Abstract
This multiple-baseline open pilot trial examined feasibility, compliance, acceptability, and preliminary indices of efficacy of Gaze-Contingent Music Reward Therapy (GC-MRT) for anxious 7-to 10-year-old children. GC-MRT is a novel therapy for anxiety disorders that relies on eye-tracking technology and operant conditioning principles to divert attention toward neutral over threat stimuli, with music serving as a reward. Using a multiple-baseline design, 12 children (Mage = 8.3 years, SD = .72, range = 7–10; 4 girls) with social anxiety disorder, generalized anxiety disorder, or separation anxiety disorder received 8 therapy sessions. Clinical status was determined via semistructured interviews and questionnaires. Patients were randomized to wait 1, 3, or 5 weeks between initial assessment and beginning of therapy. Self-reported anxiety was recorded weekly, and comprehensive clinical assessments were obtained pre- and posttreatment. All 12 patients completed the full course of GC-MRT within the allocated therapy period. Therapy credibility rates were moderate to high as reported by both children and parents. Clinician-rated anxiety levels remained consistent during baseline measurement and decreased significantly following treatment. Parent-reports also yielded significant reductions in child anxiety symptoms from pre- to posttreatment. However, child-reported anxiety did not change significantly. The results provide preliminary evidence for feasibility, acceptability, and efficacy of GC-MRT for young children with anxiety disorders. Efficacy should now be tested in randomized controlled trials.
Anxiety disorders are prevalent in youth and associated with significant distress and impairment (Beesdo, Knappe, & Pine, 2011). Although extant pharmacological and cognitive-behavioral therapies are effective, parents and children are often reluctant to use them or fail to comply with their demanding protocols. Of those who start therapy for anxiety disorders, up to 40% fail to respond (Rapee, Schniering, & Hudson, 2009), highlighting a need for novel treatments.
Attention bias modification therapy (ABMT) targets selective attention to threat, a well-replicated mechanism of anxiety (Bar-Haim, 2010; MacLeod & Clarke, 2015). Anxious individuals, across clinical definitions, exhibit attentional preferences toward threatening information (Bar-Haim, Lamy, Pergamin, Bakermans-Kranenburg, & Van IJzendoorn, 2007). Although most research has focused on transient biases, there is also evidence for more sustained biases in anxious youth (Price et al., 2013). Research also indicates that threat-related attention can shape developmental trajectories by modulating the association between early temperament and later clinical anxiety (Shechner et al., 2012). ABMT seeks to modify these biases through systematic attention retraining, with the premise that reduction in threat bias would lead to reduction in symptoms. Meta-analyses of ABMT trials in anxious adults indicate significant small-to-medium effect sizes (Linetzky, Pergamin-Hight, Pine, & Bar-Haim, 2015; Price et al., 2016). Trials in anxious youth are scarce (Eldar et al., 2012; Fitzgerald, Rawdon, & Dooley, 2016; Lowther & Newman, 2014), highlighting a need for more ABMT research in youth to gauge its efficacy. Pergamin-Hight, Pine, Fox, and Bar-Haim (2016) showed that compared to anxious adolescents, younger children derive less benefit from ABMT. This diminished benefit in younger children may reflect a still-developing capacity to engage the reaction time (RT)–based tasks used in most ABMT protocols (Chevalier & Blaye, 2016; Luna, Padmanabhan, & O’Hearn, 2010). Indeed, young children produce more errors and respond slower than adolescents on such tasks (Liu et al., 2014). Alternative ABMT procedures, better suited for the capacities of anxious young children, may enhance acceptability and efficacy.
Gaze-Contingent Music Reward Therapy (GC-MRT) is a novel ABMT based on gaze patterns rather than RTs (Lazarov, Pine, & Bar-Haim, 2017). Using eye-tracking technology and operant conditioning principles, GC-MRT increases patients’ dwelling on neutral over threat stimuli, with music serving as a reward. In GC-MRT, patients view matrices of threat and neutral faces while listening to their favorite music. The music plays only when patients direct their gaze toward neutral faces, ceasing when they focus on threat faces. A study in adult patients with social anxiety disorder (SAD) revealed greater reductions in symptoms following GC-MRT compared to a control condition in which music was not contingent upon gaze. Symptom reduction was partially mediated by reduction in dwell time on threat from pre- to posttreatment (Lazarov et al., 2017). These findings provided evidence for the efficacy of GC-MRT in anxious adults. We tested whether young children can comply with the demands of GC-MRT and whether it is acceptable to them and their parents. GC-MRT requires reduced cognitive-motor load relative to RT-based ABM procedures and incorporates listening to self-selected favorite music as a reward element (Blood & Zatorre, 2001; Saarikallio & Erkkilä, 2007), which may be more appropriate for younger samples. We evaluated compliance and acceptability of GC-MRT in anxious 7- to 10-year-olds, using an open-trial multiple-baseline design (Hawkins, Sanson-Fisher, Shakeshaft, D’Este, & Green, 2007). We also provide preliminary analyses of efficacy in cognitive target engagement and symptom reduction.
