Abstract
Objective
The purpose of this study was to assess the reliability and validity of motion palpation and pain provocation compared with sacroiliac joint (SIJ) block as the gold-standard assessment method of patients with sacroiliac joint dysfunction (SIJD).
Methods
A cross-sectional study was conducted in the Department of Sports and Exercise Medicine at Rasool Akram Hospital. Forty-eight patients suspected of having SIJD were selected from a total of 150 patients on the basis of a combination of symptoms, physical tests, and magnetic resonance imaging findings. The patients suspected of having SIJD received the SIJ block, to which the accuracy of all the physical tests was compared. Sensitivity, specificity, and positive and negative predictive values were calculated for each test. The receiver operating characteristic curve and the area under the receiver operating characteristic curve were measured.
Results
The Flexion, Abduction and External Rotation (FABER) test had the highest specificity and positive predictive values of the physical tests. Furthermore, the combination of the FABER test and the thigh thrust test improved overall diagnostic ability more so than any of the other test combinations.
Conclusion
A combination of the motion and provocation tests increased specificity and positive predictive values, and the FABER test had the highest of these single values. The palpation tests did not change after the SIJ block, suggesting that their accuracy cannot be determined using this method.
Key Indexing Terms: Diagnostic Tests, Sensitivity and Specificity, Predictive Value of Tests
Introduction
Lower back pain (LBP) is one of the most common musculoskeletal complaints; almost 80% of people experience pain in this area at least once in their lives.1 Despite its high prevalence, the etiology of LBP is not well known and is nonspecific in approximately 85% of cases.2
The disorders affecting the sacroiliac joint (SIJ), which is an area extending inferiorly in the medial part of the posterior superior iliac spine (PSIS),3,4 are defined using different terms that include sacroiliac strain, sacroiliac instability, sacroiliac arthritis, and sacroiliac joint dysfunction (SIJD). The latter is used in the case of a noninflammatory condition of the SIJ that is characterized by a reversible decreased mobility of the joint, resulting from articular causes.5
Sacroiliac joint dysfunction accounts for 10% to 27% of the causes of mechanical lower back or buttock pain,6, 7, 8, 9, 10 and one of its hallmarks is local tenderness in the SIJ.5 Sacroiliac joint dysfunction can be the sole disorder, or it can be accompanied by disc herniation or spinal stenosis.11,12
It is difficult to make an exact diagnosis of SIJD, not only because historical, physical, or radiological evidence is not absolute, but also because the symptoms can be the result of other common conditions, such as facet syndrome and disc herniation.13, 14, 15, 16 Because there is no widely accepted reference standard for diagnosing SIJD, the SIJ block is the preferred method for this purpose.17 With this method, an anesthetic agent is injected into the SIJ under fluoroscopic guidance. The rationale for using the SIJ block is that the SIJ has many nerves, which, when stimulated, can generate pain. Moreover, the level of evidence for the specificity and validity of this diagnostic test is considered moderate (level III).6,18, 19, 20, 21, 22, 23, 24, 25, 26, 27, 28 A number of authors recommend single-injection diagnostic block for clinical studies,29,30 although others suggest double (confirmatory) diagnostic block more accurately determines the source of pain by using 2 different local anesthetics with different durations of action.5,13,18,31, 32, 33, 34, 35, 36, 37, 38, 39, 40, 41, 42
However, despite such recommendations, SIJ block is not cost-effective, nor is it practical for practitioners who lack training in intra-articular injections. These considerations have led clinicians to employ physical tests, with the belief that even negative findings can be used in diagnosing SIJD. The fact that there is a wide range of physical tests, many of which are not as accurate as the SIJ block,6,40,43, 44, 45, 46, 47, 48, 49 calls into question several factors, including which tests are most helpful, whether the lack of agreement on clinical criteria for an SIJD diagnosis makes utility of these tests controversial,14, 15, 16 and whether using a combination of such tests can lead to better diagnosis.
The present study aimed to determine which physical tests have the highest sensitivity, specificity, and predictive values in determining the presence of SIJD compared with the SIJ block, in addition to which combination of physical tests has the closest diagnostic value to the SIJ block.
Methods
This cross-sectional study was carried out between 2016 and 2018 and used convenience-based sampling to recruit patients with lower back or buttock pain. A written consent compatible with the International Council for Harmonisation of Technical Requirements for Pharmaceuticals for Human Use was obtained from all participants. Ethical approval for this study was obtained from an independent ethics committee at Iran University of Medical Sciences.
Patients with lower back or buttock pain were evaluated by a sports medicine specialist through a 2-step screening process. First, physical musculoskeletal examinations were used to identify patients who were subject to an SIJD diagnosis. Patients were then evaluated for pathologies of the lumbar spine and pelvis; those with pain in these areas that emanated from other causes, such as lumbar discopathy, spinal stenosis, and spondylolisthesis, were excluded. Eligible patients were subsequently evaluated using lumbosacral and sacroiliac magnetic resonance imaging (MRI) scans to rule out other sources of pain and to further verify the results of the physical examinations.
Inclusion Criteria
The following inclusion criteria were adopted during the physical examinations and screening:
-
•
Aged 20 to 70 years
-
•
Presence of lower back or buttock pain with or without radiation to lower extremities for at least 6 weeks before study enrollment
-
•
Presence of pain or local tenderness in the SIJ region (ie, the joint between the sacrum and the ilium bones of the pelvis, covering an area extending inferiorly in the medial part of the PSIS)
-
•
Presence of pain exacerbated as a result of bending laterally or backward
-
•
Positive results on at least 2 of the pain-provocation tests (ie, Flexion, Abduction, and External Rotation [FABER], thigh thrust, Gaenslen, Yeoman, compression, distraction, and Newton tests) and one of the motion palpation tests (ie, Gillet and forward flexion tests)
Exclusion Criteria
Patients were excluded if they met any of the following criteria:
-
•
Pregnancy
-
•
Receiving physical therapy modality and nonsteroidal anti-inflammatory drugs over a 72-hour period before the study period
-
•
A history of back surgery during the 6 months before the study period
-
•
Malignant tumors in the spine or pelvis
-
•
Sacroiliitis and infections of the SIJ
-
•
Presence of any fracture in the spine or pelvis
-
•
Presence of other causes of LBP such as lumbar discopathy and spinal stenosis discovered via clinical examination and MRI scanning
Generally, SIJD-suspected participants were defined as patients with lower back or buttock pain whose symptoms indicated SIJD and who had positive results on at least 2 of the pain provocation tests (ie, FABER, thigh thrust, Gaenslen, Yeoman, compression, distraction, and Newton tests) and 1 of the motion palpation tests (ie, Gillet and forward flexion tests) in the absence of other causes of pain according to MRI test results.
