Abstract
Objectives: This study aims to identify factors that influence older adults’ reintegration to normal living 2 years following a hip fracture and the association between caregiver burden and reintegration over time. Methods: This longitudinal cohort study followed 76 community-dwelling older adults and their caregivers for 2 years post-hip fracture. The primary outcome was Reintegration to Normal Living Index (RNLI), and the secondary outcome was caregiver burden. Results: Older adults scored significantly lower on RNLI at 18 to 24 months if they had few social interactions, cognitive impairment, or lower pre-fracture functional status. During follow-up, greater independence in activities of daily living and greater mobility were each positively associated with RNLI. Caregiver burden reduced if reintegration improved. Implications: Results suggest a need for targeted interventions for older adults’ post-hip fracture to improve their function to enhance their reintegration to normal living and to support caregivers in decreasing their burden of care.
Keywords: hip fracture, reintegration to normal living, caregiver burden, cognitive impairment, rehabilitation models of care
Introduction
Reintegration to normal living (RNL) is defined as the reorganization of physical, social, and psychological characteristics of an individual into a harmonious whole so that one can resume normal living after a trauma (Wood-Dauphinee & Williams, 1987). The RNL is considered to be the ultimate aim of successful rehabilitation; however, for many older adults, this is not always achievable (Bourdeaua, Desrosiersa, & Gosselin, 2008). To date, only a few researchers have identified factors associated with RNL of older adults following rehabilitation, involving persons with stroke (Liu, Ng, Kwong, & Ng, 2015; Olawale, Usman, Oke, & Osundiya, 2018), acquired brain injury (Sady et al., 2010; Sandhaug, Andelic, Langhammer, & Mygland, 2015) and musculoskeletal conditions, which followed people with hip fractures for 3 months (Bourdeaua et al., 2008). These researchers found that higher independence in activities of daily living (ADL), functional mobility, and better cognitive function were positively associated with increased RNL. Caregiver support has been found to influence the ability for community reintegration for persons with traumatic brain injury 1 to 2 years post-injury (Sady et al., 2010).
Specific to being a caregiver for someone with a hip fracture, at 1-year post-hip fracture, increased caregiver burden was found to be associated with lower pre-fracture functional status, increased patient’s age, and younger age of the caregiver (Ariza-Vega, Ortiz-Piñ, Kristensen, Castellote-Caballero, & Jiménez-Moleón, 2017). Eleuteri, Bellanti, and Falaschi (2016) found that increased caregiver burden was associated with older adults’ lower general psychological wellbeing, anxiety, dementia, and depression, at 2-year follow-up for older adults with hip fracture.
To our knowledge, there is no study that has focused on examining older adults and their caregivers’ characteristics that are associated with RNL in persons with hip fracture following rehabilitation at 2-years post–hip fracture. In addition, the association between caregiver burden and RNL over an extended period of time for this cohort is not known. Providing evidence on the association between older adults’ reintegration into normal activities and caregiver burden is needed before interventions and support for the dyad are considered by policy decision makers. Therefore, the following research questions were proposed:
What characteristics of older adults with hip fracture and of their caregivers predict RNL and caregiver burden at 18- and 24-months post-discharge?
Is change in caregiver burden score associated with the change in RNL occurring at 18- and 24-months post-discharge?
Methods
Participants and Setting
This prospective study involved a 2-year post-discharge follow-up evaluation of participants who were initially enrolled in an intervention study, which compared the patient-centered rehabilitation model of care targeting persons with cognitive impairment (PCRM-CI) with usual care (McGilton et al., 2013). The cohort in this study included both intervention and control groups of patients with and without dementia. The participants’ inclusion criteria were as follows: age 65 years or older, living in the community at the time of the hip fracture, and having a caregiver. Caregivers’ inclusion criteria included those who were familiar with the older adults’ pre-fracture condition. Recruitment took place at two inpatient rehabilitation units in two community hospitals in Ontario, Canada, and patients were non-randomly assigned to PCRM-CI and usual care groups. The PCRM-CI intervention included five main components: (a) rehabilitation management, (b) dementia management, (c) delirium prevention, (d) education and support for the health care providers, and (e) support and education for family caregivers. The usual care consisted of rehabilitation management, including physical assessments at admission and daily 1-hr sessions of physical and occupational therapy, 5 days per week (McGilton et al., 2013), at the research sites. Older adults and/or their caregivers were re-consented at the 6-month period to participate in this longitudinal study.
