Summary
Background
The number of people presenting to hospital emergency departments after self-harming has increased in England. However, most people who self-harm do not present to hospitals, so whether this rise reflects an increase in the prevalence of self-harm in the community is unknown. Also unknown is whether the prevalence of non-suicidal self-harm (NSSH) or suicidal self-harm, or both, has increased. We aimed to establish temporal trends in the prevalence of NSSH in England.
Methods
We analysed data from participants in the 2000 (n=7243), 2007 (n=6444), and 2014 (n=6477) Adult Psychiatric Morbidity Surveys of the general population, selecting those aged 16–74 years and living in England. We used weighted data and controlled for complex survey design. We generated temporal trends in lifetime prevalence and methods of, and motivations for, NSSH, and consequent service contact. We used multiple variable logistic regression analyses to investigate factors associated with service contact.
Findings
The prevalence of self-reported lifetime NSSH increased from 2·4% (95% CI 2·0–2·8) in 2000, to 6·4% (5·8–7·2) in 2014. Increases in prevalence were noted in both sexes and across age groups—most notably in women and girls aged 16–24 years, in whom prevalence increased from 6·5% (4·2–10·0) in 2000, to 19·7% (15·7–24·5) in 2014. The proportion of the population reporting NSSH to relieve unpleasant feelings of anger, tension, anxiety, or depression increased from 1·4% (95% CI 1·0–2·0) to 4·0% (3·2–5·0) in men and boys, and from 2·1% (1·6–2·7) to 6·8% (6·0–7·8) in women and girls, between 2000 and 2014. In 2014, 59·4% (95% CI 54·7–63·9) of participants who had engaged in NSSH reported no consequent medical or psychological service contact, compared with 51·2% (42·2–60·0) in 2000 and 51·8% (47·3–56·4) in 2007. Male participants and those aged 16–34 years were less likely to have contact with health services than were female participants and older people.
Interpretation
The prevalence of NSSH has increased in England, but resultant service contact remains low. In 2014, about one in five female 16–24-year-olds reported NSSH. There are potential lifelong implications of NSSH, such as an increased frequency of suicide, especially if the behaviours are adopted as a long-term coping strategy. Self-harm needs to be discussed with young people without normalising it. Young people should be offered help by primary care, educational, and other services to find safer ways to deal with emotional stress.
Funding
NHS Digital, English Department of Health and Social Care, and the National Institute for Health Research.
Introduction
The number of studies of non-suicidal self-harm (NSSH) or non-suicidal self-injury has grown worldwide since 2000,1 leading to improved recognition and informed prevention programmes.2 People who self-harm and present to hospital are at increased risk of suicide, fatal alcohol or drug poisoning, and other causes of mortality.3 Whether the prevalence or nature of NSSH is changing is unclear, because studies of temporal trends are rare and their findings inconsistent.4
A systematic review5 of NSSH in adolescent samples worldwide showed no evidence of an increased prevalence between 2005 and 2011. In most other studies, NSSH was amalgamated with suicide attempts.6, 7, 8, 9 Analyses of Danish hospital registration data for 1994–2011, for example, showed a rising frequency of self-harm (with and without suicidal intent) in both sexes, with the greatest increases in women and girls aged 15–24 years.9 Data from the National Self-Harm Registry in Ireland showed that the frequency of self-harm increased by 22% between 2007 and 2016 in 10–24-year-olds, and by more in women and girls.8 In Geulayov and colleagues' study7 of adults presenting to five general hospitals in England, the frequency of self-harm (with and without suicidal intent) fell between 2000 and 2012 in women and girls, and between 2000 and 2008 in men and boys, before increasing again. However, analysis of English primary care data showed that the incidence of self-harm (with and without suicidal intent) increased by 68% in girls aged 13–16 years between 2011 and 2014), but did not change in boys or in girls of other ages.2
Research in context.
Evidence before this study
We searched PubMed with the terms “nonsuicidal self-harm” or “nonsuicidal self-injury” and “prevalence”, “rates”, and “trends” to identify articles published in English up to September, 2018. Available evidence for temporal trends in self-harm in England comes from studies of populations in contact with services. Findings are mixed, with some evidence that the prevalence of self-harm is increasing, particularly in young people. In most service use data, however, suicidal and non-suicidal self-harm (NSSH) are amalgamated, and temporal trends could reflect changes in patterns of help-seeking or treatment availability and coding. Findings based on people in contact with services might not be generalisable to the wider population, in whom much self-harm goes untreated.
Added value of this study
This study provides, to our knowledge, the first evidence of long-term trends in non-suicidal self-harm in the general population in England. We showed that prevalence of NSSH increased in both sexes and across all age groups between 2000 and 2014. This increase was mostly because of rises in self-cutting and increased use of NSSH to relieve unpleasant feelings. Absolute rises were highest in women and girls aged 16–24 years. Most participants reported no medical or psychological service contact after NSSH. Men and 16–34-year-olds were particularly unlikely to have service contact.
Implications of all the available evidence
The prevalence of NSSH has increased steeply. In 2014, one in five women and girls aged 16–24 years reported having self-harmed. NSSH in men could go unrecognised because they might be less likely both to seek and receive interventions. If self-harm is increasing among young people partly because it is thought of as a way of coping with emotional stress, there could be serious long-term public health implications, including normalisation of self-harm and potential increases in suicide rates. Better primary care and educational services need to be offered, and self-harm needs to be discussed in a way that helps young people to find safer ways of coping.
