Abstract
Background:
Meniscus root tears are increasingly being recognized. Meniscal extrusion has previously been associated with medial root tears; however, the relationship between secondary meniscal restraints, such as the meniscotibial (MT) ligament, extrusion, and root tears has yet to be formally evaluated.
Purpose:
To better understand the association between MT ligament competence, medial meniscal extrusion, and medial meniscus posterior root tears (MMPRTs) as well as to determine the progression of meniscal extrusion over time.
Study Design:
Case series; Level of evidence, 4.
Methods:
Serial magnetic resonance imaging (MRI) scans were reviewed for patients who showed evidence of medial meniscal extrusion and MMPRTs on at least 1 of ≥2 available MRI scans. All patients were symptomatic at the time of diagnosis. All MRI scans were analyzed independently by 2 board-certified musculoskeletal radiologists. MT ligament disruption, medial meniscal extrusion, and MMPRTs were recorded for each MRI scan. The time between MRI scans, presence of insufficiency fractures, and Outerbridge classification for the medial femur and tibia were also evaluated.
Results:
Overall, 27 knees in 26 patients were included in this study, with a total of 63 MRI scans analyzed (21 knees with 2 MRI scans, 3 with 3 MRI scans, and 3 with 4 MRI scans). All patients demonstrated clear medial meniscal extrusion and MT ligament disruption before the subsequent development of MMPRTs (P < .001). Mean extrusion at the time of initial MRI was 3.3 ± 1.1 mm and increased significantly to 5.5 ± 1.8 mm at the time of first imaging with an identified MMPRT (P < .001). The mean time between initial MRI and the first identification of an MMPRT on later MRI was 1.7 ± 1.6 years.
Conclusion:
In a sample of 27 symptomatic knees with serial MRI scans both before and after an MMPRT diagnosis, all patients demonstrated MT ligament disruption and associated meniscal extrusion before the development of subsequent medial meniscus root tears. These findings suggest that MT ligament disruption and medial meniscal extrusion represent early and predisposing events contributing to MMPRTs. Therefore, this provides a possible explanation of why meniscal extrusion is not corrected with medial meniscus root repair.
Keywords: medial meniscal extrusion, meniscotibial ligament, medial meniscus posterior root tear, MMPRT, extrusion
Meniscal tears are common, accounting for 1 in 7 clinical cases involving the knee, with an estimated prevalence of 60 to 70 per 100,000 persons.24–26 Meniscus posterior root tears, first described by Pagnani et al31 in 1991, are defined as bony avulsions or as complete radial tears within 1 cm of the meniscal attachments. Root tears result in the loss of resistance to hoop stresses in a manner functionally equivalent to complete meniscectomy.1,15,19,34 The profound increase in tibiofemoral contact pressures, reduced knee stability, and alterations in knee kinematics have piqued interest in meniscus root tears, especially as their role in rapid articular cartilage degeneration and arthritis progression is increasingly recognized.8,15,34
The meniscotibial (MT) ligament plays an important role in the stabilization and centralization of the medial meniscus.14,32 The MT ligament originates on the posteromedial aspect of the proximal tibia and is anchored to the inferior aspect of the posterior horn of the meniscus.6,20,21,32 The medial meniscus is less mobile than the lateral meniscus, and injuries to supporting structures such as the MT ligament can worsen meniscal instability and incompetence in the setting of an already destabilized posterior medial meniscal horn.6,7,32 Meniscal extrusion, defined as meniscal displacement beyond the tibial plateau margins on magnetic resonance imaging (MRI), is widely accepted as an indicator for a meniscal injury.4,14,16 Extrusion is associated with posterior meniscus root tears and the subsequent development of osteoarthritis.3,10,14,16 Previous publications have hypothesized that medial meniscus posterior root tears (MMPRTs) may be the underlying cause for extrusion3,9; however, there is increased recognition that meniscal extrusion can occur in the absence of a meniscal tear.14 In addition, there is increasing recognition that meniscus root repair alone is not always able to completely correct extrusion.3,5 These findings suggest that extrusion may be caused by additional factors other than the meniscus root attachment.
To date, there remains a paucity of data evaluating whether meniscal extrusion precedes and contributes to the development of root tears or whether root tears are the reason for subsequent meniscal extrusion. The purpose of this study was to better understand the association between MT ligament competence, medial meniscal extrusion, and MMPRTs as well as to determine the progression of meniscal extrusion over time. We hypothesized that damage to the MT ligament results in progressive meniscal extrusion and eventual MMPRTs.