Data Collection Procedures
Older adults and caregivers’ characteristics were collected at baseline (i.e., at the time of admission to the hospital) from the older adults (if they were capable) or from the caregivers by research assistants who were registered nurses. Participants’ data were also collected at the time of discharge from the unit using the Mini-Mental State Examination (MMSE) and Functional Independence Measurement (FIM) subscales (Self-care items of the FIM [FIMS] and Mobility items of the FIM [FIMM]). At 18- and 24-months post-discharge, the same nurse conducted telephone interviews with the older adults (if they were capable) and from the caregivers to collect follow-up data on the FIMS and FIMM and on Reintegration to Normal Living Index (RNLI) and the Zarit Burden Interview (ZBI).
Explanatory Variables
Older adults’ characteristics—age, sex, marital status, social interaction, and educational level as a proxy for socioeconomic status were collected. The social interaction variable was measured by assessing older adults’ frequency of social contacts with someone who does not live with him or her each week before the fracture (i.e., once a day or more, 2 to 6 times per week, once per week, and not at all).
Older adults’ health variables—cognitive impairment was measured at admission and rehabilitation center discharge using the MMSE (Folstein, Folstein, & McHugh, 1975; Mungas, 1991). Older adults were classified into two cognitive groups depending on their MMSE score: cognitively impaired (0-23) and no impairment (≥24) (Cockwell & Folstein, 2002). The MMSE was reported to have an excellent internal consistency (alpha = .90-.96) when used with older adults with and without dementia (Albert & Cohen, 1992; Foreman, 1987). Co-morbidities and the diagnosis of dementia were collected from the medical records and the pre-fracture functional status was collected during an interview with the caregiver using the Older American Resources and Service Instrument (OARS) (Fillenbaum & Smyer, 1981). Reliability of 0.87 and criterion validity has been reported for the OARS (Fillenbaum & Smyer, 1981).
Independence in ADL—The self-care items of the FIM referred to as FIMS, includes measures of eating, grooming, bathing, dressing, toileting, and continence (i.e., sphincter control). This subscale has a high internal consistency of 0.95 (Ottenbacher, Hsu, Granger, & Fiedler, 1996). The FIMS has been used with older adults with CI following hip fractures (Chaudhry, Devereaux, & Bhandari, 2013).
Functional mobility—The FIM motor subscale (FIMM), which contains 13 items, measures the older adults’ ability to walk, climb stairs, and the ability to transfer in and out of bed, toilet, and tub/shower. The FIMM has well-established reliability of 0.86 to 0.98 (Glenny & Stolee, 2009).
Caregiver characteristics—Caregiver’s age, marital status, employment status, relationship to the older adults, frequency of contact with the older adults over the past month (i.e., once a day or more, not at all, once a month, 2-4 times per month, and 5-28 times per month), and how well they knew the older adults’ health status, as well as the caregiver’s own present state of health.
Outcome Variables
The RNLI includes 11 items and was used to measure the older adults’ participation in activities, such as their self-care, ability to move around and travel within their community, and involvement in social activities based on what is necessary or important to them (Wood-Dauphinee et al., 1987). The scale takes into account the individuals’ perceptions of participating in normal activities following their illness or injury despite not identifying how integrated they were in life pre-injury state. Each item is scored using a visual analogue scale with a range from 0 (does not describe my situation) to 10 (fully describes my situation). The minimum range of scores is from 0 to 100. Higher total items scores of the RNLI indicate better reintegration (Wood-Dauphinee et al., 1987). The RNLI has demonstrated strong internal consistency when completed by a significant other (0.97) and good construct validity (0.77) with older adults (Bourget, Deblock-Bellamy, Blanchette, & Batcho, 2018).
Caregiver burden was measured using a 14-item modified version of the original ZBI (Flynn Longmire & Knight, 2011), which focuses on three factors: embarrassment/anger, older adults’ dependency, and self-criticism (Zarit, Reever, & Back-Peterson, 1980). The 14-item scale was found to offer a more parsimonious way to measure burden for both Black and White caregivers and when caregiver contact time is limited, such as when caring for persons with dementia. The items are scored from 0 to 4, with higher scores indicating higher levels of distress and burden. Total scores range from 0 to a maximum score of 56. Confirmatory factor analysis showed that the 14-item ZBI was reliable, highly correlated with the 22-item scale, and fairly normally distributed for two different groups of the race (Flynn Longmire & Knight, 2011).
