clear and US public health initiatives emerged to address the crisis.1, 2, 3 Fund reallocation and lockdown practices as directed by stay-at-home orders (SAHOs) were instituted in several states in March 2020. Pennsylvania declared a state of emergency on March 6, 2020 and issued an SAHO on March 16, 2020.4, 5, 6, 7
The Pennsylvania SAHO effectively cancelled elective procedures and severely curtailed inpatient and outpatient medical visits to increase hospital capacity to care for COVID-19 patients and reduce viral spread by limiting contact in high-risk locations.8 , 9 Concurrently, emergency department (ED) visits nationwide declined abruptly, a trend noted globally as well.10, 11, 12, 13, 14, 15, 16 The decline in ED visits was ascribed to patient fear of contracting SARS-CoV-2 infection—a fear that seemed unimpacted by nonviral acute illness. Mandated SAHOs along with unprecedented levels of unemployment might have impacted these behavioral changes.17 Although decreases in presentations of acute non-injury-related illness were reported, it was less clear whether injury-related ED visits would decrease in parallel.
With the pandemic surge, anecdotal lay press reports noted increases in intentional or violent trauma (IVT), such as firearm violence, stabbings, and assaults.18, 19, 20 Some attempted to link locations with increases in IVT to locally high rates of successful social distancing and isolation, including in Philadelphia.21, 22, 23, 24 Nationwide, as government officials trend rates of both crash and violent injury,25 , 26 such data can guide adaptations of policy, healthcare access, and public health measures.
We therefore sought to evaluate the incidence of trauma and nontrauma patients presenting to the ED of an urban, metropolitan, Level I trauma center during the COVID-19 crisis. We hypothesized that although acute care ED use declined, intentional injury care—and specifically firearm-related injury care—would increase.
Methods
Institution and data
Approval for this study was secured from the University of Pennsylvania’s Office of Regulatory Affairs IRB. A retrospective trauma and ED registry review evaluated patients presenting for emergency care to Penn Presbyterian Medical Center (PPMC), 1 of 4 Level I adult trauma centers in Philadelphia County that is underpinned by ground ambulance, air ambulance, and police drop-off services to transport injury care.
The PPMC trauma registry follows strict state requirements articulated by the Pennsylvania Trauma Outcomes Systems Foundation with dedicated registrars who collect admitted patient data daily. The PPMC ED database provides basic demographic characteristics for all ED patients, including data from all visits, discharges, and admissions. Abstracted data included demographics (age, sex, and race), mechanism and cause of injury, injury descriptors, injury severity, diagnostic and therapeutic procedures, and outcomes (disposition and hospital length of stay). We queried publicly available data on the number of Philadelphia patients with COVID-19.27 , 28
Patients and time periods
For trauma and ED visits, all patients aged 14 years and older who received emergency or injury care at PPMC during the specified dates were included. Assessment periods bracketed the Pennsylvania SAHO (March 16, 2020) to include variations that might reflect influences besides the SAHO. Therefore, we assessed care between February 1 and May 30, 2020 and compared care with the same times in each year from 2015 to 2019, accounting for annual and seasonal variation.
Data analysis
IVTs were defined as assaults, firearm-related injury, and stabbings; all others were labeled as nonintentional injuries (NIT; eg fall, found down, motor vehicle crash, and pedestrian crash). This categorization intended to separate trauma inflicted with the intent to harm vs all others. Intentional injuries were then subclassified into firearm- or stabbing-related penetrating injury. All other intentional trauma was considered blunt assault.
For the primary analysis, we compared the incidence and proportion of cases within each mechanism of injury (MOI) in the weeks before and after SAHO. These data were contrasted to the city-wide new daily COVID-19 cases in Philadelphia. Planned analyses were parsed on the basis of race, intentionality (IVT vs NIT), and penetrating vs blunt trauma within IVT.
Except when otherwise noted as proportion of cases, data were expressed as a daily frequency with 95% CIs. Data were missing for key variables in < 1% of cases. We therefore conducted a complete case analysis. Fisher exact test for proportions and Wilcoxon test for continuous variables compared group data as appropriate. Two-tailed significance was set at p < 0.05. Data analysis was facilitated using R statistical software, version 4.0.0 (R Core Team, 2018). We generated plots using the “ggplot2” package.
Results
Trauma rates and characteristics in the time period before and after the stay-at-home order
Trauma patient triage in the city of Philadelphia did not change during the time periods evaluated and the 4 Level I trauma centers received similar proportions of all types of injured patients as in the past (eTable 1). Similarly, no intentional rearrangement of ambulance volume was directed to favor bringing COVID-19 victims to one city hospital over another. Pre- (n = 357) and post-SAHO (n = 480) 2020 trauma patient data are presented in Table 1 . These data disclosed significant differences in sex (35.6% vs 27.9% female; p = 0.019) and age (47.4 ± 22.1 years vs 42.9 ± 20.3 years; p = 0.009). A higher proportion of non-White trauma patients was noted in the post-SAHO period (69.5% vs 77.7%; p = 0.008) (eTables 2 and 3).
Table 1.
Comparison of 2020 Data Before and After Pennsylvania Stay-at-Home Order
| Characteristic | Before SAHO (n = 357) | During SAHO (n = 480) | p Value |
|---|---|---|---|
| Sex, f, n (%) | 127 (35.57) | 134 (27.92) | 0.019 |
| Race, n (%) | 0.032 | ||
| Asian | 5 (1.40) | 11 (2.29) | 0.45 |
| Black | 226 (63.31) | 328 (68.33) | 0.14 |
| Other | 17 (4.76) | 34 (7.08) | 0.12 |
| White | 109 (30.53) | 107 (22.29) | 0.008 |
| Age, y, mean ± SD | 47.36 ± 22.13 | 42.90 ± 20.32 | 0.009 |
| Mechanism of injury, all, n (%) | 0.0006 | ||
| IVT, all | 70 (19.61) | 148 (30.83) | 0.0002 |
| Assault (blunt) | 33 (9.24) | 56 (11.67) | 0.31 |
| Penetrating IVT, all | 62 (17.37) | 140 (29.91) | <0.0001 |
| Stabbing | 25 (7.00) | 38 (7.92) | 0.69 |
| Gunshot wound | 45 (12.61) | 110 (22.92) | 0.0001 |
| Nonintentional, all | 168 (47.06) | 164 (34.17) | 0.0002 |
| Fall | 132 (36.97) | 135 (28.12) | 0.007 |
| Found down | 18 (5.04) | 17 (3.54) | 0.30 |
| MVC | 86 (24.09) | 112 (23.33) | 0.81 |
| Pedestrian vs motor vehicle | 18 (5.04) | 12 (2.50) | 0.060 |
| Injury Severity Score, mean ± SD | 7.54 ± 9.13 | 7.94 ± 8.84 | 0.29 |
| Assault (blunt) | 7.19 ± 10.07 | 6.24 ± 6.29 | 0.56 |
| Stabbing | 2.60 ± 2.86 | 5.91 ± 6.97 | 0.066 |
| Gunshot wound | 12.51 ± 16.63 | 10.08 ± 12.32 | 0.83 |
| Fall | 7.41 ± 6.13 | 8.56 ± 7.09 | 0.20 |
| Found down | 6.53 ± 8.12 | 3.00 ± 4.11 | 0.078 |
| MVC | 6.61 ± 7.09 | 7.46 ± 8.76 | 0.88 |
| Pedestrian vs motorized vehicle | 8.43 ± 7.48 | 6.80 ± 6.78 | 0.59 |
| Outcome, alive, n (%) | 343 (96.08) | 460 (95.83) | 1.00 |
IVT, intentional/violent; MVC, motor vehicle crash; SAHO, stay-at-home order.
