Abstract
Life course theories suggest that geographic disparities in mortality may reflect a history of place-based exposures rather than (or in addition to) contemporaneous exposures; yet, few studies examined early life place exposures and later life mortality in the US due to data limitations. The aim of this study is to assess and compare the importance of state of birth and state of residence in predicting mortality for adults over age 50 in the US. Using nationally representative data of nearly 100,000 adults over age 50 from the National Longitudinal Mortality Study, we estimated individual mortality risk using multi-level logistic regression with state of birth and state of residence as second-level random effects. We assessed whether state of residence and state of birth contributed to the variation in adult mortality. We also decomposed state-of-residence random effects to compare “movers” and “stayers.” Our results indicate that state of birth is a stronger predictor of age-, race/ethnicity- and sex-adjusted mortality in the US than state of residence at the time of death. The adult mortality profiles of many states are substantially impacted by the composition of “movers.” Failing to account for residential mobility has clouded our understanding of the patterns and causes of geographic differences in adult mortality. Measures of geographic residence across the life course can improve models of adult mortality in the US and inform interventions to address geographic disparities in longevity.
Keywords: Place of birth, Geographic disparities, Mortality
Highlights
-
•
State of birth is a stronger predictor of later age mortality than state of residence.
-
•
Geographic inequalities in mortality are results from complex groupings of “movers” and “stayers”.
-
•
Incorporating geographic residence across the life course improves models of adult mortality.
1. Introduction
Geographic differences in mortality and health in later life are large and well-documented. The gap in life expectancy across US states is approximately 7.5 years (Wilmoth, Boe, & Barbieri, 2010). Contextual factors are increasingly recognized as key determinants of population health, but much remains to be understood about which contexts matter, when, and how.
A central issue in understanding the large and important place-based differences in old age health and mortality is unpacking the forces reflected in the estimates. Life course and Developmental Origins of Adult Health and Disease (DOHaD) theories suggest that some differences in health may reflect a history of place-based exposures rather than (or in addition to) contemporaneous exposures (Ben-Shlomo & Kuh, 2002; Kuh & Ben-Shlomo, 2004). The effects of this history can both accumulate into old age and shape later exposures through various mechanisms. (Feijten, Hooimeijer, & Mulder, 2008; Gustafsson, Hammarström, & San Sebastian, 2015; Montez & Hayward, 2011).
Migration is one key mechanism differentiating past and present place-based exposures. 30–40% of the US population reside in a state they were not born in (Molloy, Smith, & Wozniak, 2011; US Census Bureau, 2011), and recent annual inter-state mobility rate is estimated to range from 1% to 3% (Hyatt, McEntarfer, Ueda, & Zhang, 2018; Kaplan & Schulhofer-Wohl, 2017; Molloy et al., 2011). Thus, a large component of place-based disparities may be attributable to early exposures that are distinct from exposures later in life. However, standard mortality estimates are based on place of death or late-life residence, and rarely draws attention to geographic exposures in early life.
Previous studies have documented the effects of state of residence contexts on adult health by examining measures of socioeconomic status (Montez, Hayward, & Wolf, 2017; Montez, Zajacova, & Hayward, 2016; Subramanian, Kawachi, & Kennedy, 2001), tax policies (Montez et al., 2017; Montez, Hayward, & Zajacova, 2019), social capital and cohesion (Montez et al., 2016; Subramanian et al., 2001) and income inequality (Backlund et al., 2007; Montez et al., 2017; Subramanian et al., 2001). Recent research has pointed to the effects of state of birth on early life health outcomes. For example, empirical studies have shown that infant birth outcomes (e.g. low birth weight) vary by state-level factors including poverty reduction policies (e.g. Earned Income Tax Credit, minimum wage) (Komro, Livingston, Markowitz, & Wagenaar, 2016; Komro, Markowitz, Livingston, & Wagenaar, 2019; Strully, Rehkopf, & Xuan, 2010), health insurance policies (e.g. Medicaid expansion) (Brown et al., 2019), and access to health care resources (Shi et al., 2004). Other studies also find that early life exposure to state policies and resources is associated with children's health care coverage and health status (Baughman & Duchovny, 2016) and school achievement (Bastian & Michelmore, 2018; Dahl & Lochner, 2012) as well as adults' work efforts and earnings (Bastian & Michelmore, 2018; Duncan, Ziol-Guest, & Kalil, 2010), all of which have important implications for subsequent health and mortality.