Statistical Analyses
Within a cohort design, both our outcomes (RNL and caregiver burden) and two independent variables (functional mobility and independence of ADL) were each measured at 18- and 24-months post-discharge. To appropriately analyze these repeated measures of both outcomes and independent variables, we used cohort (panel) linear regression: specifically, the xtreg command in STATA. All other analyses were also performed using STATA version 14. First, univariate descriptive statistics were estimated for each caregiver’s and for each participant’s characteristic at each point of measurement. Second, bivariate random-effects cohort regressions were used to examine the relationship of each characteristic of participants and their caregivers separately with (a) RNL and (b) caregiver burden. Third, a random-effects cohort multiple regression model that included each characteristic found to be statistically significant in the bivariate models was used to examine the relationship of each characteristic against each outcome. This approach appropriately accounts for multiple independent variables, time-invariant covariates such those measured once at baseline, and also time-variant covariates measured repeatedly during this follow-up period such as FIMS and FIMM (Frees, 2004; Hsiao, 2014). Fourth, a random-effects regression model was used to examine the relationship of RNL with caregivers’ burden between older adult–caregiver-dyads during the follow-up period. Finally, a fixed-effects model was used to examine if changes over time in older adults’ level of RNL were associated with time-variant changes in the burden of their care during this period. This is important because such fixed-effects cohort regression models more fully exploit the longitudinal data by controlling for between-older adults and between-caregiver differences. Each analysis combined the PCRM-CI intervention and the usual care groups of our original study because these two groups did not differ more than expected by chance alone in any post-discharge longitudinal changes in any of the outcomes.
Missing values, common in longitudinal data, can potentially bias parameter estimates or compromise the representativeness of the sample. We evaluated the scope for bias caused by being lost to contact during the 2-year follow-up by comparing those we were unable to contact 1 year after discharge to the rest of the sample. We analyzed every variable measured from baseline through rehabilitation to 6-months post-discharge from rehabilitation, including repeated measures of older adults’ mobility and function, and characteristics of their caregivers. We found no statistical evidence that these two groups differed more than expected by chance alone. Because the relationship between older adults with hip fracture living at home and their reintegration into the home is the focus of our research, attrition caused by death or moving into long-term care (LTC) could not bias our results.
Results
Figure 1 details the number of participants in the study from admission to rehabilitation through the 24-month period following discharge and the loss of follow-up due to death, admission to LTC facility, or inability to contact them. At discharge from rehabilitation, the study included 70 participants who had received PCRM-CI and 75 who received usual care. Between discharge from rehabilitation and 24-months after discharge, 12 older adults had died from the PCRM-CI group, 10 were transferred to an LTC facility (they were dropped from the study as they were no longer living at home), and 17 were unable to be contacted. Comparatively, 11 died in the usual care group, 8 were relocated to LTC, and 7 were unable to be contacted. As a result, we were able to follow 80 older adults until 2-years post-discharge. Four older adults were excluded as they did not report on caregiver burden or RNL, which resulted in a final sample of 76 older adults and their caregivers. Of the 76 dyads in the sample, 33 dyads reported both RNL and caregiver burden at 18-months post-discharge and again at 24-months, 29 dyads did not report one of those, and 14 dyads did not report caregiver burden at either time. Summarized another way, 56 dyads reported RNL at 18 months post-discharge and 67 reported at 24 months post, for a total of 123 measurements of RNL during the follow-up period. For caregiver burden, 43 dyads reported at 18 months post and 52 at 24 months post, for a total of 95 measurements of caregiver burden during the follow-up period.
Figure 1.
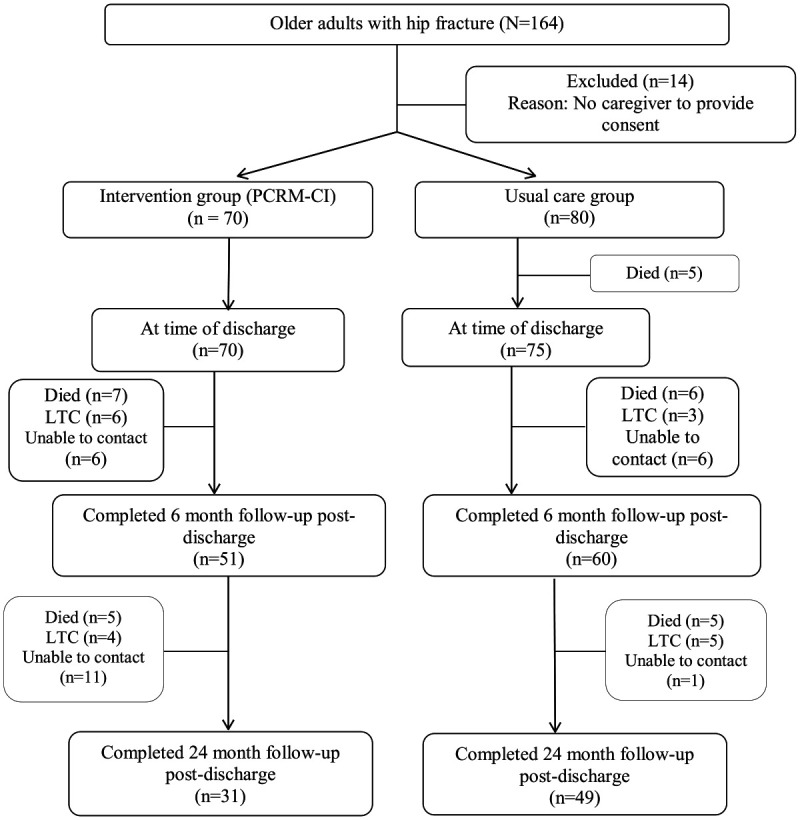
PCRM-CI participant study flow diagram.