Methods
This study was conducted after institutional review board approval. A comprehensive institutional radiology database was queried to search finalized radiology reports for “extrusion,” “root,” and “root tear” between 2010 and 2020 using an established technique, as described previously by Krych et al.16 Patients were included if they had at least 2 MRI scans of the same knee, with at least 1 MRI scan showing evidence of an MMPRT and medial meniscal extrusion. It is important to note that the timing of extrusion and its relationship to the presence of root tears upon database query were not evaluated for inclusion. Namely, patients were included if they had these findings present at any time during the imaging evaluation, regardless of chronological order. Patients were excluded if they had a concomitant tibial plateau fracture on initial MRI, prior ligament injury or meniscal surgery, or surgical intervention between the evaluated imaging time points. Of note, all medial menisci included were otherwise intact without evidence of a prior significant injury at the time of inclusion, and no patient developed new ligament tears during the course of follow-up. All patients were clinically symptomatic, consistent with medial meniscal injuries, and this was confirmed by a review of their medical chart.
Overall, 27 knees in 26 patients were included in this study, with a total of 63 MRI scans analyzed (21 knees had 2 MRI scans, 3 knees had 3 MRI scans, and 3 knees had 4 MRI scans). All MRI scans were obtained using our institution’s standard knee protocol on 1.5- or 3-T scanners, with protocols and sequencing that have varied little over the course of the past 10 years. Demographic information was collected for each patient (Table 1). Each MRI scan was analyzed independently by 2 board-certified musculoskeletal radiologists (N.G.R. and A.C.J.). The time between MRI scans was calculated, and the presence and respective amount of medial meniscal extrusion were recorded.
Table 1.
Patient Demographics and Medial Meniscus Posterior Root Tear Types (n = 26 Patients, 27 Knees)a
| Value | |
|---|---|
| Sex, n (%) | |
| Female | 20 (77) |
| Male | 6 (23) |
| Laterality, n (%) | |
| Right | 18 (67) |
| Left | 9 (33) |
| Age at initial MRI, y | 55.7 ± 9.9 |
| Outerbridge grade on initial MRI | |
| Medial tibial plateau | 1.6 ± 1.2 |
| Medial femoral condyle | 2.4 ± 1.2 |
| Body mass index, kg/m2 | 33.0 ± 8.2 |
| Time between first and last MRI, y | 2.0 ± 2.0 |
| No. of MRI scans, n | |
| 2 | 21 |
| 3 | 3 |
| 4 | 3 |
| LaPrade classification, n | |
| Type 1 | 3 |
| Type 2 | 16 |
| Type 2A | 7 |
| Type 2B | 2 |
| Type 2C | 7 |
| Type 3 | 0 |
| Type 4 | 8 |
| Type 5 | 0 |
aData are shown as mean ± SD unless otherwise indicated. MRI, magnetic resonance imaging.
Previous studies have defined a threshold of meniscal extrusion as a >3-mm displacement of the medial meniscus beyond the medial tibial plateau, not including osteophytes.11,16,34 Extrusion was measured at the level of the midbody of the meniscus and was classified using the minor (≤3 mm) and major (>3 mm) extrusion classifications as proposed by Costa et al.4 MMPRTs were categorized according to the LaPrade classification.19 The status of the coronary/MT ligament15 and the modified articular cartilage Outerbridge grades were recorded: grade 0 = normal; grade 1 = cartilage softening or swelling; grade 2 = cartilage fragmentation, fissuring, or fibrillation extending <50% of the articular thickness; grade 3 = cartilage fragmentation, fissuring, or fibrillation extending >50% of the articular thickness with no subchondral bone exposure; and grade 4 = complete articular cartilage degeneration with exposure of subchondral bone.16,22
The MT ligament was considered to be abnormal on MRI when there was a consensus that the ligament was poorly defined, attenuated, indistinct, or absent.14 The MT ligament was evaluated at 2 points, the posteromedial corner and anteriorly, with the posteromedial corner being the site of the most frequent abnormalities. Because of the diminutive size of the MT ligament and its obliquity with respect to our prescribed imaging planes, a single image with an abnormal appearance was considered abnormal, provided that the adjacent images were not completely normal.
