Abstract
The earliest evidence from China suggested that COVID-19 patients are even more vulnerable to succumbing from complications in the presence of a multimorbid status, including metabolic syndrome. Due to ongoing metabolic abnormalities, non-alcoholic fatty liver disease (NAFLD) appears to be a potential risk factor for contracting SARS-CoV-2 infection and developing related complications. This is because of the interplay of chronically active inflammatory pathways in NAFLD- and COVID-19-associated acute cytokine storm. The risk of severe disease could also be attributed to compromised liver function as a result of NAFLD. We systematically reviewed current literature to ascertain the relationship between NAFLD and severe COVID-19, independent of obesity, which is considered the major factor risk factor for both NAFLD and COVID-19. We found that NAFLD is a predictor of severe COVID-19, even after adjusting for the presence of obesity (OR 2.358; 95% CI: 1.902–2.923, p < 0.001).
Keywords: SARS-CoV-2, COVID-19, Coronavirus, NAFLD, MAFLD, Fatty liver
Introduction
Coronavirus disease 2019 (COVID-19) caused by Severe Acute Respiratory Syndrome Coronavirus-2 (SARS-CoV-2) was declared a pandemic by the World Health Organization (WHO) in March 2020. Although it is primarily a respiratory illness, transaminemia associated with COVID-19 is associated with higher mortality [1]. The initial reports from liver biopsies of COVID-19 patients showed ballooning hepatocytes with mitotic cells and eosinophilic bodies, suggesting SARS-CoV-2 induces apoptosis in liver cells [1]. Other authors have proposed that the increased levels of inflammatory mediators, such as IL-1, IL-6, and IL-10 levels, may further contribute to damaging hepatocytes in COVID-19 patients [1]. Hepatic steatosis is a commonly observed finding in patients testing positive for SARS-CoV-2 [2]. The effect of fatty liver on the severity of COVID-19 illness has not yet been studied. We aim to systematically review published literature and evaluate the severity of COVID-19 in patients with fatty liver.
Methods
A systematic literature search of PUBMED, Google Scholar, and SCOPUS databases was performed to identify studies reporting the association of fatty liver and COVID-19 through September 9, 2020. Search key terms employed were as follows: “NAFLD,” “metabolic associated fatty liver disease (MAFLD),” “fatty liver,” “COVID-19,” and “SARS-COV2.” The reference lists of these articles were also screened and hand-searched to identify further relevant studies. Included studies assessed the presence or absence of fatty liver by computed tomography (CT) or abdominal ultrasound coupled with an internal expert consensus statement to diagnose NAFLD. The presence of positive SARS-CoV-2 RT-PCR diagnosed COVID-19 infection. Whenever available, we collected data on the risk COVID-19 and its severity in patients diagnosed with fatty liver. Severe COVID-19 was defined in most studies using guidelines laid down by the National Health Commission of China. Other outcomes included were hospitalization and ICU admission, as mentioned in Table 1. We included studies that reported OR for severe COVID-19 in patients with NAFLD/MAFLD after adjusting for obesity. Data on the odds ratio (OR) with 95% confidence interval (CI) were collected and pooled to compute the pooled odds ratio using random-effects models. Heterogeneity was assessed using the I2 test, and I2 of > 50% was considered a moderate inter-study variation. A p value < 0.05 was considered statistically significant. All analyses were performed using the OpenMetaAnalyst software.
Table 1.