Characteristics of Older Adults and Their Caregivers
We present the older adults’ characteristics in Table 1. The 76 older adults with intracapsular (46%), intertrochanteric (37%), subtrochanteric, and other hip fractures (17%), had a mean age of 81.6, were mostly female (83%), 18% had a diagnosis of dementia, 78% had three or more chronic conditions, and 69% had a history of falls. There was a slight improvement in the mean score of FIMM from 18-months (27.5) to 24-months (27.8) and the mean score of RNLI from 18-months (31.3) to 24-months (33.3).
Table 1.
Characteristics of Older Adults at 18- and 24-Months Post-Discharge.
| Variables | n (%)/M ± SD (n = 76) |
|---|---|
| Socio-demographic characteristics | |
| Age (M ± SD) | 81.6 ± 8.1 |
| Sex, female (n[%]) | 63 (83) |
| Education, fewer than 12 years (n[%]) | 13 (18) |
| Marital status, married or common law partner (n[%]) | 26 (34) |
| Health status and physical functions at admission | |
| Pre-fracture functional status, OARS (M ± SD) | 24.0 ± 5.0 |
| Cognitive impairment at admission, MMSE (n[%]) | 15 (20) |
| Diagnosed dementia (n[%]) | 13 (18) |
| Chronic conditions (3 or more) (n[%]) | 59 (78) |
| History of falls (n[%]) | 51 (69) |
| Previous fall with injury (n[%]) | 42 (55) |
| Few social interactions (no social interaction or at most 1 visit per week) (n[%]) | 15 (20) |
| Health status at discharge | |
| Independence in Activities of Daily Living, FIMS (M ± SD) | 51.9 ± 4.0 |
| Functional mobility, FIMM (M ± SD) | 26.2 ± 4.3 |
| Cognitive impairment, MMSE (M ± SD) (n = 65) | 26.9 ± 3.2 |
| Health status at 18-months post-discharge (n = 56) | |
| Independence in activities of daily living, FIMS (M ± SD) | 50.4 ± 7.3 |
| Functional mobility, FIMM (M ± SD) | 27.5 ± 5.3 |
| Participation across multiple areas of life—The Reintegration to Normal Living Index (RNLI) (M ± SD) | 71.0 ± 21.2 |
| Health status at 24-months post-discharge (n = 67) | |
| Independence in activities of daily living, FIMS (M ± SD) | 50.6 ± 7.5 |
| Functional mobility, FIMM (mean ± SD) | 27.8 ± 5.6 |
| Participation across multiple areas of life—The Reintegration to Normal Living Index (RNLI) (M ± SD) | 75.7 ± 21.4 |
Note. OARS = Older Americans Resources and Services Instrument; MMSE = Mini-Mental State Examination; FIMS = Functional Independence Measure Self-care Subscale; FIMM = Functional Independence Measure Mobility Subscale.
Characteristics of the caregivers are presented in Supplementary Material 1, which can be accessed online through the Journal of Applied Gerontology. Almost all of the participants were family members, female (75%), with an average age of 65.4. Most often caregivers were the spouse (35%), worked full-time (26%), self-reported of good to excellent health (64%), and felt that they knew the health of their family member very well (85%).
Older Adults and Their Caregiver’s Characteristics as Predictors of RNLI at 18- and 24-Months Post-Discharge
Results from bivariate random-effect regression models that relate each characteristic of older adults and each of caregivers separately to older adults RNLI and caregiver burden appear in Table 2. Older adults scored lower on RNLI at 18- and 24-months post-discharge if they were older, less educated, lower pre-fracture functional status, cognitively impaired, diagnosed with dementia, had few social interactions (i.e., no social visits or at most 1 visit per week) at the time of hip fracture, three or more chronic conditions, or scored lower on either FIMS and FIMM subscales during the follow-up period (Table 2, bivariate models). Results from a model that accounted for multiple independent variables support RNLI’s negative association with cognitive impairment and few social interactions; and RNLI’s positive association with pre-fracture functional status and during the follow-up period each of the FIMS and FIMM subscales (Table 2, adjusted model). This model explains 68% of variation in RNLI. We found no statistical evidence of association between any other characteristic of older adults, nor of caregivers.
Table 2.