People presenting to hospitals or primary care differ in profile from the wider population engaging in self-harm: they are more likely to attempt suicide or overdose, but less likely to engage in NSSH or self-cutting.10 Furthermore, although many argue that the motives underpinning self-harm are multiple, fluid, and complex,11 effective intervention is likely to depend on understanding NSSH and suicide attempts as distinct issues.12 Additionally, much research done has focused on adolescents.5
We used a series of high-quality cross-sectional surveys of the general English population to establish trends in NSSH from 2000 to 2014. We examined changes in the prevalence of self-reported NSSH, the methods used, reported motivations, and reports of subsequent contact with medical or psychological services
Methods
Study design and participants
We did a secondary analysis of data from the 2000, 2007, and 2014 Adult Psychiatric Morbidity Surveys, a series of surveys of the mental health of the general population. Although the geographical and age range covered by the surveys varied (the 2000 wave included people aged 16–74 years living in England, Scotland, and Wales, whereas 2007 and 2014 waves covered England only and had no upper age limit to participate), for comparability we selected participants aged 16–74 years and living in England for our analysis (appendix p 1). Each wave of the Adult Psychiatric Morbidity Surveys had a similar stratified random probability sampling design suitable to produce a sample representative of the population living in private households in England. Sampling, procedure, and ethical review details have been previously published.16, 17, 18
Briefly, the first stage involved selection of addresses from the Postcode Address File,13 which covered 97% of households. People living in communal or institutional establishments or temporary housing, and homeless people were not sampled. Although these populations might have a higher prevalence of NSSH than the general population,14 they account for less than 2% of the overall population, and their exclusion should not affect overall estimates.15
Fieldwork took place from March to September, 2000; from October, 2006, to December, 2007; and from May, 2014, to September, 2015. Trained research interviewers visited addresses to identify private households with at least one resident aged 16 years or older. One person was randomly selected in each eligible household. Interviews were done in participants' own homes and took 1·5 h on average. Most of the questionnaire was administered face to face, but some sensitive information (eg, experience of abuse) was self-completed: participants keyed their responses into a laptop for enhanced privacy. Ethical approval was obtained from the relevant ethics committees. Our secondary analyses were approved by the National Centre for Social Research's ethical review committee.
Measures
DSM-519 includes non-suicidal self-injury and suicidal behaviour disorder as conditions for further study.20 Although intent can be difficult to establish,21 in the Adult Psychiatric Morbidity Surveys suicide attempts were distinguished from NSSH. In 2000, 2007, and 2014, participants were asked (face to face) “Have you ever deliberately harmed yourself in any way but not with the intention of killing yourself?” without further prompts. Affirmative responses to this question were used to establish lifetime NSSH. Our measure of NSSH is not equivalent to the DSM's non-suicidal self-injury because it does not take into account the frequency, recency, severity, or method of self-harm, or other criteria. Because our definition included self-injury and self-poisoning, we refer to NSSH rather than non-suicidal self-injury. Questions about NSSH were also included in the self-completion section in 2007 and 2014, but we used face-to-face responses to maximise comparability in trends with 2000. We also included a variable combining face-to-face and self-completed responses about NSSH, to provide the most recent and inclusive indication of prevalence. Only in 2014 was the most recent occasion of NSSH dated (which was coded as “past week”, “past year”, or “longer ago”). Suicide attempts were asked about with the question “Have you ever made an attempt to take your life, by taking an overdose of tablets or in some other way?”
Participants reporting NSSH were asked about methods, motivations, and subsequent service contact; the same wording was used in each wave of the Adult Psychiatric Morbidity Surveys. In 2000 and 2007, the follow-up questions were asked face to face, but in 2014 they were asked by self-completion. To ensure comparability between waves, we restricted trend measures for 2014 to participants who reported NSSH face to face. For the methods used, participants were asked “Did you cut yourself, or burn yourself, or swallow anything, or harm yourself some other way?” More than one method could be coded. Regarding motiviation, they were asked “Did you do any of these things to draw attention to your situation or to change your situation?” and “Did you do any of these things because it relieved unpleasant feelings of anger, tension, anxiety, or depression?” Participants could select neither, one, or both reasons. One variable was produced for whether participants reported being motivated by change, and one for whether participants reported being motivated by relieving unpleasant feelings (these categories were not mutually exclusive). For subsequent service contact, participants were asked “Have you received medical attention for deliberately harming yourself in any of these ways?” and “Have you ever seen a psychiatrist, psychologist, or counsellor because you had harmed yourself?” Participants were classified as having medical contact only, psychological contact only, both, or neither.
Because detailed classification of ethnicity varied somewhat between the waves, we used broad categories: white, black, Asian, and other or mixed. Housing was classified as owner-occupied or rented. People who had been in arrears with payments in the past year were identified—eg, disconnection from gas, electricity, or other fuel services because of failure to pay, being “seriously behind in paying within the time allowed” for a range of services and obligations. Highest educational qualifications and household income were elicited by showing participants lists of options, from which they could choose their response. We classified area-level deprivation into Index of Multiple Deprivation quintiles.
Symptoms of common mental disorders were measured with the Clinical Interview Schedule—Revised (CIS-R), an interviewer-administered structured interview that provides a continuous scale reflecting the overall severity of psychopathology in the week before interview.22 In our analyses, we divided participants' scores into two groups: 0–17 and 18 or higher. This threshold of 18 or higher was selected because it suggests a severity of symptoms for which intervention is warranted.18 Participants also self-rated their general health, and we grouped responses into two categories: excellent or very good, and good, fair, or poor.
Statistical analysis
We used weighted data for our analyses, and took the complex design of the survey into account. Weighting adjusted for selection probabilities and non-response, thereby rendering results representative of the household population aged 16 years or older at the time of each survey. Population control totals were obtained from the UK Office for National Statistics mid-year population estimates for age by sex and region. Bases are presented unweighted. Non-overlapping 95% CIs provided statistical evidence for differences in prevalence between periods or subgroups. We did multiple variable logistic regression analyses of factors predicting service contact as a result of NSSH. We calculated unadjusted odds ratios (ORs) for service contact, and ran two models to calculate adjusted ORs. The first adjusted model included sex, age, tenure, debt arrears, CIS-R score, and general health. The second model additionally controlled for reported method of self-harm and whether the participant reported having ever made a suicide attempt. Missing data were excluded from analyses. All analyses were done in SPSS (version 21.0) or Stata (version 14.1).