The proportion of patients presenting after a fall decreased (36.9% vs 28.1%; p = 0.007) and firearm injuries nearly doubled (gunshot wounds 12.6% vs 22.9%; p < 0.0001). No differences were noted for other MOIs when comparing the 2 time frames (p > 0.05). All combined penetrating trauma increased post SAHO (17.4% vs 29.9%; p < 0.0001). There was no significant difference in mortality or severity of injury as measured by the trauma Injury Severity Score (ISS) in the overall cohorts or those stratified by MOI (Table 1 and eTable 4).
When evaluated by race alone (eTable 2), White patients pre- and post-SAHO periods had similar MOI distributions. Meanwhile, Black patients post SAHO demonstrated greater numbers of firearm injuries (18.1% vs 28.7%; p = 0.005) and Black patients presenting post SAHO suffered more from any type of penetrating trauma (23.9% vs 36.2%; p = 0.00009); no difference in ISS or mortality was noted for this cohort either (eTable 3).
COVID-19 cases and differences in types of trauma
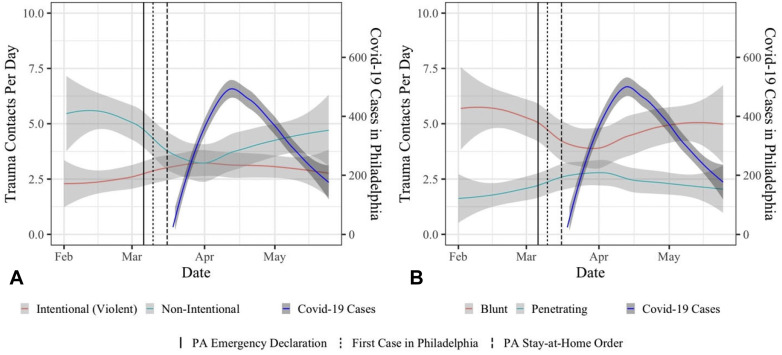
IVT significantly increased post SAHO. Both before and during the lockdown, there were more NIT cases than IVT, but post SAHO there was a significant rise in IVT (19.81% pre SAHO to 30.83% post SAHO), and a decrease in NIT from 80.2% to 69.2% (p = 0.0002) (Table 1 and Fig. 1 ). The post-SAHO period also demonstrated steadily decreasing NIT (Fig. 1A) Similarly, in the weeks that followed SAHO, penetrating trauma (gunshot wounds and stabbings) incidence remained the same or increased slightly, while blunt trauma decreased (Fig. 1B). During the post-SAHO period, the city-wide new daily COVID-19 case incidence rose steadily and peaked in mid-April (Fig. 1).
Figure 1.
Comparison of 2020 types of trauma. (A) Intentional vs nonintentional trauma (2020). (B) Blunt vs penetrating cases (2020).
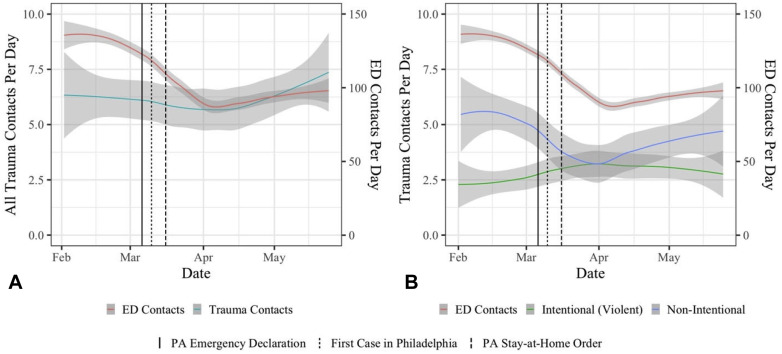
Trauma patients and nontrauma emergency department visits
Trauma patient and noninjury care ED visits at the same facility were compared before and after the SAHO was enacted. ED visits declined as the pandemic surged, with a sharp decline noted after the SAHO; total trauma patient volume remained consistent across periods (Fig. 2 A). With respect to intentionality, with SAHO the NIT declined in parallel to total noninjury ED visits, and IVT visits increased (Fig. 2B).
Figure 2.
Comparison of 2020 trauma and emergency department (ED) visits. (A) ED vs all trauma contacts (2020). (B) ED vs trauma contacts (2020).
