Abstract
Objective
Endoscopic submucosal dissection (ESD) is widely used in early-stage esophageal cancer, but the quality of life of patients with postoperative stricture is markedly reduced, requiring long-term repeat, periodic endoscopic balloon dilatation. We evaluated the combination of hydrocortisone sodium succinate and aluminum phosphate gel administered orally for stricture prevention.
Methods
We retrospectively assigned 27 patients who underwent ≥3/4 circular ESD for esophageal superficial squamous cell cancer to one of two groups according to the preventative strategy: endoscopic intralesional steroid injection and systemic steroid (IT+ST group) and oral combination of hydrocortisone sodium succinate and aluminum phosphate gel (OHA group). Stricture rate was compared between the two groups.
Results
There were six and seven complete and ≥3/4 circular ESD cases, respectively, in the IT+ST group and four and ten cases in the OHA group. Stricture rates in the IT+ST and OHA groups were 53.8% and 7.1%, respectively. Nine patients in each group developed hypokalemia after glucocorticoid administration.
Conclusions
OHA is a promising treatment strategy for stricture prevention following large-circumference ESD in patients with early stage esophageal carcinoma.
Keywords: Endoscopic submucosal dissection, stricture, oral mixture gel, steroid, local injection, esophageal cancer
Introduction
Endoscopic submucosal dissection (ESD) is the preferred therapeutic approach in early, non-metastasized esophageal squamous cell cancer. The en bloc success rate of ESD in early stage esophageal carcinoma treatment reaches 95%;1 hence, more physicians and patients choose to use ESD to treat early esophageal cancer. However, stricture following ≥3/4 circumferential ESD markedly reduces the quality of life of patients, who often require long-term repeated, periodic endoscopic balloon dilatation (EBD). Hence, identifying novel tools for the prevention of esophageal stenosis following ESD is of prime importance.
Steroids can inhibit collagen synthesis and promote collagen breakdown to suppress stricture formation. Several studies have reported the effects of prophylactic intralesional steroid injection in stricture prevention post-ESD.2–4 However, potential risks of esophageal perforation and local infection are associated with local steroid injection. Multiple studies have confirmed the effects of orally administered prednisolone in preventing stricture occurrence following ESD in esophageal carcinoma,5–7 although the stenosis rate is not sufficiently satisfactory. Therefore, we assessed a novel innovative and effective strategy using combined hydrocortisone sodium succinate and aluminum phosphate gel administered orally for stricture prevention.
The aim of the present study was to evaluate the feasibility and prophylactic effects of hydrocortisone sodium succinate/aluminum phosphate gel combination treatment administered orally after ESD for the treatment of early esophageal cancer in a small sample of cases with mucosal defect involving ≥3/4 of the esophageal lumen circumference.
Methods
Patients and grouping
This was a retrospective study of data from patients with superficial squamous cell cancer treated using large-circumference ESD for prevention of stricture at the Peking University Third Hospital from September 2014 to November 2017. Inclusion criteria were (1) age >18 years; (2) severe dysplasia of esophageal mucosa and early esophageal carcinoma, with lesions confined to the epithelium or lamina propria; (3) lesions infiltrated to the mucosal muscular or submucosal layer, with no clinical evidence of lymph node metastasis on chest CT or PET-CT scan; (4) endoscopic ESD treatment feasible, with lesion resection scope ≥3/4 of esophagus circumference; (5) no prior surgery or radiation for treatment. Exclusion criteria were (1) endoscopy contraindications, including severe cardiopulmonary dysfunction and coagulation ailments; (2) ESD treatment rejection; (3) resection scope <3/4 of esophagus circumference; (4) lesion deeper than the submucosa by pathological examination; (5) chest CT or PET-CT suggesting lymph node or distant metastasis; (6) peri- or post-operative complications requiring further therapy in patients not tolerating the medication; (7) contraindications for glucocorticoids; (8) other treatment, including local additional surgery or radiotherapy during follow-up.
The study protocol was approved by the institutional review board of the Peking University Third Hospital (approval no. 272-03), and all study procedures complied with the principles of the Declaration of Helsinki (1964). Informed consent was provided by all participants, who were retrospectively contacted for permission to use their data.