Background Data
Collected patient characteristics included sex, age, and body mass index (BMI). To determine the intensity of the SIJ pain felt during each subjective test, a 100-mm visual analog scale (VAS) was used, where 0 represented no pain and 100 denoted the most severe pain. The VAS scores were recorded mainly to measure the decline in pain level as a result of administering the SIJ block.
Motion Palpation Tests
Gillet Test
To perform the Gillet test, the examiner stood behind the patient with one thumb on the PSIS and the other thumb on the sacrum. Then, the patient was instructed to bend and pull up the leg corresponding to the PSIS being palpated. The test was repeated on the other side and compared bilaterally.
The test was considered negative if the thumb on the PSIS moved inferiorly to the thumb placed on the sacrum. In contrast, no movement on the PSIS or superior movement to the other thumb on the sacrum was taken as a positive result.45,50, 51, 52, 53
Forward Flexion Test
During the flexion test, the patient was asked to slowly bend forward as much as possible with the examiner's thumbs on their left and right PSIS. Then, the symmetry of the movement in the thumbs was assessed. A positive test result was defined as any superiority in the movement of the 2 thumbs, indicating hypomobility of the ipsilateral SIJ.44,53
Pain Provocation Tests (Subjective)
FABER Test (Patrick's Test)
During the FABER test, the patient was asked to lie supine on the examination table. The examiner brought the hip joint into the FABER positions. One knee was flexed 90°, and the affected-side foot was rested on the opposite-side knee. Subsequently, the examiner pressed the contralateral anterior superior iliac spine (ASIS) against the table and pushed the bent knee down toward the table.3,6 The test was considered positive if the patient felt pain in the SIJ on the side where the knee was flexed. At this point, pain in the buttocks was suggestive of SIJD, whereas pain in the inguinal region could have indicated hip pathology.
Thigh Thrust Test (Posterior Shear Test)
With the thigh thrust test, the patient lay in a supine position while the tested-side hip joint was flexed to approximately 90° by the examiner. An anteroposterior shear force was applied to the SIJ through the axis of the femur.3,43 Resulting pain indicated the test was positive.
Gaenslen Test
The patient lay supine, with the tested-side leg hanging over the edge of the table and the other leg flexed to the chest. The examiner applied firm pressure to the flexed knee, and a counterpressure was applied to the knee of the hanging leg. The procedure was then repeated on the opposite side.29,54 The test was considered positive if the patient felt pain in the hanging-leg side.
Yeoman Test
With this test, the patient was asked to lie prone. The examiner lifted the tested-side knee by extending it to 90° and then extended the hip joint with one elbow on the patient's buttock.3,47 Pain in the hanging-leg side was considered a positive result.
Compression Test
The patient lay in the lateral decubitus position, with the affected side up, and faced away from the examiner, who applied a downward pressure to the ipsilateral iliac crest and ASIS. The test was considered positive if the patient felt pain in the SIJ on the contralateral side.3,48
Distraction Test
The patient was placed supine on the table. With the patient's forearms crossed, the examiner applied slow and steady outward pressure to the left and right ASIS, spreading them away. The test was considered positive if the patient's pain in the SIJ increased.3,48,55
Newton's Test
The patient lay in a supine position. The examiner fully flexed and pressed the tested-side hip and knee joints toward the abdomen. The test was considered positive if the patient experienced increased pain in the SIJ. 3
SIJ Block (SIJ Injection)
Patients who met the criterion for positivity were suspected to have SIJD47 and were transferred to the pain procedure room within an hour for the double SIJ block. This test was performed by a pain specialist with more than 10 years of experience in spinal injections and who was blind to the results of the physical tests. For the SIJ block, the patient lay in a prone position with a pillow placed under the abdomen at the iliac crests. After prepping and draping, a spinal 22G needle was inserted and positioned in the SIJ. Next, 1 mL of iodixanol (Visipaque) was injected as the radiocontrast agent. The placement of the needle and the spread of iodixanol was documented via fluoroscopy (a lateral view and a 3-quarter view). Additionally, 1.5 mL of lidocaine 2% was used in the initial injection, and 1.5 mL of bupivacaine 0.5% was employed in the confirmatory block,5,6,18,26,31, 32, 33, 34, 35, 36, 37, 38, 39, 40, 41, 42 producing a double SIJ block within an hour of the SIJ block. The physical tests were repeated, and VAS pain scores were obtained again to measure possible pain relief compared with the pre-SIJ block state.27 A pain reduction of at least 60% indicated the presence of SIJD, and a reduction of smaller than 60% denoted the absence of SIJD.28,39,56
To measure the diagnostic validity of the physical tests, they were compared with the SIJ block in the SIJD-suspected patients. The comparison was performed for each individual test and different combinations.
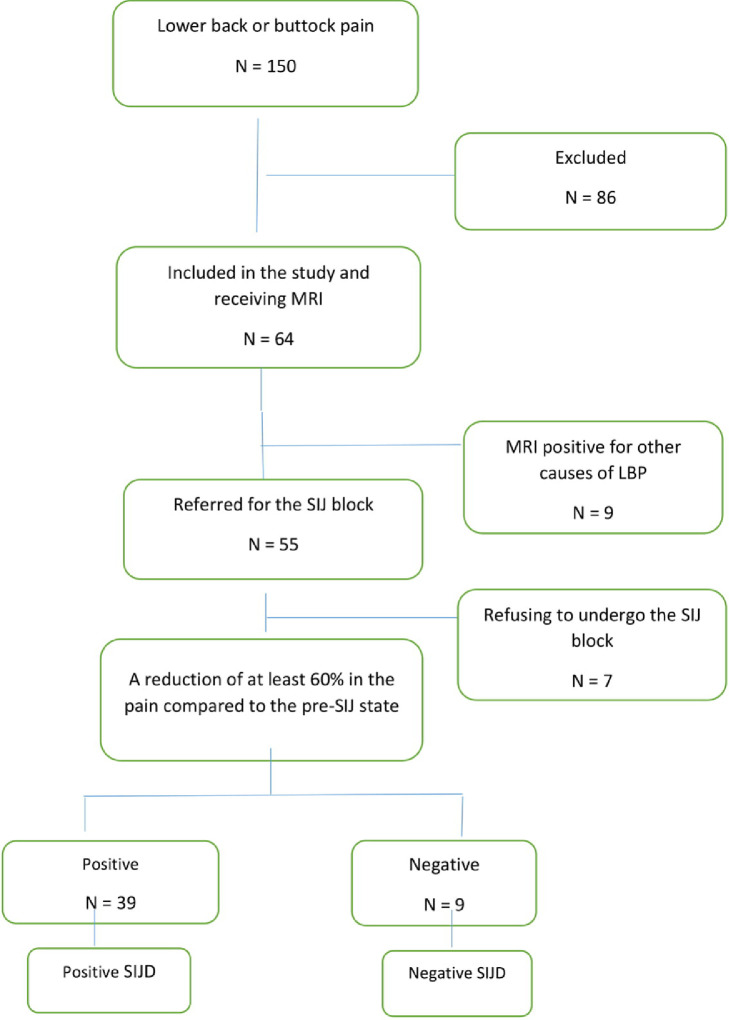
The flowchart of the study is presented in Figure 1.