Role of the funding source
The funder had no role in the study design, data collection, data analysis, data interpretation, or writing of the report. The corresponding author had full access to all the data in the study and had final responsibility for the decision to submit for publication.
Results
We analysed data for 7243 people aged 16–74 years in England in 2000, 6477 in 2007, and 6477 in 2014. Data for the number of households invited to participate, the number of people interviewed, and response rates are detailed in the appendix (p 1). Missing data were minimal (data not shown). Most missing data were a result of the 283 (4·3%) participants in the 2014 survey who did not provide responses for the self-completion section (data not shown). These participants were significantly older (p<0·0001) and had higher scores on the Clinical Interview Schedule—Revised (p=0·0010) than those who completed the self-completion section (appendix p 2). Self-completion non-response was not associated with sex (appendix p 2).
Overall, the lifetime prevalence of NSSH rose from 2·4 (95% CI 2·0–2·8) in 2000, to 3·8 (3·3–4·3) in 2007, and to 6·4 (5·8 to 7·2) in 2014. Table 1 shows the demographic characteristics of the analysed sample weighted to the age–sex–region profile of the wider population at the time of each survey. Across the three waves of the Adult Psychiatric Morbidity Surveys, the profile remained stable in terms of age and sex, but the proportion of respondents who were white fell (from 92·6% in 2000 to 89·4% in 2007 and 86·3% in 2014; table 1). In each wave, NSSH was most prevalent in the youngest age groups and least prevalent in the oldest age groups (table 1). The prevalence of NSSH did not differ significantly between ethnic groups in any wave (table 1). Prevalence was similar in male and female participants in 2000 and 2007, but was significantly higher in women and girls (7·9% [95% CI 6·9–9·0]) than in men and boys (5·0% [4·0–6·1]) in 2014 (p=0·0002; table 1). Prevalence increased in both sexes and in all age groups (table 1).
Table 1.
Prevalence of non-suicidal self-harm ever (face-to-face report) in 16–74-year-olds in England in 2000, 2007, and 2014
|
2000 (n=7243) |
2007 (n=6444) |
2014 (n=6477) |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| n (%)* | Reported non-suicidal self-harm (% [95% CI]) | p value | n (%)* | Reported non-suicidal self-harm (% [95% CI]) | p value | n (%)* | Reported non-suicidal self-harm (% [95% CI]) | p value | |
| Sex | |||||||||
| Male | 3237 (49·9%) | 65 (2·1% [1·6–2·7]) | 0·136 | 2824 (49·4%) | 98 (3·7% [3·0–4·5]) | 0·759 | 2638 (49·6%) | 119 (5·0% [4·0–6·1]) | 0·0002 |
| Female | 4006 (50·1%) | 105 (2·7% [2·2–3·4]) | .. | 3620 (50·6%) | 131 (3·8% [3·1–4·7]) | .. | 3839 (50·4%) | 291 (7·9% [6·9–9·0]) | .. |
| Age, years | |||||||||
| 16–24 | 665 (14·7%) | 37 (5·3% [3·7–7·6]) | <0·0001 | 567 (15·5%) | 59 (8·9% [6·9–11·6]) | <0·0001 | 559 (15·7%) | 90 (13·7% [11·2–16·7]) | <0·0001 |
| 25–34 | 1441 (20·6%) | 60 (3·8% [2·8–5·0]) | .. | 1035 (18·1%) | 58 (4·6% [3·5–6·1]) | .. | 1034 (18·7%) | 117 (10·3% [8·4–12·6]) | .. |
| 35–44 | 1540 (20·8%) | 42 (2·5% [1·8–3·4]) | .. | 1409 (21·1%) | 67 (4·7% [3·6–6·1]) | .. | 1178 (17·9%) | 87 (6·4% [5·1–8·0]) | .. |
| 45–54 | 1331 (18·5%) | 18 (1·0% [0·6–1·7]) | .. | 1128 (17·7%) | 30 (2·1% [1·4–3·1]) | .. | 1293 (19·3%) | 55 (2·9% [2·2–3·9]) | .. |
| 55–64 | 1194 (14·1%) | 11 (0·9% [0·5–1·6]) | .. | 1278 (16·3%) | 14 (0·9% [0·5–1·6]) | .. | 1226 (15·4%) | 45 (3·3% [2·4–4·6]) | .. |
| 65–74 | 1071 (11·4%) | 2 (0·1% [0·0–0·5]) | .. | 1027 (11·3%) | 1 (0·1% [0·0–0·8]) | .. | 1187 (13·0%) | 16 (1·1% [0·7–2·0]) | .. |
| Ethnicity† | |||||||||
| White | 6739 (92·6%) | 159 (2·5% [2·1–2·9]) | 0·706 | 5876 (89·4%) | 211 (3·9% [3·3–4·5]) | 0·239 | 5779 (86·3%) | 370 (6·5% [5·8–7·3]) | 0·743 |
| Black | 179 (2·5%) | 5 (1·6% [0·6–3·8]) | .. | 183 (3·3%) | 4 (3·2% [1·1–9·2]) | .. | 182 (3·2%) | 10 (6·6% [2·9–13·9]) | .. |
| Asian | 151 (3·0%) | 3 (1·6% [0·5–5·0]) | .. | 196 (4·2%) | 4 (1·0% [0·3–3·8]) | .. | 345 (7·6%) | 18 (5·8% [3·4–9·7]) | .. |
| Other or mixed | 127 (1·9%) | 2 (1·7% [0·4–6·7]) | .. | 156 (3·2%) | 8 (4·5% [2·2–9·2]) | .. | 147 (2·8%) | 9 (4·6% [2·2–9·1]) | .. |
The table shows data for all participants with valid data for non-suicidal self-harm (appendix p 1).
