Abstract
Background
Previous studies have shown that RNA Polymerase III Subunit G (POLR3G) has oncogenic effects in cultured cells and mice. However, the role of POLR3G in transitional cell carcinoma (TCC) has not been reported. This study explores the potential of POLR3G as a novel molecular marker for TCC.
Methods
The RNA sequencing data and clinical information of patients with TCC were downloaded from The Cancer Genome Atlas official website. Transcriptome analysis was performed as implemented in the edgeR package to explore whether POLR3G was up-regulated in TCC tissues compared to normal bladder tissues. The expression of POLR3G in bladder cancer cell line T24 and human uroepithelial cell line SV-HUC-1 were detected via quantitative real time polymerase chain reaction (qRT-PCR). Correlations between POLR3G expression and clinicopathological characteristics were analyzed using Mann-Whitney U test or Kruskal-Wallis H test. Clinicopathological characteristics associated with overall survival were explored using the Kaplan-Meier method and Cox regression analyses. Gene set enrichment analysis (GSEA) was performed to explore the associated gene sets enriched in different POLR3G expression phenotypes and the online tool Tumor IMmune Estimation Resource (TIMER) was used to explore the correlation between POLR3G expression and tumor immune infiltration in TCC.
Results
Transcriptome analysis showed that POLR3G was significantly up-regulated in TCC tissues compared to normal bladder tissues. Furthermore, qRT-PCR revealed high expression of POLR3G in T24 cells compared to SV-HUC-1 cells. Overall, POLR3G expression was associated with race, tumor status, tumor subtype, T classification, and pathological stage. Kaplan-Meier survival analysis revealed that higher POLR3G expression was associated with lower overall survival. The univariate Cox regression model revealed that age at diagnosis, pathological stage, and POLR3G expression were associated with prognosis of TCC patients. Further multivariate analyses identified these three clinicopathological characteristics as independent prognostic factors for overall survival. GSEA analysis showed that several gene sets associated with tumor development and metastasis, including TGF-β signaling, PI3K-AKT-mTOR signaling, and IL6-JAK-STAT3 signaling, were significantly enriched in POLR3G high expression phenotype. Immune infiltration analysis revealed that the expression of POLR3G was significantly correlated with infiltrating levels of immune cells, including CD8+ T cells, neutrophils, and dendritic cells; and the expression of POLR3G was also significantly correlated with the expression of immune checkpoint molecules, such as PD1, PD-L1, PD-L2, CTLA4, LAG3, HAVCR2, and TIGIT.
Conclusions
POLR3G was up-regulated in TCC and high POLR3G expression correlated with poor prognosis. POLR3G can potentially be used as a prognostic marker for TCC and might be of great value in predicting the response to immunotherapy.
Keywords: Transitional cell carcinoma, POLR3G, Biomarker, TCGA, Tumor immue infiltration, Prognosis
Introduction
Bladder cancer is the 7th most commonly diagnosed cancer in males and the 11th most commonly diagnosed cancer when both genders are considered (Ferlay et al., 2013). In 2020, an estimated 81,400 new cases of bladder cancer (62,100 men; 19,300 women) will be diagnosed in the United States of America and approximately 17,980 deaths (13,050 men; 4,930 women) will occur during the same period of time (Siegel, Miller & Jemal, 2020). Transitional cell carcinoma (TCC) is the most common histological type of bladder cancer, contributing to more than 90% of all bladder cancer cases (Witjes et al., 2020). Approximately 75% of patients with bladder cancer are present with non-muscle-invasive bladder cancer (NMIBC) at the initial diagnosis, while the remaining 25% of patients are present with muscle-invasive bladder cancer (MIBC) or metastatic bladder cancer (Witjes et al., 2020). The standard treatment for NMIBC is trans-urethral resection of bladder tumor (TURBT) followed by intravesical chemotherapy or bacillus Calmette-Guérin (BCG) immunotherapy depending on risk stratifications. For MIBC, on the other hand, neoadjuvant chemotherapies followed by radical cystectomy are first line recommendations. However, the prognosis for MIBC is poor even with effective treatments. The five-year recurrence-free survival rate was 89% for patients with T2 tumors, 50% for patients with T4 tumors, and 35% for patients with lymph node metastasis respectively (Stein et al., 2001). Patients with NMIBCs have better prognoses, however, high grade NMIBC has a 70% recurrence rate with a 15%–40% risk of progression after five years (Kashif Khan, Ahmed & Raza, 2014).