The presence of subchondral cysts, edema, collapse, or insufficiency fractures was also recorded for both the medial femoral condyle (MFC) and medial tibial plateau. Subchondral cysts were described as having sharply demarcated margins with an increased signal in subchondral bone on T2-weighted imaging.16,33,35 Subchondral edema was identified as a poorly defined area of a decreased signal in the underlying bone marrow on T1-weighted imaging and an increased signal on T2-weighted imaging.2,16 Subchondral insufficiency fractures were defined by a low-intensity signal on T1-weighted imaging beneath the articular weightbearing surfaces of the tibiofemoral compartment and a subchondral fracture line.33
Statistical Analysis
Demographics were presented using means and standard deviations as well as percentages, as appropriate. Proportions were evaluated using the Fisher exact test, and the progression of tears over time was evaluated using a paired Student t test. All statistical tests were 2-sided. P values <.05 were considered statistically significant. Analyses were conducted in R 3.4.3 (R Core Team).
Results
Initially, 40 knees and 79 MRI scans were identified with serial MRI of the same knee. Of these knees, 13 were excluded, as initial MRI demonstrated an MMPRT. Therefore, a total of 27 medial meniscus posterior root tears in 26 patients (20 female, 6 male) met the study inclusion criteria. All 26 patients were found to have a preceding MRI scan that showed an intact MMPRT. The mean age at the time of initial MRI before the MMPRT was 55.7 ± 9.9 years (median, 54 years [range, 38-78 years]). Patients were evaluated for a mean of 2.0 ± 2.0 years (median, 1.2 years [range, 0.2-6.4 years]) after their initial date of pre-MMPRT imaging, with patients having a median of 2 MRI scans (range, 2-4) over the course of follow-up. All patients progressed to an MMPRT on MRI during the course of the study.
Patients underwent their first MRI demonstrating a definitive MMPRT at a mean of 1.7 ± 1.6 years (median, 1.1 years [range, 0.1-6.4 years]) after their initial imaging without a root tear. Meniscal extrusion increased significantly from a mean of 3.3 ± 1.1 mm (median, 3.0 mm [range, 1.0-5.0 mm]) before the root tear diagnosis to 5.5 ± 1.8 mm (median, 5.0 mm [range, 2.0-9.0 mm]) (P < .001) at the time of the root tear diagnosis. All patients demonstrated MRI evidence of MT ligament disruption (P < .001) and visible meniscal extrusion (P < .001) on MRI before the first noted presence of an MMPRT.
Mean meniscal extrusion measured 5.8 ± 1.9 mm (median, 6.0 mm [range, 2.0-10.0 mm]) at the time of final imaging. Meniscal extrusion progressed in 26 of the 27 knees (96.3%). The mean modified Outerbridge grade progressed from 2.4 ± 1.2 (median, 3 [range, 0-4]) to 3.5 ± 0.8 (median, 4 [range, 2-4]) (P < .01) in the MFC and from 1.6 ± 1.2 (median, 2 [range, 0-4]) to 3.0 ± 1.2 (median, 3 [range, 0-4]) (P = .02) in the medial tibial plateau. Extrusion was found to be mildly correlated with the MFC Outerbridge grade (Spearman ρ = 0.23; P = .07) and moderately correlated with the tibial Outerbridge grade (ρ = 0.62; P < .001). Similarly, there was a moderate correlation with the presence of an MMPRT and associated MFC (ρ = 0.45; P < .001) and tibial (ρ = 0.50; P < .001) Outerbridge grades. There was 1 patient who developed a subchondral insufficiency fracture. The clinical follow-up identified 9 knees (33.3%) that went on to arthroplasty (2 unicompartmental knee arthroplasty, 7 total knee arthroplasty) at a mean of 2.6 ± 2.5 years after initial MRI.
Discussion
There is a paucity of literature examining the temporal relationship between MT ligament disruption, meniscal extrusion, and meniscus root tears. It has yet to be determined if extrusion occurs as a result of meniscus root tears or if root tears are the final result of damage to secondary meniscal restraints and associated extrusion. The purpose of this study was to better understand the association between MT ligament competence, medial meniscal extrusion, and MMPRTs, as well as to determine the progression of meniscal extrusion over time. The main finding of this study was that MT ligament disruption and associated meniscal extrusion predated MMPRTs in all 27 knees investigated, supporting the hypothesis that extrusion and MT ligament abnormalities may increase stresses at the medial meniscus posterior horn root attachment, leading to MMPRTs.