All percentages are presented weighted and bases unweighted.
Ethnicity data were missing for 47 people in 2000, 33 people in 2007, and 24 people (three of whom had reported non-suicidal self-harm) in 2014.
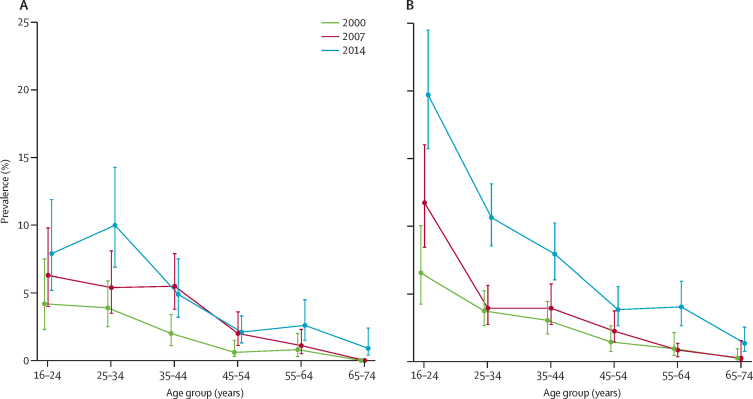
Prevalence increased in several age-by-sex groups; the percentage point increase in absolute terms was greatest in girls and young women (figure 1). In 2014 19·7% (95% CI 15·7–24·5) of female 16–24-year-olds reported NSSH in face-to-face interviews, compared with 6·5% (4·2–10·0) in 2000, and 11·7% (8·4–16·0) in 2007 (appendix p 3). Self-completion reports of NSSH were available for 2014, and suggest underreporting in the face-to-face reports. When self-completion reports were included, 25·7% (95% CI 21·0–31·0) of women and girls aged 16–24 years reported NSSH (appendix p 3).
Figure 1.
Prevalence of non-suicidal self-harm in men and boys (A) and women and girls (B), by age group
Data were self-reported in person (ie, face to face). Error bars show the 95% CIs.
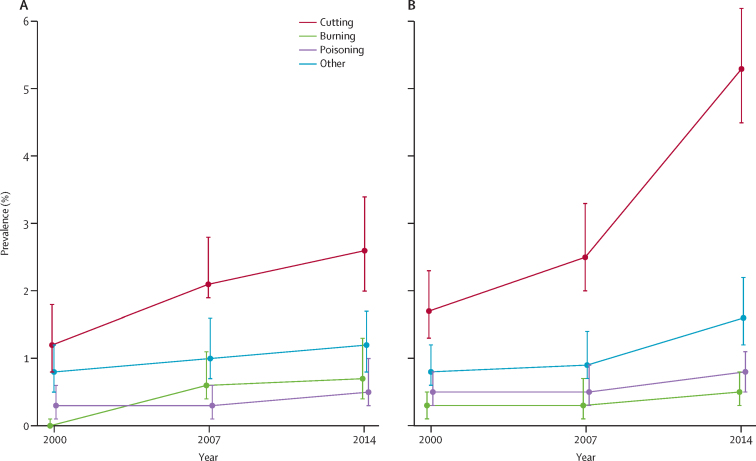
In each survey wave, around two-thirds of participants reporting NSSH had self-cut (appendix p 4). As NSSH became more common, the overall population prevalence of self-cutting also increased, from 1·5% (95% CI 1·2–1·8) in 2000, to 3·9% (3·5–4·5) in 2014 (appendix p 4). The increase was particularly pronounced in women and girls, in whom prevalence rose from 1·7% (1·3–2·3) in 2000, to 5·3% (4·5–6·2) in 2014, with the bulk of the increase occurring since 2007 (figure 2). In 2000 (p=0·129) and 2007 (p=0·334), the prevalence of self-cutting did not differ significantly by sex, whereas in 2014 it was higher in women and girls than in men and boys (p<0·0001; appendix p 4). In men and boys, the prevalence of self-burning increasing from 0·0% (95% CI 0·0–0·1) in 2000, to 0·6% (0·4–1·1) in 2007, and 0·7% (0·4–1·3) in 2014 (figure 2). The prevalence of self-poisoning remained stable in both sexes (figure 2). When participants in 2014 who reported NSSH in the self-completion section of the interview were also included, 7·0% (95% CI 6·1–8·0) of women and girls and 3·4% (2·7–4·3) of men and boys reported self-cutting (appendix p 4).
Figure 2.
Method of non-suicidal self-harm reported by men and boys (A) and women and girls (B) aged 16–74 years
Error bars show the 95% CIs.