Fig 1.
The flowchart of the study. LBP, lower back pain; MRI, magnetic resonance imaging; SIJ, sacroiliac joint.
Statistical Methods
The findings of the evaluations were analyzed using SPSS 23 (IBM Corporation, New York). The prevalence of SIJD in the patients with lower back or buttock pain was determined while considering their sex, age, and BMI. Also, 2 × 2 contingency tables were created. Moreover, sensitivity, specificity, and positive and negative predictive values were calculated for each individual test and different combinations of these tests based on the formulas presented in Table 1.57,58
Table 1.
Calculation of the Sensitivity, Specificity, and Positive and Negative Predictive Values of the Diagnostic Tests
| Positive SIJ Block | Negative SIJ Block | |
|---|---|---|
| Positive physical test | A (true positive) | B (false positive) |
| Negative physical test | C (false negative) | D (true negative) |
Sensitivity = (A/(A + C)) × 100
Specificity = (D/(B + D)) × 100
Positive Predictive Value = (A/(A + B)) × 100
Negative Predictive Value = (D/(C + D)) × 100
The receiver operating characteristic curve is an overall measure of diagnostic efficacy. It is a plot of the true-positive rate against the false-positive rate of a diagnostic test. This curve, which is defined as a plot of test sensitivity as the y coordinate vs test specificity or false-positive rate as the x coordinate, is an effective method for evaluating the validity of diagnostic tests.
The area under the curve (AUC) is the area under the receiver operating characteristic curve and a measure of how well a parameter can distinguish between 2 diagnostic groups (affected vs non-affected). The AUC can range from 0.5 (useless model) to 1.0 (perfect discrimination). A value higher than 0.7 can be interpreted as reasonable or fair; a value higher than 0.8 is considered acceptable.57 The surface of the curve was calculated and measured using SPSS.
Results
A total of 150 patients with lower back or buttock pain were examined at the beginning of the study. Sixty-four of these patients were selected to undergo an MRI. Of them, 9 patients were excluded as their LBP was the result of other causes. Further, 7 patients refused to undergo the SIJ block. Of the 48 remaining patients, 6 were male and 42 were female, ranging in age from 23 to 69 years old (average of 47.7 years) and a mean BMI of 28.4.
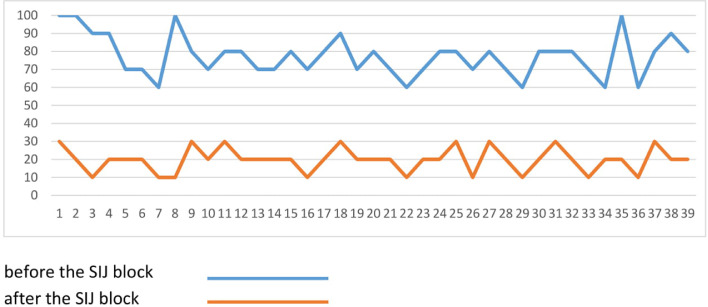
Of the 48 patients undergoing the SIJ block, 39 experienced a reduction of at least 60% in pain and were placed in the SIJD-positive group, for a prevalence of 81.25%. Although the pre-SIJ block VAS scores ranged from 60 to 100, with an average of 77, the post-SIJ block scores varied between 10 and 30, with an average of 18 (Fig 2). No adverse effects of the SIJ block were observed.
Fig 2.
VAS scores before and after the SIJ block in SIJD-positive patients. SIJD, sacroiliac joint dysfunction; VAS, visual analog scale.
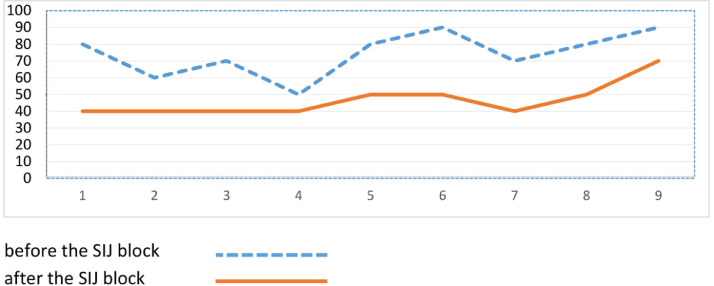
Nine patients had a reduction in pain that was less than 60% after the SIJ block and were assigned to the SIJD-negative group. Of these patients, the pre-SIJ block VAS scores ranged from 50 to 90, with an average of 74, whereas the post-SIJ block scores ranged from 40 to 70, with the average being 46 (Fig 3).
Fig 3.
VAS scores before and after the SIJ block in SIJD-negative patients. SIJD, sacroiliac joint dysfunction; VAS, visual analog scale.
Tables 2 and 3 show the sensitivity, specificity, and positive and negative predictive values for each individual physical test and different combinations of these tests, respectively. The FABER test had the highest specificity and positive predictive values.
Table 2.
Sensitivity, Specificity, and Positive and Negative Predictive Values for Each Physical Test
| FABER Test | Thigh Thrust Test | Gaenslen Test | Yeoman Test | Gillet Test | Forward Flexion Test | |
|---|---|---|---|---|---|---|
| Sensitivity (%) | 71.8 | 74.4 | 61.5 | 64.1 | 100 | 100 |
| Specificity (%) | 66.7 | 44.4 | 33.3 | 33.3 | 0 | 0 |
| PPV (%) | 90.3 | 85.3 | 80 | 80.6 | 81 | 81 |
| NPV (%) | 35.3 | 28.6 | 16.7 | 17.6 | - | - |
FABER, Flexion, Abduction and External Rotation; NPV, negative predictive value; PPV, positive predictive value.
Table 3.