Older Adults and Caregivers Predictors of Reintegration to Normal Living and Caregiver Burden at 18- and 24-Months Using Adjusted and Unadjusted Analysis.
| Predictor | Unstandardized beta (95% CI) | |||
|---|---|---|---|---|
| Reintegration to Normal Living (123 measurements of 76 older adult–caregiver dyads) | Caregiver burden (95 measurements of 62 older adult–caregiver dyads) | |||
| Unadjusted bivariate models | Adjusted for multiple independent variables (overall R2 = .68) | Unadjusted bivariate models | Adjusted for multiple independent variables (overall R2 = .15) | |
| Socio-demographic characteristics of older adult | ||||
| Age | −0.6* [–1.2, –0.03] R2 = .03 | −0.3 [–0.7, 0.05] | 0.11 [–0.2, 0.4] | |
| Female | −3.2 [–16, 9] | −1.3 [–7.4, 4.8] | ||
| Less than high school | −14* [–26, –1.5] R2 = .04 | −7.3 [–15.4, 0.9] | 5.0 [–1.1, 11.1] | |
| Married or partner | 1.0 [–8.8, 10.9] | −1.9 [–6.6, 2.9] | ||
| Older adult’s health status at admission | ||||
| Pre-fracture functional status | 2.3*** [1.6, 3.1] R2=.32 | 1.0* [0.2, 1.8] | −0.7*** [–1.1, 0.3] R2 = .13 | −0.4 [–1.0, 0.1] |
| Cognitive impairment | −25*** [–35, –16] R2 = .28 | −9.4* [–18.7, –0.05] | 6.2* [1.0, 11.5] R2 = .09 | 2.7 [–3.3, 8.7] |
| Diagnosed dementia | −14* [–26, –2.6] R2 = .07 | 5.1 [–4.5, 14.6] | 2.6 [–2.9, 8.0] | |
| Few social interactions | −16** [–27, –4.4] R2 = .12 | −11.0** [–18.9, –3.1] | 2.1 [–3.3, 7.5] | |
| Chronic conditions (3 or more) | −11* [–22, –0.3] R2 = .05 | −4.2 [–11.3, 2.9] | 3.2 [–2.7, 9.0] | |
| History of previous falls | 3.7 [–6.6, 13.9] | 3.9 [–1.3, 9.1] | ||
| Older adult’s health status at 18- and 24-months post-discharge | ||||
| Independence in activities of daily living (FIMS) | 1.4*** [1.0, 1.8] R2 = .49 | 0.8** [0.3, 1.3] | −0.3* [–0.6, –0.04] R2 = .08 | −0.1 [–0.5, 0.3] |
| Functional mobility (FIMM) | 1.7*** [1.2, 2.2] R2 = .41 | 0.7* [0.004, 1.3] | −0.4* [–0.8, –0.04] R2 = .08 | −0.1 [–0.7, 0.5] |
| Caregiver’s characteristics | ||||
| Caregiver age | 0.2 [–0.2, 0.6] | −0.2 [–0.4, 0.01] | ||
| Caregiver in full-time employment | 4.7 [–15.6, 6.1] | 0.02 [–5.3, 5.4] | ||
| Caregiver contact less frequent than every day | −4.3 [–1.1, 5.5] | 3.2 [–1.8, 8.3] | ||
| Caregiver’s own health good to excellent | 1.5 [–8.2, 11.3] | −1.2 [–6.0, 3.6] | ||
| Caregiver knows older adult’s health well to very well | 11 [–2.1, 24] | −3.7 [–10.7, 3.3] | ||
Note. Each multiple regression model is adjusted for each covariate found statistically significant in its bivariate regression. FIMS = Functional Independence Measure Self-care Subscale; FIMM = Functional Independence Measure Mobility Subscale.
p < .05. **p < .01. ***p < .001.
Older Adults and Their Caregivers’ Characteristics as Predictors of Caregiver Burden at 18- and 24-Months Post-Discharge
Following bivariate regression analyses, caregivers perceived their burden of care at 18- and 24-months post-discharge to be significantly greater if they were caring for an older adult with lower pre-fracture functional status, cognitively impaired, or an older adult who scored lower on either FIM sub-scale (Table 2, adjusted table). Results from a random-effects regression model that accounted for multiple independent variables found little statistical evidence for these covariates (overall R2 = .15), but RNLI alone explained 42% of the variation in caregiver burden between older adult–caregiver-dyads during this follow-up period (Table 3, random-effects regression model). We found no statistical evidence of an association between any other characteristic of older adults, nor of caregivers. Multicollinearity was also examined in each of these regression models. In each case, estimates for regression coefficients for FIMS and FIMM were stable when one or the other was dropped from the analysis, so both were included in our results. All other pairs of covariates had correlations less than 0.5.
Table 3.