However, few studies have directly linked state of birth and adult mortality, partially due to lack of suitable data. Indeed, many large studies of mortality in the US lack the capacity to consider geographic exposures at multiple points in the life course. Surveys that ask about state of birth (e.g. Health and Retirement Study) often lack a sufficient number of observations for exploring state-level variation in mortality, and larger datasets (e.g. National Vital Statistics System) do not tabulate the population at risk for mortality by early life geographic details (e.g. state of birth).
Using a unique data source that combines information on place of birth and place of residence for a large representative sample of Americans, our study addresses the following 3 questions: (1) how much does US adult mortality vary across states of residence? (2) how much does US adult mortality vary across states of birth? and (3) how much of the variation in US adult mortality across states of residence is due to “stayers” (whose state of birth and state of residence were the same) and “movers” (whose state of birth and state of residence were difference)? While we are not able to examine specific mechanisms through which state of birth and/or state of residence affect mortality in this Short Communication, our aim is to draw attention to the contribution of early life places (i.e. states of birth) to the effects usually attributed to states of residence in comparisons of mortality across the US.
2. Methods
The data used in this study were derived from the National Longitudinal Mortality Study (NLMS). NLMS is a nationally-representative, random sample of non-institutionalized Americans developed for studying demographic, socioeconomic, and occupational disparities in mortality (Makuc et al., 1984). The public-use file consists of a subset of 11 of the 26 Current Population Survey (CPS) cohorts in the full NLMS. The 11 surveys, collected throughout the early 1980s, were combined and re-weighted so they are considered equivalent to a large sample representative of the US population on April 1, 1983. For study members who died, records were linked to the National Death Index (NDI), a centralized national mortality database (Curb et al., 1985). All participants were followed up for 11 years, except for those who deceased during the period. The third release of the NLMS public-use file included the state of residence (at the time of baseline interview) and state of birth for the study participants for the first time, allowing us to compare the significance of both state of residence and state of birth in predicting adult mortality risk. We focused our analysis on individuals who were aged 50 and over at the baseline interview and excluded respondents who were foreign born or had missing information for place of birth or survey weight. Our analytic sample includes 94,458 US-born individuals. In our analysis of “movers” and “stayers”, only state migration streams with more than 20 individuals were included.
2.1. Measures
Mortality. We used a binary variable Death Indicator (INDDEA) to denote whether the study participant died (1 = yes, 0 = no) during the 11-year follow-up period after the Current Population Survey (CPS) interview.
State of Birth. State of birth was constructed from the Place of Birth (POB) variable in the original study. NLMS uses the National Death Index Geographical Codes for states of birth. We used a crosswalk to recode the states so that the coding conforms with the Federal Information Processing Standards (FIPS) for state codes.
State of Residence. State Recode (STATER) was used to indicate the state of residence of study participants at the date of interview. In NLMS, the first digit of STATER is the Census Bureau division code and the second digit is the state within each division. Similar to state of birth, we also recoded state of residence according to the state FIPS codes.
Covariates. Age is a continuous variable indicating the age of study participants at the date of interview. The age of participants in our sample ranges from 50 to 90. According to the survey manual, the age variable is top coded at 90 years, meaning individuals who were older than 90 years at baseline were considered 90 years old. Sex was also used as a covariate to account for the differential mortality risk between men and women. Race and ethnicity were used to account for the differential mortality risk between racial and ethnic groups. We decided against additional controls, such as years of schooling and income, because these variables are conditioned on state contexts and thus are potential mediators of the total state effects on adult mortality.