Grouping was based on prophylactic drug regimens. Since September 2014, the department of gastroenterology at our hospital administered hormone treatment to all patients undergoing large-area ESD to prevent the occurrence of esophageal stenosis. Because the effect of combined local injection and oral steroid treatment would have had a superposition effect, and in line with the method used in previous studies (unpublished data), we initially administered triamcinolone acetonide and prednisone to patients but found that a certain incidence of stenosis persisted. With the development of ESD technology, we sought a simpler, safer, and more effective way to prevent esophageal stenosis and therefore started to administer patients a mixed steroid gel from May 2016. Therefore, we included two groups of patients in our analysis according to prophylactic drug regimen.
Patients treated with endoscopic intralesional steroid (triamcinolone acetonide 80 mg) injection and systemic steroid comprised an IT+ST group, while patients who received hydrocortisone sodium succinate and aluminum phosphate gel combination orally were in the OHA group. Patients in the IT+ST group were administered 80 mg intralesional steroid following ESD. Then, they were administered 30 mg/day prednisone on day 2 after ESD, followed by a gradually tapering prednisone dose (30 mg/day in first 2 weeks and reducing 5 mg/day weekly) after confirmation of no perforation; administration of systemic steroid was discontinued 8 weeks later. OHA group patients initially received a hydrocortisone sodium succinate (50 mg) and aluminum phosphate gel (20 mg) combination, four times per day (qid) on day 2 after ESD, followed by a gradually tapered OHA dose (hydrocortisone sodium succinate: 50 mg qid for 2 weeks, 25 mg qid for 2 weeks, 12.5 mg for 4 weeks; aluminum phosphate 20 mg qid constant dose). The two groups were compared for stricture rate.
ESD procedure
Each case of ESD was performed by the same chief physician with extensive experience in endoscopic minimally invasive surgery and in ESD for hundreds of cases of early esophageal cancer. Patients underwent gastroscopy and biopsy prior to admission, and had a definite ESD indication. Preoperatively, routine biochemical and coagulation assays, electrocardiography, echocardiography, chest radiology, and pulmonary function assays were performed to rule out contraindications for ESD, as detailed in the eligibility criteria. Patients were placed in the left decubitus position with uninterrupted routine ECG monitoring and were administered routine intravenous general anesthesia using propofol and other anesthetic agents. CO2 air pump inflation was applied perioperatively, with a transparent cap in front of the gastroscope.
Endoscopic techniques
Pathological changes in lesions were assessed by transoral endoscopy. A Fuji Intelligent Color Enhancement (FICE) technology and magnifying endoscopy with blue laser imaging (ME-BLI) (Fujinon, Tokyo, Japan) were employed to assess the morphology of capillary loops in epithelial papillae. Lesions were stained using 1.5% to 2% Lugol’s iodine solution for observation. The lesion boundary was defined based on the non-stained area and marked with argon plasma coagulation (APC) or Dual Knife J (Olympus Optical Co., Tokyo, Japan) electrocoagulation mode at 0.5 cm from the edge with 0.5 cm marking intervals. Next, 0.005% adrenaline, glycerol fructose, and methylene blue solution were administered into the lesion submucosa at various locations. For submucosal dissection, IT-NANO and Dual Knife J (Olympus Optical Co.) were used alternately to separate the submucosal layer from the perioral area of the lesion along the above markings. Finally, lesion ligation was performed with a snare followed by complete resection. Perioperatively, electrocoagulation and APC hemostasis were used to stop bleeding and cool norepinephrine salt water was employed to wash the bleeding area. Preventive electrocoagulation hemostasis forceps were used for large vessel bleeding.
Specimens were assessed for marked points to evaluate whether resection was complete, were measured and photographed by a pathologist, and were fixed using neutral formaldehyde before examination.
To control bleeding, APC and electrocoagulation hemostatic forceps were used for exposed blood vessels, with careful assessment of the presence of small perforations. Titanium clips were used for wound closure to manage possible hemorrhagic foci, suspicious perforation, or muscular layer injury. Combined local hormone injection and oral administration was applied to prevent esophagostenosis. Patients in the IT+ST group were then administrated triamcinolone acetonide 80 mg (2 mL) by injection at 8 points into the submucosa of the lower and upper margins of the lesion as well as into the thin residual submucosa of the wound, avoiding needle penetration into the muscularis propria which can potentially cause muscularis propria necrosis or delayed perforation.