Cohort Regression Results Assessing the Relationship Between Caregiver Burden and Older Adult Reintegration to Normal Living at 18-Months and 24-Months Post-Discharge From Hip Fracture Rehabilitation.
| Parameter | Estimate (95 measurements on 62 olderadult–caregiver dyads) | |
|---|---|---|
| Random-effect model | Fixed-effect model | |
| Unstandardized beta for changes in RNLI associated with change in caregiver burden (95% confidence interval) | −0.3 [–0.4, –0.2]*** | −0.3 [–0.6, –0.03]* |
| SD among olderadult–caregiver dyads | 5.4 | 6.6 |
| SD repeated measures within olderadult–caregiver dyads | 4.6 | 4.6 |
| Fraction of variance among olderadult–caregiver dyads | 0.58 | 0.67 |
| Overall R2 | .42 | .42 |
Note. Caregiver burden as measured by Zarit Burden Interview (ZBI); Olderadult reintegration as measured by Reintegration to Normal Living Index (RNLI). The random-effects model does not adjust for any other characteristics of older adults or caregivers. In contrast, the fixed-effects cohort regression model exploits the longitudinal data to control for between-dyad differences of both the older adult and the caregiver.
p < .05. ***p < .001.
Changes in Caregiver Burden Score Were Associated With Changes in RNLI
The results from the fixed-effects regression model show that change occurring from 18- to 24-months post-discharge in a caregivers’ perception of their burden of care was inversely associated with change in the RNLI score of their older adult (Table 3). Burden reduced if reintegration improved within olderadult–caregiver-dyads during this post-discharge follow-up period.
Discussion
One of the main goals for older adults who experience a hip fracture is to reintegrate into normal ADL (Levasseur, Desrosiers, & Noreau, 2004). Ours is the first attempt at linking the older adults’ ability to return to family and community life and engage in normal activities post-hip fracture and its’ association with caregiver burden, physical, and cognitive abilities of the older adult and their social interactions at 18- and 24-months post hip fracture surgery. Our novel findings highlight that reintegration and caregiver burden are associated so if reintegration into usual activities for the older adult is improved, caregiver burden might be reduced and vice a versa. This work adds to the relatively few reports of factors influencing RNL and provides opportunities to improve the recovery of older adults post-hip fracture.
Results of the current study show that older adults, who experienced lower pre-fracture functional status and/or cognitive impairment, scored lower on RNLI. Conversely, greater independency in ADL and functional mobility was positively associated with RNLI. Bourdeaua and colleagues (2008) found similar results, whereby persons with cognitive impairment were associated with lower RNLI scores and higher RNLI scores were associated with greater independence in older adults’ ADL and functional mobility at 3-months post-hip fracture. In terms of policy implications, perhaps using RNLI scores could be a useful assessment to identify individuals in the community who are in need of scarce home and social care services. Providing access to education for informal caregivers or additional home care services can help maintain the persons’ abilities for as long as possible (Poulos et al., 2017), which is crucial when maintaining the independence of older adults with cognitive impairment.
Our study revealed additional factors influencing RNL, namely the number of social interactions and caregiver burden. The results lead to the possibility that caregiver burden might be reduced if the person with a hip fracture reintegrates into their past routines. Likewise, if the caregiver has less burden, the older adult might be better reintegrated into normal routines as the caregiver might have more energy to drive the older adult to community events or invite their friends over for a visit. These results provide insights into possible interventions that provide support for caregivers. One way of providing support is through ensuring respite breaks which may be beneficial for both the caregiver and older adult. Another type of intervention that may provide psychosocial support for caregivers are interventions that enhance social interactions and help with the reintegration into regular routines, like walking programs provided by community services and support groups. Similar to other studies (Sady et al., 2010), a positive social support system including the number of social visits made by friends was positively associated with reintegration into normal living. Overall, older adults who received more visits were better reintegrated during the follow-up period. This provides insights into possible interventions in the future—more friendly home visits are required, as community involvement and support networks have never been so important for those highly complex vulnerable older adults wishing to remain at home and their caregivers.
The results of the study also suggest that older adults’ pre-fracture functional status function, mobility, and cognitive status were associated with caregivers’ burden. Similar findings have found that family members of older adults with CI post-hip fracture perceived more burden and sadness than family members of older adults with intact cognition (Hedman, Stromberg, Grafstrom, & Heikkila, 2011). On average, the caregivers in this study were women in their late 60s, being either spouses or daughters. Due to the unexpected event of a hip fracture, most caregivers provide care without prior training or knowledge (Avila, Pereira, & Bocchi, 2015). There must, therefore, be an awareness of the caregivers’ vulnerabilities and risks. They may be putting themselves at risk for injuries related to heavy lifting and the increasing care required of their relatives who may become more impaired over time.