2.2. Analytic strategy
We first summarized the demographic distribution of our study sample. Next, we estimated a series of multi-level logistic regression models with state of residence and/or state of birth random effects. The first model estimates the log-odds of mortality for individual i from state of residence j. The second model estimates the log-odds of mortality for individual i from state of birth k. The third/full model estimates the log-odds of mortality from both state of residence and state of birth. All models were adjusted for age (in single years), sex and race/ethnicity. The full model is specified as Equation (1):
| (1) |
where and In the model, is the average log-odds of mortality among individuals in the sample, is the effect of state of residence and is the effect of state of birth. Both are assumed to be normally distributed. is the error term. All regression models are weighted to account for the study design. Last, using the 2000 US population as the standard population, we calculated age-standardized mortality rates by state of residence as well as by state of residence and state of birth interaction. To illustrate the heterogeneity in mortality across states of birth and residence, we created figures showing the differences in mortality rate between “stayers” and “movers” within states of residence. All statistical analyses were carried out in R, version 3.6.3 (R Core Team, 2020).
3. Results
Summary statistics of the study sample are presented in Table 1. Among the 94,458 individuals in our sample, 33,612 (35.6%) died during the 11-year follow-up period. The mean age at time of interview of those who subsequently died was 69.62 (standard deviation (SD) = 9.96); while the mean age at interview for those who lived throughout the follow-up period was 59.31 (SD = 7.33). Among those died, 16,036 (47.7%) were female, compared to 36,274 (59.6%) among those who survived.
Table 1.
Descriptive statistics.
| Death indicator |
||
|---|---|---|
| 0 | 1 | |
| N | 60,846 | 33,612 |
| Age | 59.31 (7.33) | 69.62 (9.96) |
| Age group | ||
| 50–54 years | 18,871 (31.0%) | 2402 (7.1%) |
| 55–59 years | 16,562 (27.2%) | 3738 (11.1%) |
| 60–64 years | 11,877 (19.5%) | 4732 (14.1%) |
| 65-59 years | 7501 (12.3%) | 5761 (17.1%) |
| 70–74 years | 3681 (6.0%) | 5794 (17.2%) |
| 75–79 years | 1452 (2.4%) | 5091 (15.1%) |
| 80–84 years | 566 (0.9%) | 3589 (10.7%) |
| 85 years and over | 336 (0.6%) | 2505 (7.5%) |
| Sex | ||
| Male | 25,007 (40.4%) | 17,919 (52.3%) |
| Female | 36,876 (59.6%) | 16,369 (47.7%) |
| Race/ethnicity | ||
| Non-Hispanic White | 53,799 (88.4%) | 29,503 (87.8%) |
| Non-Hispanic Black | 4996 (8.2%) | 3370 (10.0%) |
| Non-Hispanic Other | 882 (1.4%) | 336 (1.0%) |
| Hispanic | 1169 (1.9%) | 403 (1.2%) |
| Census region | ||
| Midwest | 17,416 (28.6%) | 9881 (29.4%) |
| Northeast | 12,091 (19.9%) | 6504 (19.4%) |
| South | 17,678 (29.1%) | 10,498 (31.2%) |
| West | 13,661 (22.5%) | 6729 (20.0%) |
Next, we used Equation (1) to estimate the random effects of state of residence and state of birth on old age mortality, adjusted for sex, race/ethnicity and age. The results of the multi-level logistic regression models are shown in Table 2. Diagnostic statistics suggest that model 3 (which includes both state of residence and state of birth random effects) performs best. The variance of state of birth (0.03) was slightly larger that of state of residence (0.02), meaning that a larger proportion of the variance in old age mortality risk can be explained by state of birth random effects compared to state of residence random effects.
Table 2.
Results of multilevel logistic regression models.