Baseline characteristics of included studies
| Study | Location | Sample size | Males | Patients with NAFLD | Patient outcome for the severity of disease (COVID-19) included in our analysis |
|---|---|---|---|---|---|
| Mahamid [3] | Israel | 71 | 20 | 22 | COVID-19 severity assessed using diagnosis and treatment protocol for novel Coronavirus pneumonia released by National Health Commission and State Administration of Traditional Chinese Medicine* |
| Targher [4] | China | 310 | 149 | 94 | Criteria for severe COVID-19 a laid down by the National Health Commission, China |
| Zhou et al. 1 [5] | China | 327 | – | 93 | Criteria for severe COVID-19 a laid down by the National Health Commission, China |
| Zho et al. 2 [6] | China | 110 | 82 | 55 | Criteria for severe COVID-19 a laid down by the National Health Commission, China |
| Ji et al. [7] | China | 202 | 113 | 76 | According to Chinese National Health commission |
| Gao et al. [8] | China | 130 | 82 | 65 | Criteria for severe COVID-19 a laid down by the National Health Commission, China |
| Hashemi et al. [9] | USA | 363 | 201 | 55 | ICU admission |
| Bramante et al. [10] | USA | 6700 | 3752 | 373 | Hospitalization |
*National Health Commission; National Administration of Traditional Chinese Medicine. Diagnosis and treatment protocol for novel coronavirus pneumonia (Trial Version 7). Chin Med J (Engl) 2020; 133:1087–1095
Results
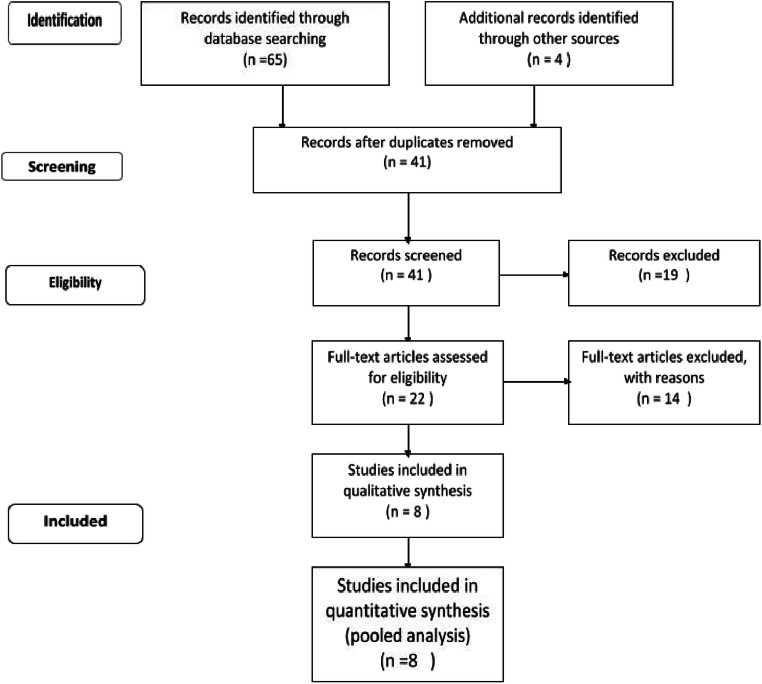
The flow chart depicting the process of study screening is presented in Fig. 1. An initial electronic search yielded 65 articles, and 3 others were identified via cross-reference search. After excluding duplicates, 41 studies were found to be eligible for screening their abstracts and full texts. Out of the 41 screened, 23 were not relevant to our study, 5 were review articles/editorials, and the rest did not contain extractable data. Eight studies were included in the quantitative analysis of the pooled odds ratio (OR). The total sample size consisted of 8142 COVID-positive patients, out of which 833 patients had NAFLD. The characteristics of the included studies are summarized in Table 1.
Fig. 1.
Study flow chart
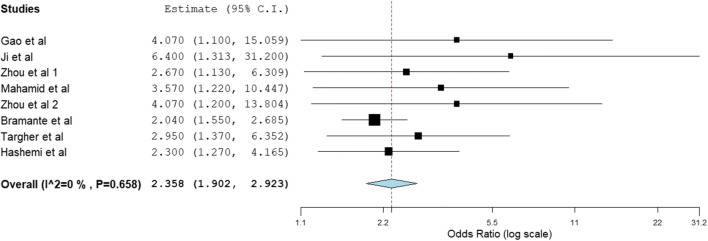
The pooled OR for severe COVID-19 in NAFLD, after adjusting for obesity was 2.358 (95% CI: 1.902–2.923, p < 0.001; Fig. 2). A minimal heterogeneity was identified in the analysis. No significant differences were observed in the leave-one-out sensitivity analysis for disease severity.
Fig. 2.
Pooled odds ratio for severe COVID-19
Discussion
Patients with pre-existing liver disorders, such as liver cirrhosis and hepatocellular carcinoma, are considered to have a higher susceptibility for any kind of infection and sepsis secondary to impaired host defense [11]. Cardiometabolic risk factors such as obesity also have been identified as potential risk factors for mortality in COVID-19 [12].