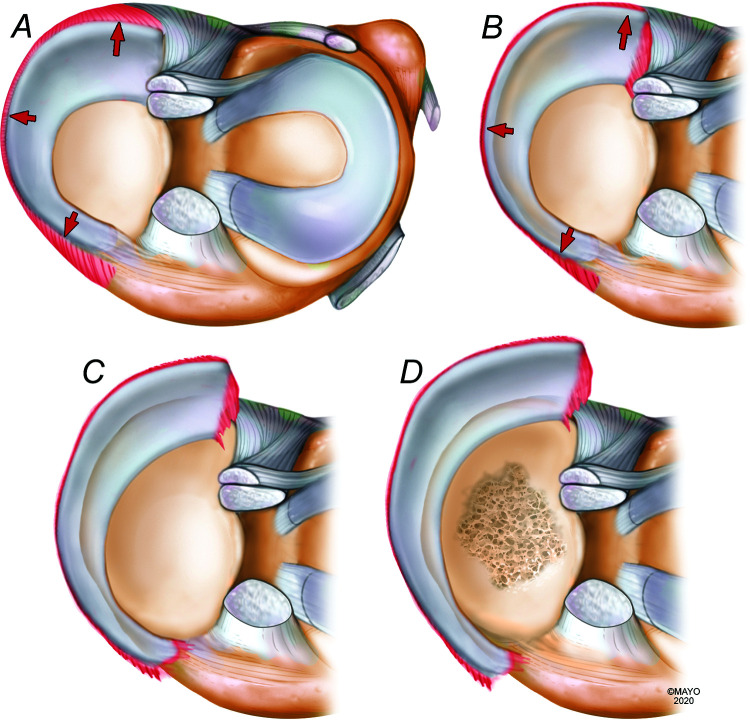
The current literature suggests that medial meniscal extrusion may occur as a result of an MMPRT.3,9 However, the exact chronological and temporal relationship between extrusion, secondary restraints, and root tears has yet to be established. The current study suggests that medial meniscal extrusion consistently precedes and may potentially predispose to a subsequent MMPRT during a series of progressive pathological steps. Given the consistent chronological order on MRI, we propose that MT ligament stress and attenuation (Figure 1A) lead to a progressive loss of MT ligament competence, subsequently causing early meniscal extrusion (Figure 1B). As secondary restraints such as the MT ligament are lost, forces are increasingly concentrated at the meniscus root, leading to MMPRTs and further extrusion (Figure 1C). Rapid progressive articular cartilage degeneration ensues as a result of the posterior horn root tear and loss of meniscal function (Figure 1D). Of note, our study demonstrated a temporal correlation but did not prove cause and effect. Additionally, meniscus root tears have been noted to be associated with ligament (ie, anterior cruciate ligament) tears in young patients; however, the role of MT ligament injuries in this acute traumatic population has yet to be determined.27
Figure 1.
Illustration of the proposed progression of meniscal extrusion to a medial meniscus posterior root tear (MMPRT). (A) Meniscotibial (MT) ligament stress and attenuation. (B) Progressive loss of MT ligament function, increased root stress, and early meniscal extrusion. (C) MMPRT and associated increasing extrusion. (D) Rapid articular degeneration in the setting of an incompetent extruded meniscus.
A recent study by Krych et al14 investigated the presence of isolated meniscal extrusion and documented high rates of associated MT ligament abnormalities (65%), supporting the above proposed mechanism outlining that MT ligament stress predisposes to early meniscal extrusion and subsequent root tears. Medial meniscal extrusion is complex, but there is a relative consensus in the literature that once present, extrusion tends to progress rapidly. This study found that extrusion progressed in 96.3% of the knees analyzed and that mean extrusion increased significantly from 3.3 ± 1.1 to 5.5 ± 1.8 mm over a mean follow-up period of 1.7 ± 1.6 years. A previous study of 33 patients with MMPRTs and medial meniscal extrusion demonstrated increased extrusion from 3.4 to 4.5 mm during a mean interval of only 48 days.28 Another study analyzed the MRI scans of patients with confirmed MMPRTs and medial meniscal extrusion and found a positive correlation between the amount of medial meniscal extrusion and the time from initial injury, further highlighting the progressive nature of extrusion and associated abnormalities; however, this study was limited by a lack of serial MRI scans.9 An additional note of interest is the relative preponderance of female patients (76.9%) in our study. This is consistent with previous literature on MMPRTs and is likely multifactorial in cause.17,23 Previously, it has been suggested that once an MMPRT occurs, female patients may be particularly susceptible to increased symptomatic subchondral loading, given their lower bone mineral density at the proximal tibia.17 Further studies using a prospective design will be needed; however, this study is the first, to our knowledge, that analyzes a longer term progression of serial MRI by 2 board-certified musculoskeletal radiologists.