Sensitivity, Specificity, and Positive and Negative Predictive Values for Different Combinations of Physical Tests
| Three or More Positive Tests | Four or More Positive Tests | Five or More Positive Tests | |
|---|---|---|---|
| Sensitivity (%) | 94.9 | 92.3 | 59 |
| Specificity (%) | 11.1 | 22.2 | 55.5 |
| PPV (%) | 82.2 | 83.7 | 85.1 |
| NPV (%) | 33.3 | 40 | 23.8 |
NPV, negative predictive value; PPV, positive predictive value.
Tables 4 and 5 present the distribution of the positivity of each individual physical test and different combinations of these tests, respectively, in SIJD-positive and SIJD-negative patients.
Table 4.
The Positivity of Each Physical Test in SIJD-Positive and SIJD-Negative Patients
| Test | SIJD-Positive | SIJD-Negative | |
|---|---|---|---|
| FABER test | Positive | 28 | 3 |
| Negative | 11 | 6 | |
| Thigh thrust test | Positive | 29 | 5 |
| Negative | 10 | 4 | |
| Gaenslen test | Positive | 15 | 6 |
| Negative | 24 | 3 | |
| Yeoman test | Positive | 25 | 6 |
| Negative | 14 | 3 | |
| Gillet test | Positive | 39 | 9 |
| Negative | 0 | 0 | |
| Forward flexion test | Positive | 39 | 9 |
| Negative | 0 | 0 | |
FABER, Flexion, Abduction, and External Rotation; SIJD, sacroiliac joint dysfunction.
Table 5.
The Positivity of Different Combinations of Physical Tests in SIJD-Positive and SIJD-Negative Patients
| Combinations of Physical Tests | SIJD-Positive | SIJD-Negative |
|---|---|---|
| Fewer than 3 positive tests | 0 | 0 |
| Three or more positive tests | 37 | 8 |
| Fewer than 4 positive tests | 3 | 2 |
| Four or more positive tests | 36 | 7 |
| Fewer than 5 positive tests | 16 | 5 |
| Five or more positive tests | 23 | 4 |
| Fewer than 6 positive tests | 29 | 8 |
| Six positive tests | 10 | 1 |
SIJD, sacroiliac joint dysfunction.
The results for dual combinations of pain provocation tests are shown in Table 6. A combination of FABER and thigh thrust tests showed the highest improvement in the overall diagnostic power (as measured by improvement in the AUC). More specifically, this combination resulted in an AUC of 69.2%, a sensitivity value of 71.7%, and a specificity value of 66%.
Table 6.
Sensitivity, Specificity, and Positive and Negative Predictive Values and AUC Levels in Dual Combinations of Provocative Tests
| FABER and Thigh Thrust | FABER and Gaenslen | FABER and Yeoman | Thigh Thrust and Gaenslen | Thigh Thrust and Yeoman | Gaenslen and Yeoman | |
|---|---|---|---|---|---|---|
| Sensitivity (%) | 71.7 | 48.71 | 43.58 | 48.71 | 43.58 | 35.89 |
| Specificity (%) | 66 | 77.77 | 66.66 | 66.66 | 55.55 | 55.55 |
| PPV (%) | 90.32 | 90.47 | 85 | 86.36 | 80.95 | 15.66 |
| NPV (%) | 35.29 | 25.92 | 21.42 | 23.07 | 18.51 | 77.7 |
| AUC | 69.2% | 63.2 | 55.1 | 57.7 | 49.6 | 45.7 |
AUC, area under the curve; FABER, Flexion, Abduction, and External Rotation; NPV, negative predictive value; PPV, positive predictive value.
Discussion
The findings of this study revealed that the positive predictive values of the provocation tests were high (larger than 80%) and the sensitivity values of these tests exceeded 60%. Moreover, the thigh thrust test was the most sensitive (74.4%), and the FABER test was the most specific (66.7%).
Studies on the accuracy of the FABER test have been inconsistent in their findings. For example, our study found its specificity to be 66.7%, but Dreyfuss et al45 reported a 16% specificity for this test. This significant difference can be attributed to that not only did the authors consider a reduction of larger than 90% in VAS scores as SIJD-positive but also administered a single injection of a local anesthetic and a corticosteroid with long-term effectiveness. Similarly, Broadhurst et al59 report a 100% specificity of the FABER test. This is the result of the pain relief criterion used, which was lower and thus more lenient in the current study, and also that they injected the patients who had a positive FABER test and not those with a negative FABER result.59
Although we observed a sensitivity value of 71.8% for the FABER test, Broadhust et al59 reported this value to be 77% when the diagnostic criterion had been set at a reduction of 70% in pain, but found a sensitivity of 50% when the criterion was 90% pain relief. In contrast, this test had a lower sensitivity (57%) than in the studies by van der Wurff et al,60,61 because the SIJ was injected blindly; blocking under fluoroscopic guidance can increase sensitivity by raising the probability of infiltration into the SIJ.
In this study, the positive and negative predictive values of the FABER test were 90.3 and 35.3%, respectively. In the review article by Cattley et al,52 the FABER test was referred to as an unreliable and invalid test in SIJD diagnosis. The authors cited methodological quality, technique application, and VAS pain parameters as reasons for this.
The thigh thrust test had a sensitivity of 74.4% and a specificity of 44.4% in our study. The sensitivity and specificity of this test were 36% and 50%, respectively, in Dreyfuss et al.45 Broadhurst et al59 reported a sensitivity value of 80% with the pain relief criterion having been set at 70%, and a sensitivity of 69% using a pain relief criterion of 90%. In both cases, study authors observed a specificity value of 100%. The sensitivity, specificity, and positive and negative predictive values obtained in the study by Laslett et al13 for the thigh thrust test were 50%, 69%, 58%, and 92%, respectively, using a pain reduction threshold of 80%. The larger cutoff value was associated with a lower reported sensitivity; however, to reduce the probability of false positivity, it is better to use a cutoff value that is as close to 100% as possible in all of the physical tests.
The Gaenslen's test had a sensitivity value of 61.5% and a specificity value of 33.3% in our study. The sensitivity, specificity, and positive and negative predictive values found in Laslett et al13 for this test were 37%, 71%, 47%, and 76%, respectively. The specificity of this test in the study by Broadhurst59 was reported as 100%, which may be attributed to the use of a different protocol (eg, setting a higher cutoff and the injection of 4 cc of lidocaine being restricted to patients with a positive result on the Gaenslen's test).
