Abstract
Introduction
The rapid spread of the pandemic caused by the severe acute respiratory syndrome coronavirus 2 (SARS‐CoV‐2/)(COVID‐19) virus resulted in governments around the world instigating a range of measures, including mandating the wearing of face coverings on public transport/in retail outlets.
Methods
We developed a sequential assessment of the risk reduction provided by face coverings using a step‐by‐step approach. The UK Office of National Statistics (ONS) Population Survey data were utilised to determine the baseline total number of community‐derived infections. These were linked to reported hospital admissions/hospital deaths to create case admission risk ratio and admission‐related fatality rate. We evaluated published evidence to establish an infection risk reduction for face coverings. We calculated an Infection Risk Score (IRS) for a number of common activities and related it to the effectiveness of reducing infection and its consequences, with a face covering, and evaluated their effect when applied to different infection rates over 3 months from July 24, 2020, when face coverings were made compulsory in England on public transport/retail outlets.
Results
We show that only 7.3% of all community‐based infection risk is associated with public transport/retail outlets. In the week of July 24, The reported weekly community infection rate was 29 400 new cases at the start (July 24). The rate of growth in hospital admissions and deaths for England was around −15%/week, suggesting the infection rate, R, in the most vulnerable populations was just above 0.8. In this situation, average infections over the evaluated 13 week follow‐up period, would be 9517/week with face covering of 40% effectiveness, thus, reducing average infections by 844/week, hospital admissions by 8/week and deaths by 0.6/week; a fall of 9% over the period total. If, however, the R‐value rises to 1.0, then, average community infections would stay at 29 400/week and mandatory face coverings could reduce average weekly infections by 3930, hospital admissions by 36 and deaths by 2.9/week; a 13% reduction.
If the R‐value rose and stayed at 1.2, then, expected average community‐derived hospital admissions would be 975/week and 40% effective face coverings would reduce this by 167/week and reduce possible expected hospital deaths from 80/week to 66/week.
These reductions should be seen in the context that there was an average of 102 000/week all‐cause hospital emergency admissions in England in June and 8900 total reported deaths in the week ending August 7, 2020.
Conclusion
We have illustrated that the policy on mandatory use of face coverings in retail outlets/on public transport may have been very well followed, but may be of limited value in reducing hospital admissions and deaths, at least at the time that it was introduced, unless infections begin to rise faster than currently seen. The impact appears small compared with all other sources of risk, thereby raising questions regarding the effectiveness of the policy.
What’s known
The rapid spread of the pandemic caused by the severe acute respiratory syndrome coronavirus 2 (SARS‐CoV‐2) (COVID‐19) virus has resulted in governments around the world instigating a range of measures to limit spread and facilitate economical recovery.
One of these measures, adopted by several countries, includes the use of face coverings in enclosed spaces were social distancing is not possible, including public transport.
What’s new
Around 7% of all community‐based infection risk is associated with public transport and retail outlets.
This contrasts with 57% associated with work or study, for those aged 16 years and over.
The benefits of public wearing of face masks compared with all other sources of risk, needs continually to be evaluated. Wearing of face masks in the work place may be more effective.
1. INTRODUCTION
The international coronavirus disease (COVID‐19) pandemic caused by the severe acute respiratory syndrome coronavirus 2 (SARS‐CoV‐2) virus has resulted in governments around the world instigating a range of measures to limit spread and facilitate economic recovery. One of these measures recommended by the World Health Organisation in updated guidance on the June 5, 2020, and adopted by many countries, includes the use of non‐medical fabric face coverings in enclosed spaces where there is known or suspected widespread transmission and where social distancing is not possible. 1
In the United Kingdom (UK), after initially suggesting that face coverings were not necessary, despite prior reports in April 2020 at the height of the pandemic suggesting that they might be useful when used in a risk‐based way, 2 the UK government introduced mandatory mass use of face coverings on public transport on the June 15, 2020, and in retail outlets on the July 24, 2020. 3 This was aimed at offsetting some of the additional infection risks being taken by reduced social distancing from 2 metres to “1 metre plus,” thereby facilitating easing of restrictions and supporting plans to stimulate the economy, particularly in the hard‐hit retail sector. One of the drivers to the implementation of this policy was the review published by the Royal Society of Medicine and the British Academy which stated that “cloth face coverings are effective in reducing source virus transmission, ie, outward protection of others, when they are of optimal material and construction (high‐grade cotton, hybrid and multilayer) and fitted correctly and for source protection of the wearer.” 4
UK government guidance at the time stated that; “The best available scientific evidence is that, when used correctly, wearing a face‐covering may reduce the spread of coronavirus droplets in certain circumstances, helping to protect others.” 3 This statement is undoubtedly true. However, the real‐world impact of the use of face covering on public transport and in retail outlets in the UK has received little attention. At the time of writing this article, there are no data to assess this objectively.