| Model 1 | Model 2 | Model 3 | |
|---|---|---|---|
| Fixed effects | |||
| Age | 3.69*** (3.69, 3.70) | 3.68*** (3.68, 3.69) | 3.69*** (3.68, 3.69) |
| Sex (ref: Male) | |||
| Female | 0.44*** (0.44, 0.44) | 0.44*** (0.44, 0.44) | 0.44*** (0.44, 0.44) |
| Race/ethnicity (ref: Non-Hispanic White) | |||
| Non-Hispanic Black | 1.33 *** (1.33, 1.33) | 1.29*** (1.29, 1.30) | 1.26*** (1.25, 1.27) |
| Non-Hispanic Other | 0.97*** (0.96, 0.98) | 0.99 (0.97, 1.00) | 1.00 (0.99, 1.02) |
| Hispanic | 0.90*** (0.89, 0.91) | 0.97*** (0.96, 0.98) | 0.96*** (0.95, 0.97) |
| (Intercept) | 0.71*** (0.69, 0.74) | 0.71*** (0.68, 0.74) | 0.71*** (0.67, 0.75) |
| Random effects | |||
| State of residence () | 0.02 | 0.02 | |
| State of birth () | 0.03 | 0.03 | |
| Log Likelihood | −10,925,315 | −10,919,682 | −10,910,142 |
| Akaike Inf. Crit. | 21,850,644 | 21,839,379 | 21,820,299 |
| Bayesian Inf. Crit. | 21,850,710 | 21,839,445 | 21,820,375 |
Note: *p < 0.5; **p < 0.01; ***p < 0.001. Fixed effects are presented in odds ratios.
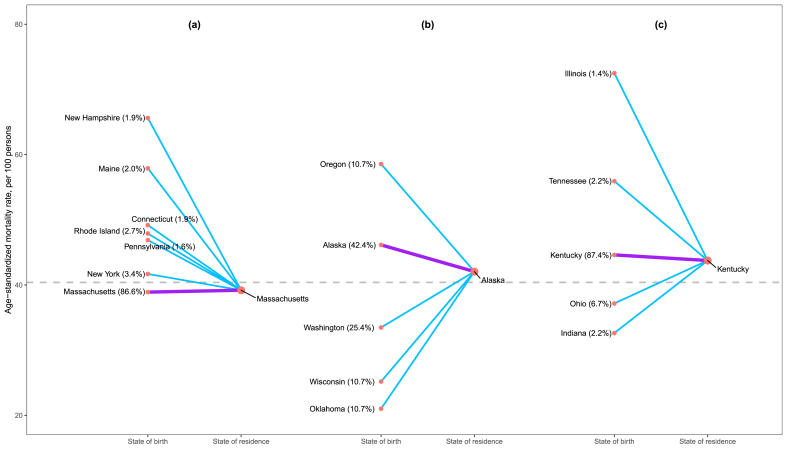
Fig. 1 shows three examples of our decomposition of the contribution of “movers” and “stayers” to variation in state of residence-based mortality rate estimates. The remaining figures are shown in Appendix A. These figures demonstrate the extent to which typically calculated measures of geographic disparities in mortality are actually complex groupings of mortality rates of “stayers” and mortality rates of a diverse set of “movers”. In addition, we created a figure (see Appendix B) showing similar decompositions for state of birth-based mortality rates. The latter figure highlights variation in mortality experiences among those who emigrate from each state, while the former figure displays the varied mortality experiences of migrants from different origins in each destination.
Fig. 1.
Decomposition of state of residence-based mortality rate by state of birth. The figure plots age-standardized mortality rates based on three groups of respondents' state of residence (Alaska, Massachusetts, and Kentucky) and then links these estimated rates with their contributing sources based on respondents' state of birth. The purple lines link “stayers” (those with state of birth = state of residence). The blue lines link “movers” from other states of birth with at least 20 respondents in our sample. The proportions of “movers” (by state of birth) and “stayer” within each state of residence are noted. (For interpretation of the references to colour in this figure legend, the reader is referred to the Web version of this article.)
In the case of Massachusetts (Fig. 1a), standard measures of mortality by place of residence appear to be driven upwards by the higher mortality risk of those who moved to Massachusetts from other East Coast states. Massachusetts residents who were born in the state enjoy a lower mortality risk than those who emigrated to it, suggesting that movers were either less healthy on average than those born in Massachusetts, or that the experience of moving to Massachusetts was somehow deleterious for their longevity. In contrast, the standard death rates for those residing in Alaska (Fig. 1b) and Kentucky (Fig. 1c) are driven down by the lower mortality of several groups of movers. The movers’ longevity displays considerable heterogeneity. For example, relative to those native to Kentucky, those who came to Kentucky from Ohio or Indiana experienced lower mortality while those who moved to Kentucky from Illinois or Tennessee saw considerably higher mortality risks. As shown in Appendix A for the 50 states and the District of Columbia, all but Louisiana have state of birth death rates higher than their state of residence death rates. 37 states and the District of Columbia have state of birth death rates lower than their state of residence death rates; for each of the other 12 states, the state of birth death rates are all higher than their state of residence death rates. Appendix B reveals the heterogeneity in death rates among those born in each state depending on their residence at the time of death. For some states (including Arizona, Hawaii, Georgia, Montana, New Hampshire, Rhode Island, Vermont, and Wyoming), people who were born in those states but migrated to a different state all have higher death rates than those who stayed.