Nonalcoholic fatty liver disease, NAFLD (also known as metabolic associated fatty liver disease, MAFLD), is considered to be the hepatic manifestation of metabolic syndrome, which encompasses obesity, diabetes, dyslipidemia, and insulin resistance [13]. It is understandable that due to these concurrent issues, NAFLD would predispose to severe COVID-19. A multicenter retrospective study by Zheng et al. further validated this information. They showed that obesity conferred a ~ sixfold higher risk of severe COVID-19 in patients with NAFLD. The OR for the severity of COVID-19 illness was 6.32 in obese NAFLD patients than in non-obese patients with NAFLD [14].
However, our pooled analysis points out yet another interesting observation about COVID-19 and fatty liver disease. We found that NAFLD was associated with an increased risk of severe COVID-19, even after adjusting for obesity as a possible confounding factor. We believe that liver fat and associated inflammation could exacerbate the virus-associated cytokine storm, leading to worsening COVID-19. Targher et al. found that increasing liver fibrosis measured by NFS/FIB-4 score was linked to increased severity of disease in COVID-19 patients [4]. Moreover, liver fat has been independently linked to an increased risk of testing positive for COVID-19 [15]. A study showed that NAFLD was independently associated with a significant ALT elevation after adjusting for BMI and other factors [16].
Hence, it is conceivable that injury caused by fat accumulation in the liver and subsequent fibrosis could be one of the plausible reasons for the poor disease course observed in patients with NAFLD.
Conclusions
Nonalcoholic fatty liver disease is associated with a higher risk of symptomatic, severe, and progressive COVID-19. The association is significant even after adjusting for an important confounding factor, obesity. Hence, it can be concluded that the hepatic manifestation of COVID-19 is independently linked to the severity of coronavirus disease. However, the exact relationship between liver fat and COVID-19 remains to be elucidated.
Author Contributions
Conception and design: Sonali Sachdeva and Harshwardhan Khandait
Literature search: Sonali Sachdeva, Harshwardhan Khandait, and Rupak Desai
First draft: Sonali Sachdeva and Jonathan Kopel
Critical revision and editing: All authors
Final approval: All authors
All authors have made substantive contributions to the study, and all authors endorse the data and conclusions.
Footnotes
This article is part of the Topical Collection on Covid-19
This manuscript, as submitted or its essence in another version, is not under consideration for publication elsewhere and will not be published elsewhere while under review by Digestive and Liver Diseases.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Sonali Sachdeva, Email: sonalisachdeva1993@gmail.com.
Harshwardhan Khandait, Email: harshkhandait1@gmail.com.
Jonathan Kopel, Email: jonathan.kopel@ttuhsc.edu.
Mark M. Aloysius, Email: madhoka@thewrightcenter.org
Rupak Desai, Email: drrupakdesai@gmail.com, Email: rdesa30@emory.edu.
Hemant Goyal, Email: doc.hemant@yahoo.com.