For TCC, the most important histopathological prognostic variables are tumor stage and lymph node status (Dutta et al., 2016; Stein et al., 2001). However, no predictive molecular markers are routinely used in clinical practice. Thus, identifying effective markers is essential for predicting prognoses and directing treatments for patients with TCC. Although previous studies have revealed that RNA Polymerase III Subunit G (POLR3G) overexpression can have oncogenic effects in cultured cells and mice (Haurie et al., 2010; Khattar et al., 2016), its role in TCC has still not been reported. Herein, the aim of this study is to evaluate the correlation between POLR3G and prognoses of patients with TCC.
Materials & Methods
Data acquisition
The RNA sequencing (RNA-seq) data (Workflow types: HTSeq-FPKM; HTSeq-Counts) and corresponding clinical information of patients with TCC (Project: TCGA-BLCA, Disease type: transitional cell papillomas and carcinomas) were downloaded from GDC Data Portal (https://portal.gdc.cancer.gov/). Counts data were used for transcriptome analysis. TPM data were calculated based on FPKM data, and were used for further analysis. Only patients with both RNA-seq data and survival information were included in this study.
Cell lines and cell culture
Human bladder cancer cell line T24 and immortalized normal urothelial cell line SV-HUC-1 were purchased from National Infrastructure of Cell Line Resource (Beijing, China). Cell lines were maintained in Roswell Park Memorial Institute (RPMI) 1640 medium (Gibco) supplemented with 10% fetal bovine serum (Gibco) and 1% penicillin/streptomycin (Gibco). All cells were maintained in a humidified atmosphere with 5% CO2 at 37 °C.
RNA extraction and qRT-PCR
Total RNA was extracted from cells using the RNA simple Total RNA Kit (Tiangen). FastQuant RT Kit (Tiangen) was used for cDNA synthesis. The quantitative real time polymerase chain reactions (qRT-PCR) were performed using KAPA SYBR FAST Universal q-PCR Kit (KAPA). The relative mRNA levels of genes were calculated using cycle threshold (CT) methods, and β-actin was used as an endogenous control. Three replicate samples were studied for detection of mRNA expression. The primers were listed below: POLR3G (forward): 5′-CGCAGGCAAAGGCACAC-3′; POLR3G (reverse): 5′-CCTCTTTTTTCCAA TTCCTCCA-3′; β-actin (forward): 5′-CCAACCGCGAGAAGATGA-3′; β-actin (reverse): 5′-CCAGAGGCGTACAGGGATAG-3′.
Gene set enrichment analysis
Gene set enrichment analysis (GSEA) is widely applied to determine whether predefined gene sets are differentially expressed in different phenotypes (Subramanian et al., 2005). To identify signaling pathways that are differentially activated in TCCs, we conducted GSEA analysis between high and low POLR3G expression groups. GSEA analysis was performed using GSEA software (version 4.0.3). The h.all.v7.1.symbols.gmt (hallmark) dataset was obtained from the Molecular Signatures Database (MsigDB) (Liberzon et al., 2015). Enrichment analysis was performed by default weighted enrichment statistics, with the random combinatorial count set as 1,000. Gene sets were judged as significantly enriched by P < 0.05 as well as false discovery rates (FDR) < 0.25.
Tumor infiltrating immune cells and immune checkpoint molecule expression analysis
Tumor IMmune Estimation Resource (TIMER) (Li et al., 2017) is a web server for comprehensive analysis of tumor-infiltrating immune cells, which applies a previously published statistical approach called the deconvolution that uses the gene expression profiles to produce an inference on the number of tumor-infiltrating immune cells (Li et al., 2016). Survival module was used to explore the association between immune cell infiltration (B cells, CD4+ T cells, CD8+ T cells, neutrophils, macrophages, and dendritic cells) and clinical outcome in bladder cancer. Gene module was used to explore the correlations between the expression of POLR3G and immune cell infiltration. Correlation module was used to explore the correlations between POLR3G expression and immune checkpoint molecule expression, including PDCD1 (also known as PD1), CD274 (also known as PD-L1), PDCD1LG2 (also known as PD-L2), CTLA4, LAG3, HAVCR2, and TIGIT.