All 27 knees in our cohort demonstrated early signs of MT ligament disruption during the temporal course, leading to MMPRTs. This is relevant, given that recent studies have shown that nonanatomic meniscus root repair alone does not fully correct medial meniscal extrusion.3,5 These findings suggest that other restraints such as the MT ligament may play an important role in preventing initial extrusion and may need to be addressed at the time of meniscus root repair. The relevance of residual extrusion after root repair is well established, with multiple studies demonstrating that increased extrusion is associated with inferior outcomes after repair and an increased risk of arthritis.3,5,10,18 The biomechanical ability of the meniscus to function normally by resisting hoop stresses and protecting the cartilage will not be achieved if extrusion is not corrected. Furthermore, of the 13 cases excluded because of the presence of an MMPRT on initial MRI, 12 had MT ligament abnormalities with a mean associated initial extrusion of 2.4 ± 1.2 mm. Of note, the single patient with an isolated MMPRT and an intact MT ligament demonstrated only 1.0 mm of extrusion, suggesting that MT ligament disruption generally precedes MMPRTs (present in 39 of the 40 knees initially evaluated), but if it remains intact, the MT ligament may keep the meniscus reduced with minimal extrusion, given its role as a secondary restraint.
Technical efforts to address residual extrusion after root repair are evolving. Koga et al12,13 described a technique in which the midbody is centralized and stabilized onto the rim of the tibial plateau to reduce the meniscus and prevent extrusion. Results of early reports have been generally positive, suggesting that centralization may better restore native biomechanics and protect articular cartilage compared with root repair alone.5,12,29,30 Our findings that MT ligament disruption occurred before an MMPRT also suggest that MT ligament repair or functional reconstruction through centralization or other procedures may be a useful augment to MMPRTs (Figures 1 and 2). Furthermore, MT ligament repair may be a viable early intervention before the progression to an MMPRT, but further investigation with clinical trials is required to document efficacy.
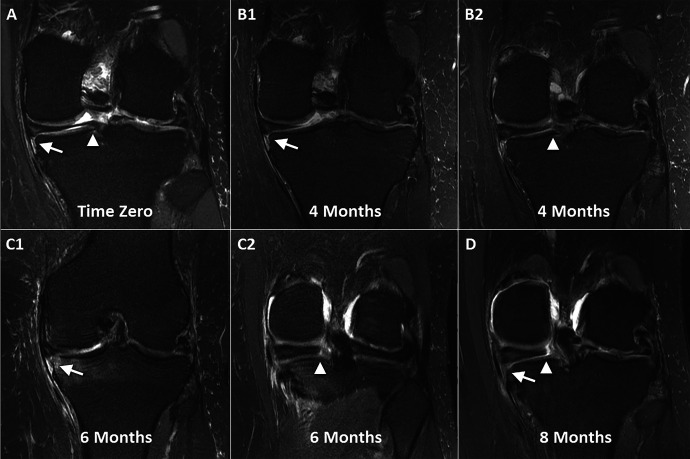
Figure 2.
Serial magnetic resonance imaging showing the progression of a meniscotibial (MT) ligament tear, medial meniscal extrusion, and eventual medial meniscus posterior root tear. (A) Initial T2-weighted coronal imaging demonstrates bright MT ligament edema (arrow) while the root remains intact (arrowhead). There is a degenerative signal in the meniscus with irregularity and trace extrusion. (B1) Repeat imaging at 4 months demonstrates a further increase in the signal and MT ligament attenuation (arrow), increased extrusion, and (B2) new partial tearing and an increased signal in the meniscus root (arrowhead). (C1) Imaging at 6 months from baseline demonstrates marked attenuation of the MT ligament (arrow), substantial extrusion, the progression of femoral chondromalacia, and (C2) a concurrent full-thickness radial root tear (arrowhead). (D) At 8 months, there is radiographic loss of the MT ligament (arrow) and clearly visible complete tearing and displacement of the meniscus root (arrowhead).