Regarding the other tests, the observed discrepancies between the studies may be due to the adoption of different executive approaches. A review of the existing literature indicates that studies have used various thresholds of pain reduction after the SIJ block, ranging from 50% to 90%. For instance, Polly56 and van der Wurff60 used a 50% pain reduction as a diagnostic criterion for SIJD, but Irwin et al26 set a pain reduction of 70% after administering the confirmatory SIJ block. Schwarzer et al62 employed a single-injection SIJ block and set a threshold of 75% reduction in pain; Maigne et al6 used a reduction of 75% but with a double block. Slipman et al18 and Young et al63 used a reduction of 80% in pain after a single block. Lastly, Dreyfuss et al45 used a single injection of a local anesthetic and corticosteroids, in addition to pain provocation tests, and adopted a threshold of 90% reduction in pain severity. In the present study, the threshold was set at 60% because all of the SIJD-suspected patients received the double block and this study used established, stringent inclusion criteria for identifying SIJD-suspected patients, believing that these measures can justify a threshold lower than those set in more lenient studies.28 Indeed, studies that only used pain reduction without any other diagnostic criteria had to set a higher threshold for diagnosing positive SIJD.19,41,46,59
Some studies used the single block,18,19,59 whereas others5,6,13,26,39,42,64 (including the current study) adopted the double block approach. This study used the double block because it has been demonstrated that the prevalence of SIJ pain is estimated to range between 10% and 38% using a double block paradigm, whereas the false-positive rate of the single block is 20% to 54%.28
Additionally, in some studies,4 corticosteroids were injected instead of or in combination with lidocaine,19 which can influence the results of the SIJ block. More specifically, corticosteroids have a delayed onset of action but can reduce pain more effectively than lidocaine, which results in almost instant pain relief.65
Although the SIJ block is considered the gold standard in the diagnosis of SIJD, in 20% or sometimes up to 50% of cases, the SIJ block yields false-positive results, which can overestimate the sensitivity of the alternative diagnostic tools.16,28,66,67,68 These false results are caused by the extravasation of the locally injected anesthetic to the surrounding structures, such as ligaments, muscles, and lumbosacral nerve roots, potential sources of pain. The vertical position of the SIJ makes this joint prone to the leakage of the anesthetic, and leakage may occur regardless of the type of SIJ block (eg, fluoroscopy, computed tomography scan, sonography, and MRI) employed.28 Thus, gathering supplemental forms of evidence through multiple tests can help to diagnose SIJD more reliably.
According to the findings of this study, a combination of the motion and provocation tests increased specificity and positive predictive values but decreased sensitivity and negative predictive values. This is particularly considerable if there are several tests being combined. Furthermore, a combination of 3 or more positive provocation tests plus at least 1 positive motion palpation test produced the best results.
Laslett et al40 showed that patients with a positive diagnostic SIJ block are at least 3 × and as much as 20 × as likely to have had a combination of 3 or more positive provocative tests than patients with a negative SIJ block. Similarly, Laslett et al13 found that the positivity of 2 of 4 tests (ie, distraction, compression, thigh thrust, or sacral thrust) or 3 or more provocation-motion tests were the best predictors of a positive SIJ block.
In the present study, a combination of FABER and thigh thrust tests was more accurate than any other combination. The next most accurate results were obtained from a combination of FABER and Gaenslen tests. Because FABER and thigh thrust tests had the highest sensitivity and specificity values (see Table 2), it seems reasonable to use a combination of these 2 tests for SIJD diagnosis.
Here, Gillet and forward flexion tests had a sensitivity value of 100% and 0 specificity. This is owing to the inclusion of patients with at least 1 positive palpation test in accordance with our eligibility criteria. It turned out that Gillet and forward flexion tests were both positive in all of the included patients. The positive predictive value of both these tests was 81%.
It was also found that the results of neither the Gillet test nor the forward flexion test changed after the SIJ block. This was because these tests indicate mobility of the ilium and the sacrum and are not influenced by the SIJ block. It seems that in SIJD cases without a biomechanical disturbance, these motion tests are not necessarily positive and also may be positive in patients without SIJD.3,50 Thus, it is reasonable to use a combination of provocation tests and motion palpation tests for SIJD diagnosis.
In contrast, Dreyfuss et al69 showed the false positivity of motion tests by observing that they were positive in 20% of asymptomatic patients. They also found that the sensitivity and specificity of the standing flexion and Gillet tests were poor19 because they were compared with the SIJ block as the gold standard. In this regard, other studies70,71 compared motion tests with provocation tests and showed that agreement ranged from 67% to 97% for pain provocation tests but was 48% for palpation tests. Furthermore, kappa values varied between 0.43 and 0.84 for provocation tests but were –0.06 for palpation tests. Vanelderen et al also expressed that in the presence of a weak predictive value of provocation tests, combined batteries of physical tests can help ascertain SIJD diagnosis.72 Hence, it can be concluded that joint hypomobility leading to positive motion tests does not mean a patient has SIJD, but the positivity of at least 3 provocation tests and at least 1 motion test increases the predictivity of SIJD. Among the provocation tests, a combination of FABER and thigh thrust tests was more successful in diagnosing SIJD. The authors believe that a combination of physical tests in addition to patient history findings and clinical data can compensate for the low diagnostic power of these tests.
Limitations
A major limitation of the present study is that the adoption of at least 1 positive palpation test as a diagnostic criteria resulted in the 0 specificity of the palpation tests in SIJD-negative patients. Another limitation is the low cutoff point (60%) in pain reduction. If this point was more than 60%, this may have resulted in lower sensitivity in each test. If the number of participants and thus the number of SIJ blocks was higher, there could have been various results regarding the accuracy of the physical tests.
Conclusion
This study found that the FABER test had the highest single specificity and positive predictive values of all of the provocation tests under discussion. Further, a combination of the FABER and thigh thrust tests improved the overall diagnostic power. In addition, greater numbers of positive physical tests contribute more to an SIJD diagnosis. It is also recommended that at least 3 provocation tests be used in addition to motion palpation tests when confirming an SIJD diagnosis. Finally, as the existing literature reports inconclusive findings for the use of individual physical tests, it is advisable to use a combination of such tests in conjunction with other sources of data, including patient history, symptoms, and imaging, to diagnose SIJD.
Funding Sources and Conflicts of Interest
Funding of the SIJ block and diagnostic fluoroscopy of the patients was paid by Iran University of medical sciences. The authors do not have any conflict of interest.
Contributorship Information
Concept development (provided idea for the research): P.N.
Design (planned the methods to generate the results): P.N., F.I.
Supervision (provided oversight, responsible for organization and implementation, writing of the manuscript): P.N., F.I.
Data collection/processing (responsible for experiments, patient management, organization, or reporting data): E.S., M.S.
Analysis/interpretation (responsible for statistical analysis, evaluation, and presentation of the results): E.S., L.N.