While data are emerging from other countries on the impact of precautionary measures, including the use of face coverings, these address the issue from a range of perspectives. For example, Hseih et al attempted to estimate the impact by examining the coincidence of mass mask use and influenza infections. 5 However, it is difficult to determine whether the take‐up of face coverings wearing was responsible for the observed changes. Chu et al performed a systematic review and meta‐analysis of 172 observational studies across 16 countries and six continents, on three precautionary measures, including the use of face coverings . 6 They suggested that face masks have value in reducing the spread of infection. However, in the assessment of face masks, the majority of studies were in healthcare settings; only three (n = 725; examining the SARS virus in China and Vietnam) were from non‐healthcare settings, where wearing face masks was associated with a lower risk of infection (relative risk 0.56, 95% CI 0.40 to 0.79). The American College of Physicians also raises questions around the evidence to support the effectiveness of face coverings in reducing transmission. 7 The only study we identified that examined the introduction of face coverings on public transport and in retail outlets examined the association between introduction of face coverings in a specific region of Germany relative to when they were introduced in other comparator regions. 8 While this study suggested that “face masks reduce the daily growth rate of reported infections by around 40%,” the design of the study means that it is difficult to assign the observed effect to the introduction of compulsory face coverings in a causal fashion.
While there is a debate about the effectiveness of face coverings in terms of the spread of infections, there is also an argument that such analysis should also assess the wider consequences, including economic and mental health‐associated effects. To our knowledge, there is no published data on the economic impact of the use of face coverings in the UK, though Goldman Sachs estimated that introducing national mandatory use of face coverings could potentially prevent additional restrictions that would otherwise cost around 5% of US GDP. 9 Furthermore a recent short review by Tian et al 10 found that, in relation to face coverings, the evidence indicates that a higher‐level specification of face masks are essential to protect healthcare workers from COVID‐19 infection and that community face coverings in the case of well individuals could be beneficial in certain circumstances, where transmission may be pre‐symptomatic.
In terms of mental health, while it may be argued that, irrespective of the actual effectiveness, the mandating of use of face coverings in enclosed spaces provides a measure of reassurance to the wearer, there are potentially wider mental health implications which make a thorough assessment critical, particularly at a time when mental well‐being is being stretched to the limits. 11 , 12 , 13 Wearing of face coverings may provide a degree of short‐term reassurance to people with some types of mental health challenge, 14 whilst others may perceive the increased use of face coverings as heightening their sense of threat and insecurity. 15
Given the potential physical, social, economic and mental implications of implementing this policy, we sought to model its potential impact. Using available data, we examined the number of infections, hospital admissions and hospital deaths potentially prevented by the use of face coverings in retail outlets and on public transport.
2. METHODS
2.1. Baseline data on community infections
We developed a sequential assessment of the risk reduction provided by face coverings using a step‐by‐step approach. As a baseline, we utilised the Office of National Statistics (ONS) Population Survey data to determine the baseline total number of community‐derived infections. 16 The ONS Population Survey released on the July 24, 2020 16 provided data that estimated, for the most recent week for which data are available (July 13‐19, 2020). This excluded those in hospitals, care homes or other institutional settings (but not those who work in these settings). This baseline figure of 2800 cases per day is used in subsequent modelling.
2.2. Step 1: Source of infection
We considered the impact on the number of infections within the community rather than in hospitals or care homes, as these are where people using retail and public transport will be most reflected. There will be some cross infections but the level of this is beyond the scope of this analysis but is likely to be small.
Given that it is unlikely that people displaying more severe symptoms of infection would use public transport or visit retail outlets, we then utilised ONS and wider literature data to estimate the proportion of asymptomatic or pre‐symptomatic cases.
The ONS data suggests that only around one‐third of individuals testing positive for COVID‐19 on a swab test reported having symptoms. 17 This was based on self‐reported symptoms, and therefore, may be an underestimate. According to Diana et al, transmission by pre‐symptomatic people accounts for around 40%‐60% of transmissions and asymptomatic cases accounts for around 15% of transmissions, indicating that between 55% and 75% of infections may be derived from people without symptoms. 18 While posted on the preprint service website, medRxiv, early in the pandemic, these data were reviewed and assessed by the Centre for Evidence‐Based Medicine on July 23, 2020. 19 According to Yin and Jin, there is no difference in transmissibility between those with and without symptoms. 20 For the modelling, we used a conservative estimate of 80% of infections from pre‐ or asymptomatic cases.
2.3. Step 2: Infection risk by activity
We calculated an Infection Risk Score (IRS) for a number of common activities. First, based on location, we categorised daily activities into the following: home, work, public transport, retail outlets, other activities (indoors) and other activities (outside). We calculated the average length of time spent per day on each of these activities. This was based on the UK Time Use Survey, 2014‐2015, 21 as quoted in a Scottish government report, 22 and a Resolution Foundation report in July 2020. 23 This describes average minutes per day spent by those aged 16 years and over on the following activities: (a) Paid work, (b) Unpaid work (subdivided into housework; shopping, services and household management; childcare; travel; construction and repairs; and voluntary work), (c) Study and (d) Leisure: (subdivided into TV and other leisure; social life, culture and entertainment; and sports and outdoor leisure). Each of these categories was assigned to one of the groups listed in Table 1, with 8 hours allocated to sleep (based on the Resolution Foundation report, 23 which quotes the UK Time Use Survey as assigning 8.5 hours to sleep for the 18‐64 age group). For the modelling, we assumed that 50% of all travel time was using public transport and that the category defined in the UK Time Use Survey as “shopping, services and household management” comprised 50% of time allocated to various forms of shopping, including for groceries, clothing and that undertaken for leisure. We realise that these are likely to be overestimates (68% of workers typically travelled to work by car according to the UK Department of Transport's Transport Statistics Great Britain 2019), 24 while household management includes house cleaning, washing and other household chores that would typically take up more than 50% of “shopping, services and household management” activities), but elected to take a conservative approach.