Gastroscopy for stricture assessment
Gastroscopy was carried out immediately in the case of dysphagia, or 8 weeks post-ESD for assessing any possible stricture [difficulty in swallowing solid materials or the inability to pass an gastroscopy (9.2-mm-diameter endoscope)]. The primary end point of this study was stricture rate post-ESD.
Statistical analysis
Statistical analysis was performed using one-way ANOVA or Fisher’s exact test and SPSS 23.0 software (IBM Corp., Armonk, NY, USA). Values of P < 0.05 were considered statistically significant.
Results
Data from 27 patients were included in our analysis, with 13 patients in the IT+ST group and 14 patients in the OHA group. The characteristics of patients in the two groups are presented in Table 1. Demographic and pathological indexes including age, sex, tumor location, and resection size were similar between the two groups. There were six and seven complete and ≥3/4 circular ESD cases, respectively, in the IT+ST group, while four and ten patients underwent complete and ≥3/4 circular ESD, respectively, in the OHA group. No complications, including postsurgical bleeding, perforation, pneumomediastinum or local infection, were related to ESD in this study. Minor bleeding was observed perioperatively in all patients, with hemostasis achieved in all cases.
Table 1.
Patient characteristics.
| OHA group | IT+ST group | P-value | |
|---|---|---|---|
| Mean age (years) | 68.6 ± 9.0 | 64.6 ± 9.3 | 0.272 |
| Sex ratio (male:female) | 11:3 | 13:0 | 0.222 |
| 3/4 circular/>3/4 circular/complete circular ESD | 6/4/4 | 1/6/6 | 0.139 |
| Tumor location (UTE/MTE/LTE) | 1/12/7 | 3/8/5 | >0.05 |
| Wound length (cm) | 7.8 ± 2.9 | 7.9 ± 2.8 | 0.927 |
| Tumor depth M1/M2/M3/SM1/SM2 | 4/8/0/1/1 | 1/9/1/1/1 | 0.889 |
Values are mean ± standard deviation; OHA group, oral combination of hydrocortisone sodium succinate and aluminum phosphate gel; IT + ST group, endoscopic intralesional steroid injection and systemic steroid; ESD, endoscopic submucosal dissection; UTE, upper thoracic esophagus; MTE, middle thoracic esophagus; LTE, lower thoracic esophagus.
Tumor staging: M1, epithelial layer of mucosa; M2, lamina propria; M3, muscularis mucosae; SM1, submucous superficial layer invading less than 200 µm; SM2, submucous deep layer invading more than 200 µm.8
Post-surgery, stricture rates were 7.1% (1/14) and 53.8% (7/13) in the OHA and IT+ST groups, respectively (Table 2), and the differences between the two groups were statistically significant (P < 0.05). Furthermore, the number of balloon dilatation in patients with stenosis was markedly lower in the OHA group compared with the IT+ST group (P < 0.05; Table 2).
Table 2.
Stricture rates following endoscopic submucosal dissection.
| OHA group | IT+ST group | P-value | |
|---|---|---|---|
| Stricture, n (%) | 1 (7.1%) | 7 (53.8%) | 0.013 |
| Numbers of balloon dilation,Median (quartile) | 0 (0,0) | 0.5 (0,1) | 0.018 |
| Hypokalemia, n (%) | 9 (64.3%) | 9 (69.2%) | – |
OHA group, oral combination of hydrocortisone sodium succinate and aluminum phosphate gel; IT+ST group, endoscopic intralesional steroid injection and systemic steroid.
In our study, hypokalemia was reported between treatment days 2 and 11 in 18 patients (Table 2), 9 in the OHA group and 9 in the IT+ST group. Of these 18 patients, 6 had mild hypokalemia (3.0–3.5 mmol/L), 9 moderate hypokalemia (2.5–3.0 mmol/L), and 3 severe hypokalemia ( < 2.5 mmol/L). The serum potassium level was restored to normal of all the patients after potassium supplementation. No serious adverse events were reported for any patient in the study.