We expected that (a) GC-MRT would show satisfactory acceptability and credibility for patients and their parents, (b) GC-MRT would lead to reduction in dwell time on threat from pre- to posttherapy, and (c) GC-MRT would lead to a greater reduction in symptoms following treatment relative to the multiple-baseline period.
METHOD
Study Design
In this open trial with multiple baselines, patients received eight sessions of GC-MRT, twice a week over 4 weeks (Lazarov et al., 2017). Patients were randomly assigned to three waiting baseline conditions: 1, 3, or 5 weeks before treatment started (n = 4 per condition).
Participants
Following studies with similar design (e.g., Au et al., 2017; Shahar, Bar-Kalifa, & Alon, 2017), we recruited 12 anxious 7- to 10-year-olds (Mage = 8.3 years, SD = 0.72, range = 7–10; four girls). This age range is when anxiety disorders start to emerge (Kessler et al., 2005). The study was conducted between May 2017 and April 2018. Sixty-eight parents responded to advertisements on social media about a treatment study for anxious youth, of which 19 passed the initial telephone screen verifying the presence of SAD, generalized anxiety disorder (GAD), or separation anxiety (SA) symptoms per the Diagnostic and Statistical Manual of Mental Disorders (DSM–5; American Psychiatric Association, 2013) and were invited to an in-person clinical interview. These disorders are frequently comorbid in childhood and reflect recruitment parameters of previous clinical trials in youth (Beidel, Turner, & Morris, 1999; White et al., 2017). Six children did not meet inclusion criteria, and one could not commit to a therapy schedule. Inclusion criteria were (a) meeting DSM criteria of SAD, GAD, or SA and (b) normal or corrected-to-normal vision. Exclusion criteria were (a) inability to calibrate eye-tracking; (b) present or past diagnosis of organic mental disorder, psychotic disorder, pervasive developmental disorder, or mental retardation; (c) high likelihood of hurting self or others; and (d) concurrent psychosocial treatment. Table 1 lists age, gender, and diagnoses for each participant. No differences were noted in gender and age between the different baseline groups (p = .12 and p = .77, respectively). The local Institutional Review Board approved the study. Parents and children provided written informed consent/assent (Clinicaltrials.gov identifier: NCT03171363).
TABLE 1.
Age, Gender, and Diagnostic Status of Each of the 12 Participants
| Subject | Gender | Age | Diagnostic Status |
|---|---|---|---|
| 1 | M | 8 | SA, GAD |
| 2 | F | 8 | SA |
| 3 | M | 7 | SAD, SA, GAD |
| 4 | F | 9 | SA, GAD |
| 5 | M | 8 | SAD, SA, GAD |
| 6 | M | 9 | SA, GAD |
| 7 | M | 9 | SAD, SA |
| 8 | M | 8 | SA, GAD |
| 9 | F | 8 | SAD, SA |
| 10 | M | 9 | SAD, SA, GAD |
| 11 | M | 7 | SAD, SA, GAD |
| 12 | F | 9 | SA, GAD |
Note. SAD = Social Anxiety Disorder, SA = Separation Anxiety, GAD = General Anxiety Disorder, M = Male, F = Female.
Clinical Status
Diagnoses were ascertained using the Anxiety Disorders Interview Schedule–Child/Parent-IV administered separately to child and parent. This semistructured interview assesses child anxiety, mood, and externalizing disorders according to the DSM-IV (Silverman & Albano 1996). Clinical interviews were conducted by two clinical psychologists trained to 85% reliability with a senior psychologist. The clinician combined the information obtained from child and parent to determine diagnostic status. Supervision sessions were used to monitor diagnostic decisions.
Treatment Adherence and Credibility
We evaluated adherence to treatment by counting the number of sessions attended, noting whether the predetermined number of training trials was completed in each session and recording the time frame within which the protocol was completed. The Credibility/Expectancy Questionnaire (CEQ) was used at posttreatment to gauge treatment credibility. Children and parents used a 9-point scale to rate (a) how logical the treatment seemed, (b) how successful it was in treating symptoms, and (c) their confidence in recommending it to a friend (Devilly & Borkovec, 2000).
Anxiety Symptoms
The clinician-rated Pediatric Anxiety Rating Scale (PARS) was completed based on the clinical interviews. Each PARS item was scored as present or absent during the past week, with endorsed symptoms being further rated on five dimensions of severity (severity of distress, frequency, avoidance, interference at home, and interference out of home). We applied the five-item total score as recommended for clinical trials (Riddle, 2002). Each item was rated using a scale from 0 (no symptoms) to 5 (extreme symptoms). The PARS has adequate internal consistency and interrater reliability, sensitivity to change in treatment studies, and convergent validity (Ginsburg, Keeton, Drazdowski, & Riddle, 2011; Riddle, 2002).
The self-reported Screen for Child Anxiety Related Emotional Disorders–Child/Parent Version (SCARED-C/P; Birmaher et al., 1999) consists of 41 items describing anxiety symptoms rated on a 3-point scale. Separate child and parent SCARED total scores were used in analyses. The SCARED is internally reliable, is sensitive to change, and has demonstrated good convergent and divergent validity (Muris, Merckelbach, Ollendick, King, & Bogie, 2002). In the present sample, Cronbach’s alpha for SCARED-C was .89, .83, and .86 for Baseline 1, Baseline 2, and posttreatment assessments, respectively, and .77, .87, and .80 for SCARED-P assessments, respectively.