4. Discussion
Recent research on contextual factors (i.e. social and policy environment) has made important contributions towards explaining geographic disparities in adult mortality. However, contemporaneously measured place-based exposures do not accurately capture the far-reaching effects of early life place exposures on later life mortality. Our findings in this Short Communication study are noteworthy in several ways. First, including state of birth measures is consequential for our understanding of geographic disparities in adult mortality. The regression diagnostics show that the model incorporating the random effects of both state of birth and state of residence better predicts mortality risk than does the model with the random effects of state of residence only. Analysis of variance (ANOVA) testing results also reveal that improvement in model fit is significant when state of birth measures are included.
Second, we compare the relative significance of state of birth and state of residence in predicting individual mortality risk. The intra-class correlation coefficient (ICC), which is the fraction of the total variation in the data that is accounted for by between-group (in our case, between-state of birth and between-state of residence) variation (Gelman & Hill, 2007), is used as the measure. The ICC, after accounting for age, sex and race/ethnicity, is 0.9% for state of birth level and 0.6% for state of residence level, albeit both effects are small. ICC can also be interpreted as the correlation among observations within the same group. The mortality risk of individuals within the same state of birth, no matter what their states of residence are, is more similar than individuals within the same state of residence. Although the difference between state of birth and state of residence random effects is small, our results point to the fact that state of birth is as a meaningful predictor of adult mortality risk as state of residence.
Third, we display decompositions of state of residence-based measures of geographic disparities in adult mortality based on “mover” and “stayer” status of the populations. One of the challenges in demographic research is knowing the composition and vital statistics of various strands within mobile populations and weighing their importance in place-based measures of mortality (Kasakoff & Adams, 2000). Here, we show that standard estimates of each state's mortality rate are influenced to varying extents by individuals who moved between states whose populations experience diverse mortality conditions (see Appendix A). Our findings also highlight heterogeneity across migration paths, with some migrants moving to relatively better health environments and others experiencing higher mortality risks in their destinations. While emigrants from certain states enjoy a mortality advantage consistent with ideas about migrant selection or moving to opportunity, those born in states such as Connecticut, Georgia, Vermont, and Wyoming who later moved to another state experienced higher mortality than those who chose to stay put (see Appendix B). The decomposition of state of birth- and state of residence-based mortality rates points to the complexity in the lives of migrants and underscores the need to understand adult mortality from life course perspectives.
Our study has some limitations. First, our data lack the information on the timing of inter-state migration among “movers.” The effects of state of birth on subsequent mortality may be more or less pronounced depending on the duration of the initial exposure and the age at migration. Similarly, the effects of state of residence on adult mortality may be more pronounced for those “movers” who migrated earlier in life and therefore spent more time in their final destination. There is evidence that people who moved across states are more likely to have made such location decision earlier in their lives (Molloy et al., 2011), but more remains to be learned. A related issue is that although we know about our study participants’ location at birth and at the time of interview, we do not know about the number, timing, or destination of other moves that might have taken place in the interim. The lack of a complete migration history between birth and time of interview inhibits our understanding of how migration processes may determine the duration of place-based exposures and consequently affect mortality risk. Furthermore, our geographic unit of analysis is state, which is the only geography at which places of birth and residence are measured in our data. Within-state heterogeneity in early life social and policy environments relevant to older age mortality may be equally important in explaining disparities in state of residence-based mortality rates.
Despite these limitations, our study is one of the first to directly link both state of birth and state of residence to adult mortality. Our results point to the importance of early life place-based exposures, in addition to contemporaneous exposures, in explaining geographic disparities in later life mortality. Future work, with larger sample sizes, should continue to decompose geographic disparities in mortality rates by sex, race/ethnicity, and cohort as well as uncover mechanisms linking state of birth to later life mortality outcomes.