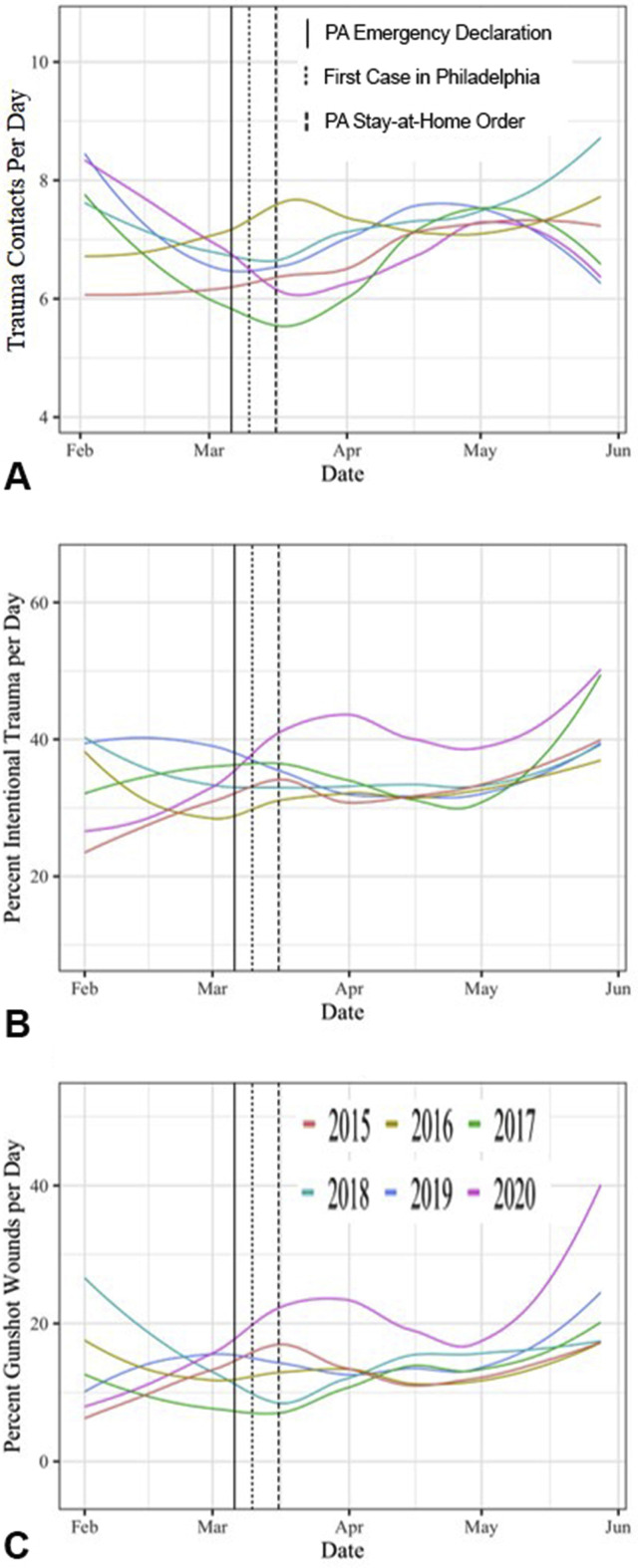
Comparisons across 2015-2020
To distinguish the impact of the SAHO from seasonal crossover from winter (and the holiday seasons) to spring, pre-, and post-SAHO period data from 2020 were compared with those from 2015-2019 (Table 2 ). Only the rate of motor vehicle crashes (MVCs) was different during the pre-SAHO period comparing 2020 with 2015-2019, with reduced MVCs noted in 2020 (p = 0.008); demographics and other domains, including overall trauma volume, sex, and age distribution remained similar (eTable 4). The 2020 post-SAHO period (after March 16, 2020) demonstrated similar changes in race composition compared with the same periods in 2015 through 2019. A greater number of Black patients (p = 0.0006) and a lower number of White patients (p = 0.036) was a durable finding in comparing all years against 2020 during this period. Strikingly, a vast percent increase in gunshot wounds was noted (62.4%; p = 0.00002) during the post-SAHO 2020 period compared with that in 2015-2019. Other differences included a modest decrease in pedestrian injury (p = 0.035) and changes overall in MOI (p = 0.018; Table 2 and Fig. 3 ). Post-SAHO 2020 trauma volumes demonstrated a greater proportion of penetrating injury (p = 0.003) and IVT (p = 0.00009) than earlier years. No differences were noted for ISS within or across groups, and mortality was similar across all years.
Table 2.
Comparison of Data Across Earlier Years and 2020 after Stay-at-Home Order (March 16, 2020)
| Characteristic | 2015 (n = 519) | 2016 (n = 547) | 2017 (n = 514) | 2018 (n = 566) | 2019 (n = 572) | 2020 (n = 480) | p Value |
|---|---|---|---|---|---|---|---|
| Sex, f, n (%) | 184 (35.52) | 166 (30.35) | 157 (30.60) | 185 (32.69) | 184 (32.17) | 134 (27.92) | 0.17 |
| Race, n (%) | 0.04 | ||||||
| Asian | 16 (3.10) | 14 (2.56) | 12 (2.34) | 11 (1.94) | 18 (3.15) | 11 (2.29) | 0.79 |
| Black | 302 (58.53) | 339 (61.97) | 344 (67.06) | 376 (66.43) | 356 (62.24) | 328 (68.33) | 0.005 |
| Other | 42 (8.14) | 32 (5.85) | 27 (5.26) | 24 (4.24) | 30 (5.24) | 34 (7.08) | 0.49 |
| White | 156 (30.23) | 162 (29.62) | 130 (25.34) | 155 (27.39) | 168 (29.37) | 107 (22.29) | 0.036 |
| Age, y, mean ± SD | 45.40 ± 21.43 | 46.17 ± 21.48 | 45.47 ± 20.08 | 46.55 ± 20.72 | 46.92 ± 20.85 | 42.90 ± 20.32 | 0.31 |
| Mechanism of injury, all, n (%) | 0.018 | ||||||
| IVT, all | 109 (21.00) | 119 (21.76) | 104 (20.23) | 130 (22.97) | 120 (20.98) | 148 (30.83) | 0.0008 |
| Assault (blunt) | 69 (13.29) | 63 (11.52) | 74 (14.40) | 67 (11.84) | 68 (11.89) | 56 (11.67) | 0.68 |
| Penetrating IVT, all | 108 (21.01) | 112 (20.59) | 98 (19.10) | 124 (21.95) | 116 (20.35) | 140 (29.91) | 0.003 |
| Stabbing | 36 (6.94) | 45 (8.23) | 37 (7.20) | 40 (7.07) | 39 (6.82) | 38 (7.92) | 0.94 |
| Gunshot wound | 73 (14.07) | 74 (13.53) | 67 (13.04) | 90 (15.90) | 81 (14.16) | 110 (22.92) | 0.0002 |
| Nonintentional, all | 235 (43.35) | 234 (42.78) | 214 (41.63) | 259 (45.76) | 264 (46.15) | 164 (34.17) | 0.001 |
| Fall | 174 (33.53) | 177 (32.36) | 168 (32.68) | 201 (35.51) | 198 (34.62) | 135 (28.12) | 0.17 |
| Found down | 23 (4.43) | 30 (5.48) | 19 (3.70) | 31 (5.48) | 26 (4.55) | 17 (3.54) | 0.53 |
| MVC | 116 (22.35) | 131 (23.95) | 122 (23.74) | 110 (19.43) | 120 (20.98) | 112 (23.33) | 0.40 |
| Pedestrian vs motorized vehicle | 28 (5.39) | 27 (4.94) | 27 (5.25) | 27 (4.77) | 40 (6.99) | 12 (2.50) | 0.035 |
| Outcome, alive, n (%) | 492 (94.80) | 521 (95.25) | 499 (97.08) | 543 (95.94) | 548 (95.80) | 460 (96.03) | 0.55 |
| Injury Severity Score, mean ± SD) | 8.55 ± 10.66 | 7.90 ± 10.21 | 8.03 ± 10.21 | 7.86 ± 8.84 | 8.37 ± 10.69 | 7.94 ± 8.84 | 0.65 |
| Assault (blunt) | 5.51 ± 5.74 | 5.98 ± 6.28 | 6.06 ± 5.88 | 5.15 ± 4.48 | 6.00 ± 6.51 | 6.24 ± 6.29 | 0.67 |
| Stabbing | 4.34 ± 6.73 | 4.11 ± 11.10 | 3.72 ± 5.61 | 3.55 ± 5.45 | 4.76 ± 6.74 | 5.91 ± 6.97 | 0.36 |
| Gunshot wound | 16.61 ± 20.34 | 11.38 ± 15.01 | 12.77 ± 16.83 | 13.29 ± 15.40 | 14.89 ± 18.01 | 10.08 ± 12.32 | 0.13 |
| Fall | 7.71 ± 6.26 | 8.01 ± 7.53 | 9.33 ± 10.49 | 8.06 ± 6.30 | 7.67 ± 8.42 | 8.56 ± 7.09 | 0.77 |
| Found down | 6.59 ± 7.24 | 5.56 ± 9.02 | 3.18 ± 3.30 | 3.32 ± 3.88 | 5.80 ± 6.46 | 3.00 ± 4.11 | 0.18 |
| MVC | 8.18 ± 8.38 | 8.76 ± 10.83 | 6.46 ± 6.57 | 7.88 ± 7.32 | 7.64 ± 9.11 | 7.46 ± 8.76 | 0.44 |
| Pedestrian vs motorized vehicle | 8.84 ± 9.49 | 8.04 ± 10.34 | 9.48 ± 9.23 | 5.67 ± 4.70 | 10.15 ± 11.08 | 6.80 ± 6.78 | 0.96 |
IVT, intentional/violent; MVC, motor vehicle crash.
Figure 3.
Comparison of data from 2015 to 2020. (A) Trauma cases by year. (B) Percent intentional trauma by year. (C) Percent gunshot wounds by year.
Discussion