Threat-Related Gaze-Tracking Assessment
Gaze behavior was recorded using a RED500 eye-tracking system and analyzed with BeGaze software (SensoMotoric Instruments, Inc., Teltow, Germany). Sampling rate was 500 Hz. Operating distance to the monitor (22-in. Dell P2213, screen resolution = 1680 × 1050) was 70 cm. Each trial began with a centrally presented cross on which the child had to fixate for 1,000 ms to invoke the next display. Then, a 4 × 4 matrix (16 different faces) was presented for 6,000 ms. Each matrix consisted of eight neutral and eight disgusted faces. Disgusted facial expressions have been used in previous studies on pediatric anxiety (Benoit, McNally, Rapee, Gamble, & Wiseman, 2007; Shechner et al., 2014) and are considered powerful threat stimuli (Costafreda, Brammer, David, & Fu, 2008), to which anxious participants typically react to with higher Anterior Cingulate Cortex (ACC) and amygdala activation and faster emotion rating responses (Amir et al., 2005), relative to other facial expressions. Half the faces in a matrix were female, with the four inner faces always displaying two disgusted and two neutral faces. Face stimuli were taken from the Karolinska Directed Emotional Faces set (Lundqvist, Flykt, & Öhman, 1998) and divided into two sets (A and B). A patient assessed with set A was trained with set B, and vice versa, counterbalanced across participants. Participants look freely at each matrix until it disappeared. The assessment task comprised 30 trials with 2,000 ms intertrial intervals.
Two areas of interest (AOIs) were defined: the eight threat faces (threat AOI) and the eight neutral faces (neutral AOI). Total dwell time in milliseconds per AOI for each matrix was obtained, and the proportion of dwell time on the threat AOI relative to total dwell time in each matrix was calculated, reflecting the proportion of time a participant’s gaze was focused on threat. Average percentage dwell time on threat was computed across the 30 matrices. Cronbach’s alpha in this sample was .82 and .75 at pre- and posttreatment, respectively.
Gaze-Contingent Music Reward Therapy
GC-MRT used a modified version of the assessment task just described designed to divert patients’ attention toward the neutral faces and away from the threat faces. Treatment followed the protocol of Lazarov et al. (2017). Each session began with the patient selecting a 12-min music track of a performer they like and want to listen to during the session. Music tracks were selected from an extensive menu reflecting popular artists and hits according to YouTube statistics. Next, eye-tracking calibration was conducted, followed by presentation of the 30 faces-matrices (24 s each, without intertrial intervals). Patients heard their selected music only when fixating on the neutral AOI. When fixating the threat AOI, the music stopped. The treatment consisted of eight sessions delivered twice a week over 4 weeks.
The treatment task ran E-Prime, version 2 (Psychology Software Tools, Pittsburgh, PA). Eye-tracking parameters were the same as for the free viewing measurement task just described. Total dwell time for each AOI in each matrix was recorded, and the proportion of dwell time on the threat AOI relative to the total dwell time on each matrix was calculated for each matrix. An index of the average percentage of time participants dwelled on threat was computed across the 30 matrices.
Procedure
Parents were screened over the phone using questions reflecting DSM symptoms of SAD, GAD, and SA. Parents reporting an above cutoff number of symptoms for at least one of the diagnoses just listed (i.e., one symptom of SAD, one symptom of GAD, and three symptoms of SA, per DSM-5) while reporting substantial impairment or distress, were invited for a full in-clinic interview. Upon arrival at the university, parents and children received a thorough explanation of the study and provided written consent/assent. Then a clinical psychologist conducted separate interviews with the child and the parent using the Anxiety Disorders Interview Schedule–Child/Parent-IV and completing the PARS. Children and parents completed the SCARED. Those meeting inclusion criteria completed a baseline assessment 1 week later, which included the gaze-tracking assessment task and self-reported SCARED. Next, the 1-week baseline group commenced treatment. The other two groups completed the SCARED via an Internet link once a week during the waiting period. After 3 or 5 weeks (per allocation), patients and their parents were invited to a second baseline assessment, which included PARS, gaze-tracking assessment task, and SCARED. Following this second baseline, assessment treatment started. For all groups, GC-MRT consisted of eight 20-min sessions delivered twice a week over 4 weeks. Throughout the treatment, parents and children completed the SCARED once a week after their therapy session. One week after treatment completion, participants were invited for a posttreatment assessment including the same measures used in baseline assessments, and the CEQ.
Data Analysis
Descriptive statistics on treatment compliance and credibility are reported. Three paired t tests examine change in anxiety over time on the primary outcome (PARS), comparing (a) Baseline Assessment 1 and posttreatment, (b) Baseline Assessment 1 and Baseline Assessment 2, and (c) Baseline Assessment 2 and posttreatment.