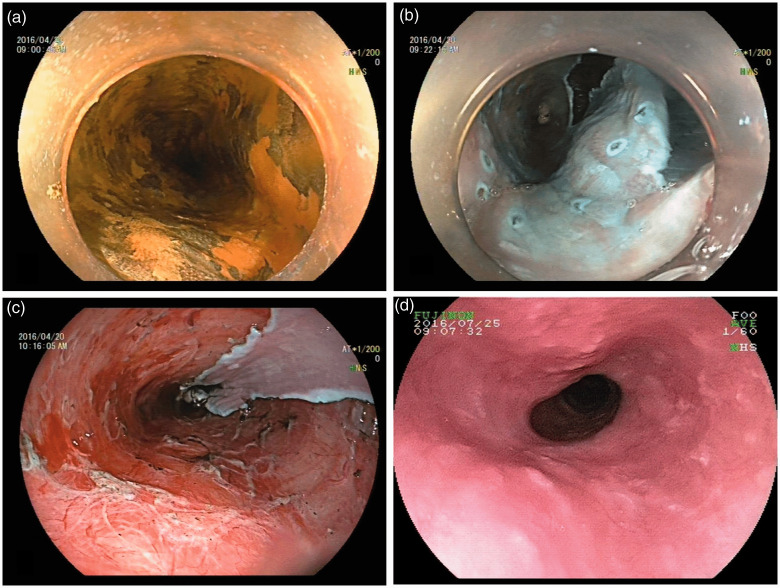
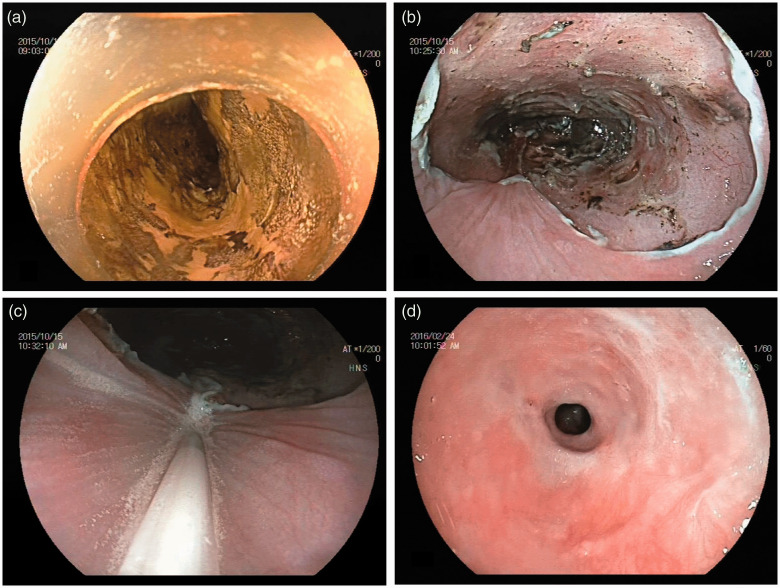
Representative OHA and IT+ST group cases are displayed in Figures 1 and 2, respectively.
Figure 1.
Endoscopic views of the esophagus in an OHA group case: (a) Chromoendoscopy with iodine staining revealed a discolored area in the mid-thoracic esophagus. Superficial esophageal cancer extended over three-quarters of the circumference, (b and c) Artificial ulcer immediately after endoscopic submucosal dissection (ESD), which resulted in a mucosal defect affecting more than three-quarters of the circumference and (d) No esophageal stricture was found during reexamination. OHA, oral combination of hydrocortisone sodium succinate and aluminum phosphate gel.
Figure 2.
Endoscopic views of the esophagus in an IT+ST group case: (a) Chromoendoscopy with iodine staining revealed a discolored area in the mid-thoracic esophagus. Superficial esophageal cancer extended over three-quarters of the circumference, (b) Artificial ulcer immediately after endoscopic submucosal dissection (ESD), which resulted in a mucosal defect affecting more than three-quarters of the circumference, (c) Injection of triamcinolone into the ulcer margin and (d) Esophageal stenosis was found upon reexamination. IT+ST, endoscopic intralesional steroid injection and systemic steroid.