The chief limitation of the study is the loss to follow-up and the reduced sample size. But we note that covariates whose association with an outcome was as small as R2 = .03 to .07 were found to be statistically significant in these analyses and that a post hoc power calculation at 80% power confirms a required effect size as measured by Cohen’s ƒ2 of about 0.07 for these regressions. The main strengths of this study are its population and design. We were able to follow older adults and their caregivers over a 2-year period and longitudinally track caregiver and older adults’ outcomes. We also were able to employ robust statistical methods to identify and minimize biases.
Conclusion
The study indicates that reintegration into normal living is more likely to occur for older adults who are less dependent. The older adults’ ability to be reintegrated into normal living is associated with reduced caregiver burden. The results suggest a need for targeted interventions to support the caregivers of older adults and to ensure that older adults maintain their abilities as long as possible.
Supplemental Material
Supplemental material, Supplement_Aug_6 for Factors That Influence the Reintegration to Normal Living for Older Adults 2 Years Post Hip Fracture by Katherine S. McGilton, Abeer Omar, Steven S. Stewart, Charlene H. Chu, Meagan B. Blodgett, Jennifer Bethell and Aileen M. Davis in Journal of Applied Gerontology
Acknowledgments
We wish to acknowledge the older adults and care partners who allowed us into their lives to understand their journeys. Dr. McGilton is supported by the Walter and Maria Schroeder Institute for Brain Innovation & Recovery.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Ethical Approval: University Health Network Research Ethics Board: # 09-016
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This study was supported by a demonstration grant from the Canadian Institutes of Health Research—Institute of Aging (DPA—93049).
ORCID iDs: Abeer Omar  https://orcid.org/0000-0002-4713-2874
https://orcid.org/0000-0002-4713-2874
Charlene H. Chu  https://orcid.org/0000-0002-0333-7210
https://orcid.org/0000-0002-0333-7210
Supplemental Material: Supplemental material for this article is available online.
References
- Albert M., Cohen C. (1992). The test for severe impairment: An instrument for the assessment of patients with severe cognitive dysfunction. Journal American Geriatrics Society, 40, 449-453. [DOI] [PubMed] [Google Scholar]
- Ariza-Vega P., Ortiz-Piña M., Kristensen M., Castellote-Caballero Y., Jiménez-Moleón J. (2017). High perceived caregiver burden for relatives of older adults following hip fracture surgery. Disability and Rehabilitation, 201, 1-8. doi: 10.1080/09638288.2017.1390612 [DOI] [PubMed] [Google Scholar]
- Avila M., Pereira G., Bocchi S. (2015). Informal caregivers of older people recovering from surgery for hip fractures caused by a fall: Fall prevention. Ciência & Saúde Coletiva, 20, 1901-1907. [DOI] [PubMed] [Google Scholar]
- Bourdeaua I., Desrosiersa J., Gosselin S. (2008). Predictors of reintegration to normal living in older adults discharged from an intensive rehabilitation program. International Journal of Rehabilitation Research, 31, 267-274. doi: 10.1097/MRR.0b013e3282fc0ff2 [DOI] [PubMed] [Google Scholar]
- Bourget N., Deblock-Bellamy A., Blanchette A. K., Batcho C. S. (2018). Use and psychometric properties of the Reintegration to Normal Living Index in rehabilitation: A systematic review. Annals of Physical and Rehabilitation Medicine, 61, 262-269. doi: 10.1016/j.rehab.2017.12.004 [DOI] [PubMed] [Google Scholar]
- Chaudhry H., Devereaux P. J., Bhandari M. (2013). Cognitive dysfunction in hip fracture patients. Orthopedic Clinic of North America, 44, 153-162. [DOI] [PubMed] [Google Scholar]
- Cockwell J. R., Folstein M. F. (2002). Mini-mental status exam. In Copeland J. R. M., Abou-Saleh M. T., Blazer D. G. (Eds.), Principles and practice of geriatric psychiatry (2nd ed., pp. 140-156). Chichester, UK: John Wiley; Retrieved from https://onlinelibrary.wiley.com/doi/pdf/10.1002/0470846410.ch27%28ii%29 [Google Scholar]
- Eleuteri S., Bellanti G., Falaschi P. (2016). Hip fracture: Preliminary results supporting significative correlations between the psychological wellbeing of patients and their relative caregivers. Journal of Gerontology and Geriatrics, 64, 104-111. [Google Scholar]
- Fillenbaum G. G., Smyer M. A. (1981). The development, validity, and reliability of the OARS multidimensional functional assessment questionnaire. Journal of Gerontology, 36, 428-434. [DOI] [PubMed] [Google Scholar]