This study is not without important limitations. The retrospective design is prone to inherent biases, including reliance on complete and accurate recordkeeping. MRI scans were not taken at regular intervals but rather were obtained according to the discretion of the treating physician. Patients were only included if they had multiple MRI scans, which may have selected for patients who were more symptomatic and more likely to have a quicker progression of extrusion. It is unknown in these knees whether extrusion and MT ligament abnormalities could have been present sooner, predating clinical symptoms; furthermore, patients who had isolated MT ligament disruption or who had MMPRTs but never developed extrusion during the course of 2 to 4 MRI scans would not have been included in this analysis. Given the retrospective and exploratory study design aimed to investigate the temporal nature of extrusion and root tears, this study strongly supports, but does not definitively prove, the chronological order of root tears and extrusion. Exceptions may occur, and formal prospective series with imaging over multiple and predetermined time points are necessary to further investigate the temporal phenomena observed. Finally, the sample size of this study was relatively small, given the low number of patients with serial MRI scans who did not have associated ligamentous injuries. MRI analysis could have also missed the diagnosis of meniscal extrusion or resulted in unrecognized MMPRTs in some patients, given that these have been established to be difficult to consistently visualize on imaging.18
Conclusion
In a sample of 27 symptomatic knees with serial MRI scans both before and after an MMPRT diagnosis, all patients demonstrated MT ligament disruption and associated meniscal extrusion before the development of subsequent medial meniscus root tears. These findings suggest that MT ligament disruption and medial meniscal extrusion represent early and predisposing events contributing to MMPRTs. Therefore, this provides a possible explanation of why meniscal extrusion is not corrected with medial meniscus root repair.
Footnotes
Final revision submitted May 4, 2020; accepted May 20, 2020.
This article and its contents are solely the responsibility of the authors and do not necessarily represent the official views of the National Institutes of Health.
One or more of the authors has declared the following potential conflict of interest or source of funding: This study was partially funded by a grant from the National Institute of Arthritis and Musculoskeletal and Skin Diseases for the Musculoskeletal Research Training Program (T32AR56950). A.J.K. has received research support from Aesculap/B. Braun, Ceterix Orthopaedics, Exactech, Gemini Medical, and Histogenics; consulting fees from Arthrex, DePuy, JRF Ortho, and Vericel; speaking fees from Arthrex; and royalties from Arthrex; is a board or committee member for the Musculoskeletal Transplant Foundation; and has stock/stock options in Responsive Arthroscopy. M.D.L. has a family member who has received research support from Smith & Nephew; consulting fees from Arthrex, Linvatec, Ossur, and Smith & Nephew; and royalties from Arthrex, Ossur, Smith & Nephew, and Thieme. M.H. has received hospitality payments from DePuy Synthes. C.L.C. has received educational support from Arthrex and hospitality payments from Arthrex and Zimmer Biomet. M.J.S. has received research support from Arthrex and Stryker, consulting fees from Arthrex, and royalties from Arthrex. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval for this study was obtained from the Mayo Clinic (study No. PR15-000601-05).