Statistical analysis
The data processing and further statistical analyses were performed using R (v.3.6.3)
Transcriptome analysis of the differentially expressed genes (DEGs) in the TCC tissues and normal bladder tissues was performed using edgeR package (Robinson, McCarthy & Smyth, 2010). The differential expression of POLR3G between T24 cells and SV-HUC-1 cells was analyzed via independent t test. The relationships between clinicopathological characteristics and POLR3G expression were analyzed using the Mann–Whitney U test or Kruskal-Wallis H test. The Kaplan–Meier method and Cox regression models were used to explore the influence of POLR3G expression on overall survival along with other clinicopathological characteristics (age at diagnosis, gender, race, and pathological stage). The cut-off value of POLR3G expression was determined by its median value. P < 0.05 was considered to indicate a statistically significant difference.
Results
Clinical characteristics
The clinical characteristics of 404 patients with TCC in The Cancer Genome Atlas (TCGA) are presented in Table 1. There were 299 (74.01%) male patients and 105 (25.99%) female patients with a median age of 69 years old at the time of diagnosis. Race information was available for 388 patients, among which 322 (82.99%) patients were white, 43 (11.08%) were Asian, and 23 (5.93%) were black or African American. At least 202 (63.72%) patients were tumor free while 115 (36.28%) patients still had tumors. Overall, 2 (0.50%) of the patients showed stage I, 129 (32.09%) stage II, 137 (34.08%) stage III, and 134 (33.33%) stage IV. Among 363 patients diagnosed with clear N stage, 129 (35.54%) had lymph node metastases. From 205 patients diagnosed with clear M stage, 11 (5.37%) had distant metastases. Median follow-up for subjects alive at last contact was 21.3 months (range 0–169 months).
Table 1. Patient characteristics of patients with TCC in TCGA.
| Clinical characteristics | Total (n = 404) | Percentage (%) |
|---|---|---|
| Age at diagnosis (y) | ||
| ≤60 | 86 | 21.34 |
| >60 | 317 | 78.66 |
| Gender | ||
| Female | 105 | 25.99 |
| Male | 299 | 74.01 |
| Race | ||
| White | 322 | 82.99 |
| Asian | 43 | 11.08 |
| Black or African American | 23 | 5.93 |