Literature search (performed the literature search): E.S.,R.M.
Writing (responsible for writing a substantive part of the manuscript): P.N., E.S., L.N.
Critical review (revised manuscript for intellectual content, this does not relate to spelling and grammar checking): P.N., F.I., M.S.
Other (list other specific novel contributions): R.M. (reporting the MRI of the patients)
Practical Applications.
-
•
In this study, using 2 palpation tests of Gillet and forward flexion was not suitable for diagnosing sacroiliac joint dysfunction.
-
•
The prevocational tests were more reliable than the Gillet and forward flexion that are a marker of anterior rotation of ilium on the sacrum.
-
•
The combination of the provocative tests had more sensitivity than each test solitarily.
Alt-text: Unlabelled box
References
- 1.Krismer M, van Tulder M. Low back pain (non-specific) Best Pract Res Clin Rheumatol. 2007;21(1):77–91. doi: 10.1016/j.berh.2006.08.004. [DOI] [PubMed] [Google Scholar]
- 2.Ehrlich GE, Chaltaev NG. World Health Organization, Department of Noncommunicable Disease Management; 1999. Low back pain initiative. [Google Scholar]
- 3.Chi B. Sacroiliitis. In: Warfield CA, Fausett HJ, editors. Manual of Pain Management. 2nd ed. Lippincott Williams and Wilkins; Philadelphia, PA: 2002. pp. 95–98. [Google Scholar]
- 4.Katz V, Schofferman J, Reynolds J. The sacroiliac joint: a potential cause of pain after lumbar fusion to the sacrum. J Spinal Disord Tech. 2003;16(1):96–99. doi: 10.1097/00024720-200302000-00015. [DOI] [PubMed] [Google Scholar]
- 5.Ombregt L. Clinical examination of the sacroiliac joint. In: Ombregt L, editor. A System of Orthopaedic Medicine. 3rd ed. London, UK: Churchill Livingstone; 2013. pp. 595–600. [Google Scholar]
- 6.Hoy D, Brooks P, Blyth F, Buchbinder R. The epidemiologyof low back pain. Best Pract Res Clin Rheumatol. 2010;24(6) doi: 10.1016/j.berh.2010.10.002. 769-681. [DOI] [PubMed] [Google Scholar]
- 7.Manchikanti L, Singh V, Pampati V. Evaluation of the relative contributions of various structures in chronic low back pain. Pain Physician. 2001;4(4):308–316. [PubMed] [Google Scholar]
- 8.Maigne JY, Aivakiklis A, Pfefer F. Results of sacroiliac joint double block and value of sacroiliac pain provocation test in 54 patients with low back pain. Spine (Phila Pa 1976) 1996;21(16):1889–1892. doi: 10.1097/00007632-199608150-00012. [DOI] [PubMed] [Google Scholar]
- 9.Nejati P, Safarcherati A, Karimi F. Effectiveness of exercise therapy and manipulation on sacroiliac joint dysfunction: a randomized controlled trial. Pain Physician. 2019;22(1):53–61. [PubMed] [Google Scholar]
- 10.Nejati P, Karimi F, Safarcherati A. The effect of manipulation in sacroiliac joint dysfunction. J Isfahan Med School. 2016;34(402):1218–1224. [Google Scholar]
- 11.Schmid HJA. Iliosacrale diagnose und Behandlung 1978-1982. Man Med. 1985;23:101–108. [Google Scholar]
- 12.Bernard TN, Kirkaldy-Willis WH. Recognizing specific characteristics of nonspecific low back pain. Clin Orthop. 1987;217:266e280. [PubMed] [Google Scholar]
- 13.Laslett M, Aprill CN, McDonald B, Young SB. Diagnosis of sacroiliac joint pain: a validity of individual provocation tests and composites of tests. Man Ther. 2005;10(3):207–218. doi: 10.1016/j.math.2005.01.003. [DOI] [PubMed] [Google Scholar]
- 14.Laslett M, McDonald B, Tropp H, Aprill CN, Oberg B. Agreement between diagnoses reached by clinical examination and available reference standards: a prospective study of 216 patients with lumbopelvic pain. BMC Musculoskelet Disord. 2005;6:28. doi: 10.1186/1471-2474-6-28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Tong HC, Heyman OG, Lado DA, Isser MM. Interexaminer reliability of three methods of combining test results to determine side of sacral restriction, sacral base position, and innominate bone position. J Am Osteopath Assoc. 2006;106(8):464–468. [PubMed] [Google Scholar]
- 16.Hansen HC, McKenzie-Brown AM. Sacroiliac joint interventions: a systematic review. Pain Physician. 2007;10(1):165–184. [PubMed] [Google Scholar]
- 17.Laslett M. Evidence-based diagnosis and treatment of the painful sacroiliac joint. J Man Manip Ther. 2008;16(3):142–152. doi: 10.1179/jmt.2008.16.3.142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.18Manchikanti L, Boswell MV, Singh V, Hansen HC. Sacroiliac joint pain: should physicians be blocking lateral branches, medial branches, dorsal rami, or ventral rami? Reg Anesth Pain Med. 2003;28(5):490–491. doi: 10.1016/s1098-7339(03)00391-2. [DOI] [PubMed] [Google Scholar]
- 19.McKenzie-Brown AM, Shah RV, Sehgal N, Everett CR. A systematic review of sacroiliac joint interventions. Pain Physician. 2005;8(1):115–126. [PubMed] [Google Scholar]
- 20.Cohen SP. Sacroiliac joint pain: a comprehensive review of anatomy, diagnosis and treatment. Anesth Analg. 2005;101(5):1440–1453. doi: 10.1213/01.ANE.0000180831.60169.EA. [DOI] [PubMed] [Google Scholar]
- 21.Foley BS, Buschbacher RM. Sacroiliac joint pain: anatomy, biomechanics, diagnosis, and treatment. Am J Phys Med Rehabil. 2006;85(12):997–1006. doi: 10.1097/01.phm.0000247633.68694.c1. [DOI] [PubMed] [Google Scholar]
- 22.Forst SL, Wheeler MT, Fortin JD, Vilensky JA. The sacroiliac joint: anatomy, physiology and clinical significance. Pain Physician. 2006;9(1):61–68. [PubMed] [Google Scholar]