COVID management has a number of elements that do not appear to directly interface with injury care. Public health measures directed at viral transmission reduction both inside and outside of healthcare facilities might seem remote from urgent, emergent acute health conditions, or injury management. Nonetheless, public health measures like SAHO reshape the fabric of human interaction in ways that impact the frequency at which any healthcare is sought. For instance, social isolation derails key elements of social interaction, including interpersonal communication, basic supply availability, and finances, therefore altering healthcare access and use.
We normally expect the frequency of ED visits for urgent or emergent conditions, such as myocardial ischemia, appendicitis, or stroke, to remain relatively stable, even with socioeconomic disturbances. A pandemic presents a unique environment where fear of contagion in the hospital can impede a patient’s willingness to present for care. Our data support this notion and align with other reports on reduced acute care frequency on contagion fear. This is further supported by the steady decrease in ED visits as the prevalence of COVID-19 increased. This was not likely driven by the virus itself, but rather by the fact that as public reports of COVID-19 cases increased, so did contagion fear and compliance with SAHO. This theory would need testing, as the reason for overall decreased visits to the ED in Philadelphia or elsewhere was not explored in this study. However, given the reduced social contact mandated by a SAHO, the belief that injury frequency would also decrease during a pandemic is intuitively attractive. Indeed, reduced ED acute care visits were paralleled by decreases in NIT visits. Unfortunately, the opposite was noted for IVT at our center, meriting additional inquiry.
Major societal disruptions directly affect urban violence and injury through the interface between public health measures and injury care. The duration of societal disruption appears to be an important element driving increases in injury. Although New York City noted no change in homicide rate after 9/11, Houston saw substantial increases in violent injury after Hurricane Katrina.29 , 30 Perhaps, the longer-lasting social disturbance duration correlates with economic instability and unemployment compared with the point devastation of 9/11—in spite of its great emotional and political impact.31 Public health measures during a pandemic have broad overlap with financial peril because enforced economy reductions, social distancing, and reduced mechanisms for social outlet are shuttered. Therefore, increased social tension plausibly forces individuals to stay in close quarters, perhaps increasing intentional or violent injury in domiciles or communities. Although assault and other forms of blunt violent trauma might also be expected to increase, we only saw an increase in penetrating violent injury only with no increase in blunt assault IVT. This lack of a significant increases in nonpenetrating violent injury was similar in both White and Black populations. It is unclear how this can be explained other than the existing pervasiveness of gun violence in the city, which was further compounded by the high-tension circumstances around the SAHO, bolstering the preexisting public health problems in these communities. Specifically, the isolated increase in gunshot wounds could be driven by decreased numbers of people present in city streets and urban spaces, allowing violence and crime to progress unwitnessed and unchecked by overtaxed law enforcement agencies.
We suggest that there might be 2 distinct harms from social isolation: patients who do not present to the ED for potentially life-threatening acute care conditions to avoid virus exposure, and increasing violent injury in the midst of an overburdened law enforcement system. Both events can impact epidemiologic reporting and analysis, critically stressing already challenged Emergency Medical Services and law enforcement agencies.
Trauma patient volumes in urban health systems characteristically vary in nature and severity across season and time of year.32 These seasonal variations are typical and locally related to social norms, weather patterns, scheduled public events, and other environmental factors.33 , 34 Our data demonstrate an association between pandemic-related public health measures and both trauma patient volume and injury profile at an urban Level I trauma center. Social isolation policies instituted in March 2020 were associated with a sharp increase in IVT, in spite of a decrease in NIT and overall ED patient volume. Decreases in MVCs were anticipated as the early SAHO period was anecdotally characterized by markedly decreased road traffic. A corresponding decrease in pedestrian injury was similarly expected. Because the increase in IVT is unique compared with the preceding 5 years, trauma and public health systems are presented with an opportunity to mitigate future occurrences during periods of social norm disruption.