TABLE 1.
The contribution of different activities on Infection Risk Score and the impact of face coverings on infection risk
| Location | Time hrs/day | Relative infection risk | IRS | % of total IRS | IRS reduction (using face coverings) | |||
|---|---|---|---|---|---|---|---|---|
| 20% risk reduction | 40% risk reduction | 60% risk reduction | 80% risk reduction | |||||
| Home (including sleep) | 16.69 | 1 | 16.69 | 28.3% | 16.7 | 16.7 | 16.7 | 16.7 |
| Work/study | 5.61 | 6 | 33.66 | 57.1% | 33.6 | 33.6 | 33.6 | 33.6 |
| Public transport | 0.47 | 5 | 2.35 | 4.0% | 1.9 | 1.4 | 0.9 | 0.5 |
| Retail | 0.39 | 5 | 1.97 | 3.3% | 1.6 | 1.2 | 0.8 | 0.4 |
| Leisure inside | 0.44 | 7 | 3.05 | 5.2% | 3.0 | 3.0 | 3.0 | 3.0 |
| Leisure outside | 0.41 | 3 | 1.22 | 2.1% | 1.2 | 1.2 | 1.2 | 1.2 |
| Total infection risk score | 58.96 | 58.0 | 57.2 | 56.3 | 55.5 | |||
| Percentage overall risk reduction | −1.5% | −2.9% | −4.4% | −5.8% | ||||
Each activity was then assigned a risk of infection. This was based on a risk stratification approach used by the Texas Medical Association, as ranked by physicians from the Texas Medical Association COVID‐19 Task Force and the Texas Medical Association Committee on Infectious Diseases. 25 This was then sense‐checked using ONS data, 26 which allowed assessment of the infection risk associated with working from home versus working in other environments. These two components were combined to calculate the activity IRS, and then, summed. The % of this total allowed us to assess the percentage contributions to the risk associated with each activity, all other aspects assumed being equal.
We elected to use conservative overestimates of the IRS associated with transport/retail activities. It should be noted that having to wear face coverings may inhibit frivolous or spontaneous travel and shopping activities, and hence, the proportion of time spent on these activities following the implementation of the mandatory policy may decrease, at least after an initial surge following the easing of restrictions.
2.4. Step 3: Impact of the use of face coverings
The effectiveness of face coverings in reducing infections will be dependent on two broad factors: (i) the proportion of infections that are because of aerosols and other airborne routes of transmission and (ii) the efficacy of face coverings of reducing the spread of such airborne‐associated infections. Neither of these is likely to be 100%.
Face coverings are unlikely to be effective in mitigating against all transmission routes. The World Health Organisation (WHO) published a detailed assessment of routes of transmission. 27 The European Centre for Disease Prevention and Control states that infection is understood to be mainly transmitted via large respiratory droplets. 28 However, the proportion of infections caused by airborne or other routes that could be prevented by face coverings, while less than 100%, is difficult to quantify. Indeed, 80% might be considered a conservative estimate.
Furthermore, the efficiency of face coverings in regard to preventing airborne transmission is likely to be highly variable, 29 not least because of the wide range of types of face coverings used (from scarves to surgical‐grade masks), and their correct usage (as emphasised in UK government guidance 3 ). Indeed, laboratory‐based experimental data from van der Sande et al suggests that home‐made face coverings offered around 29%‐78% protection against aerosol transmission over short periods, while surgical masks provided 50%‐91% protection. 29 Efficiency in population settings, and in cases of prolonged contact, is likely to be lower and more variable than these estimates. However, on the contrary, if two people who come into close contact are both wearing face coverings, infection risk is likely to be further reduced.
Combined, the reduction in infection risk associated with the use of face coverings were modelled as using a range of values covering estimates (20%, 40%, 60% and 80%) as example scenarios.
2.5. Assessment of the impact of the use of face coverings on infections, hospital admissions and deaths
Using this stepped approach, we assessed the potential impact of face coverings on (a) number of current and consequent future infections, (b) number of hospital admissions and (c) number of hospital deaths.
The ONS Coronavirus (COVID‐19) Infection Survey pilot 16 reported the modelled daily incidence infection rate for each week based on exploratory modelling. At the time of writing, the modelling used to calculate the incidence rate was a Bayesian model and used all swab test results to estimate the incidence rate of new infections for each different type of respondent who tested negative when they first joined the study. This can be multiplied by 7 to give an expected total number of new community infections each week from all sources. The number reported in the week before the imposition of face coverings on the July 24, 2020 was taken as the baseline for this study.
NHS England 30 reported daily hospital COVID‐19 admission data which included all people admitted to hospital who already had a confirmed COVID‐19 status at the point of admission and those who tested positive in hospital after admission. Inpatients diagnosed with COVID‐19 after admission were reported as being admitted on the day before their diagnosis. Admissions included data from all NHS acute hospitals and mental health and learning disability trusts, as well as independent service providers commissioned by the NHS. It was assumed that patients would be admitted 7 days after their original infection and so a ratio of hospital admission to the previous week's number of infections enabled us to calculate an infections admission rate (IAR). However, in these admitted patients, infections might have occurred within either the community, care homes or hospital so we conservatively assumed that 50% of this infection hospitalisation rate occurred within the community (data from Germany 31 suggests that this might be significantly lower than this).