| Tumor status | ||
| With tumor | 115 | 36.28 |
| Tumor free | 202 | 63.72 |
| Tumor subtype | ||
| Papillary | 110 | 32.93 |
| Non-papillary | 224 | 67.07 |
| T classification | ||
| T1 | 3 | 0.81 |
| T2 | 119 | 32.08 |
| T3 | 192 | 51.75 |
| T4 | 57 | 15.36 |
| Lymph node metastasis | ||
| Negative | 234 | 64.46 |
| Positive | 129 | 35.54 |
| Distant metastasis | ||
| Negative | 194 | 94.63 |
| Positive | 11 | 5.37 |
| Pathological stage | ||
| Stage I | 2 | 0.50 |
| Stage II | 129 | 32.09 |
| Stage III | 137 | 34.08 |
| Stage IV | 134 | 33.33 |
Notes.
- TCC
- Transitional cell carcinoma
- TCGA
- The Cancer Genome Atlas
POLR3G was up-regulated in multiple cancer types including TCC
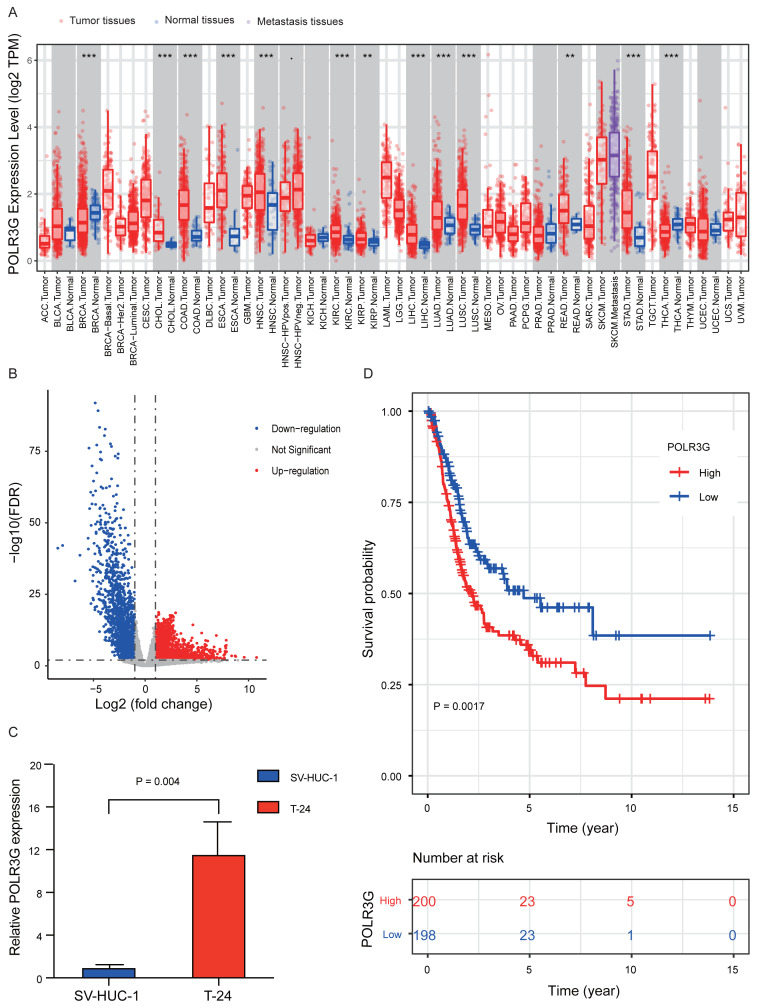
TIMER analyses revealed that POLR3G expression was up-regulated in multiple cancer types, including cholangiocarcinoma, colon adenocarcinoma, esophageal carcinoma, kidney renal clear cell carcinoma. (Fig. 1A). RNA-Seq differential expression analysis revealed that 2,211 genes were up-regulated (log2FC > 1, and FDR < 0.01) in TCC tissues compared to normal bladder tissues, including POLR3G (log2FC = 1.038, FDR = 0.006), and 1,853 genes were down-regulated (log2FC <-1, and FDR <0.01). (Fig. 1B and Table S1). Furthermore, qRT-PCR results showed higher expression levels of POLR3G in T24 cells compared to SV-HUC-1 cells (P = 0.004; Fig. 1C).
Figure 1. POLR3G expression in different disease states and survival curve of patients with TCC.
(A) Differential expressions of POLR3G in multiple cancer types analyzed by TIMER. P value significant codes: 0 ≤ *** < 0.001 ≤ ** < 0.01 ≤ * < 0.05 ≤ . < 0.1 (B) RNA-Seq differential expression analysis in TCC tissues and normal bladder tissues. (C) Differential expressions of POLR3G in T24 cells compared to SV-HUC-1 cells. (D) Impact of POLR3G expression on overall survival of patients with TCC in TCGA.
Relationship between POLR3G expression and clinicopathological characteristics
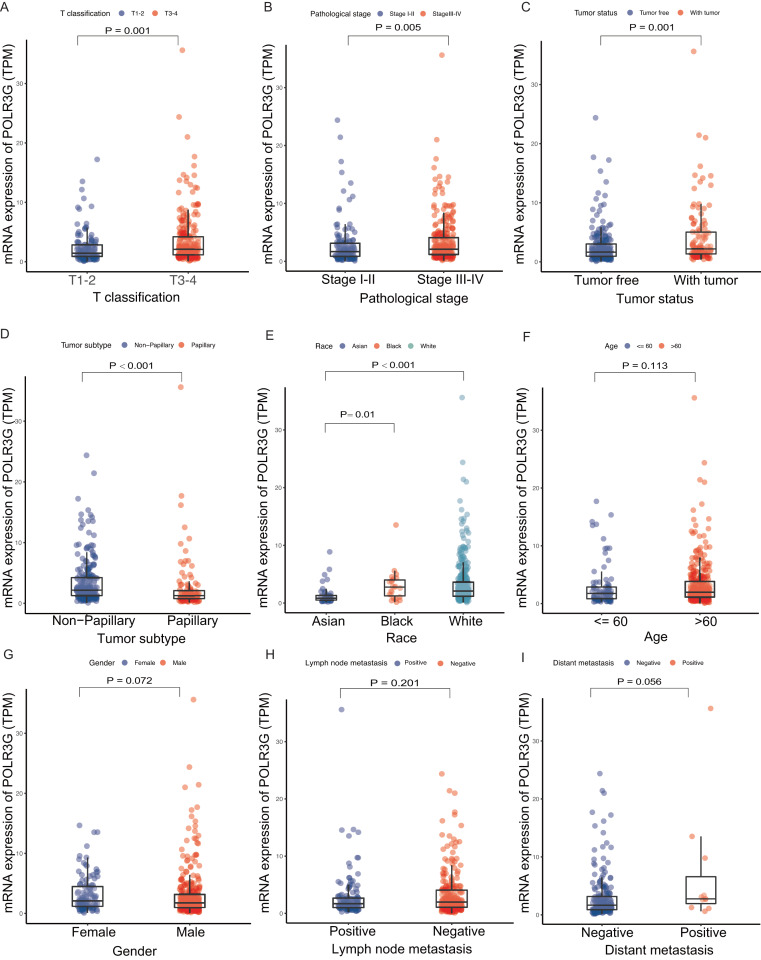