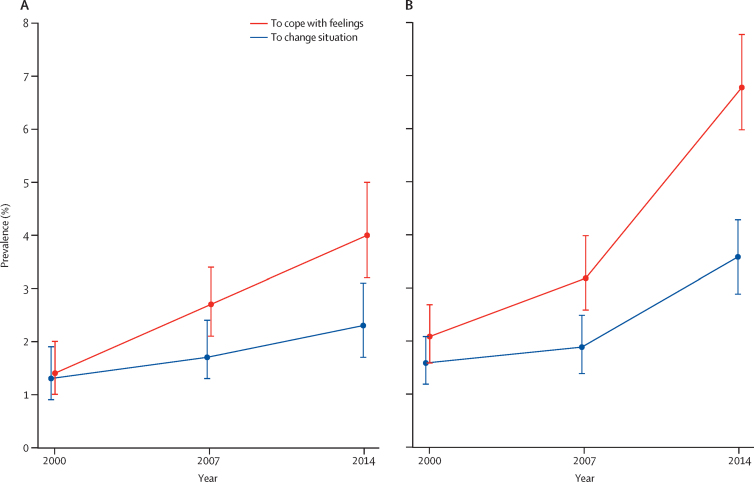
The proportion of the population reporting NSSH to relieve unpleasant feelings of anger, tension, anxiety, or depression roughly tripled in prevalence in both sexes between 2000 and 2014, from 1·4% (95% CI 1·0–2·0) to 4·0% (3·2–5·0) in men and boys, and from 2·1% (1·6–2·7) to 6·8% (6·0–7·8) in women and girls (figure 3). In 2000 and 2007, the prevalence of NSSH to cope with these feelings did not differ significantly by sex, but it was significantly more common in women and girls than in men and boys in 2014 (figure 3; appendix p 5). The prevalence of NSSH to cope with feelings was highest in women and girls aged 16–24 (17·7% [95% CI 13·9–22·3]). The corresponding prevalence in male 16–24-year-olds was 5·8% (95% CI 3·6–9·3). When those who reported NSSH in the self-completion section in 2014 were included, 22·4% (95% CI 18·0–27·5) of female 16–24-year-olds reported NSSH to cope (appendix p 5). Overall, 14·5% (95% CI 11·8–17·7) of people aged 16–24 years reported using NSSH to cope with feelings (appendix p 5). The proportion of participants reporting NSSH to change their situation increased overall, but less steeply than the proportion using NSSH as a coping mechanism (figure 3). The proportion of participants using NSSH to change their situation did not differ by sex in any of the three waves (figure 3; appendix p 5).
Figure 3.
Reasons for non-suicidal self-harm among men and boys (A) and women and girls (B) aged 16–74 years
Error bars show the 95% CIs.
The proportion of people who engaged in NSSH and reported no subsequent medical or psychological service contact remained stable between 2000 (51·2% [95% CI 42·2–60·0]) and 2007 (51·8% [47·3–56·4]), but increased somewhat in 2014 (59·4% [54·7–63·9]), although this increase was not significant (table 2). When participants in 2014 who reported NSSH only in the self-completion section were included, 62·6% (95% CI 58·9–66·1) reported no medical or psychological service contact after NSSH (table 2).
Table 2.
Medical or psychological service contact as a result of non-suicidal self-harm in 16–74-year-olds in England, 2000, 2007, and 2014
| n (% [95% CI]) | |
|---|---|
| 2000 | |
| No medical or psychological contact | 87 (51·2% [42·2–60·0]) |
| Medical contact only | 22 (14·6% [9·2–22·4]) |
| Psychological contact only | 22 (13·2% [8·2–20·8]) |
| Both medical and psychological contact | 39 (20·9% [14·9–28·5]) |
| 2007 | |
| No medical or psychological contact | 118 (51·8% [47·3–56·4]) |
| Medical contact only | 16 (7·1% [5·1–9·8]) |
| Psychological contact only | 41 (18·3% [14·4–23·1]) |
| Both medical and psychological contact | 54 (22·7% [18·8–27·1]) |
| 2014 | |
| No medical or psychological contact | 169 (59·4% [54·7–63·9]) |
| Medical contact only | 18 (4·0% [2·8–5·7]) |
| Psychological contact only | 54 (15·5% [13·1–18·3]) |
| Both medical and psychological contact | 77 (21·1% [17·7–25·0]) |
| 2014 (including self-completion reporting) | |
| No medical or psychological contact | 242 (62·6% [58·9–66·1]) |
| Medical contact only | 28 (4·6% [3·5–6·0]) |
| Psychological contact only | 59 (13·0% [11·1–15·2]) |
| Both medical and psychological contact | 95 (19·9% [17·0–23·1]) |
Women and girls who engaged in NSSH had roughly twice the odds of medical or psychological service contact that men and boys had (unadjusted OR 1·99 [95% CI 1·22–3·25]; table 3). Adjustment for sex, age, tenure, debt arrears, mental health, general health, method of self-harm, and ever attempting suicide, did not reduce these odds (table 3). Service contact after NSSH was also higher in people aged 35–74 years than in those aged 16–34 years in both adjusted and unadjusted analyses (table 3). People living in rented accommodation were more likely than owner-occupiers to have contact with services in all three analyses (table 3). None of the other socioeconomic indicators tested, such as educational qualifications, household income, and area-level deprivation, was significant, and they were therefore not retained in models (data not shown).
Table 3.