NHS England 30 also reported daily the deaths of patients who had died in hospitals and had either tested positive for COVID‐19 or where COVID‐19 was mentioned on the death certificate. All deaths were recorded against the date of death. In our analysis, the length of stay in hospital before death was assumed to be 2 weeks so the ratio of total deaths to the total admissions 2 weeks previously give an estimate of hospital admissions fatality rate (AFR). We conservatively assume that the AFR from community admissions are similar to those from care homes and hospital infections.
The benefit of any mitigation measure was assessed not only as those avoided directly, but also those consequent future infections. We estimated this based on the re‐infection rate (R‐value) and re‐infection cycle time, over a defined period (3 months). We utilised 3 months as, by the end of this period, the situational outlook would likely be reviewed. European Centre for Disease Prevention and Control 32 report viral RNA shedding peaking in the second week after infection so a conservative re‐infection cycle time of 8 days was applied from July 24, 2020. At this time, the UK Government reported an R‐value range for the UK of 0.7‐0.9 and a growth rate was given as −4% to −1% as of July 24, 2020. 33 Consequently, three R‐values; namely 0.8 (the accepted level at the time of the introduction of mandatory face coverings), 1.0 (a worsening to equilibrium) and 1.2 (the pandemic restarting) were used in our analysis. For each of these, we calculated the total number of consequent future infections that could be expected to flow from the original infections.
Baseline effectiveness of face coverings and the IRS calculated above for retail outlets and public transport was applied to each scenario to calculate the expected infections, hospitalisations and deaths over the next 3 months. The sensitivity of the results to the assumptions on face‐covering effectiveness was tested by calculation of the above for no face coverings (0%), 20%, 40%, 60% and 80%.
3. RESULTS
3.1. Baseline data & proportion of pre‐symptomatic and asymptomatic cases
Based on the ONS survey data, we modelled the impact of face coverings based on 2800 community cases per day. Of these, 80% are estimated to be because of transmission from pre‐symptomatic and asymptomatic cases. These generate a baseline figure for assessment of the impact of face coverings of 2240 community cases.
3.2. Infection risk by activity
Table 1 shows the calculated IRS for each of the six common activities. This shows that around 7.3% (4.3/58.9) of all community‐based risk of infection is associated with public transport and retail outlets (4.0% for public transport and 3.3% for retail outlets). Hence, any measure to reduce infections within these sectors will have a relatively minor impact. In contrast, 57.1% of the risk was associated with paid work and 28.3% with activities carried out at home.
3.3. Impact of face coverings on Infection Risk Score
We then assessed the impact of the use of face coverings in retail outlets and on public transport on the overall IRS, using the four different degrees of effectiveness of face coverings in reducing transmission, namely 20%, 40%, 60% and 80%. Table 1 shows that risk score reduced from 58.9 to 58.0 (1.5% reduction in overall risk) for a face covering‐associated efficacy of 20%, to 57.2 (2.9% reduction in overall risk) for an efficacy of 40%, to 56.3 (4.4% reduction in overall risk) for an efficacy of 60%, and to 55.5 (5.8% reduction in overall risk) for an efficacy of 80%. A surgical mask, as used in hospitals, with an efficacy of over 90% would only reduce overall risk by 6.6% up to the maximum 7.3%.
3.4. Impact on current and future infection
At the start of the period beginning July 24, 2020, the ONS community survey reported a daily incidence of 0.78/10 000 (0.4‐1.49); equivalent to 4200 new community infections each day. The latest ONS community incidence report at the time of writing was 0.44 (at August 7, 2020). This is the equivalent to a fall of 14%/week. Hospital admissions and deaths are falling at similar rates. This all suggests that the underlying R‐value in the population was just above 0.8.
In the 4 weeks prior to the August 13, 2020, the community infection admission rate, including an assumed 50% from community infections, would then be 0.9%. The admission fatality rate during the same period was found to be 8.2%.
Figure 1A shows graphically the impact of the different assumed R‐value (0.8, 1.0, 1.2) on the infection outcomes over the 13 weeks and the potential cumulative numbers for both with or without face coverings for the three levels of R then on infections (Figure 1B), community hospitalisation (Figure 1C) and deaths (Figure 1D). We show, for each of the assigned R‐value, the impact of wearing face coverings in public transport and retail environments on new infections/week, cumulate deaths, hospital admissions and cumulative infections.
FIGURE 1.
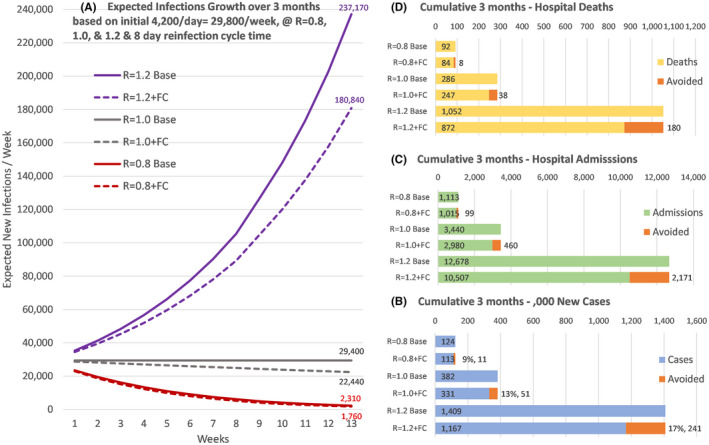
Expected number of new community cases each week over 13 weeks based on R‐values of 0.8%, 1.0% or 1.2% and 40% effectiveness of face coverings (FC). (a) for the expected difference if face coverings are used on public transport and in retail outlets, and cumulative over the period with and without face coverings showing amounts avoided for the total number of community cases (b), community hospitalisation (c) and hospital deaths expected (d)
This showed, based on 4200 new community infections/day (29 400/week), and R‐value of 0.8 (both derived from ONS data from the time of introduction of mandatory face coverings at the end of July 2020) and a 40% effectiveness of face coverings, that the number of direct and indirect infections associated with public transport and retail outlets over the 3 months would be reduced from 124 000 by 11 000; a reduction of 9%.