References
- 1. Allaire R, Muriuki M, Gilbertson L, Harner CD. Biomechanical consequences of a tear of the posterior root of the medial meniscus: similar to total meniscectomy. J Bone Joint Surg Am. 2008;90(9):1922–1931. [DOI] [PubMed] [Google Scholar]
- 2. Choi JY, Chang EY, Cunha GM, et al. Posterior medial meniscus root ligament lesions: MRI classification and associated findings. AJR Am J Roentgenol. 2014;203(6):1286–1292. [DOI] [PubMed] [Google Scholar]
- 3. Chung KS, Ha JK, Ra HJ, Nam GW, Kim JG. Pullout fixation of posterior medial meniscus root tears: correlation between meniscus extrusion and midterm clinical results. Am J Sports Med. 2017;45(1):42–49. [DOI] [PubMed] [Google Scholar]
- 4. Costa CR, Morrison WB, Carrino JA. Medial meniscus extrusion on knee MRI: is extent associated with severity of degeneration or type of tear? AJR Am J Roentgenol. 2004;183:17–23. [DOI] [PubMed] [Google Scholar]
- 5. Daney BT, Aman ZS, Krob JJ, et al. Utilization of transtibial centralization suture best minimizes extrusion and restores tibiofemoral contact mechanics for anatomic medial meniscal root repairs in a cadaveric model. Am J Sports Med. 2019;47(7):1591–1600. [DOI] [PubMed] [Google Scholar]
- 6. DePhillipo NN, Moatshe G, Brady A, et al. Effect of meniscocapsular and meniscotibial lesions in ACL-deficient and ACL-reconstructed knees: a biomechanical study. Am J Sports Med. 2018;46(10):2422–2431. [DOI] [PubMed] [Google Scholar]
- 7. El-Khoury GY, Usta HY, Berger RA. Meniscotibial (coronary) liagament tears. Skeletal Radiol. 1984;11(3):191–196. [DOI] [PubMed] [Google Scholar]
- 8. Faucett SC, Geisler BP, Chahla J, et al. Meniscus root repair vs meniscectomy or nonoperative management to prevent knee osteoarthritis after medial meniscus root tears: clinical and economic effectiveness. Am J Sports Med. 2019;47(3):762–769. [DOI] [PubMed] [Google Scholar]
- 9. Furumatsu T, Kamatsuki Y, Fujii M, et al. Medial meniscus extrusion correlates with disease duration of the sudden symptomatic medial meniscus posterior root tear. Orthop Traumatol Surg Res. 2017;103(8):1179–1182. [DOI] [PubMed] [Google Scholar]
- 10. Kim SJ, Choi CH, Chun YM, et al. Relationship between preoperative extrusion of the medial meniscus and surgical outcomes after partial meniscectomy. Am J Sports Med. 2017;45(8):1864–1871. [DOI] [PubMed] [Google Scholar]
- 11. Koenig JH, Ranawat AS, Umans HR, Difelice GS. Meniscal root tears: diagnosis and treatment. Arthroscopy. 2009;25(9):1025–1032. [DOI] [PubMed] [Google Scholar]
- 12. Koga H, Muneta T, Watanabe T, et al. Two-year outcomes after arthroscopic lateral meniscus centralization. Arthroscopy. 2016;32(10):2000–2008. [DOI] [PubMed] [Google Scholar]
- 13. Koga H, Muneta T, Yagishita K, et al. Arthroscopic centralization of an extruded lateral meniscus. Arthrosc Tech. 2012;1(2):e209–e212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Krych AJ, Bernard CD, Leland DP, et al. Isolated meniscus extrusion associated with meniscotibial ligament abnormality. Knee Surg Sports Traumatol Arthrosc. Published online July 22, 2019. doi: 10.1007/s00167-019-05612-1 [DOI] [PubMed] [Google Scholar]
- 15. Krych AJ, Hevesi M, Leland DP, Stuart MJ. Meniscal root injuries. J Am Acad Orthop Surg. 2020;28(12):491–499. [DOI] [PubMed] [Google Scholar]
- 16. Krych AJ, Johnson NR, Mohan R, et al. Arthritis progression on serial MRIs following diagnosis of medial meniscal posterior horn root tear. J Knee Surg. 2018;31(7):698–704. [DOI] [PubMed] [Google Scholar]
- 17. Krych AJ, Reardon PJ, Johnson NR, et al. Non-operative management of medial meniscus posterior horn root tears is associated with worsening arthritis and poor clinical outcome at 5-year follow-up. Knee Surg Sports Traumatol Arthrosc. 2017;25(2):383–389. [DOI] [PubMed] [Google Scholar]