Discussion
Given its effectiveness in lesion removal and low risk of trauma and mortality, ESD is widely used in the treatment of early, non-metastasized esophageal squamous cell cancer.8 However, inflammatory reactions and scar contracture associated with ESD can result in esophageal stricture. According to statistics from 2010 to 2014, esophageal stenosis occurs in 90% of patients with extensive ESD.9 Repeated treatment including balloon dilation and/or bougienage is usually required after stricture formation and when the patient’s quality of life decreases dramatically. Therefore, novel tools to prevent esophageal stenosis post-ESD are of prime importance. A variety of methods have been used previously for stricture prevention. Preventive EBD has been reported to reduce stenosis incidence to some extent.10 However, the procedure is repeated several times, imposing a significant burden on patients; in addition, the decrease in stricture rate remains unsatisfactory.5 Hashimoto et al.2 and Yasuaki et al.3 demonstrated that local injection of steroids is effective in preventing esophageal stenosis. Nevertheless, this approach can lead to esophageal perforation and infection. Rajan et al.11 reported a study in which four experimental pigs were all complicated with esophageal abscess after local administration of triamcinolone acetonide. Meanwhile, prednisolone administered orally has been shown to be effective for esophageal stricture prevention post-ESD.5–7 However, a stenosis rate of around 30% persists, and the treatment is associated with potential risks of prednisolone-related adverse events.4,12–14 Hydrocortisone sodium succinate is the main active ingredient of hormonal ointments for external use in dermatology. Clinical studies have confirmed that hydrocortisone can be absorbed locally in the gastrointestinal mucosa and play an anti-inflammatory role. Aluminum phosphate gel is commonly used as a protective agent for the mucosa of the digestive tract, has is characterized by a specific viscosity and larger contact area with the wound compared with the tablet form of aluminum phosphate. We therefore hypothesized that hydrocortisone could be combined with aluminum phosphate gel to increase its contact area, resulting in a mixed gel that might prevent scar formation and protect the mucous membrane. We instructed patients to lie down for a period of time after taking the gel to further increase contact time with the wound, thus maximizing efficacy and absorption of the hormone treatment. This method is simple and does not require an additional invasive procedure, thus increasing patient safety. Given the lack of previous studies on our treatment approach, our study procedures were based on the timing, dose, and course of treatment of prednisone. The reciprocal relationship between prednisone acetate and hydrocortisone is 5mg:20mg.15 Therefore, the initial dosage of prednisone was 30 mg and the corresponding dosage of hydrocortisone was 120 mg. To account for the effect of local injection of triamcinolone acetonide, an initial dose of hydrocortisone >120 mg was required. To increase wound absorption, hydrocortisone was given four times per day, with the initial dosage set at 200 mg (50 mg per administration). After 2 weeks, the dosage was reduced to half, and after 2 weeks, it was reduced to half again. However, to ensure the stability of local drug concentration, the frequency of drug use remained unchanged. Therefore, we assessed a new innovative strategy using OHA to prevent esophageal stricture occurrence, with promising outcomes observed in our analysis.
In the present study, we found that the stricture rate was markedly lower in the OHA group in comparison with the IT+ST group (P < 0.05). At the same time, the rate of balloon dilatation procedures in the OHA group was significantly lower than that in the IT+ST group (P < 0.05). These results showed that intralesional steroid injection and oral prednisone were suboptimal for the prevention of stricture formation, while the oral mixture gel was highly effective, had no risk of complications of injection such as perforation, and was easier to administer.
Eighteen patients developed hypokalemia following glucocorticoid administration. However, this adverse event quickly resolved in all patients following potassium supplementation, and no serious complications were reported.
Four patients with submucosal invasion selected ESD instead of surgery because initial CT results suggested no mediastinal lymphadenectasis. The first case underwent further surgery 2 months after ESD because of a residual lesion.
This study had several limitations, including its small sample size and retrospective design, with potential bias. Hence, large randomized controlled studies are required to confirm our hypothesis.