References
- 1.Boregowda U, Aloysius MM, Perisetti A, Gajendran M, Bansal P, Goyal H. Serum activity of liver enzymes is associated with higher mortality in COVID-19: a systematic review and meta-analysis. Front Med (Lausanne) 2020;7:431. doi: 10.3389/fmed.2020.00431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Medeiros AK, Barbisan CC, Cruz IR, de Araújo EM, Libânio BB, Albuquerque KS, Torres US. Higher frequency of hepatic steatosis at CT among COVID-19-positive patients. Abdom Radiol (NY) 2020;45(9):2748–2754. doi: 10.1007/s00261-020-02648-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mahamid M, Nseir W, Khoury T, Mahamid B, Nubania A, Sub-Laban K, et al. Nonalcoholic fatty liver disease is associated with COVID-19 severity independently of metabolic syndrome: a retrospective case-control study. Eur J Gastroenterol Hepatol. 2020. 10.1097/MEG.0000000000001902 Publish Ahead of Print. [DOI] [PMC free article] [PubMed]
- 4.Targher G, Mantovani A, Byrne CD, Wang XB, Yan HD, Sun QF, Pan KH, Zheng KI, Chen YP, Eslam M, George J, Zheng MH. Risk of severe illness from COVID-19 in patients with metabolic dysfunction-associated fatty liver disease and increased fibrosis scores. Gut. 2020;69(8):1545–1547. doi: 10.1136/gutjnl-2020-321611. [DOI] [PubMed] [Google Scholar]
- 5.Zhou YJ, Zheng KI, Wang XB, Yan HD, Sun QF, Pan KH, Wang TY, Ma HL, Chen YP, George J, Zheng MH. Younger patients with MAFLD are at increased risk of severe COVID-19 illness: a multicenter preliminary analysis. J Hepatol. 2020;73(3):719–721. doi: 10.1016/j.jhep.2020.04.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Zhou YJ, Zheng KI, Wang XB, Sun QF, Pan KH, Wang TY, Ma HL, Chen YP, George J, Zheng MH. Metabolic-associated fatty liver disease is associated with severity of COVID-19. Liver Int. 2020;40(9):2160–2163. doi: 10.1111/liv.14575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ji D, Qin E, Xu J, Zhang D, Cheng G, Wang Y, Lau G. Non-alcoholic fatty liver diseases in patients with COVID-19: A retrospective study. J Hepatol. 2020;73(2):451–453. doi: 10.1016/j.jhep.2020.03.044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gao F, Zheng KI, Wang XB, Yan HD, Sun QF, Pan KH, et al. Metabolic associated fatty liver disease increases coronavirus disease 2019 disease severity in nondiabetic patients. J Gastroenterol Hepatol. 2020. 10.1111/jgh.15112. [DOI] [PMC free article] [PubMed]
- 9.Hashemi N, Viveiros K, Redd WD, Zhou JC, McCarty TR, Bazarbashi AN, et al. Impact of chronic liver disease on outcomes of hospitalized patients with COVID-19: a multicentre United States experience. Liver Int. 2020. 10.1111/liv.14583. [DOI] [PMC free article] [PubMed]
- 10.Bramante C, Tignanelli CJ, Dutta N, Jones E, Tamariz L, Clark JM, Usher M, Metlon-Meaux G, Ikramuddin S. Non-alcoholic fatty liver disease (NAFLD) and risk of hospitalization for Covid-19. medRxiv [Preprint]. 2020:2020.09.01.20185850. 10.1101/2020.09.01.20185850.
- 11.Strnad P, Tacke F, Koch A, Trautwein C. Liver — guardian, modifier and target of sepsis. Nat Rev Gastroenterol Hepatol. 2017;14(1):55–66. doi: 10.1038/nrgastro.2016.168. [DOI] [PubMed] [Google Scholar]
- 12.Hussain A, Mahawar K, Xia Z, Yang W, El-Hasani S. Obesity and mortality of COVID-19. Meta-analysis. Obes Res Clin Pract. 2020;14(4):295–300. doi: 10.1016/j.orcp.2020.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 13.Hashimoto E, Taniai M, Tokushige K. Characteristics and diagnosis of NAFLD/NASH. J Gastroenterol Hepatol. 2013;28(Suppl 4):64–70. doi: 10.1111/jgh.12271. [DOI] [PubMed] [Google Scholar]
- 14.Zheng KI, Gao F, Wang XB, Sun QF, Pan KH, Wang TY, Ma HL, Chen YP, Liu WY, George J, Zheng MH. Letter to the Editor: Obesity as a risk factor for greater severity of COVID-19 in patients with metabolic associated fatty liver disease. Metabolism. 2020;108:154244. doi: 10.1016/j.metabol.2020.154244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Roca-Fernández A, Dennis A, Nicolls R, McGonigle J, Kelly M, Banerjee R. High liver fat associates with higher risk of developing symptomatic COVID-19 infection - initial UK biobank observations. 2020. 10.1101/2020.06.04.20122457.
- 16.Huang R, Zhu L, Wang J, Xue L, Liu L, Yan X, et al. Clinical features of COVID-19 patients with non-alcoholic fatty liver disease. Hepatol Commun. 2020. 10.1002/hep4.1592. [DOI] [PMC free article] [PubMed]