Expression levels of POLR3G were strongly correlated with T classification (T1-2 vs. T3-4, P = 0.001; Fig. 2A), pathological stage (stage I-II vs. stage III-IV, P = 0.005; Fig. 2B), tumor status (tumor free vs. with tumor, P = 0.001; Fig. 2C), tumor subtype (papillary vs. non-papillary, P < 0.001; Fig. 2D), and race (P < 0.001; Fig. 2E). No statistically significant differences were observed between groups stratified by age (≤ 60 years old vs. >60 years old, P = 0.113; Fig. 2F), gender (female vs. male, P = 0.072; Fig. 2G), lymph node metastasis (positive vs. negative, P = 0.201; Fig. 2H), and distant metastasis (positive vs. negative, P = 0.056; Fig. 2I).
Figure 2. Association with POLR3G expression and clinicopathological characteristics.
Clinicopathologic characteristics included were listed as followed: (A) T classification. (B) Pathological stage. (C) Tumor status. (D) Tumor subtype. (E) Race. (F) Age at diagnosis. (G) Gender. (H) Lymph node metastasis. (I) Distant metastasis.
Survival outcomes and Cox regression analysis
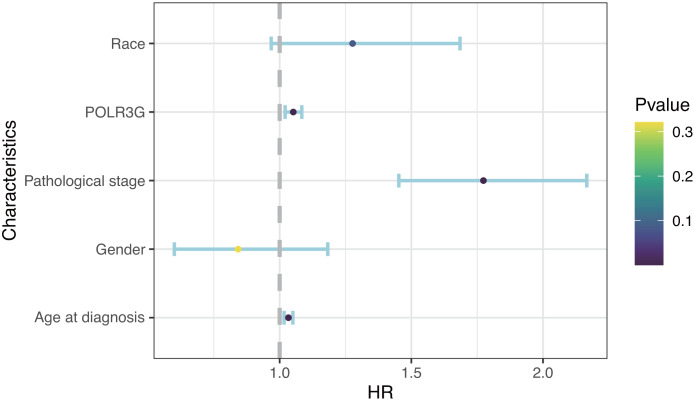
Kaplan–Meier survival analysis revealed that higher expression of POLR3G was associated with worse prognoses (P = 0.002; Fig. 1D). The univariate Cox regression model revealed that age at diagnosis (HR = 1.03, 95% CI = 1.02 to 1.05, P < 0.001), pathological stage (HR = 1.71, 95% CI = 1.41 to 2.08, P < 0.001), and POLR3G expression (HR = 1.04, 95% CI = 1.01 to 1.07, P = 0.02) were associated with overall survival of patients with TCC. Furthermore, multivariate Cox regression after adjustment indicated that age at diagnosis (HR = 1.03, 95% CI = 1.02 to 1.05, P < 0.001), pathological stage (HR = 1.77, 95% CI = 1.45 to 2.17, P < 0.001), and POLR3G expression (HR = 1.05, 95% CI = 1.02 to 1.08, P = 0.001) were independent prognostic factors for overall survival in patients with TCC (Table 2, Fig. 3).
Table 2. Univariate and multivariate Cox regression analysis of overall survival.
| Characteristics (n = 381) | Univariate analysis | Multivariate analysis | ||
|---|---|---|---|---|
| HR (95% CI) | P value | HR (95% CI) | P value | |
| Age at diagnosis | 1.03 (1.02–1.05) | <0.001 | 1.03 (1.02–1.05) | <0.001 |
| Gender | 0.82 (0.59–1.16) | 0.263 | 0.84 (0.60–1.18) | 0.321 |
| Race | 1.04 (0.78–1.38) | 0.783 | 1.28 (0.97–1.68) | 0.084 |
| Pathological stage | 1.71 (1.41–2.08) | <0.001 | 1.77 (1.45–2.17) | <0.001 |
| POLR3G expression | 1.04 (1.01–1.07) | 0.021 | 1.05 (1.02–1.08) | 0.001 |
Notes.