To further examine treatment response, the multiple SCARED data collected during baseline and treatment were analyzed using the TAU-U test (Parker, Vannest, Davis, & Sauber, 2011). The TAU-U is a combination between Kendall’s Rank Correlation and the Mann–Whitney U test, uniquely created for single case designs to evaluate the difference between baseline and treatment phases (Parker, Vannest, & Davis, 2011). TAU-U examines the proportion of nonoverlapping data between stages (baseline vs. treatment), including all time points while controlling for baseline trends (e.g., a reduction in symptoms through the baseline period). TAU-U effect size for each participant was calculated, followed by an overall weighted average effect size combining data from all participants. This weighted average constitutes the proportion of data that are nonoverlapping between stages across all participants (Parker et al., 2011). TAU-U was calculated using the TAU-U calculator (http://www.singlecaseresearch.org/calculators/tau-u; Parker et al., 2011).
Finally, a repeated measures analysis of variance was used to evaluate change in percentaeg of dwell time on threat during treatment sessions (Sessions 1–8). In addition, we compared dwell time on threat at the very beginning of treatment and at the end of treatment. Following Lazarov et al. (2017), we calculated baseline dwell time on threat during the first five metrics of Session 1 and compared it to dwell time on threat during the final treatment session. To test for generalization of training to faces not used in training (near transfer) a paired t test comparing dwell time on threat from pre- to posttreatment was conducted.
In all analyses, alpha was set to .05, two-sided. Effect sizes are reported using eta-squared for analyses of variance and Cohen’s d for t tests. Corrections for multiple comparisons were performed using the Bonferroni correction method. Statistical procedures were performed in SPSS, version 24.0.
RESULTS
Treatment Compliance and Credibility
All 12 children completed the full course of GC-MRT (eight sessions, all trials) within the allocated time frame suggesting excellent tolerance and acceptability. Most children and parents found the treatment moderately to highly credible (see Table 2 for means, standard deviations, and ranges of the three CEQ subscales and total score). Nine children found GC-MRT highly credible (range = 7–9), two reported moderate credibility (range = 4–6), and one reported low credibility (range = 1–3). Parents reported high credibility for four participants, moderate credibility for six participants, and low credibility for one participant.
TABLE 2.
Means, SDs, and Ranges for Children and Parents Reported CEQ Items
| Child |
Parent |
|||||
|---|---|---|---|---|---|---|
| CEQ Item | M | SD | Range | M | SD | Range |
| (1) How logical does the therapy offered to you seem? | 6.9 | 2.2 | 2–9 | 6.6 | 1.4 | 5–9 |
| (2) How successfully do you think this treatment was in reducing your anxiety symptoms? | 6 | 3.1 | 1–9 | 5.4 | 2 | 2–8 |
| (3) How confident would you be in recommending this treatment to a friend who experiences similar problems? | 7 | 2.5 | 1–9 | 6.4 | 2.4 | 1–9 |
| Total score | 6.6 | 2.2 | 1.3–8.7 | 6.1 | 1.6 | 3–8.7 |
Note. CEQ = Credibility/Expectancy Questionnaire.
Clinician-Rated Anxiety
Paired t tests examining changes in PARS anxiety levels over time revealed (a) a reduction in anxiety from Baseline Assessment 1 to posttreatment, t(11) = 4.95, p < .001, d = 1.43; (b) no change from Baseline Assessment 1 to Baseline Assessment 2 for those who underwent a second baseline assessment, t(7) = −.28, p = .78, d = −.10; and (c) reduction in anxiety from Baseline Assessment 2 to posttreatment, t(7) = 3.16, p = .02, d = 1.12 (Table 3 for PARS means and standard deviations).
TABLE 3.