- 23.Hansen HC, Helm S. Sacroiliac joint pain and dysfunction. Pain Physician. 2003;6(2):179–189. [PubMed] [Google Scholar]
- 24.Boswell MV, Shah RV, Everett CR. Interventional techniques in the management of chronic spinal pain: evidence-based practice guidelines. Pain Physician. 2005;8(1):1–47. [PubMed] [Google Scholar]
- 25.Zelle BA, Gruen GS, Brown S, George S. Sacroiliac joint dysfunction: evaluation and management. Clin J Pain. 2005;21(5):446–455. doi: 10.1097/01.ajp.0000131413.07468.8e. [DOI] [PubMed] [Google Scholar]
- 26.Irwin RW, Watson T, Minick RP, Ambrosius WT. Age, body mass index, and gender differences in sacroiliac joint pathology. Am J Phys Med Rehabil. 2007;86(1):37–44. doi: 10.1097/phm.0b013e31802b8554. [DOI] [PubMed] [Google Scholar]
- 27.Merskey H, Bogduk N. Classification of chronic pain. In: Merskey H, Bogduk N, editors. Descriptions of Chronic Pain Syndromes and Definition of Pain Terms. 2nd ed. IASP Press; Seattle, WA: 1994. pp. 180–181. [Google Scholar]
- 28.Rupert MP, Lee M, Manchikanti L, Datta S, Cohen SP. Evaluation of sacroiliac joint interventions: a systematic appraisal of the literature. Pain Physician. 2009;12(2):399–418. [PubMed] [Google Scholar]
- 29.Slipman CW, Jackson HB, Lipetz JS. Sacroiliac jointpain referral zones. Arch Phys Med Rehabil. 2000;81(3):334–338. doi: 10.1016/s0003-9993(00)90080-7. [DOI] [PubMed] [Google Scholar]
- 30.Dreyfuss MD. Practice guidelines and protocols for sacroiliac joint blocks. Paper presented at: International Spine Intervention Society 9th Annual Scientific Meeting; San Francisco, CA; 2001. [Google Scholar]
- 31.Murata Y, Takahashi K, Yamagata M, Takahashi Y, Shimada Y, Moriya H. Origin and pathway of sensory nerve fibers to the ventral and dorsal sides of the sacroiliac joint in rats. J Orthop Res. 2001;19(3):379–383. doi: 10.1016/S0736-0266(00)90017-2. [DOI] [PubMed] [Google Scholar]
- 32.Fortin JD, Kissling RO, O'Connor BL, Vilensky JA. Sacroiliac joint innervation and pain. Am J Orthop. 1999;28(12):687–690. [PubMed] [Google Scholar]
- 33.Grob KR, Neuhuber WL, Kissling RO. Innervation of the sacroiliac joint of the human. Z Rheumatol. 1995;54(2):117–122. [PubMed] [Google Scholar]
- 34.Ikeda R. Innervation of the sacroiliac joint. Macroscopical and histological studies. Nippon Ika Daigaku Zasshi. 1991;58(5):587–596. doi: 10.1272/jnms1923.58.587. [DOI] [PubMed] [Google Scholar]
- 35.Vilensky JA, O'Connor BL, Fortin JD. Histologic analysis of neural elements in the human sacroiliac joint. Spine (Phila Pa 1976) 2002;27(11):1202–1207. doi: 10.1097/00007632-200206010-00012. [DOI] [PubMed] [Google Scholar]
- 36.Sakamoto N, Yamashita T, Takebayashi T, Sekine M, Ishii S. An electrophysiologic study of mechanoreceptors in the sacroiliac joint and adjacent tissues. Spine (Phila Pa 1976) 2001;26(20):E468–E471. doi: 10.1097/00007632-200110150-00008. [DOI] [PubMed] [Google Scholar]
- 37.Solonen KA. The sacroiliac joint in the light of anatomical, roentgenological, and clinical studies. Acta Orthop Scand. 1957;27:1–27. [PubMed] [Google Scholar]
- 38.Minaki Y, Yamashita T, Ishii S. An electrophysiological study on the mechanoreceptors in the lumbar spine and adjacent tissues. Neurol Orthop. 1996;20:23–35. [Google Scholar]
- 39.van der Wurff P, Buijs EJ, Groen GJ. A multitest regimen of pain provocation tests as an aid to reduce unnecessary minimally invasive sacroiliac joint procedures. Arch Phys Med Rehabil. 2006;87(1):10–14. doi: 10.1016/j.apmr.2005.09.023. [DOI] [PubMed] [Google Scholar]
- 40.Laslett M, Young SB, Aprill CN, McDonald B. Diagnosing painful sacroiliac joints: a validity study of a McKenzie evaluation and sacroiliac provocation tests. Aust J Physiother. 2003;49(2):89–97. doi: 10.1016/s0004-9514(14)60125-2. [DOI] [PubMed] [Google Scholar]
- 41.Maigne JY, Boulahdour H, Chatellier G. Value of quantitative radionuclide bone scanning in the diagnosis of sacroiliac joint syndrome in 32 patients with low back pain. Eur Spine J. 1998;7(4):328–331. doi: 10.1007/s005860050083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.van der Wurff P, Buijs EJ, Groen GJ. Intensity mapping of pain referral areas in sacroiliac joint pain patients. J Manipulative Physiol Ther. 2006;29(3):190–195. doi: 10.1016/j.jmpt.2006.01.007. [DOI] [PubMed] [Google Scholar]
- 43.Kokmeyer DJ, van der Wurff P, Aufdemkampe G, Fickenscher TCM. The reliability of multitest regimens with sacroiliac pain provocation tests. J Manipulative Physiol Ther. 2002;25(1):42–48. doi: 10.1067/mmt.2002.120418. [DOI] [PubMed] [Google Scholar]
- 44.Vincent-Smith B. Gibbons P Inter-examiner and intra-examiner reliability of the standing flexion test. Man Ther. 1999;4(2):87–93. doi: 10.1054/math.1999.0173. [DOI] [PubMed] [Google Scholar]
- 45.Dreyfuss P, Michaelsen M, Pauza K, McLarty J, Bogduk N. The value of medical history and physical examination in diagnosing sacroiliac joint pain. Spine (Phila Pa 1976) 1996;21(22):2594–2602. doi: 10.1097/00007632-199611150-00009. [DOI] [PubMed] [Google Scholar]
- 46.Slipman CW, Sterenfeld EB, Chou LH, Herzog R, Vresilovic E. The predictive value of provocative sacroiliac joint stress maneuvers in the diagnosis of sacroiliac joint syndrome. Arch Phys Med Rehabil. 1998;79(3):288–292. doi: 10.1016/s0003-9993(98)90008-9. [DOI] [PubMed] [Google Scholar]