- HR
- hazard ratio
- CI
- confidence interval
Figure 3. Multivariate Cox analysis of POLR3G expression and other clinicopathological characteristics.
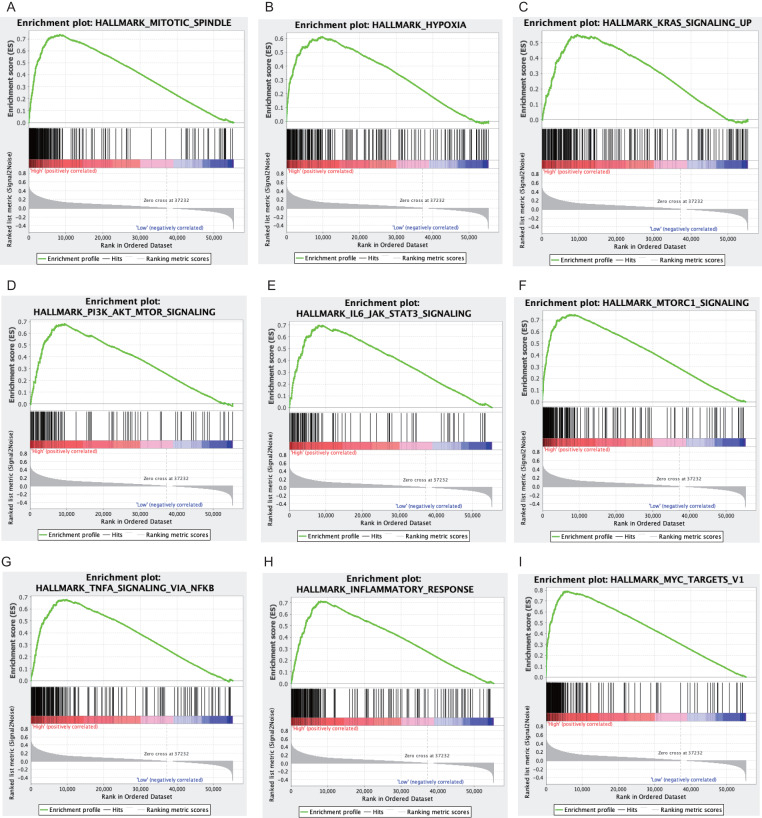
Gene sets enriched in POLR3G high expression phenotype
In the hallmark dataset, 41 gene sets were significantly enriched in POLR3G high expression phenotype (Table 3). Several of the gene sets are associated with oncogenesis, progression, and metastasis of cancer, such as mitotic spindle, hypoxia, Kras signaling up, PI3K-AKT-mTOR signaling, IL6-JAK-STATS3 signaling, mTORC1 signaling, TNF- α signaling via NF- κB, inflammatory response, and Myc targets v1(Figs. 4A–4I).
Table 3. Gene sets enriched in POLR3G high expression phenotype.