Odds ratios for self-reported medical or psychological service contact as a result of non-suicidal self-harm in 16–74-year-olds in England, 2014
|
Unadjusted |
Model 1* |
Model 2† |
|||||
|---|---|---|---|---|---|---|---|
| Odds ratio (95% CI) | p value | Odds ratio (95% CI) | p value | Odds ratio (95% CI) | p value | ||
| Sex | |||||||
| Male | Reference | .. | Reference | .. | Reference | .. | |
| Female | 1·99 (1·22–3·25) | 0·006 | 2·40 (1·41–4·08) | 0·001 | 2·49 (1·43–4·25) | 0·001 | |
| Age, years | |||||||
| 16–34 | Reference | .. | Reference | .. | Reference | .. | |
| 35–74 | 1·67 (1·08–2·57) | 0·022 | 1·89 (1·15–3·10) | 0·012 | 1·82 (1·06–3·11) | 0·029 | |
| Tenure | |||||||
| Owner occupier | Reference | .. | Reference | .. | Reference | .. | |
| Renter | 2·65 (1·64–4·29) | <0·0001 | 2·58 (1·47–4·51) | 0·001 | 2·59 (1·45–4·63) | 0·001 | |
| In debt arrears | |||||||
| Not in arrears | Reference | .. | Reference | .. | Reference | .. | |
| Arrears in past year | 1·16 (0·68–1·96) | 0·587 | 0·76 (0·42–1·39) | 0·378 | 0·67 (0·36–1·24) | 0·202 | |
| CIS–R score | |||||||
| CIS–R less than 18 | Reference | .. | Reference | .. | Reference | .. | |
| CIS–R 18 or more | 2·43 (1·51–3·91) | <0·0001 | 1·95 (1·15–3·31) | 0·013 | 1·42 (0·80–2·52) | 0·234 | |
| General health | |||||||
| Excellent or very good | Reference | .. | Reference | .. | Reference | .. | |
| Poor, fair or good | 2·78 (1·74–4·45) | <0·0001 | 2·00 (1·17–3·42) | 0·011 | 1·63 (0·93–2·87) | 0·090 | |
| Self-harm method | |||||||
| Used other method only | Reference | .. | .. | .. | Reference | .. | |
| Self-cut | 1·37 (0·87–2·15) | 0·170 | .. | .. | 1·31 (0·77–2·22) | 0·314 | |
| Ever attempted suicide | |||||||
| Had not made an attempt | Reference | .. | .. | .. | Reference | .. | |
| Had made a suicide attempt | 4·13 (2·58–6·62) | <0·0001 | .. | .. | 3·25 (1·91–5·53) | <0·0001 | |
CIS-R=Clinical Interview Schedule—Revised.
Adjusted for sex, age, tenure, debt arrears, mental health, and general health.
Adjusted for sex, age, tenure, debt arrears, mental health, general health, method of self-harm, and ever attempting suicide.
People with worse mental (unadjusted OR 2·43 [95% CI 1·51–3·91]) or general (2·78 [1·74–4·45]) health were more likely to have contact with services after NSSH than were those with better mental or general health. After adjustment for the nature of self-harming behaviour, these associations weakened, and were no longer significant (table 3). In both unadjusted (OR 4·13 [95% CI 2·58–6·62]) and adjusted (3·25 [1·91–5·53]) analyses, the odds of reporting service contact after NSSH were increased in people who had at some point also made a suicide attempt (table 3).
Discussion
In an analysis of data from high-quality cross-sectional surveys of the English population, we noted steep increases in the lifetime prevalence of self-reported NSSH between 2000 and 2014. This increase was evident in both men and boys and in women and girls, and across all age groups. The absolute rise was greatest in female 16–24-year-olds, in whom the proportion increased from 6·5% (95% CI 4·2–10·0) in 2000, to 19·7% (15·7–24·5) in 2014 (with the bulk of the increase occurring since 2007).
Sex specific rises in self-harm (with and without suicidal intent) have previously been reported in service settings in Denmark,9 Ireland,8 and England.2 The rise in the prevalence of NSSH in our study was largely because of an increased prevalence of self-cutting, from 1·5% (95% CI 1·2–1·8) in 2000, to 3·9% in 2014 (3·5–4·5). This increase was more pronounced in women and girls than in men and boys, and in 2014 self-cutting was significantly more common in female than in male participants. We found no evidence of an increase in self-poisoning. There was some indication of an increase in self-burning among men between 2000 and 2007, although numbers were low and this finding should be treated with caution. Our findings for self-cutting and self-poisoning were consistent with those of previous research.7
The number of people using NSSH to relieve unpleasant feelings of anger, tension, anxiety, or depression roughly tripled between 2000 and 2014, and the prevalence of NSSH to try to change a situation roughly doubled. Although the use of NSSH as a coping strategy increased steeply across the population, it was most pronounced in young people. More than 10% of young people reported having self-harmed to relieve unpleasant feelings of anger, tension, anxiety, or depression in the 2014 wave. This finding is important because individuals who start to self-harm when young might adopt the behaviour as a long-term coping strategy.12 There is also a risk that the behaviour could lead in time to increases in suicides and suicide attempts.30 Since 2010, an upward trend in suicide has been evident among people aged younger than 20 years in the UK.29 Anxiety and depression in the English general population have also increased in children31 and young women.18 The factors underlying these adverse trends in young people's mental health are unclear and require further research to inform appropriate prevention strategies.32
At least half of those who reported NSSH also reported no subsequent medical or psychological contact as a result, consistent with the findings of previous research.10 Thus, studies of the prevalence of NSSH in service users will be affected by the determinants of contact. In 2014, in our analyses, contact with health services was less likely in male participants than in female participants, and in younger participants than in older participants (in analyses adjusted for sex, age, tenure, debt arrears, mental health, general health, method of NSSH and previous suicide attempts). Service contact after NSSH was more common among people with poor general or mental health than among those with good health, perhaps because they were more likely to be in contact with services already. We also found that service contact was increased in those who had also made a suicide attempt, perhaps because of a need for medical treatment. Overall, between 2000 and 2014, we noted no evidence of an increase in treatment contact among people who self-harmed, suggesting that changes in the prevalence of NSSH in health-care settings probably reflect changes in the community prevalence of NSSH.
The repeat probability-sample surveys of whole adult populations with consistent methods that we analysed provide valuable evidence about temporal trends in NSSH. However, such surveys inevitably have limitations. First, precision of some estimates is low because of the small numbers of participants reporting NSSH, especially in the 2000 survey, in which the prevalence of NSSH was lowest. Second, the findings could be subject to bias due to non-participation, although the response rate—69% in 2000, and 57% in 2007 and 2014—was in line with that in similar surveys.23 Mental health is associated with the propensity to take part in surveys and could affect our estimates of the prevalence of NSSH.24 The development of non-response weights to address participation biases from known characteristics have been described previously.18 However, non-response weighting has little effect on results, suggesting that non-responders were similar to responders in many characteristics. Third, in terms of balancing comparability and validity, we prioritised consistency over improvement or updating of survey questions. The issue of self-harm intent is complex and the answers that participants could select about motivations were reductive. Even with open questions, reasons given could reflect subsequent rationalisations.21 Use of the word “attention” could have been interpreted as an implication that NSSH is attention seeking, which could have led to people not choosing endorsing this option. The coping or affect regulation model of self-harm is now much more widely accepted.25 Although methods largely remained consistent across the three survey waves, mode changes could have affected the trends reported. In 2000 and 2007, the follow-up questions were asked face to face, whereas in 2014 they were part of the self-completion interview. More socially stigmatised feelings and behaviours might thus be underreported in 2000 and 2007.26 To maximise cross-wave comparability, data for methods of, reasons for, and service contact after NSSH were restricted to those participants who reported NSHH face to face. These prevalences should thus be considered consistent underestimates.