Neither injury severity nor patient mortality changed across periods. This was a surprising finding because during other periods of major disturbances, 2 key behaviors have been observed that can increase both ISS and mortality: participation in dangerous behavior (that can predispose to trauma) due to higher risk thresholds, and inadvertent existence in a dire circumstance that can predispose to greater injury severity.35 That neither was observed in our study serves to strengthen the link between social isolation and IVT. In addition, our data suggest that within the catchment area for our urban center, the increase in IVT asymmetrically impacts Black populations more than White.
We found increases in gunshot wounds that disproportionately affected young, Black men—the urban demographic already overrepresented across decades of inner-city firearm-related intentional injury.36 Ironically, similar urban subpopulations also appear at greater risk of COVID-19 infection and mortality.37 , 38 Although injury caused by interpersonal violence not only increased in an absolute number, it also greatly increased as a proportion of overall trauma patient volume. This unique increase should inform essential local and regional public health preparations and strategies for social distancing as we anticipate ongoing public health measures ahead of the upcoming winter flu season. Relatedly, trauma centers, Emergency Medical Services and law enforcement operating in areas impacted by SAHO should prepare for increases in local trauma patient flow, especially in cities like Philadelphia, where police vehicles transport penetrating injury victims to hospital directly from the scene.
In preparing for the next health crisis, as well as adapting to the current ongoing one, public health measures should plan to mitigate untoward impacts on specific populations and leverage both the inpatient care and the outreach efforts of the US trauma system to help achieve that goal. The American College of Surgeons Committee on Trauma and state verification systems should incorporate programs to combat this into their recurrent verification assessments. Hospitals and hospital networks cannot, and should not, be the sole funders of these activities. Instead, both state and federal funding should be directed to support injury reduction and prevention programs with a targeted focus on IVT. Crafting partnerships between trauma centers, their surrounding communities, and the local public health and law enforcement departments, as well as federal agencies, such as the Bureau of Alcohol, Tobacco, Firearms and Explosives and the US Customs and Border Protection, can be of substantial benefit in bolstering such efforts. It must be noted that the firearm injury epidemic is not limited to pandemic periods and needs ongoing and focused attention past the pandemic period. Firearm violence impacts approximately 33,000 Americans per year with a large disparity between White and non-White victims. Mass casualty and active shooter events are only a small fraction of US firearm violence, even though they garner the most focused attention.39
This was a single-institution study that encompassed 1 region of West Philadelphia and therefore might not be readily extrapolatable to other regions. We used the severity of the COVID-19 pandemic and case surge to present the daily reports that the city population was receiving and informed how their behavior changed in staying in their homes, understanding that this is a poor surrogate for how SAHO compliance progressed. Adherence to social isolation guidelines is difficult to quantify, capture, or predict and public behavior in other crises might be different. Suicide attempts were not included in the group of IVT because the trauma registry does not capture this sample well (they often do not present to the trauma bay but to the main ED), although conceivably this group of self-inflicted injuries might have been greatly affected by the SAHO-mandated isolation that might have worsened depression and other suicide-related behaviors. We also did not assess unemployment rates or geolocate injury occurrences to link them with socioeconomic factors in specific locales. Specific triggers of the increased IVT were inferred from context but not from dedicated patient-level query. Finally, we were unable to determine the physical location of where the violent injury had occurred (ie inside vs outside and home vs place of work), as this information is rarely available in the electronic medial record for trauma victims and is not captured by the Trauma Registry.
This inquiry approached the impact of an SAHO on total ED care and trauma care during a period of reduced transient population through the catchment area. This approach allowed a more focused assessment of the resident population and the impact of the SAHO on injury profiles, with the goal of discerning one or more avenues of supporting local population health and survival.
Conclusions
Trauma volumes and routine ED visits appear to decrease with social isolation during a mandated public health approach to pandemic management. Decreases in MVCs and nonintentional injury were evident and anticipated during the period of lockdown. However, increased intentional violent injury, particularly penetrating trauma, was noted with an asymmetric racial allocation in young Black men. Because the increase in IVT associated with the SAHO issued to help address viral containment appears distinct from the rate of IVT in the prior 5 years, additional inquiry is warranted, and specific action should be undertaken addressing the impact of social isolation on injury. Although pandemic care serves as the current trigger, natural and man-made disasters can establish many of the same circumstances that promote intentional injury. Public and private health system leaders should develop partnerships that embrace medical professional organization support to proactively reduce violent injury, and specifically firearm-related injury, during periods of social isolation.
Author Contributions
Study conception and design: Abdallah, Zhao, Kaufman, Pascual
Acquisition of data: Pascual
Analysis and interpretation of data: Abdallah, Zhao
Drafting of manuscript: Abdallah, Zhao, Kaufman, Pascual
Critical revision: Hatchimonji, Swendiman, Kaplan, Seamon, Schwab
Footnotes
CME questions for this article available at http://jacscme.facs.org
Disclosure Information:Authors have nothing to disclose. Timothy J Eberlein, Editor-in-Chief, has nothing to disclose. Ronald J Weigel, CME Editor, has nothing to disclose.
Drs Abdallah and Zhao contributed equally to this work.
Appendix
eTable 1.
Comparison of Patient Residence ZIP Codes Before and after Pennsylvania Stay-at-Home Order (March 16, 2020)
| ZIP code | Before SAHO (n = 357) |
During SAHO (n = 480) |
p Value | ||
|---|---|---|---|---|---|
| n | % | n | % | ||
| Hospital∗ | 31 | 8.68 | 58 | 12.08 | 0.14 |
| Neighborhood | 154 | 43.14 | 203 | 42.29 | 0.83 |
| Other | 172 | 48.18 | 219 | 45.62 | 0.48 |
SAHO, stay-at-home-order.
Limited to only the ZIP code in which the trauma center is located.
eTable 2.