If the infection rate was to increase to and stayed at, 1.0 then weekly infections would remain at 29 400 (or 382 200 over 3 months). A 40% effective face covering worn in public transport and retail could reduce the 3‐month total by 51 000 or 13%.
3.5. Impact on hospital admissions and death rates
Table S1 showed that, based on data from the ONS and NHS England, that the average rate of hospitalisation (reduced by 50% to remove hospital and care home admissions, as justified in the Methods section) over the previous week was 0.9% of community infections. Deaths in hospital, when linked to hospital admissions recorded over the prior 2 weeks, were found to be 8.2% of these admissions.
When the R‐value was 0.8, with face‐covering effectiveness at 40%, average community hospital admissions fell from 86/week to 78/week and community infected hospital deaths fell from 7.0/week to 6.4/week (Table 2).
TABLE 2.
Projections for average weekly values over the 3 months from the introduction of mandatory face coverings on July 24, 2020 (based on starting at 29 400 new cases/week)
| Ongoing R‐value | Mask transmission reduction | Community cases | Community hospitals admissions | Community hospital deaths | Difference community cases | Difference community hospitals admissions | Difference community hospital deaths | % Difference to no face coverings |
|---|---|---|---|---|---|---|---|---|
| 0.8 | No face covering | 9517 | 86 | 7.0 | ||||
| 20% | 9083 | 82 | 6.7 | −434 | −4 | −0.3 | −5% | |
| 40% | 8673 | 78 | 6.4 | −844 | −8 | −0.6 | −9% | |
| 60% | 8286 | 75 | 6.1 | −1231 | −11 | −0.9 | −13% | |
| 80% | 7920 | 71 | 5.8 | −1597 | −15 | −1.2 | −17% | |
| 1.0 | No face covering | 29 400 | 265 | 21.7 | ||||
| 20% | 27 356 | 246 | 20.2 | −2044 | −18 | −1.5 | −7% | |
| 40% | 25 470 | 229 | 18.8 | −3930 | −36 | −2.9 | −13% | |
| 60% | 23 731 | 214 | 17.5 | −5669 | −51 | −4.2 | −19% | |
| 80% | 22 127 | 199 | 16.3 | −7273 | −66 | −5.4 | −25% | |
| 1.2 | No face covering | 108 358 | 975 | 80.0 | ||||
| 20% | 98 637 | 888 | 72.8 | −9720 | −87 | −7 | −9% | |
| 40% | 89 804 | 808 | 66.3 | −18 554 | −167 | −14 | −17% | |
| 60% | 81 780 | 736 | 60.4 | −26 578 | −239 | −20 | −25% | |
| 80% | 74 492 | 670 | 55.0 | −33 865 | −305 | −25 | −31% |
Key Assumptions: Asymptomatic = 80%; Retail/Public Transport Infections = 7.3%; Case Hospitalisation Admission Rate = 0.9%; Hospital Admission Fatality Rate = 8.2%.
If R rose and stayed at 1.0, then, expected average community‐derived hospital admissions would be 265/week and 40% effective face coverings would reduce this by 36/week and reduce possible expected hospital deaths from 22/week to 19/week (Table 2).
If R rose and stayed at 1.2, then, expected average community‐derived hospital admissions would be 975/week and 40% effective face coverings would reduce this by 167/week and reduce possible expected hospital deaths from 80/week to 66/week (Table 2).
The above findings can be put into the context that the ONS 34 reported 93% of adults had worn face coverings when shopping in the 7 days to August 21, 2020. Furthermore, NHS England 35 reported that there were 102 000/week all‐cause hospital emergency admissions in England in June 2020 down 27% on the previous year and there were a total of 8900 reported deaths by the ONS 35 , 36 in the week ending August 7 of which 3430 occurred in hospitals.
4. DISCUSSION
We have modelled the potential impact of the use of face coverings worn in retail outlets and on public transport on the number of UK COVID‐19 infections and associated hospital admissions and mortality rates. Overall, we demonstrated that only around 7% of all community‐based infection risk for those aged more than 16 years of age is associated with public transport and retail outlets. This contrasts with 57% associated with work or study, for those aged 16 years and over. This illustrates the limitations of the impact of any policy to reduce infections in the public transport and retail outlets sectors alone, irrespective of the efficiency of the intervention. It perhaps suggests that measures targeted at the workplace may be more worthwhile.