Author Statement
Wei Xu: Conceptualization, Methodology, Software, Investigation, Writing- Original draft preparation. Michal Engelman: Conceptualization, Writing- Original draft preparation, Writing- Reviewing and Editing, Funding acquisition. Alberto Palloni: Writing- Reviewing and Editing, Funding acquisition. Jason Fletcher: Conceptualization, Writing- Reviewing and Editing, Funding acquisition.
Declaration of competing interest
None.
Acknowledgement
This research was supported by the NIA (R01AG060109). The authors gratefully acknowledge use of the facilities of the Center for Demography of Health and Aging at the University of Wisconsin-Madison, funded by NIA Center Grant P30 AG017266. This paper uses data obtained from the public-use file of the National Longitudinal Mortality Study. The file is provided to persons interested in research by the U.S. Census Bureau. The views expressed in this paper are those of the authors and do not necessarily reflect the views of the National Longitudinal Mortality Study, the Bureau of the Census, or the project sponsors: the National Heart, Lung, and Blood Institute, the National Cancer Institute, the National Institute on Aging, and the National Center for Health Statistics.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.ssmph.2020.100680.
Appendix A. Supplementary data
The following are the Supplementary data to this article:
References
- Backlund E., Rowe G., Lynch J., Wolfson M.C., Kaplan G.A., Sorlie P.D. Income inequality and mortality: A multilevel prospective study of 521 248 individuals in 50 US states. International Journal of Epidemiology. 2007;36(3):590–596. doi: 10.1093/ije/dym012. [DOI] [PubMed] [Google Scholar]
- Bastian J., Michelmore K. The long-term impact of the earned income tax credit on children's education and employment outcomes. Journal of Labor Economics. 2018;36(4):1127–1163. doi: 10.1086/697477. [DOI] [Google Scholar]
- Baughman R.A., Duchovny N. State earned income tax credits and the production of child health: Insurance coverage, utilization, and health status. National Tax Journal. 2016;69(1):103–131. doi: 10.17310/ntj.2016.1.04. [DOI] [Google Scholar]
- Ben-Shlomo Y., Kuh D. A life course approach to chronic disease epidemiology: Conceptual models, empirical challenges and interdisciplinary perspectives. International Journal of Epidemiology. 2002;31(2):285–293. doi: 10.1093/ije/31.2.285. [DOI] [PubMed] [Google Scholar]
- Brown C.C., Moore J.E., Felix H.C., Stewart M.K., Bird T. Mac, Lowery C.L. Association of state medicaid expansion status with low birth weight and preterm birth. Journal of the American Medical Association. 2019;321(16):1598. doi: 10.1001/jama.2019.3678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Curb J.D., Ford C.E., Pressel S., Palmier M., Babcock C., Hawkins M. Ascertainment of vital status through the national death index and the social security administration. American Journal of Epidemiology. 1985;121(5):754–766. doi: 10.1093/aje/121.5.754. [DOI] [PubMed] [Google Scholar]
- Dahl G.B., Lochner L. The impact of family income on child achievement: Evidence from the earned income tax credit. The American Economic Review. 2012;102(5):1927–1956. doi: 10.1257/aer.102.5.1927. [DOI] [Google Scholar]
- Duncan G.J., Ziol-Guest K.M., Kalil A. Early-childhood poverty and adult attainment, behavior, and health. Child Development. 2010;81(1):306–325. doi: 10.1111/j.1467-8624.2009.01396.x. [DOI] [PubMed] [Google Scholar]
- Feijten P., Hooimeijer P., Mulder C.H. Residential experience and residential environment choice over the life-course. Urban Studies. 2008;45(1):141–162. doi: 10.1177/0042098007085105. [DOI] [Google Scholar]
- Gelman A., Hill J. 2007. Data analysis using regression and multilevel/hierarchical models. [Google Scholar]
- Gustafsson P.E., Hammarström A., San Sebastian M. Cumulative contextual and individual disadvantages over the life course and adult functional somatic symptoms in Sweden. The European Journal of Public Health. 2015;25(4):592–597. doi: 10.1093/eurpub/cku213. [DOI] [PubMed] [Google Scholar]