Means and SDs for PARS Scores at Each Assessment-Point by Group
| Baseline Assessment 1 | Baseline Assessment 2 | Post-Treatment | |
|---|---|---|---|
| 1-Week Baseline (n = 4) | 14 (3.55) | – | 9.75 (2.22) |
| 3-Week Baseline (n = 4) | 14 (2.00) | 14.25 (1.89) | 8.75 (1.26) |
| 5-Week Baseline (n = 4) | 15 (3.16) | 15 (4.89) | 11.25 (4.64) |
| Total | 14.33 (2.74) | 14.62 (3.46) | 9.92 (2.97) |
p < .05
Parent and Child Reported Anxiety
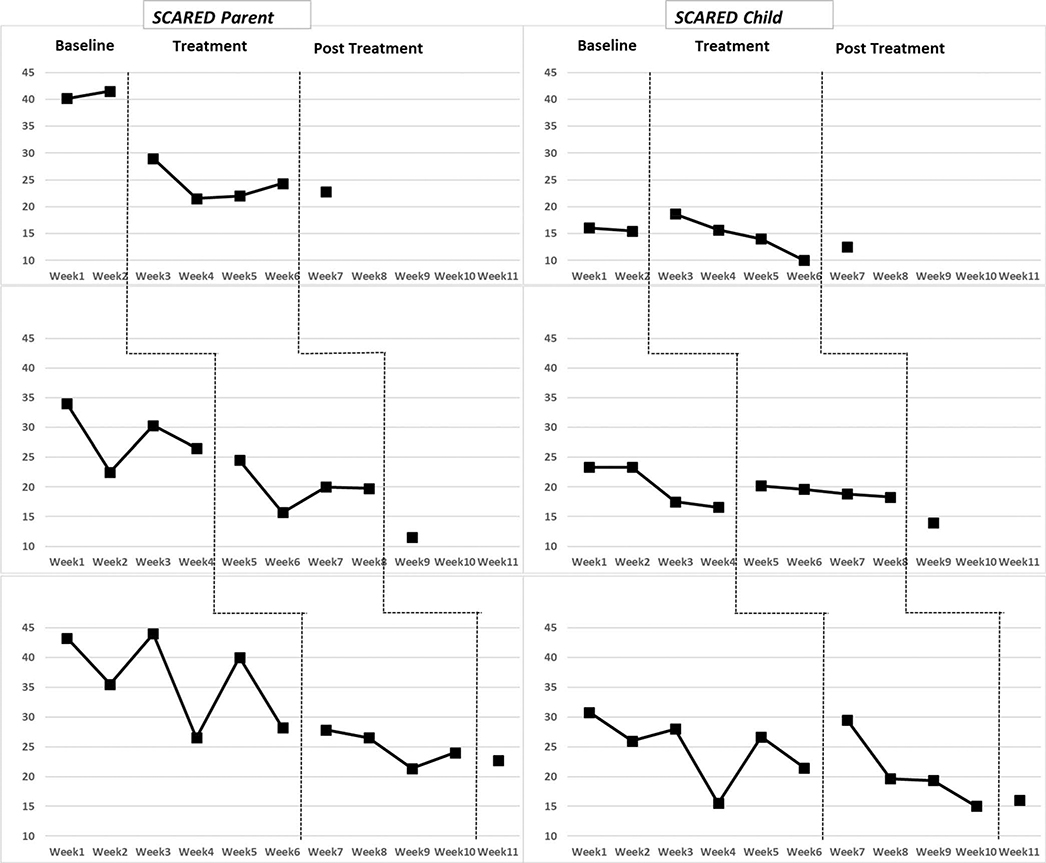
Parent and child SCARED scores are depicted in Figure 1. TAU-U analyses demonstrated declines from baseline through treatment and to posttreatment for parent-reported SCARED, TAU = −.68, p < .001, 95% confidence interval [−.98, −.37]. Changes in child-reported SCARED scores were nonsignificant, TAU = −.09, p = .56, 95% confidence interval [−.39, .21].
FIGURE 1.
Mean group scores for child and parent SCARED ratings across 1-week (n = 4), 3-week (n = 4) and 5-week (n = 4) baseline periods.
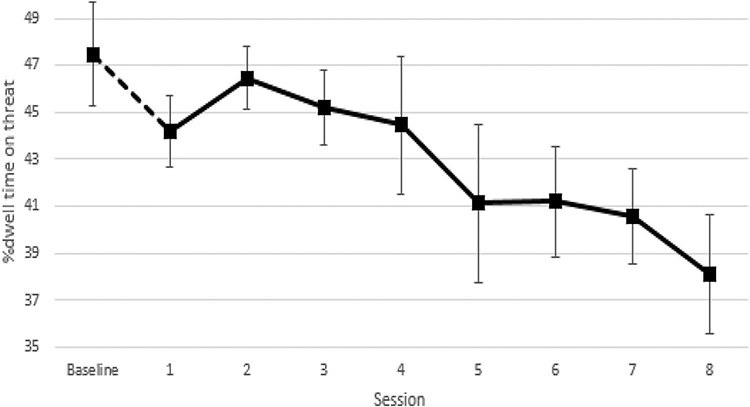
Change in Dwell Time on Threat
An overall reduction of 7.5% in dwell time on threat was noted from baseline (first five matrices) to the last therapy session. Nine of the 12 participants demonstrated gradual reduction in dwell time on threat across sessions and overall. One participant started with a very low and outlying (≥ 3 SDs) baseline dwell time on threat (22% relative to a mean of 46% in the current sample). Winsorizing the outlying measurements of this participant revealed a nonsignificant reduction in percentage of dwell time on threat over sessions, F(7, 77) = 1.82, p = .16, η2 = .14. Excluding this one outlying participant from analyses led to a significant effect, F(7, 70) = 2.91, p = .01, η2 = .23 (Figure 2). In addition, a nonsignificant 5% reduction in dwell time on threat was noted from pre- to posttreatment in the free viewing task, t(11) = 1.42, p = .18, d = .41. The correlations between change in percentage of dwell time on threat pre- to posttreatment and pre- to posttreatment changes in clinician rated and self-reported anxiety were r = .30, p = .35 and r = .39, p = .22, respectively.
FIGURE 2.
Percent dwell time on threat across therapy sessions. Bars indicate standard errors.
DISCUSSION
Feasibility and acceptability of GC-MRT for clinically anxious young children were examined here for the first time. All 12 children completed the full course of treatment and complied with all treatment demands, and both children and parents reported acceptable treatment credibility. It appears that GC-MRT may meet the unique needs of young anxious children and their parents in terms of treatment acceptability.