- Flynn Longmire C. V., Knight B. G. (2011). Confirmatory factor analysis of a brief version of the Zarit Burden Interview in Black and White dementia caregivers. The Gerontologist, 51, 453-462. doi: 10.1093/geront/gnr011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Folstein M. F., Folstein S. E., McHugh P. R. (1975). “Mini-mental state”: A practical method for grading the cognitive state of patients for the clinician. Journal of Psychiatric Research, 12, 189-198. [DOI] [PubMed] [Google Scholar]
- Foreman M. D. (1987). Reliability and validity of mental status questionnaires in elderly hospitalized patients. Nursing Research, 36, 216-220. [PubMed] [Google Scholar]
- Frees E. W. (2004). Longitudinal and panel data: Analysis and applications in the social sciences. Cambridge, UK: Cambridge University Press. [Google Scholar]
- Glenny C., Stolee P. (2009). Comparing the functional independence measure and the interRAI/MDS for use in the functional assessment of older adults: A review of the literature. BMC Geriatrics, 9, 52. doi: 10.1186/1471-2318-9-52 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hedman A., Stromberg L., Grafstrom M., Heikkila K. (2011). Hip fracture older adults’ cognitive state affects family members’ experiences—A diary study of the hip fracture recovery. Scandinavian Journal of Caring Sciences, 25, 451-458. doi: 10.1111/j.1471-6712.2010.00848.x [DOI] [PubMed] [Google Scholar]
- Hsiao C. (2014). Analysis of panel data (3rd ed.). New York, NY: Cambridge University Press. [Google Scholar]
- Levasseur M., Desrosiers J., Noreau L. (2004). Is social participation associated with quality of life of older adults with physical disabilities? Disability Rehabilitation, 26, 1206-1213. [DOI] [PubMed] [Google Scholar]
- Liu T., Ng S., Kwong P., Ng G. (2015). Fear avoidance behavior, not walking endurance, predicts the community reintegration of community-dwelling stroke survivors. Archives of Physical Medicine & Rehabilitation, 96, 1684-1690. doi: 10.1016/j.apmr.2015.05.005 [DOI] [PubMed] [Google Scholar]
- McGilton K., Davis A., Naglie G., Mohamed N., Flannery G., Jaglal S., Stewart S. (2013). Evaluation of older adults-centered rehabilitation model targeting older persons with a hip fracture, including those with cognitive impairment. BMC Geriatrics, 13(1), 136. doi: 10.1186/1471-2318-13-136 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mungas D. (1991). In-office mental status testing: A practical guide. Geriatrics, 46, 54–58, 63, 66. [PubMed] [Google Scholar]
- Olawale O. A., Usman J. S., Oke K. I., Osundiya O. C. (2018). Evaluation of predictive factors influencing community reintegration in adult patients with stroke. Journal of Neurosciences in Rural Practice, 9, 6-10. doi: 10.4103/jnrp.jnrp_386_17 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ottenbacher K. J., Hsu Y., Granger C. V., Fiedler R. C. (1996). The reliability of the functional independence measure: A quantitative review. Archives of Physical Medicine & Rehabilitation, 77, 1226-1232. [DOI] [PubMed] [Google Scholar]
- Poulos C. J., Bayer A., Beaupre L., Clare L., Poulos R. G., Wang R. H., McGilton K. S. (2017). A comprehensive approach to reablement in dementia. Alzheimer’s & Dementia (New York, N. Y.), 3, 450-458. doi: 10.1016/j.trci.2017.06.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sady M. D., Sander A. M., Clark A. N., Sherer M., Nakase-Richardson R., Malec J. F. (2010). Relationship of preinjury caregiver and family functioning to community integration in adults with traumatic brain injury. Archives of Physical Medicine & Rehabilitation, 91, 1542-1550. doi: 10.1016/j.apmr.2010.07.012 [DOI] [PubMed] [Google Scholar]
- Sandhaug M., Andelic N., Langhammer B., Mygland A. (2015). Community integration 2 years after moderate and severe traumatic brain injury. Brain Injury, 29, 915-920. doi: 10.3109/02699052.2015.1022880 [DOI] [PubMed] [Google Scholar]
- Wood-Dauphinee S., Williams J. I. (1987). Reintegration to normal living as a proxy to quality of life. Journal of Chronic Diseases, 40, 491-502. [DOI] [PubMed] [Google Scholar]
- Zarit S. H., Reever K. E., Back-Peterson J. (1980). Relatives of the impaired elderly: Correlates of feelings of burden. The Gerontologist, 20, 649-655. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, Supplement_Aug_6 for Factors That Influence the Reintegration to Normal Living for Older Adults 2 Years Post Hip Fracture by Katherine S. McGilton, Abeer Omar, Steven S. Stewart, Charlene H. Chu, Meagan B. Blodgett, Jennifer Bethell and Aileen M. Davis in Journal of Applied Gerontology