Fourth, some of the increased reporting of NSSH could reflect changing conceptualisations of NSSH: behaviours that people did not deem NSSH in previous surveys could be more likely to be included in 2014. Furthermore, as NSSH has become less stigmatised, some people might have felt more able to disclose it in later surveys.27 Previous underreporting could mean that the actual increase in NSSH is less pronounced than our findings suggest. Fifth, the sample was too small for robust analysis by ethnic group, and questions might not have captured how NSSH manifests in different ethnic groups. No option was presented for punching or hitting against something—methods of NSSH that are more common in men than in women.28 Although these methods of NSSH could have been captured by the “other” response option, not having a direct prompt could have led to underreporting. Finally, our lifetime indicator did not take into account frequency or recency of NSSH. Although participants were asked about engaging in NSSH in the past year in the 2014 survey, this question was not included in 2000 or 2007, so trends could not be examined.
In conclusion, we found an increase in the prevalence of NSSH in all age groups in England, but particularly in young women and girls. An increase in the prevalence of using self-harm to cope with emotional stress could have serious long-term public health implications. There is a risk that self-harm will become normalised for young people. Furthermore, NSSH increases the risk of later suicide; a cohort effect is possible by which suicide rates in these groups could potentially increase. Young people need health and educational services to be available, and health and other professionals need to discuss self-harm with young people and encourage them to find safer ways of coping.
Data sharing
The Adult Psychiatric Morbidity Surveys datasets are in the UK Data Service archive. NHS Digital manages the survey series and reviews requests for access to the latest dataset. Requests for access to the 2014 dataset that we used in this analysis should be made to the Data Access Request Service at NHS Digital.
Acknowledgments
Acknowledgments
The English Department of Health and Social Care is the primary funder of the Adult Psychiatric Morbidity Surveys, which were commissioned by NHS Digital. Our analyses were independent research funded by the National Institute for Health Research (NIHR) Policy Research Programme (PHPEHF50/27; 023/0167). DG is supported by the NIHR Biomedical Research Centre at University Hospitals Bristol NHS Foundation Trust. PEB acknowledges the support of the University College London Hospitals NIHR Biomedical Research Centre. LMH is supported by the NIHR Biomedical Research Centre at the South London Maudsley NHS Foundation Trust and Kings College London. The views expressed in this Article are those of the authors and not necessarily those of the NIHR or the Department of Health and Social Care. We are indebted to the tens of thousands of people across England who generously participated in Adult Psychiatric Morbidity Surveys.
Contributors
SM, CC, PEB, TB, RJ, AH, and SW contributed to survey design and conduct. All authors advised on the design and conduct of secondary analyses. SM did the analyses and drafted the Article, which was critically reviewed and approved by all authors.
Declaration of interests
We declare no competing interests.
Supplementary Material
References
- 1.Klonsky ED, Victor SE, Saffer BY. Nonsuicidal self-injury: what we know, and what we need to know. Can J Psychiatry. 2014;59:565–568. doi: 10.1177/070674371405901101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Morgan C, Webb R, Carr M. Incidence, clinical management, and mortality risk following self harm among children and adolescents: cohort study in primary care. BMJ. 2017;359:j4351. doi: 10.1136/bmj.j4351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hawton K, Harriss L, Zahl D. Deaths from all causes in a long-term follow-up study of 11 583 deliberate self-harm patients. Psychol Med. 2006;36:397–405. doi: 10.1017/S0033291705006914. [DOI] [PubMed] [Google Scholar]
- 4.Cipriano A, Cella S, Cotrufo P. Nonsuicidal self-injury: a systematic review. Front Psychol. 2017;8:1946. doi: 10.3389/fpsyg.2017.01946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Muehlenkamp JL, Claes L, Havertape L, Plener PL. International prevalence of adolescent non-suicidal self-injury and deliberate self-harm. Child Adolesc Psychiatry Ment Health. 2012;6:10. doi: 10.1186/1753-2000-6-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Armitage CJ, Rahim WA, Rowe R, O'Connor RC. Trends in self-harm in Kuala Lumpur, 2005–2011. Arch Suicide Res. 2016;20:22–28. doi: 10.1080/13811118.2015.1004493. [DOI] [PubMed] [Google Scholar]
- 7.Geulayov G, Kapur N, Turnbull P. Epidemiology and trends in non-fatal self-harm in three centres in England, 2002–2012: findings from the Multicentre Study of Self-harm in England. BMJ Open. 2016;6:6. doi: 10.1136/bmjopen-2015-010538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Griffin E, McMahon E, McNicholas F, Corcoran P, Perry IJ, Arensman E. Increasing rates of self-harm among children, adolescents and young adults: A 10-year national registry study 2007–2016. Soc Psychiatry Psychiatr Epidemiol. 2018;53:663–671. doi: 10.1007/s00127-018-1522-1. [DOI] [PubMed] [Google Scholar]