In conclusion, the novel treatment strategy of OHA has the potential to prevent esophageal stricture following large-circumference ESD in patients with early stage esophageal carcinoma. However, further investigation is required to validate these findings.
Declaration of conflicting interests
The authors declare that there is no conflict of interest
Funding
The study was supported by the Beijing Municipal Science & Technology Commission (grant no. Z171100001017091).
ORCID iD
Yonghui Huang https://orcid.org/0000-0002-0238-746X
References
- 1.Ishizaka K, Machida T, Tanaka Met al. Clinical efficacy of naftopidil on lower urinary tract symptoms after radical prostatectomy. Int J Urol 2009; 16: 299–302. [DOI] [PubMed] [Google Scholar]
- 2.Hanaoka N, Ishihara R, Takeuchi Yet al. Intralesional steroid injection to prevent stricture after endoscopic submucosal dissection for esophageal cancer: a controlled prospective study. Endoscopy 2012; 44: 1007–1011. [DOI] [PubMed] [Google Scholar]
- 3.Nagami Y, Shiba M, Tominaga Ket al. Locoregional steroid injection prevents stricture formation after endoscopic submucosal dissection for esophageal cancer: a propensity score matching analysis. Surg Endosc 2016; 30: 1441–1449. [DOI] [PubMed] [Google Scholar]
- 4.Wang W, Ma Z. Steroid administration is effective to prevent strictures after endoscopic esophageal submucosal dissection: a network meta-analysis. Medicine (Baltimore) 2015; 94: e1664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Isomoto H, Yamaguchi N, Nakayama Tet al. Management of esophageal stricture after complete circular endoscopic submucosal dissection for superficial esophageal squamous cell carcinoma. BMC Gastroenterol 2011; 11: 46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kataoka M, Anzai S, Shirasaki Tet al. Efficacy of short period, low dose oral prednisolone for the prevention of stricture after circumferential endoscopic submucosal dissection (ESD) for esophageal cancer. Endosc Int Open 2015; 3: E113–E117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sato H, Inoue H, Kobayashi Yet al. Control of severe strictures after circumferential endoscopic submucosal dissection for esophageal carcinoma: oral steroid therapy with balloon dilation or balloon dilation alone. Gastrointest Endosc 2013; 78: 250–257. [DOI] [PubMed] [Google Scholar]
- 8.Gastroenterology Branch of Chinese Medical Association, Cancer Endoscopy Committee of Chinese Anti Cancer Association. Consensus of Chinese early esophageal cancer screening and endoscopic diagnosis and treatment. Chinese J Pract Med 2015; 35: 320–377. [Google Scholar]
- 9.Ono S, Kodashima S, Fujishiro Met al. Clinical outcomes of endoscopic submucosal dissection for esophageal squamous carcinoma (in Japanese). Stomach Intest 2009; 44: 345–358. [Google Scholar]
- 10.Ezoe Y, Muto M, Horimatsu Tet al. Efficacy of preventive endoscopic balloon dilation for esophageal stricture after endoscopic resection. J Clin Gastroenterol 2011; 45: 222–227. [DOI] [PubMed] [Google Scholar]
- 11.Rajan E, Gostout C, Feitoza Aet al. Widespread endoscopic mucosal resection of the esophagus with strategies for stricture prevention: a preclinical study. Endoscopy 2005; 37: 1111–1115. [DOI] [PubMed] [Google Scholar]
- 12.Gaujoux-Viala C, Dougados M, Gossec L. Efficacy and safety of steroid injections for shoulder and elbow tendonitis: a meta-analysis of randomised controlled trials. Ann Rheum Dis 2009; 68: 1843–1849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sarnes E, Crofford L, Watson Met al. Incidence and US costs of corticosteroid-associated adverse events: a systematic literature review. Clin Ther 2011; 33: 1413–1432. [DOI] [PubMed] [Google Scholar]
- 14.Stuck AE, Minder CE, Frey FJ. Risk of infectious complications in patients taking glucocorticosteroids. Rev Infect Dis 1989; 11: 954–963. [DOI] [PubMed] [Google Scholar]
- 15.Ge J, Xu Y. Internal medicine. Beijing: People’s Medical Publishing House, 2014. [Google Scholar]