Our initial noncontrolled data also suggest meaningful reductions in anxiety from pre- to posttreatment. The multiple-baseline design revealed that clinician-rated and parent-reported anxiety remained stable during baseline and decreased from baseline to posttreatment, with 10 of 12 participants demonstrating substantial reductions in anxiety. However, child-reported anxiety did not change following treatment, apparently due to low baseline self-reported anxiety. Children’s self-reported anxiety was significantly lower than reported by parents and clinicians, consistent with prior data on informant discrepancies (De Reyes & Kazdin, 2005). Ratings in anxious children may be uniquely influenced by social desirability (Van De Mortel, 2008) or other cognitive factors (Vasey & MacLeod, 2001). Although diagnosed with a primary anxiety disorder by trained clinicians, children’s average baseline self-reported SCARED score in this study was lower than typical clinical cutoffs (Birmaher et al., 1999).
The small sample size and lack of control condition preclude clear deductions regarding cognitive target engagement. Although not significant, the data do suggest a trend of gradual reduction in dwell time on threat across sessions in most participants and, on average, a pattern that is highly similar to that found for anxious adults receiving GC-MRT (Lazarov et al., 2017). These preliminary results may serve as an initial indication for more robust mechanism-oriented studies to come of GC-MRT in youth.
The results of the current study should be considered in light of important limitations. First, evidence of efficacy, even with the applied multiple-baseline design, is still minimal. Robust evidence requires a larger RCT with adequate controls. Second, although the sample size used here is adequate for feasibility and acceptance testing, it has limited power to detect small or medium effects such as cognitive target engagement. Third, children reported lower levels of anxiety than parents or clinicians. Although this reporting pattern is common, it still suggests low levels of subjective anxiety in the studied patients, and thus generalizability might be limited to more severely anxious patients. Fourth, delineating normative threat-related gaze patterns in youth at different developmental stages could assist in anchoring the current findings relative to this broader context and advance insight into treatment mechanisms. Finally, future studies may wish to extend the testing of acceptability and efficacy of GC-MRT to other age ranges and examine alternative stimuli characteristics.
In sum, the present study indicates that GC-MRT can be effectively delivered to anxious youth. GC-MRT was well tolerated; compliance was excellent; and for most patients, anxiety symptoms reduced considerably from pre- to posttreatment. We hope that the current findings provide a compelling base for future RCTs of GC-MRT for pediatric anxiety that could test its efficacy as a stand-alone treatment as well as adjuvant for other treatments.
FUNDING
This research was supported by grant No. 2013349 from the United States-Israel Binational Science Foundation.
Footnotes
DISCLOSURE STATEMENT
No potential conflict of interest was reported by the authors.
Registration information
ClinicalTrials.gov identifier: (https://clinicaltrials.gov/ct2/show/NCT03171363).
REFERENCES
- American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (DSM-5). American Psychiatric Pub. [Google Scholar]
- Amir N, Klumpp H, Elias J, Bedwell JS, Yanasak N, & Miller LS (2005). Increased activation of the anterior cingulate cortex during processing of disgust faces in individuals with social phobia. Biological Psychiatry, 57(9), 975–981. doi: 10.1016/j.biopsych.2005.01.044 [DOI] [PubMed] [Google Scholar]
- Au TM, Sauer-Zavala S, King MW, Petrocchi N, Barlow DH, & Litz BT (2017). Compassion-based therapy for trauma-related shame and posttraumatic stress: Initial evaluation using a multiple baseline design. Behavior Therapy, 48(2), 207–221. doi: 10.1016/j.beth.2016.11.012 [DOI] [PubMed] [Google Scholar]
- Bar-Haim Y (2010). Research review: Attention bias modification (ABM): A novel treatment for anxiety disorders. Journal of Child Psychology and Psychiatry and Allied Disciplines, 51(8), 859–870. doi: 10.1111/j.1469-7610.2010.02251.x [DOI] [PubMed] [Google Scholar]
- Bar-Haim Y, Lamy D, Pergamin L, Bakermans-Kranenburg MJ, & Van IJzendoorn MH (2007). Threat-related attentional bias in anxious and nonanxious individuals: A meta-analytic study. Psychological Bulletin, 133(1), 1–24. doi: 10.1037/0033-2909.133.1.1 [DOI] [PubMed] [Google Scholar]
