Dear Editor,
The recent coronavirus disease (COVID‐19), which was first reported in China, has spread around the world, causing major public health concerns. 1 Several treatments have been proposed for the treatment of COVID‐19, including hydroxychloroquine, monoclonal antibodies, corticosteroids, favipiravir, lopinavir/ritonavir, anticoagulants, and azithromycin. 2 Here, we present a case of pustular psoriasis, exacerbated by COVID‐19 in a patient with a history of hydroxychloroquine use. Patient consent for publication is achieved.
The patient was a 47‐year‐old woman, presenting with pustular lesions over the past 3 weeks. The COVID‐19 symptoms, including sore throat, myalgia, fever, and dry cough (for 8 days), had developed over the past 6 weeks. The chest computed tomography (CT) scan showed bilateral peripheral ground‐glass opacities and infiltrations. Oxygen saturation was in the normal range. She was tested for COVID‐19, and the positive result of polymerase chain reaction (PCR) assay confirmed the diagnosis. She was quarantined for 14 days and treated with hydroxychloroquine (400 mg twice on the first day and then 200 mg twice for the next 4 days). However, she had continued the use of hydroxychloroquine (200 mg) daily for 5 weeks.
The patient had been diagnosed with pustular psoriasis 4 years ago. She had been treated with methotrexate for 1 year (12.5 mg weekly for 3 months and 7.5 mg weekly for the next 9 months), and no similar lesions had developed during this period. She had a history of rheumatoid arthritis and had received hydroxychloroquine treatment for 12 months 4 years ago. On physical examination, active pustular lesions were found on the trunk and extremities. The lesions had developed 3 weeks after the emergence of COVID‐19 symptoms and had gradually progressed. The results of laboratory tests, including complete blood cell count and biochemical tests, were normal. Also, complement levels, as well as collagen vascular tests, including rheumatoid factor (RF) and anti‐cyclic citrullinated peptide (anti‐CCP) tests, were all within the normal range.
The levels of C‐reactive protein (CRP) and lactate dehydrogenase (LDH) were 50 mg/L and 915 U/L, respectively. However, a nasopharyngeal COVID‐19 test still indicated a positive result. A skin punch biopsy was performed on the trunk lesions. Microscopic examination showed subcorneal pustules on the skin tissue, characterized by many neutrophils, moderate psoriasiform epidermal hyperplasia, and mild spongiosis (Figure 1). The exocytosis of neutrophils into the spongiotic areas (spongiform pustules), dilated tortuous capillaries in the edematous dermal papillae, and infiltration of mixed inflammatory cells, including lymphocytes and neutrophils, were also observed (Figure 2).
FIGURE 1.

Generalized pustular lesions and erythematous scaly lesions
FIGURE 2.
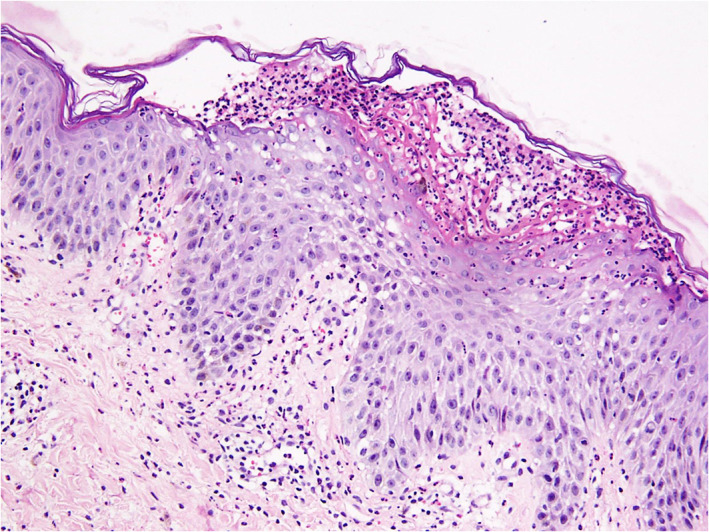
Subcorneal pustules covered by a thin layer of orthokeratosis and the exocytosis of neutrophils into spongiotic areas (spongiform pustules), dilated tortuous capillaries in the edematous dermal papillae, and infiltration of mixed inflammatory cells, including lymphocytes and neutrophils
Kutlu and Metin 3 reported the first case of psoriasis exacerbation in a patient with COVID‐19, who was treated with hydroxychloroquine and oseltamivir. There have been several mechanisms proposed for hydroxychloroquine to induce psoriasis, as the inhibition of epidermal transglutaminase, induction of IL17, and so on. But in a systematic review, it is mentioned that many of the patients who developed psoriasis also had other inflammatory diseases, which may be a source for concomitant psoriasis, due to cytokine dysregulations such as IL17 and 23. 4 COVID‐19 may also cause theses cytokine dysregulations and predispose patients to inflammatory diseases in susceptible patients.
So far (August 2020), two cases of plaque psoriasis and one case of guttate psoriasis have been reported secondary to COVID‐19. 4 , 5 , 6 Ozaras et al, who reported one case of plaque psoriasis, found that after COVID‐19 treatment, the patient's psoriatic lesions also regressed without any specific treatment 4 ; in other words, COVID‐19 was responsible for these lesions. Here, we reported the first case of pustular psoriasis, exacerbated by COVID‐19. Although the patient had used hydroxychloroquine, she had a history of hydroxychloroquine use without exacerbation of psoriasis; therefore, it seems that COVID‐19 led to the psoriasis flare‐up.
CONFLICT OF INTEREST
The authors declare no potential conflict of interest.
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to privacy or ethical restrictions.
REFERENCES
- 1. Wu Z, McGoogan JM. Characteristics of and important lessons from the Coronavirus Disease 2019 (COVID‐19) outbreak in China: summary of a report of 72 314 cases from the Chinese Center for Disease Control and Prevention. JAMA. 2020;323:1239–1242. 10.1001/jama.2020.2648. [DOI] [PubMed] [Google Scholar]
- 2. Galluccio F, Ergonenc T, Garcia Martos A, et al. Treatment algorithm for COVID‐19: a multidisciplinary point of view. Clinic Rheumatol. 2020;39(7):2077‐2084. 10.1007/s10067-020-05179-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Kutlu Ö, Metin A. A case of exacerbation of psoriasis after oseltamivir and hydroxychloroquine in a patient with COVID‐19: will cases of psoriasis increase after COVID‐19 pandemic? Dermatol Ther. 2020;e13383. 10.1111/dth.13383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Sachdeva M, Mufti A, Maliyar K, Lytvyn Y, Yeung J. Hydroxychloroquine effects on psoriasis: a systematic review and a cautionary note for COVID‐19 treatment. J Am Acad Dermatol. 2020;83:579‐586. 10.1016/j.jaad.2020.05.074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Ozaras R, Berk A, Ucar DH, Duman H, Kaya F, Mutlu H. Covid‐19 and exacerbation of psoriasis. Dermatol Ther. 2020;33:e13632. 10.1111/dth.13632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Gananandan K, Sacks B, Ewing I. Guttate psoriasis secondary to COVID‐19. BMJ Case. 2020;13(8):1‐2. 10.1136/bcr-2020-237367. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to privacy or ethical restrictions.