- 18. Kwak YH, Lee S, Lee MC, Han HS. Large meniscus extrusion ratio is a poor prognostic factor of conservative treatment for medial meniscus posterior root tear. Knee Surg Sports Traumatol Arthrosc. 2018;26(3):781–786. [DOI] [PubMed] [Google Scholar]
- 19. LaPrade CM, James EW, Cram TR, et al. Meniscal root tears: a classification system based on tear morphology. Am J Sports Med. 2015;43(2):363–369. [DOI] [PubMed] [Google Scholar]
- 20. LaPrade MD, Kennedy MI, Wijdicks CA, LaPrade RF. Anatomy and biomechanics of the medial side of the knee and their surgical implications. Sports Med Arthrosc Rev. 2015;23:63–70. [DOI] [PubMed] [Google Scholar]
- 21. LaPrade RF, Engebretsen AH, Ly TV, et al. The anatomy of the medial part of the knee. J Bone Joint Surg Am. 2007;89(9):2000–2010. [DOI] [PubMed] [Google Scholar]
- 22. Lee CR, Bin SI, Kim JM, Kim NK. Magnetic resonance imaging findings in symptomatic patients after arthroscopic partial meniscectomy for torn discoid lateral meniscus. Arthroscopy. 2016;32(11):2366–2372. [DOI] [PubMed] [Google Scholar]
- 23. Lee JH, Lim YJ, Kim KB, Kim KH, Song JH. Arthroscopic pullout suture repair of posterior root tear of the medial meniscus: radiographic and clinical results with a 2-year follow-up. Arthroscopy. 2009;25(9):951–958. [DOI] [PubMed] [Google Scholar]
- 24. Logerstedt DS, Snyder-Mackler L, Ritter RC, Axe MJ; Orthopedic Section of the American Physical Therapy Association. Knee pain and mobility impairments: meniscal and articular cartilage lesions. J Orthop Sports Phys Ther. 2010;40(6):A1–A35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Majewski M, Susanne H, Klaus S. Epidemiology of athletic knee injuries: a 10-year study. Knee. 2006;13(3):184–188. [DOI] [PubMed] [Google Scholar]
- 26. Masini BD, Dickens JF, Tucker CJ, et al. Epidemiology of isolated meniscus tears in young athletes. Orthop J Sports Med. 2015;3(7 suppl 2):2325967115S2325900107. [Google Scholar]
- 27. Matheny LM, Ockuly AC, Steadman JR, LaPrade RF. Posterior meniscus root tears: associated pathologies to assist as diagnostic tools. Knee Surg Sports Traumatol Arthrosc. 2015;23(10):3127–3131. [DOI] [PubMed] [Google Scholar]
- 28. Okazaki Y, Furumatsu T, Shimamura Y, et al. Time-dependent increase in medial meniscus extrusion after medial meniscus posterior root tear analyzed by using magnetic resonance imaging. Knee Surg Relat Res. 2019;31(2):120–125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Ozeki N, Koga H, Matsuda J, et al. Biomechanical analysis of the centralization procedure for extruded lateral menisci with posterior root deficiency in a porcine model. J Orthop Sci. 2020;25(1):161–166. [DOI] [PubMed] [Google Scholar]
- 30. Ozeki N, Muneta T, Kawabata K, et al. Centralization of extruded medial meniscus delays cartilage degeneration in rats. J Orthop Sci. 2017;22(3):542–548. [DOI] [PubMed] [Google Scholar]
- 31. Pagnani MJ, Cooper DE, Warren RF. Extrusion of the medial meniscus. Arthroscopy. 1991;7:297–300. [DOI] [PubMed] [Google Scholar]
- 32. Peltier A, Lording T, Maubisson L, et al. The role of the meniscotibial ligament in posteromedial rotational knee stability. Knee Surg Sports Traumatol Arthrosc. 2015;23(10):2967–2973. [DOI] [PubMed] [Google Scholar]
- 33. Roemer FW, Frobell R, Hunter DJ, et al. MRI-detected subchondral bone marrow signal alterations of the knee joint: terminology, imaging appearance, relevance and radiological differential diagnosis. Osteoarthritis Cartilage. 2009;17(9):1115–1131. [DOI] [PubMed] [Google Scholar]
- 34. Swamy N, Wadhwa V, Bajaj G, Chhabra A, Pandey T. Medial meniscal extrusion: detection, evaluation and clinical implications. Eur J Radiol. 2018;102:115–124. [DOI] [PubMed] [Google Scholar]
- 35. Wang Y, Wluka AE, Pelletier JP, et al. Meniscal extrusion predicts increases in subchondral bone marrow lesions and bone cysts and expansion of subchondral bone in osteoarthritic knees. Rheumatology (Oxford). 2010;49(5):997–1004. [DOI] [PubMed] [Google Scholar]