- Beesdo K, Knappe S, & Pine DS (2011). Anxiety and anxiety disorders in children and adolescents: Developmental issues and implications for DSM-V. Psychiatric Clinics of North America, 32(3), 483–524. doi: 10.1016/j.psc.2009.06.002.Anxiety [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beidel DC, Turner SM, & Morris TL (1999). Psychopathology of childhood social phobia. Journal of the American Academy of Child & Adolescent Psychiatry, 38(6), 643–650. doi: 10.1097/00004583-199906000-00010 [DOI] [PubMed] [Google Scholar]
- Benoit KE, McNally RJ, Rapee RM, Gamble AL, & Wiseman AL (2007). Processing of emotional faces in children and adolescents with anxiety disorders. Behaviour Change, 24(4), 183–194. doi: 10.1375/bech.24.4.183 [DOI] [Google Scholar]
- Birmaher B, Brent DA, Chiappetta L, Bridge J, Monga S, & Baugher M (1999). Psychometric properties of the screen for child anxiety related emotional disorders (SCARED): A replication study. Journal of the American Academy of Child and Adolescent Psychiatry, 38(10), 1230–1236. doi: 10.1097/00004583-199910000-00011 [DOI] [PubMed] [Google Scholar]
- Blood AJ, & Zatorre RJ (2001). Intensely pleasurable responses to music correlate with activity in brain regions implicated in reward and emotion. Proceedings of the National Academy of Sciences, 98(20), 11818–11823. doi: 10.1073/pnas.191355898 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chevalier N, & Blaye A (2016). Metacognitive monitoring of executive control engagement during childhood. Child Development, 87(4), 1264–1276. doi: 10.1111/cdev.12537 [DOI] [PubMed] [Google Scholar]
- Costafreda SG, Brammer MJ, David AS, & Fu CHY (2008). Predictors of amygdala activation during the processing of emotional stimuli: A meta-analysis of 385 PET and fMRI studies. Brain Research Reviews, 58(1), 57–70. doi: 10.1016/j.brainresrev.2007.10.012 [DOI] [PubMed] [Google Scholar]
- De Reyes ALL, & Kazdin AEE (2005). Informant discrepancies in the assessment of childhood psychopathology: A critical review, theoretical framework, and recommendations for further study. Psychological Bulletin, 131(4), 483–509. doi: 10.1037/0033-2909.131.4.483 [DOI] [PubMed] [Google Scholar]
- Devilly GJ, & Borkovec TD (2000). Psychometric properties of the credibility/expectancy questionnaire. Journal of Behavior Therapy and Experimental Psychiatry, 31(2), 73–86. doi: 10.1016/S0005-7916(00)00012-4 [DOI] [PubMed] [Google Scholar]
- Eldar S, Ph D, Apter A, Lotan D, Edgar KP, Fox NA, … BarHaim Y (2012). Attention bias modification treatment for pediatric anxiety disorders: A randomized controlled trial. American Journal of Psychiatry, (15), 213–220. doi: 10.1176/appi.ajp.2011.11060886 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fitzgerald A, Rawdon C, & Dooley B (2016). A randomized controlled trial of attention bias modification training for socially anxious adolescents. Behaviour Research and Therapy, 84, 1–8. doi: 10.1016/j.brat.2016.06.003 [DOI] [PubMed] [Google Scholar]
- Ginsburg GS, Keeton CP, Drazdowski TK, & Riddle MA (2011). The utility of clinicians ratings of anxiety using the Pediatric Anxiety Rating Scale (PARS). Child and Youth Care Forum, 40(2), 93–105. doi: 10.1007/s10566-010-9125-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hawkins NG, Sanson-Fisher RW, Shakeshaft A, D’Este C, & Green LW (2007). The multiple baseline design for evaluating population-based research. American Journal of Preventive Medicine, 33(2), 162–168. doi: 10.1016/j.amepre.2007.03.020 [DOI] [PubMed] [Google Scholar]
- Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, & Walters EE (2005). Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Archives of General Psychiatry, 62(6), 593–602. doi: 10.1001/archpsyc.62.6.593 [DOI] [PubMed] [Google Scholar]
- Lazarov A, Pine DS, & Bar-Haim Y (2017). Gaze-contingent music reward therapy for social anxiety disorder: A randomized controlled trial. American Journal of Psychiatry, 174(7), 649–656. doi: 10.1176/appi.ajp.2016.16080894 [DOI] [PubMed] [Google Scholar]
- Linetzky M, Pergamin-Hight L, Pine DS, & Bar-Haim Y (2015). Quantitative evaluation of the clinical efficacy of attention bias modification treatment for anxiety disorders. Depression and Anxiety, 32(6), 383–391. doi: 10.1002/da.22344 [DOI] [PubMed] [Google Scholar]
- Liu G, Chen DD, Qin C, Chan JSY, Peng K, & Yan JH (2014). Visuomotor control in continuous response time tasks across different age groups. Perceptual and Motor Skills, 119(1), 169–182. doi: 10.2466/25.10.PMS.119c13z8 [DOI] [PubMed] [Google Scholar]
- Lowther H, & Newman E (2014). Attention bias modification (ABM) as a treatment for child and adolescent anxiety: A systematic review. Journal of Affective Disorders, 168, 125–135. doi: 10.1016/j.jad.2014.06.051 [DOI] [PubMed] [Google Scholar]