- 47.Szadak KM, van der Wurff, van Tulder MW, Zuurmond WW, Perez RS. Diagnostic validity of criteria for SIJD: a systematic review. J Pain. 2009;10(4):354–368. doi: 10.1016/j.jpain.2008.09.014. [DOI] [PubMed] [Google Scholar]
- 48.Magee DJ. 4th ed. Philadelphia, PA: Saunders Elsevier; 2006. Orthopedic Physical Assessment; pp. 642–643. [Google Scholar]
- 49.Barnsley L, Lord S, Bogduk N. Comparative local anaesthetic blocks in the diagnosis of cervical zygapophysial joint pain. Pain. 1993;55(1):99–106. doi: 10.1016/0304-3959(93)90189-V. [DOI] [PubMed] [Google Scholar]
- 50.Cooperstein R, Truong F. Does the Gillet test assess sacroiliac motion or asymmetric one-legged stance strategies? J Can Chiropr Assoc. 2018;62(2):85–97. [PMC free article] [PubMed] [Google Scholar]
- 51.Meijne W, Van Neerbos K, Aufdemkampe G. Intraexaminer and interexaminer reliability of the Gillet test. J Manip Physiol Ther. 1999;22(1):4–9. doi: 10.1016/s0161-4754(99)70098-9. [DOI] [PubMed] [Google Scholar]
- 52.Cattley P, Winyard J, Trevaskis J, Eaton S. Validity and reliability of clinical tests for the sacro-iliac joint. A review of literature. Australas Chiropr Osteopathy. 2002;10(2):73–80. [PMC free article] [PubMed] [Google Scholar]
- 53.Mitchell TD, Urli KE, Breitenbach J, Yelverton C. The predictive value of the sacral base pressure test in detecting specific types of sacroiliac dysfunction. J Chiropr Med. 2007;6(2):45–55. doi: 10.1016/j.jcme.2007.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Hoppenfeld S. Appleton-Century-Crofts; New York, NY: 1976. Physical Examination of the Spine and Extremities. [Google Scholar]
- 55.Cook C, Hegedus E. Prentice Hall; New Jersey: 2013. Orthopedic Physical Examination Test: An Evidence Based Approach. [Google Scholar]
- 56.Polly D, Cher D, Whang PG, Frank C, Sembrano J, Study Group INSITE. Does level of response to SI joint block predict response to SI joint fusion? Int J Spine Surg. 2016;21:10:4. doi: 10.14444/3004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Altman DG, Machin D, Bryant TN, Gardner MJ. 2nd ed. British Medical Journal; Bristol: 2000. Statistics with Confidence. [Google Scholar]
- 58.Bryant TN. Confidence interval analysis for Windows. In: Altman DG, Machin D, Bryant TN, Gardner MJ, editors. Statistics with Confidence. 2nd ed. London, UK: BMJ Books; 2000. [Google Scholar]
- 59.Broadhurst NA, Bond MJ. Pain provocation tests for the assessment of sacroiliac joint dysfunction. J Spin Disord. 1998;11(4):341–345. [PubMed] [Google Scholar]
- 60.van der Wurff P, Hagmeijer RH, Meyne W. Clinical tests of the sacroiliac joint. A systemic methodological review. Part 1: reliability. Man Ther. 2000;5(1):30–36. doi: 10.1054/math.1999.0228. [DOI] [PubMed] [Google Scholar]
- 61.van der Wurff P, Meyne W, Hagmeijer RH. Clinical tests of the sacroiliac joint. Man Ther. 2000;5(2):89–96. doi: 10.1054/math.1999.0229. [DOI] [PubMed] [Google Scholar]
- 62.Schwarzer AC, Aprill CN, Bogduk M. The sacroiliac joint in chronic low back pain. Spine (Phila Pa 1976) 1995;20(1):31–37. doi: 10.1097/00007632-199501000-00007. [DOI] [PubMed] [Google Scholar]
- 63.Young S, Aprill CN, Laslett M. Correlation of clinical examination characteristics with three sources of chronic low back pain. Spine J. 2003;3(6):460–465. doi: 10.1016/s1529-9430(03)00151-7. [DOI] [PubMed] [Google Scholar]
- 64.Bogduk N, McGuirk B. Vol. 13. Elsevier Science BV; Amsterdam, The Netherlands: 2002. (Medical Management of Acute and Chronic Low Back Pain, vol.). [Google Scholar]
- 65.Paulsen R, Aass N, Kaasa S, Dale O. Do corticosteroids provide analgesic effects in cancer patients? A systematic literature review. J Pain Symptom Manage. 2013;46(1):96–105. doi: 10.1016/j.jpainsymman.2012.06.019. [DOI] [PubMed] [Google Scholar]
- 66.Maigne JY, Planchon CA. Sacroiliac joint pain after fusion. A study with anesthetic blocks. Eur Spine J. 2005;14(7):654–658. doi: 10.1007/s00586-004-0692-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Simopoulos TT, Manchikanti L, Singh V. A systematic evaluation of prevalence and diagnostic accuracy of sacroiliac joint interventions. Pain Physician. 2012;15(3):E305–E344. [PubMed] [Google Scholar]
- 68.Berthelot JM, Labat JJ, Le Goff B, Gouin F, Maugars Y. Provocative sacroiliac joint maneuvers and sacroiliac joint block are unreliable for diagnosing sacroiliac joint pain. Joint Bone Spine. 2006;73(1):17–23. doi: 10.1016/j.jbspin.2004.08.003. [DOI] [PubMed] [Google Scholar]
- 69.Dreyfuss P, Dreyer S, Griffin J, Hoffman J, Walsh N. Positive sacroiliac screening tests in asymptomatic adults. Spine (Phila Pa 1976) 1994;19(10):1138–1143. doi: 10.1097/00007632-199405001-00007. [DOI] [PubMed] [Google Scholar]
- 70.Robinson HS, Brox JI, Robinson R, Bjelland E, Solem S, Telje T. The reliability of selected motion and pain provocation tests for the sacroiliac joint. Man Ther. 2007;12(1):72–79. doi: 10.1016/j.math.2005.09.004. [DOI] [PubMed] [Google Scholar]
- 71.Hungerford BA, Gilleard W, Moran M, Emmerson C. Evaluation of the ability of physical therapists to palpate intrapelvic motion with the Stork test on the support side. Phys Ther. 2007;87(7):879–887. doi: 10.2522/ptj.20060014. [DOI] [PubMed] [Google Scholar]
- 72.Vanelderen P, Szadek K, Cohen SP. Sacroiliac joint pain. Pain Pract. 2010;10(5):470–480. doi: 10.1111/j.1533-2500.2010.00394.x. [DOI] [PubMed] [Google Scholar]