Comparison of 2020 Data Before and after Pennsylvania Stay-at-Home Order (March 16, 2020) for White Patients
| Characteristic | Before SAHO (n = 109) | During SAHO (n = 107) | p Value |
|---|---|---|---|
| Sex, f, n (%) | 42 (38.5) | 36 (33.6) | 0.48 |
| Age, y, mean ± SD | 56.0 ± 22.2 | 55.5 ± 21.2 | 0.86 |
| Mechanism of injury, all, n (%) | 0.76 | ||
| IVT, all | 7 (6.4) | 10 (9.3) | 0.46 |
| Assault (blunt) | 7 (6.4) | 10 (9.3) | 0.46 |
| Penetrating IVT, all | 5 (4.6) | 10 (9.3) | 0.19 |
| Stabbing | 4 (3.7) | 4 (3.7) | 1.0 |
| Gunshot wound | 3 (2.8) | 6 (5.6) | 0.33 |
| Nonintentional, all | 73 (67.0) | 63 (58.9) | 0.26 |
| Fall | 63 (57.8) | 57 (53.3) | 0.58 |
| Found down | 7 (6.4) | 3 (2.8) | 0.33 |
| MVC | 22 (20.2) | 24 (22.4) | 0.74 |
| Pedestrian vs motorized vehicle | 3 (2.8) | 3 (2.8) | 1.00 |
| Injury Severity Score, mean ± SD | 8.0 ± 7.1 | 8.7 ± 7.0 | 0.33 |
| Assault (blunt) | 10.0 ± 8.8 | 6.0 ± 4.5 | 0.32 |
| Stabbing | 3.2 ± 4.5 | 7.8 ± 9.4 | 0.62 |
| Gunshot wound | 4.7 ± 4.0 | 9.5 ± 6.6 | 0.28 |
| Fall | 8.1 ± 6.6 | 8.9 ± 6.7 | 0.48 |
| Found down | 7.2 ± 8.9 | 5.7 ± 4.5 | 0.79 |
| MVC | 9.1 ± 8.4 | 9.9 ± 8.2 | 0.69 |
| Pedestrian vs motorized vehicle | 6.0 ± 6.2 | 9.7 ± 11.0 | 0.82 |
| Outcome, alive, n (%) | 106 (97.2) | 105 (98.1) | 1.0 |
IVT, intentional/violent; MVC, motor vehicle crash; SAHO, stay-at-home order.
eTable 3.
Comparison of 2020 Data Before and After Pennsylvania Stay-at-Home Order (March 16, 2020) for Black Patients
| Characteristic | Before SAHO (n = 226) | During SAHO (n = 328) | p Value |
|---|---|---|---|
| Sex, f, n (%) | 81 (35.8) | 85 (25.9) | 0.014 |
| Age, y, mean ± SD | 43.2 ± 20.9 | 39.6 ± 18.8 | 0.095 |
| Mechanism of injury, all, n (%) | 0.018 | ||
| IVT | 60 (26.5) | 124 (37.8) | 0.006 |
| Assault (blunt) | 22 (9.7) | 42 (12.8) | 0.28 |
| Penetrating IVT, all | 54 (23.9) | 116 (35.4) | 0.005 |
| Stabbing | 19 (8.4) | 30 (9.1) | 0.88 |
| Gunshot wound | 41 (18.1) | 94 (28.7) | 0.005 |
| Nonintentional trauma, all | 83 (36.7) | 87 (26.5) | 0.011 |
| Fall | 58 (25.7) | 69 (21.0) | 0.22 |
| Found down | 11 (4.9) | 10 (3.0) | 0.37 |
| MVC | 61 (27.0) | 75 (22.9) | 0.27 |
| Pedestrian vs motorized vehicle | 14 (6.2) | 8 (2.4) | 0.044 |
| Injury Severity Score, mean ± SD | 7.5 ± 10.3 | 7.2 ± 8.0 | 0.39 |
| Assault (blunt) | 6.8 ± 11.1 | 5.5 ± 4.6 | 0.33 |
| Stabbing | 2.4 ± 2.7 | 6.1 ± 7.1 | 0.048 |
| Gunshot wound | 13.0 ± 17.3 | 9.0 ± 10.4 | 0.51 |
| Fall | 6.9 ± 5.7 | 8.3 ± 7.0 | 0.24 |
| Found down | 6.1 ± 8.1 | 1.1 ± 0.4 | 0.068 |
| MVC | 5.5 ± 6.3 | 6.2 ± 7.4 | 0.83 |
| Pedestrian vs motorized vehicle | 9.4 ± 8.3 | 4.8 ± 4.8 | 0.27 |
| Outcome, alive, n (%) | 215 (95.1) | 313 (95.7) | 0.84 |
IVT, intentional/violent; MVC, motor vehicle crash; SAHO, stay-at-home order.
eTable 4.
Comparison of Data from 2015 to 2020 Before Stay-at-Home Order (March 16, 2020)
| Characteristic | 2015 (n = 268) | 2016 (n = 331) | 2017 (n = 293) | 2018 (n = 313) | 2019 (n = 315) | 2020 (n = 357) | p Value |
|---|---|---|---|---|---|---|---|
| Sex, f, n (%) | 87 (32.46) | 107 (32.33) | 95 (32.42) | 94 (30.03) | 112 (35.56) | 127 (35.57) | 0.65 |
| Race, n (%) | 0.20 | ||||||
| Asian | 11 (4.10) | 10 (3.02) | 5 (1.71) | 6 (1.92) | 4 (1.27) | 5 (1.40) | 0.17 |
| Black | 146 (54.48) | 211 (63.75) | 194 (66.21) | 198 (63.26) | 196 (62.22) | 226 (63.31) | 0.096 |
| Other | 18 (6.72) | 24 (7.25) | 19 (6.48) | 18 (5.75) | 18 (5.71) | 17 (4.76) | 0.80 |
| White | 93 (34.70) | 86 (25.98) | 74 (25.26) | 91 (29.07) | 97 (30.79) | 109 (30.53) | 0.13 |
| Age, y, mean ± SD | 50.71 ± 22.29 | 47.15 ± 21.00 | 47.50 ± 20.64 | 45.30 ± 20.82 | 48.71 ± 22.54 | 47.36 ± 22.13 | 0.23 |
| Mechanism of injury, all | 0.13 | ||||||
| IVT, all, n (%) | 45 (16.79) | 64 (19.34) | 58 (19.80) | 78 (24.92) | 60 (19.05) | 70 (19.61) | 0.25 |
| Assault (blunt) | 33 (12.31) | 42 (12.69) | 42 (14.33) | 32 (10.22) | 47 (14.92) | 33 (9.24) | 0.18 |
| Penetrating IVT, all, mean ± SD | 0.18 ± 0.38 | 0.18 ± 0.39 | 0.17 ± 0.37 | 0.25 ± 0.43 | 0.18 ± 0.39 | 0.17 ± 0.38 | 0.15 |
| Stabbing, n (%) | 16 (5.97) | 20 (6.04) | 25 (8.53) | 23 (7.35) | 21 (6.67) | 25 (7.00) | 0.85 |
| Gunshot wound, n (%) | 29 (10.82) | 44 (13.29) | 33 (11.26) | 55 (17.57) | 39 (12.38) | 45 (12.61) | 0.19 |
| Nonintentional, all, n (%) | 156 (58.21) | 161 (48.64) | 143 (48.81) | 154 (49.20) | 149 (47.30) | 168 (47.06) | 0.083 |
| Fall | 127 (47.39) | 128 (38.67) | 106 (36.18) | 119 (38.02) | 122 (38.73) | 132 (36.97) | 0.089 |
| Found down | 14 (5.22) | 15 (4.53) | 22 (7.51) | 15 (4.79) | 12 (3.81) | 18 (5.04) | 0.47 |
| MVC | 34 (12.69) | 64 (19.34) | 50 (17.06) | 49 (15.65) | 59 (18.73) | 86 (24.09) | 0.008 |
| Pedestrian vs motorized vehicle | 15 (5.60) | 18 (5.44) | 15 (5.12) | 20 (6.39) | 15 (4.76) | 18 (5.04) | 0.96 |