In addition to this, the requirement to wear face coverings may increase anxiety in some people and thereby result in a reluctance to utilise public transport and/or visit retail outlets. This may, therefore, reduce the time spent on these activities. While it is also possible that the use of face coverings may increase the confidence of other people, it is difficult to say whether this will negate the above effect. Certainly, public transport usage and retail footfall does not appear to have returned to pre‐pandemic levels, 37 , 38 and hence, the 7.3% may be an overestimate of the contribution of these activities to overall risk. However, in our modelling, given the difficulty in calculating this impact, we assumed this change in behaviour to be neutral.
For the determination of the impact of face coverings on reduction in infections, we used a range of R‐values to allow estimation of the potential change in the impact of face coverings in different phases of the pandemic that are relevant at this stage. The impact of any mitigation measure will have a more significant impact, at least in terms of overall numbers, the higher the R‐value. We showed that, with an R‐value of 0.8, with face covering of 40% effectiveness, average infections would be reduced by 844/week, hospital admissions by 8/week and deaths by 0.6/week; a fall of 9% over the period total. If, however, the R‐value rises to 1.0, then, average community infections would stay at 29 400/week and face coverings could reduce average weekly infections by 3930, hospital admissions by 36/week and deaths by 2.9/week; a 13% reduction. At an R‐value of 1.2, then, expected average community‐derived hospital admissions would be 975/week and 40% effective face coverings would reduce this by 167/week and reduce possible expected hospital deaths from 80/week to 66/week.
These reductions should be seen in the context of the reality that 93% of adults had worn face coverings when shopping in the 7 days to August 21, 2020. 34 These figures should be viewed with the perspective that there were a total of 437 500 emergency admissions reported 35 in June 2020, 17.3% lower than the same month last year and that all‐cause deaths at the start of August 2020 were reported 36 , 37 at 1270/day, of which 490 occurred in hospital.
This raises interesting questions around the timing of the implementation of the policies to mandate the use of face coverings in the retail and transport contexts; a time when the R‐value was less than one (most UK government reports suggested 0.7‐0.9) and the daily infection rate was relatively low in comparison to the peak in April 2020. 33 Use of face coverings in retail outlets and on public transport is of limited value, particularly when the R‐value is below 1, in contrast to March/April 2020 when the R‐value was much higher.
We also used a range of efficiencies of face coverings, reflecting the wide range of types of coverings, 3 variability in correct usage (particularly over prolonged periods) and uncertainty around which modes of transmission could be influenced by their use. 27 Realistically, an estimate of around 40% is likely to be a sensible conservative estimate, particularly in the context of the work by van der Sande et al 29 Under this assumption, the modelling showed that, if the R‐value was 0.8, the hospital deaths avoided would be less than 0.1/day and if, in the case that R‐value rose and stayed at 1.2, this could rise to 2 deaths/day avoided.
This study shows that face coverings, even when appropriate materials are used, and handling and wearing are fully compliant, can only generate limited benefits when used at low reinfection rates. By preventing potential future infections, they may play a more important role at times when reinfection rates are high. Indeed, UK government reports published in April suggested that the use of face coverings may have had some value, at least using a risk‐based approach, 2 but that the timing of their introduction was clearly too late for this to be of any significant impact.
Given our findings, we suggest that guidance on the potential usefulness of face coverings might benefit from greater clarity of message that is better targeted to those most likely to benefit (using a risk‐based approach), and in activities where the impact is likely to be larger. For example, the availability of more effective, surgical standard face masks (with clear guidance on correct use) for those more vulnerable to serious consequences of infection, and in contexts where they are at greater risk (such as in the workplace) might be of greater impact in terms of reduction in hospital admissions and deaths. Furthermore, as evidence suggests that effectiveness is higher when compliance is high and with proper use, 39 clear guidance on their use would be necessary, ideally alongside a more targeted, “carrot”‐based messaging as opposed to the mass mandating “stick” approach used to date.
This approach might also minimise the mental health consequences of widespread use of face coverings, 11 including by sending a more reassuring and realistic message to the population around risk. It may also encourage economic activity both in terms of high street spending and return to work.
Finally, these findings in no way relate to the use of approved face coverings in the care of vulnerable, frail and older individuals in the care home, hospital or primary care setting.
4.1. Strengths and Limitations
We recognise that such modelling is based on a range of assumptions. To address this, we have sought to use UK government/ONS data wherever possible, as these are the data that are likely to have been used to inform policy. We have also erred on the side of caution in our estimates. Furthermore, we recognise that the number of reported cases is influenced by the number of tests performed, and indeed by the false positive and negative rates of the tests (the impact of which may vary by incidence of the disease). Where estimates may differ widely (such as for face‐covering efficiency in reducing transmission), or subject to change (such as R‐value or number of daily cases), we have presented a range of scenarios to give a sense of the impact of face coverings at various levels of R face‐covering effectiveness.
5. CONCLUSION
We have illustrated that the policy on mandatory use of face coverings in retail outlets and on public transport in the UK, may have limited value in reducing hospital admissions and mortality rates, at least given the timing in relation to the course of the pandemic, when the policy was introduced.
We suggest that a National Institute for Health and Clinical Excellence (NICE) review is merited, assessing the cost‐effectiveness of the use of face coverings as a clinical intervention alongside other preventative measures, as a means of reduction in hospital admissions and indeed mortality.
DISCLOSURE
The authors declare that they have no conflict of interest.