- 9.Morthorst BR, Soegaard B, Nordentoft M, Erlangsen A. Incidence rates of deliberate self-harm in Denmark 1994–2011: a nationwide register study. Crisis. 2016;37:256–264. doi: 10.1027/0227-5910/a000391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Geulayov G, Casey D, McDonald KC. Incidence of suicide, hospital-presenting non-fatal self-harm, and community-occurring non-fatal self-harm in adolescents in England (the iceberg model of self-harm): a retrospective study. Lancet Psychiatry. 2017;5:167–174. doi: 10.1016/S2215-0366(17)30478-9. [DOI] [PubMed] [Google Scholar]
- 11.O'Connor R, Wetherall K, Cleare S. Suicide attempts and non-suicidal self-harm: national prevalence study of young adults. BJPsych Open. 2018;4:142–148. doi: 10.1192/bjo.2018.14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mars B, Heron J, Crane C. Differences in risk factors for self-harm with and without suicidal intent: findings from the ALSPAC cohort. J Affect Disord. 2014;168:407–414. doi: 10.1016/j.jad.2014.07.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Office for National Statistics . Office for National Statistics; London: 2014. The coverage of the postcode address file and address base for sampling. [Google Scholar]
- 14.Hawton K, Linsell L, Adeniji T, Sariaslan A, Fazel SF. Self-harm in prisons in England and Wales: an epidemiological study of prevalence, risk factors, clustering, and subsequent suicide. Lancet. 2014;383:1147–1154. doi: 10.1016/S0140-6736(13)62118-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Office for National Statistics . Office for National Statistics; London: 2015. 2011 census analysis: what does the 2011 census tell us about people living in communal establishments? [Google Scholar]
- 16.Singleton N, Bumpstead R, O'Brien M, Lee A, Meltzer H. Her Majesty's Stationery Office; London: 2001. Psychiatric morbidity among adults living in private households, 2000. [DOI] [PubMed] [Google Scholar]
- 17.McManus S, Meltzer H, Brugha T, Bebbington PE, Jenkins R. Health and Social Care information Centre; Leeds: 2009. Adult psychiatric morbidity in England, 2007: results of a household survey. [Google Scholar]
- 18.McManus S, Bebbington PE, Jenkins R, Brugha T. NHS Digital; Leeds: 2016. Mental health and wellbeing in England: Adult Psychiatric Morbidity Survey 2014. [Google Scholar]
- 19.American Psychiatric Association . 5th edn. American Psychiatric Association; Washington, DC: 2013. Diagnostic and statistical manual of mental disorders. [Google Scholar]
- 20.Plener PL, Fegert JM. Nonsuicidal self-injury: a condition for further study. Child Adolesc Psychiatry Ment Health. 2015;9:30. doi: 10.1186/s13034-015-0067-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kapur N, Cooper J, O'Connor RC, Hawton K. Non-suicidal self-injury vs attempted suicide: new diagnosis or false dichotomy? Br J Psychiatry. 2013;202:326–328. doi: 10.1192/bjp.bp.112.116111. [DOI] [PubMed] [Google Scholar]
- 22.Lewis G, Pelosi AJ, Araya R, Dunn G. Measuring psychiatric disorder in the community; a standardised assessment for use by lay interviewers. Psychol Med. 1992;22:465–486. doi: 10.1017/s0033291700030415. [DOI] [PubMed] [Google Scholar]
- 23.Barnes W, Bright G, Hewat C. Office for National Statistics; London: 2010. Making sense of Labour Force Survey response rates. [Google Scholar]
- 24.Knudsen AK, Hotopf M, Skogen JC, Øverland S, Mykletun A. The health status of nonparticipants in a population-based health study. Am J Epidemiol. 2010;172:130614. doi: 10.1093/aje/kwq257. [DOI] [PubMed] [Google Scholar]
- 25.Laye-Gindhu A, Schonert-Reichi KA. Nonsuicidal self-harm among community adolescents: understanding the ‘whats’ and ‘whys’ of self-harm. J Youth Adolesc. 2005;34:447–457. [Google Scholar]
- 26.Tourangeau R, Rips L, Rasinski K. Cambridge University Press; Cambridge: 2000. The psychology of survey response. [Google Scholar]
- 27.Wiens K, Williams JVA, Lavorato DH. Is the prevalence of major depression increasing in the Canadian adolescent population? Assessing trends from 2000 to 2014. J Affect Disord. 2017;210:22–26. doi: 10.1016/j.jad.2016.11.018. [DOI] [PubMed] [Google Scholar]
- 28.Bresin K, Schoenleber Gender differences in the prevalence of nonsuicidal self-injury: a meta-analysis. Clin Psychol Rev. 2015;31:35–64. doi: 10.1016/j.cpr.2015.02.009. [DOI] [PubMed] [Google Scholar]
- 29.Office for National Statistics Suicides in the UK. https://www.ons.gov.uk/peoplepopulationandcommunity/birthsdeathsandmarriages/deaths/datasets/suicidesintheunitedkingdomreferencetables
- 30.Mars B, Heron J, Klonsky ED. Predictors of future suicide attempt among adolescents with suicidal thoughts or non-suicidal self-harm: a population-based birth cohort study. Lancet Psychiatry. 2019;6:327–337. doi: 10.1016/S2215-0366(19)30030-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Sadler K, Vizard T, Ford T, Goodman A, Goodman R, McManus S. NHS Digital; Leeds: 2018. Trends and characteristics: Mental Health of Children and Young People in England 2017. [Google Scholar]
- 32.Gunnell D, Kidger J, Elvidge H. Adolescent mental health in crisis. BMJ. 2018;361:k2608. doi: 10.1136/bmj.k2608. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The Adult Psychiatric Morbidity Surveys datasets are in the UK Data Service archive. NHS Digital manages the survey series and reviews requests for access to the latest dataset. Requests for access to the 2014 dataset that we used in this analysis should be made to the Data Access Request Service at NHS Digital.