| Injury Severity Score, mean ± SD | 8.47 ± 9.03 | 8.15 ± 10.55 | 7.98 ± 10.01 | 8.40 ± 10.40 | 9.50 ± 11.46 | 7.54 ± 9.13 | 0.90 |
| Assault (blunt) | 6.33 ± 4.93 | 6.51 ± 7.22 | 6.05 ± 5.79 | 5.77 ± 6.48 | 6.12 ± 5.29 | 7.19 ± 10.07 | 0.81 |
| Stabbing | 4.14 ± 6.57 | 9.00 ± 17.52 | 6.29 ± 8.04 | 3.35 ± 3.17 | 3.48 ± 4.03 | 2.60 ± 2.86 | 0.046 |
| Gunshot wound | 12.79 ± 12.87 | 11.21 ± 12.92 | 15.44 ± 21.79 | 14.40 ± 17.90 | 21.33 ± 21.91 | 12.51 ± 16.63 | 0.27 |
| Fall | 7.93 ± 7.80 | 7.72 ± 9.24 | 8.04 ± 6.79 | 6.43 ± 5.48 | 8.95 ± 6.78 | 7.41 ± 6.13 | 0.91 |
| Found down | 9.50 ± 10.99 | 3.92 ± 6.76 | 4.89 ± 5.99 | 5.92 ± 4.56 | 7.67 ± 7.71 | 6.53 ± 8.12 | 0.89 |
| MVC | 8.11 ± 10.40 | 7.50 ± 9.44 | 6.28 ± 6.12 | 10.18 ± 9.28 | 8.14 ± 9.53 | 6.61 ± 7.09 | 0.73 |
| Pedestrian vs motorized vehicle | 13.00 ± 10.86 | 12.64 ± 12.97 | 11.30 ± 12.55 | 12.36 ± 12.06 | 5.57 ± 5.83 | 8.43 ± 7.48 | 0.069 |
| Outcome, alive, n (%) | 255 (95.15) | 316 (95.47) | 284 (96.93) | 302 (96.49) | 300 (95.24) | 343 (96.08) | 0.85 |
IVT, intentional/violent; MVC, motor vehicle crash.
References
- 1.Ohannessian R., Duong T.A., Odone A. Global telemedicine implementation and integration within health systems to fight the COVID-19 pandemic: a call to action. JMIR Public Health Surveill. 2020;6 doi: 10.2196/18810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Tanne J.H., Hayasaki E., Zastrow M. Covid-19: how doctors and healthcare systems are tackling coronavirus worldwide. BMJ. 2020;368:m1090. doi: 10.1136/bmj.m1090. [DOI] [PubMed] [Google Scholar]
- 3.Vaccaro A.R., Getz C.L., Cohen B.E. Practice management during the COVID-19 pandemic. J Am Acad Orthop Surg. 2020;28:464–470. doi: 10.5435/JAAOS-D-20-00379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Orso A., Tornoe R., Collins Walsh S. Philadelphia orders shutdown of businesses, city services as coronavirus spreads. The Philadelphia Inquirer. https://www.inquirer.com/health/coronavirus/philadelphia-shutdown-coronavirus-20200316.html Available at: Published March 16, 2020. Accessed June 22, 2020.
- 5.Kellner H. Philadelphia announces first case of COVID-19 coronavirus. Department of Public Health, Philadelphia, PA. Available at: https://www.phila.gov/2020-03-10-philadelphia-announces-first-case-of-covid-19-coronavirus/. Published March 10, 2020. Accessed June 22, 2020.
- 6.Stokes E.K., Zambrano L.D., Anderson K.N. Coronavirus disease 2019 case surveillance—United States, January 22–May 30, 2020. MMWR Morb Mortal Wkly Rep. 2020;69(24):759–765. doi: 10.15585/mmwr.mm6924e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gov Wolf puts statewide COVID-19 mitigation efforts in effect, stresses need for every Pennsylvanian to take action to stop the spread. https://www.governor.pa.gov/newsroom/gov-wolf-puts-statewide-covid-19-mitigation-efforts-in-effect-stresses-need-for-every-pennsylvanian-to-take-action-to-stop-the-spread/ Available at: Published March 16, 2020. Accessed July 23, 2020.
- 8.Magro F., Abreu C., Rahier J.-F. The daily impact of COVID-19 in gastroenterology. United Eur Gastroenterol J. 2020;8:520–527. doi: 10.1177/2050640620920157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Søreide K., Hallet J., Matthews J.B. Immediate and long-term impact of the COVID-19 pandemic on delivery of surgical services. Br J Surg. 2020 Apr 30 doi: 10.1002/bjs.11670. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.CDC Coronavirus disease 2019 (COVID-19) https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/racial-ethnic-minorities.html Available at:
- 11.Hartnett K.P., Kite-Powell A., DeVies J. Impact of the COVID-19 pandemic on emergency department visits—United States, January 1, 2019–May 30, 2020. MMWR Morb Mortal Wkly Rep. 2020;69(23):699–704. doi: 10.15585/mmwr.mm6923e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Tam C.-C.F., Cheung K.-S., Lam S. Impact of coronavirus disease 2019 (COVID-19) outbreak on ST-segment–elevation myocardial infarction care in Hong Kong, China. Circ Cardiovasc Qual Outcomes. 2020;13(4) doi: 10.1161/CIRCOUTCOMES.120.006631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Impacto de la pandemia de COVID-19 sobre la actividad asistencial en cardiología intervencionista en España. Gestión. https://www.recintervcardiol.org/es/gestion/impacto-de-la-pandemia-de-covid-19-sobre-la-actividad-asistencial-en-cardiologia-intervencionista-en-espana Available at:
- 14.Krumholz H.M. Where have all the heart attacks gone? The New York Times. https://www.nytimes.com/2020/04/06/well/live/coronavirus-doctors-hospitals-emergency-care-heart-attack-stroke.html Available at: Published April 6, 2020. Accessed June 14, 2020.