Supporting information
Supplementary Material
Heald AH, Stedman M, Tian Z, Wu P, Fryer AA. Modelling the impact of the mandatory use of face coverings on public transport and in retail outlets in the UK on COVID‐19‐related infections, hospital admissions and mortality. Int J Clin Pract. 2021;75:e13768. 10.1111/ijcp.13768
DATA AVAILABILITY STATEMENT
All the data used in the preparation of this manuscript is publicly available from the sources cited in the paper and referenced accordingly.
REFERENCES
- 1. World Health Organisation . Advice on the use of masks in the context of COVID‐19: interim guidance; June 5, 2020. https://apps.who.int/iris/handle/10665/332293. Accessed October 6, 2020.
- 2.DELVE: Report on face masks for the general public; April 2020. https://www.gov.uk/government/publications/delve‐report‐on‐face‐masks‐for‐the‐general‐public‐21‐april‐2020. Accessed October 6, 2020.
- 3. UK Department of Health and Social Care . Face coverings: when to wear one and how to make your own; July, 2020. https://www.gov.uk/government/publications/face‐coverings‐when‐to‐wear‐one‐and‐how‐to‐make‐your‐own. Accessed August 31, 2020.
- 4. Royal Society . Face masks and coverings for the general public: behavioural knowledge, effectiveness of cloth coverings and public messaging. 2020. https://royalsociety.org/‐/media/policy/projects/set‐c/set‐c‐facemasks.pdf?la=en‐GB&hash=A22A87CB28F7D6AD9BD93BBCBFC2BB24BW
- 5. Hsieh CC, Lin CH, Wang WYC, Pauleen DJ, Chen JV. The outcome and implications of public precautionary measures in Taiwan‐declining respiratory disease cases in the COVID‐19 pandemic. Int J Environ Res Public Health. 2020;17:4877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Chu DK, Akl EA, Duda S, et al. Physical distancing, face masks, and eye protection to prevent person‐to‐person transmission of SARS‐CoV‐2 and COVID‐19: a systematic review and meta‐analysis. Lancet. 2020;395:1973‐1987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Qaseem A, Etxeandia‐Ikobaltzeta I, Yost J, et al. Use of N95, surgical, and cloth masks to prevent COVID‐19 in health care and community settings: living practice points from the American College of Physicians (Version 1) Ann Intern Med. 2020;M20–3234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Mitze T, Kosfeld R, Rode J, Wälde K. Face masks considerably reduce COVID‐19 cases in Germany: a synthetic control method approach. http://ftp.iza.org/dp13319.pdf. Accessed October 6, 2020. [DOI] [PMC free article] [PubMed]
- 9. Sachs G. Face masks and GDP. https://www.goldmansachs.com/insights/pages/face‐masks‐and‐gdp.html. Accessed August 31, 2020.
- 10. Tian Z, Stedman M, Whyte M, Anderson SG, Thomson G, Heald AH. IJCP Personal protective equipment (PPE) and infection among healthcare workers—What is the evidence? Int J Clin Pract. 2020: e13617. 10.1111/ijcp.13617 [DOI] [PubMed] [Google Scholar]
- 11. Pierce M, Hope H, Ford T, et al. Mental health before and during the COVID‐19 pandemic: a longitudinal probability sample survey of the UK population. Lancet Psychiatry. 2020;S2215–0366:30308‐30314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Shi L, Lu ZA, Que JY, et al. Prevalence of and risk factors associated with mental health symptoms among the general population in China during the coronavirus disease 2019 Pandemic. JAMA Netw Open. 2020;3:e2014053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Holmes EA, O'Connor RC, Perry VH, et al. Multidisciplinary research priorities for the COVID‐19 pandemic: a call for action for mental health science. Lancet Psychiatry. 2020;7:547‐560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Szczesniak D, Ciulkowicz M, Maciaszek J, et al. Psychopathological responses and face mask restrictions during the COVID‐19 outbreak: results from a nationwide survey. Brain Behav Immun. 2020;87:161‐162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. MIND . Mask anxiety, face coverings and mental health. https://www.mind.org.uk/information‐support/coronavirus/mask‐anxiety‐face‐coverings‐and‐mental‐health/. Accessed August 31, 2020.
- 16. Office for National Statistics . Coronavirus (COVID‐19) Infection Survey pilot: England; July 24, 2020. https://www.ons.gov.uk/releases/covid19infectionsurveyenglandprovisionalresults24july2020. Accessed August 31, 2020.
- 17. Office for National Statistics . Coronavirus (COVID‐19) infections in the community in England; July 2020. https://www.ons.gov.uk/peoplepopulationandcommunity/healthandsocialcare/conditionsanddiseases/articles/coronaviruscovid19infectionsinthecommunityinengland/july2020. Accessed August 31, 2020.
- 18. Buitrago‐Garcia DC, Egli‐Gany D, Counotte MJ, et al. The role of asymptomatic SARS‐CoV‐2 infections: rapid living systematic review and meta‐analysis. medRxiv. 2020. 10.1101/2020.04.25.20079103 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. The Centre for Evidence‐Based Medicine . The role of asymptomatic SARS‐CoV‐2 infections: systematic review. https://www.cebm.net/study/the‐role‐of‐asymptomatic‐sars‐cov‐2‐infections‐systematic‐review/. Accessed August 31, 2020.