- Luna B, Padmanabhan A, & O’Hearn K (2010). What has fMRI told us about the development of cognitive control through adolescence? Brain and Cognition, 72(1), 101–113. doi: 10.1016/j.bandc.2009.08.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lundqvist D, Flykt A, & Öhman A (1998). The Karolinska directed emotional faces (KDEF). CD ROM from Department of Clinical Neuroscience, Psychology Section, Karolinska Institutet, 91, 630. [Google Scholar]
- MacLeod C, & Clarke PJF (2015). The attentional bias modification approach to anxiety intervention. Clinical Psychological Science, 3(1), 58–78. doi: 10.1177/2167702614560749 [DOI] [Google Scholar]
- Muris P, Merckelbach H, Ollendick T, King N, & Bogie N (2002). Three traditional and three new childhood anxiety questionnaires: Their reliability and validity in a normal adolescent sample. Behaviour Research and Therapy, 40(7), 753–772. doi: 10.1016/S0005-7967(01)00056-0 [DOI] [PubMed] [Google Scholar]
- Parker RI, Vannest KJ, & Davis JL (2011). Effect size in single-case research: A review of nine nonoverlap techniques. Behavior Modification, 35(4), 303–322. doi: 10.1177/0145445511399147 [DOI] [PubMed] [Google Scholar]
- Parker RI, Vannest KJ, Davis JL, & Sauber SB (2011). Combining nonoverlap and trend for single-case research: Tau-U. Behavior Therapy, 42(2), 284–299. doi: 10.1016/j.beth.2010.08.006 [DOI] [PubMed] [Google Scholar]
- Pergamin-Hight L, Pine DS, Fox NA, & Bar-Haim Y (2016). Attention bias modification for youth with social anxiety disorder. Journal of Child Psychology and Psychiatry and Allied Disciplines, 57(11), 1317–1325. doi: 10.1111/jcpp.12599 [DOI] [PubMed] [Google Scholar]
- Price RB, Siegle GJ, Silk JS, Ladouceur C, McFarland A, Dahl RE, & Ryan ND (2013). Sustained neural alterations in anxious youth performing an attentional bias task: A pupilometry study. Depression and Anxiety, 30(1), 22–30. doi: 10.1002/da.21966 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Price RB, Wallace M, Kuckertz JM, Amir N, Graur S, Cummings L, … Bar-Haim Y (2016). Pooled patient-level meta-analysis of children and adults completing a computer-based anxiety intervention targeting attentional bias. Clinical Psychology Review, 50, 37–49. doi: 10.1016/j.cpr.2016.09.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rapee RM, Schniering CA, & Hudson JL (2009). Anxiety disorders during childhood and adolescence: Origins and treatment. Annual Review of Clinical Psychology, 5(1), 311–341. doi: 10.1146/annurev.clinpsy.032408.153628 [DOI] [PubMed] [Google Scholar]
- Riddle T (2002). The pediatric anxiety rating scale (PARS): Development and psychometric properties. Journal of the American Academy of Child and Adolescent Psychiatry, 41(9), 1061–1069. doi: 10.1097/00004583-200209000-00006 [DOI] [PubMed] [Google Scholar]
- Saarikallio S, & Erkkilä J (2007). The role of music in adolescents’ mood regulation. Psychology of Music, 35(1), 88–109. doi: 10.1177/0305735607068889 [DOI] [Google Scholar]
- Shahar B, Bar-Kalifa E, & Alon E (2017). Emotion-focused therapy for social anxiety disorder: Results from a multiple-baseline study. Journal of Consulting and Clinical Psychology, 85(3), 238–249. doi: 10.1037/ccp0000166 [DOI] [PubMed] [Google Scholar]
- Shechner T, Britton JC, Pérez-Edgar K, Bar-Haim Y, Ernst M, Fox NA, … Pine DS (2012). Attention biases, anxiety, and development: Toward or away from threats or rewards? Depression and Anxiety, 29(4), 282–294. doi: 10.1002/da.20914 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shechner T, Rimon-Chakir A, Britton JC, Lotan D, Apter A, Bliese PD, … Bar-Haim Y (2014). Attention bias modification treatment augmenting effects on cognitive behavioral therapy in children with anxiety: Randomized controlled trial. Journal of the American Academy of Child and Adolescent Psychiatry, 53(1), 61–71. doi: 10.1016/j.jaac.2013.09.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Silverman WK, & Albano AM (1996). The Anxiety disorders interview schedule for DSM-IV: Child and parent versions. San Antonia, TX: Psychological Corporation. [Google Scholar]
- Van De Mortel TF (2008). Faking it: Social desirability response bias in self- report research Faking it: Social desirability response bias in self-report research. Australian Journal of Advanced Nursing, 25(4), 40–48. Retrieved from http://www.ajan.com.au/ajan_25.4.htm [Google Scholar]
- Vasey MW, & MacLeod C (2001). Information-processing factors in childhood anxiety: A review and developmental perspective In Vasey MW, & Dadds MR (Eds.), The developmental psychopathology of anxiety (pp. 253–277). Oxford University Press. [Google Scholar]
- White LK, Sequeira S, Britton JC, Brotman MA, Gold AL, Berman E, … Bar-Haim Y (2017). Complementary features of attention bias modification therapy and cognitive-behavioral therapy in pediatric anxiety disorders. American Journal of Psychiatry, 174(8), 775–784. doi: 10.1176/appi.ajp.2017.16070847 [DOI] [PMC free article] [PubMed] [Google Scholar]