- 15.Tsamakis K., Rizos E., J Manolis A. COVID-19 pandemic and its impact on mental health of healthcare professionals. Exp Ther Med. 2020;19:3451–3453. doi: 10.3892/etm.2020.8646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Boukhris M., Hillani A., Moroni F. Cardiovascular implications of the COVID-19 pandemic: a global perspective. Can J Cardiol. 2020;36:1068–1080. doi: 10.1016/j.cjca.2020.05.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kawohl W., Nordt C. COVID-19, unemployment, and suicide. Lancet Psychiatry. 2020;7:389–390. doi: 10.1016/S2215-0366(20)30141-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Jeltsen M. As nation stays home, early indicators suggest rise in domestic violence killings. HuffPost. https://www.huffpost.com/entry/increase-domestic-violence-killings-coronavirus-stay-at-home_n_5e907808c5b63e73d7e38fe7 Available at: Published April 12, 2020. Accessed June 14, 2020.
- 19.Vanderklippe N. Domestic violence reports rise in China amid COVID-19 lockdown. The Globe and Mail. https://www.theglobeandmail.com/world/article-domestic-violence-reports-rise-in-china-amid-covid-19-lockdown/ Available at: Published March 29, 2020. Accessed October 29, 2020.
- 20.Mohler G., Bertozzi A.L., Carter J. Impact of social distancing during COVID-19 pandemic on crime in Los Angeles and Indianapolis. J Crim Justice. 2020;68:101692. doi: 10.1016/j.jcrimjus.2020.101692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Smith R., Zeidan A., Sciarretta J. Doctors: violent trauma will surge amid coronavirus upheaval. We're already seeing it. https://www.usatoday.com/story/opinion/2020/04/17/coronavirus-violence-trauma-doctors-anticipate-surge-serious-injuries-column/5137991002/ Available at: Published April 17, 2020. Accessed June 14, 2020.
- 22.Bates J. “We’re catching it double.” Amid coronavirus lockdowns, gun violence continues to plague Chicago. Time. https://time.com/5818553/gun-violence-chicago-coronavirus/ Available at: Published April 11, 2020. Accessed June 14, 2020.
- 23.Newall M., Palmer C., Purcell D. Even a pandemic can’t slow Philly’s gun violence. The Philadelphia Inquirer. https://www.inquirer.com/news/philadelphia-gun-violence-shootings-rise-coronavirus-pandemic-20200424.html Available at: Published April 24, 2020. Accessed June 17, 2020.
- 24.Kaufman E. Opinion: Please, stop shooting. We need the beds. The New York Times. https://www.nytimes.com/2020/04/01/opinion/covid-gun-violence-hospitals.html Available at: Published April 1, 2020. Accessed October 29, 2020.
- 25.Rui P., Ashman J.J., Akinseye A. National Center for Health Statistics; Hyattsville, MD: 2019. Emergency department visits for injuries sustained during sports and recreational activities by patients aged 5–24 years, 2010–2016. National Health Statistics Reports. Number 133. [PubMed] [Google Scholar]
- 26.Bowen E.A., Murshid N.S. Trauma-informed social policy: a conceptual framework for policy analysis and advocacy. Am J Public Health. 2016;106:223–229. doi: 10.2105/AJPH.2015.302970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Testing and data. Department of Public Health, Philadelphia, PA. Available at: https://www.phila.gov/programs/coronavirus-disease-2019-covid-19/testing-and-data/. Accessed July 23, 2020.
- 28.COVID tests and cases OpenDataPhilly. https://www.opendataphilly.org/dataset/covid-cases Available at:
- 29.Claassen C, Carmody T, Stewart S, et al. Effect of the 9-11 terrorist attacks on suicide and homicide in the vicinity of the attacks. Paper presented at: 137st American Public Health Association Annual Meeting and Exposition; November 7–11, 2009; Philadelphia, PA.
- 30.Uniform Crime Reporting (UCR) Program. Federal Bureau of Investigation. https://www.fbi.gov/services/cjis/ucr Available at:
- 31.Madan A.K., Sapozhnik J., Tillou A. Unemployment rates and trauma admissions. World J Surg. 2007;31:1930–1933. doi: 10.1007/s00268-007-9190-4. [DOI] [PubMed] [Google Scholar]
- 32.Stonko D.P., Dennis B.M., Callcut R.A. Identifying temporal patterns in trauma admissions: informing resource allocation. PLoS One. 2018;13 doi: 10.1371/journal.pone.0207766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ramgopal S., Dunnick J., Siripong N. Seasonal, weather, and temporal factors in the prediction of admission to a pediatric trauma center. World J Surg. 2019;43:2211–2217. doi: 10.1007/s00268-019-05029-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Røislien J., Søvik S., Eken T. Seasonality in trauma admissions—are daylight and weather variables better predictors than general cyclic effects? PLoS One. 2018;13 doi: 10.1371/journal.pone.0192568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Turner C., McClure R., Pirozzo S. Injury and risk-taking behavior—a systematic review. Accid Anal Prev. 2004;36:93–101. doi: 10.1016/s0001-4575(02)00131-8. [DOI] [PubMed] [Google Scholar]
- 36.Beard J.H., Morrison C.N., Jacoby S.F. Quantifying disparities in urban firearm violence by race and place in Philadelphia, Pennsylvania: a cartographic study. Am J Public Health. 2017;107:371–373. doi: 10.2105/AJPH.2016.303620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Oppel R.A., Jr., Gebeloff R., Lai K.K.R. The fullest look yet at the racial inequity of coronavirus. The New York Times. https://www.nytimes.com/interactive/2020/07/05/us/coronavirus-latinos-african-americans-cdc-data.html Published July 5, 2020. Accessed October 29, 2020.
- 38.Chowkwanyun M., Reed A.L. Racial health disparities and Covid-19—caution and context. N Engl J Med. 2020;383:201–203. doi: 10.1056/NEJMp2012910. [DOI] [PubMed] [Google Scholar]
- 39.Mesic A., Franklin L., Cansever A. The relationship between structural racism and Black-White disparities in fatal police shootings at the state level. J Natl Med Assoc. 2018;110:106–116. doi: 10.1016/j.jnma.2017.12.002. [DOI] [PubMed] [Google Scholar]