- 20. Yin G, Jin H. Comparison of transmissibility of coronavirus between symptomatic and asymptomatic patients: reanalysis of the Ningbo COVID‐19 data. JMIR Public Health Surveill. 2020;6:e19464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Gershuny J, Sullivan O. United Kingdom Time Use Survey, 2014‐2015. UK Data Service. SN: 8128. 2020. 10.5255/UKDA-SN-8128-1 [DOI]
- 22. The Scottish Government . Centre for Time Use Research Time Use Survey 2014–15; Results for Scotland; February 2019. https://www.gov.scot/binaries/content/documents/govscot/publications/research‐and‐analysis/2019/03/centre‐time‐use‐research‐time‐use‐survey‐2014‐15‐results‐scotland/documents/centre‐time‐use‐research‐time‐use‐survey‐2014‐15/centre‐time‐use‐research‐time‐use‐survey‐2014‐15/govscot%3Adocument/centre‐time‐use‐research‐time‐use‐survey‐2014‐15.pdf. Accessed August 31, 2020.
- 23. Bangham G, Gustafsson M. The time of your life: Time use in London and the UK over the past 40 years, Resolution Foundation, July 2020.
- 24. UK government Department of Transport . Transport Statistics Great Britain 2019. https://www.gov.uk/government/statistics/transport‐statistics‐great‐britain‐2019. Accessed October 6, 2020.
- 25. Texas Medical Association . Know your risk during COVID‐19. https://www.texmed.org/uploadedFiles/Current/2016_Public_Health/Infectious_Diseases/309193%20Risk%20Assessment%20Chart%20V2_FINAL.pdf. Accessed August 31, 2020.
- 26. Office for National Statistics . Coronavirus (COVID‐19) Infection Survey; May 2020. https://www.ons.gov.uk/peoplepopulationandcommunity/healthandsocialcare/conditionsanddiseases/datasets/coronaviruscovid19infectionsurveydata/2020. Accessed August 31, 2020.
- 27. World Health Organisation . Transmission of SARS‐CoV‐2: implications for infection prevention precautions; July 2020. https://www.who.int/news‐room/commentaries/detail/transmission‐of‐sars‐cov‐2‐implications‐for‐infection‐prevention‐precautions. Accessed August 31, 2020.
- 28. European Centre for Disease Prevention and Control . Transmission of COVID‐19. https://www.ecdc.europa.eu/en/covid‐19/latest‐evidence/transmission. Accessed August 31, 2020.
- 29. van der Sande M, Teunis P, Sabel R. Professional and home‐made face masks reduce exposure to respiratory infections among the general population. PLoS One. 2008;3:e2618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.England Covid‐19 Hospital Admissions. https://coronavirus.data.gov.uk/healthcare. Accessed August 31, 2020.
- 31.Epidemiological bulletin: Infection environment of COVID‐19 outbreaks in Germany. September 2020. https://www.rki.de/DE/Content/Infekt/EpidBull/Archiv/2020/Ausgaben/38_20.pdf?__blob=publicationFile. Accessed October 6, 2020.
- 32.European Centre for Disease Prevention and Control Transmission of COVID‐19. https://www.ecdc.europa.eu/en/covid‐19/latest‐evidence/transmission. Accessed August 31, 2020.
- 33.UK Gov Guidance. The R number and growth rate in the UK. https://www.gov.uk/guidance/the‐r‐number‐in‐the‐uk#The‐R‐number‐range‐for,as‐of‐31‐July‐2020.The‐R‐number‐range‐for,as‐of‐24‐July‐2020.The‐R‐number‐range‐for,as‐of‐17‐July‐2020. Accessed August 31, 2020.
- 34.Coronavirus and the social impacts on Great Britain; August 7, 2020. https://www.ons.gov.uk/peoplepopulationandcommunity/healthandsocialcare/healthandwellbeing/bulletins/coronavirusandthesocialimpactsongreatbritain/7august2020. Accessed August 31, 2020.
- 35.NHS England hospital emergency admissions; June 2020. https://www.england.nhs.uk/statistics/wp‐content/uploads/sites/2/2020/07/Statistical‐commentary‐June‐2020‐jf8hj.pdf. Accessed August 31, 2020.
- 36.Office for National Statistics Deaths week ending 7th August. https://www.ons.gov.uk/peoplepopulationandcommunity/birthsdeathsandmarriages/deaths/bulletins/deathsregisteredweeklyinenglandandwalesprovisional/weekending7august2020#deaths‐registered‐by‐place‐of‐occurrence. Accessed August 31, 2020.
- 37. NHS England . Department for Transport. Transport use during the coronavirus (COVID‐19) pandemic. https://www.england.nhs.uk/statistics/statistical‐work‐areas/covid‐19‐daily‐deaths/UKhttps://www.gov.uk/government/statistics/transport‐use‐during‐the‐coronavirus‐covid‐19‐pandemic. Accessed August 31, 2020.
- 38.Office for National Statistics Population Survey Modelled Daily Incidence. https://www.ons.gov.uk/peoplepopulationandcommunity/healthandsocialcare/conditionsanddiseases/bulletins/coronaviruscovid19infectionsurveypilot/englandandwales14august2020. Accessed August 31, 2020.
- 39. Sim SW, Moey KS, Tan NC. The use of facemasks to prevent respiratory infection: a literature review in the context of the Health Belief Model. Singapore Med J. 2014;55:160‐167. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Material
Data Availability Statement
All the data used in the preparation of this manuscript is publicly available from the sources cited in the paper and referenced accordingly.