- Hyatt H., McEntarfer E., Ueda K., Zhang A. Interstate migration and employer-to-employer transitions in the United States: New evidence from administrative records data. Demography. 2018;55(6):2161–2180. doi: 10.1007/s13524-018-0720-5. [DOI] [PubMed] [Google Scholar]
- Kaplan G., Schulhofer-Wohl S. Understanding the long-run decline in interstate migration. International Economic Review. 2017;58(1):57–94. doi: 10.1111/iere.12209. [DOI] [Google Scholar]
- Kasakoff A.B., Adams J.W. The effects of migration, place, and occupation on adult mortality in the American North, 1740-1880. Historical Methods. 2000;33(2):115–130. doi: 10.1080/01615440009598954. [DOI] [PubMed] [Google Scholar]
- Komro K.A., Livingston M.D., Markowitz S., Wagenaar A.C. The effect of an increased minimum wage on infant mortality and birth weight. American Journal of Public Health. 2016;106(8):1514–1516. doi: 10.2105/AJPH.2016.303268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Komro K.A., Markowitz S., Livingston M.D., Wagenaar A.C. Effects of state-level earned income tax credit laws on birth outcomes by race and ethnicity. Health Equity. 2019;3(1):61–67. doi: 10.1089/heq.2018.0061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuh D., Ben-Shlomo Y. Oxford University Press; 2004. A life course approach to chronic Disease epidemiology. [DOI] [PubMed] [Google Scholar]
- Makuc M., McMillen M., Feinleib M., McMillen M., Schwartz S., Rogot E. Proceedings of the section on social statistics. American Statistical Association; 1984. An overview of the US national longitudinal mortality study. [Google Scholar]
- Molloy R., Smith C.L., Wozniak A. Internal migration in the United States. The Journal of Economic Perspectives. 2011;25(3):173–196. doi: 10.1257/jep.25.3.173. [DOI] [Google Scholar]
- Montez J.K., Hayward M.D. Vol. 2. 2011. Early life conditions and later life mortality; pp. 187–206. (International handbook of adult mortality). [DOI] [Google Scholar]
- Montez J.K., Hayward M.D., Wolf D.A. Do U.S. states' socioeconomic and policy contexts shape adult disability? Social Science & Medicine. 2017;178:115–126. doi: 10.1016/j.socscimed.2017.02.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Montez J.K., Hayward M.D., Zajacova A. Educational disparities in adult health: U.S. States as institutional actors on the association. Socius: Sociological Research for a Dynamic World. 2019;5 doi: 10.1177/2378023119835345. 237802311983534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Montez J.K., Zajacova A., Hayward M.D. Explaining inequalities in women's mortality between U.S. States. SSM - Population Health. 2016;2:561–571. doi: 10.1016/j.ssmph.2016.07.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- R Core Team . 2020. R: A language and environment for statistical computing.https://www.r-project.org Vienna, Austria. Retrieved from. [Google Scholar]
- Shi L., Macinko J., Starfield B., Xu J., Regan J., Politzer R. Primary care, infant mortality, and low birth weight in the states of the USA. Journal of Epidemiology & Community Health. 2004;58(5):374–380. doi: 10.1136/jech.2003.013078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Strully K.W., Rehkopf D.H., Xuan Z. Effects of prenatal poverty on infant health: State earned income tax credits and birth weight. American Sociological Review. 2010;75(4):534–562. doi: 10.1177/0003122410374086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Subramanian S.V., Kawachi I., Kennedy B.P. Does the state you live in make a difference? Multilevel analysis of self-rated health in the US. Social Science & Medicine. 2001;53(1):9–19. doi: 10.1016/S0277-9536(00)00309-9. [DOI] [PubMed] [Google Scholar]
- Us Census Bureau Lifetime mobility in the United States: 2010. American Community Survey Briefs. 2011;(10–07):1–4. [Google Scholar]
- Wilmoth J.R., Boe C., Barbieri M. International differences in mortality at older ages: Dimensions and sources. 2010. Geographic differences in life expectancy at age 50 in the United States compared with other high-income countries. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.