| Gene set | NES | NOM P value | FDR q value |
|---|---|---|---|
| IL6 JAK STAT3 signaling | 2.83 | <0.001 | <0.001 |
| Allograft rejection | 2.72 | <0.001 | <0.001 |
| mTORC1 signaling | 2.7 | <0.001 | <0.001 |
| Protein secretion | 2.69 | <0.001 | <0.001 |
| Inflammatory response | 2.67 | <0.001 | <0.001 |
| Glycolysis | 2.58 | <0.001 | <0.001 |
| Heme metabolism | 2.56 | <0.001 | <0.001 |
| Mitotic spindle | 2.53 | <0.001 | <0.001 |
| Androgen response | 2.46 | <0.001 | <0.001 |
| Interferon-γ response | 2.46 | <0.001 | <0.001 |
| TNF-α signaling via NF-kB | 2.44 | <0.001 | <0.001 |
| PI3K AKT mTOR signaling | 2.42 | <0.001 | <0.001 |
| G2M checkpoint | 2.36 | <0.001 | <0.001 |
| Hypoxia | 2.34 | <0.001 | <0.001 |
| UV response down | 2.32 | <0.001 | <0.001 |
| Apical junction | 2.28 | <0.001 | <0.001 |
| Kras signaling up | 2.28 | <0.001 | <0.001 |
| Complement | 2.28 | <0.001 | <0.001 |
| Myc targets v1 | 2.22 | <0.001 | <0.001 |
| Unfolded protein response | 2.18 | <0.001 | 0.006 |
| UV response up | 2.08 | <0.001 | 0.011 |
| IL2 STAT5 signaling | 2.06 | <0.001 | 0.015 |
| Interferon-α response | 2.03 | <0.001 | 0.014 |
| Epithelial mesenchymal transition | 2.03 | <0.001 | 0.014 |
| E2F targets | 2.03 | <0.001 | 0.013 |
| Apoptosis | 2.02 | <0.001 | 0.013 |
| TGF-β signaling | 2.02 | <0.001 | 0.012 |
| Adipogenesis | 2 | <0.001 | 0.012 |
| Coagulation | 1.96 | <0.001 | 0.015 |
| Reactive oxygen species pathway | 1.88 | <0.001 | 0.026 |
| P53 pathway | 1.87 | <0.001 | 0.03 |
| Fatty acid metabolism | 1.87 | <0.001 | 0.029 |
| Estrogen response early | 1.84 | <0.001 | 0.028 |
| Myc targets v2 | 1.83 | <0.001 | 0.027 |
| DNA repair | 1.77 | <0.001 | 0.035 |
| Oxidative phosphorylation | 1.77 | <0.001 | 0.034 |
| Angiogenesis | 1.66 | <0.001 | 0.056 |
| Apical surface | 1.62 | <0.001 | 0.057 |
| Spermatogenesis | 1.59 | <0.001 | 0.065 |
| Estrogen response late | 1.57 | <0.001 | 0.076 |
| Cholesterol homeostasis | 1.46 | <0.001 | 0.087 |
Notes.
- NES
- normalized enrichment score
- NOM P value
- nominal P value
- FDR
- false discovery rate
Figure 4. Enrichment plots from gene set enrichment analysis.
Gene sets enriched in POLR3G high phenotype: (A) Mitotic spindle. (B) Hypoxia. (C) Kras signaling up. (D) PI3K-AKT-mTOR signaling. (E) IL6-JAK-STATS3 signaling. (F) mTORC1 signaling. (G) TNF-α signaling via NF-κ B. (H) inflammation response. (I) Myc targets v1.
POLR3G expression was associated with levels of immune cell infiltration and immune checkpoint molecule expression
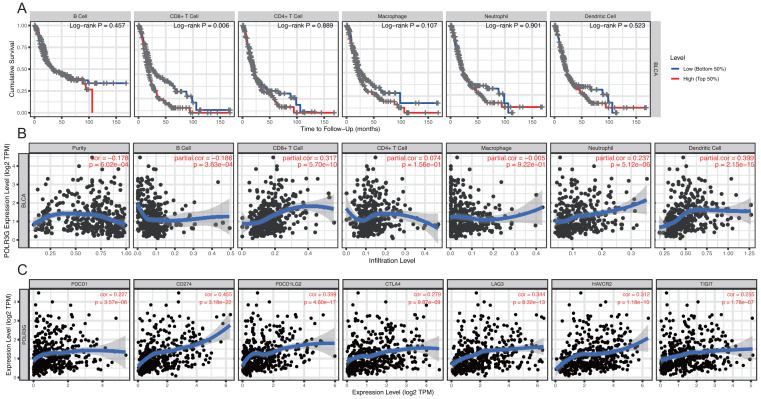
Analysis of TIMER survival module indicated that the infiltration of CD8+ T cells is related to the cumulative survival rate in TCC (P = 0.006, Fig. 5A). Gene module analysis revealed that POLR3G expression was negatively correlated with tumor purity (cor = −0.178, P = 6.02e −04) and positively correlated with infiltrating levels of CD8+ T cell (cor = 0.317, P = 5.70e −10), neutrophil cells (cor = 0.237, P = 5.12e −06), and dendritic cells (cor = 0.399, P = 2.15e−15) in TCC (Fig. 5B). Moreover, Correlation module analysis revealed that the expression of POLR3G was significantly correlated with the expression of immune checkpoint molecules including PDCD1 (cor = 0.227, P = 3.57e −06), CD274 (cor = 0.455, P = 3.18e −22), PDCD1LG2 (cor = 0.399, P = 4.60e−17), CTLA-4(cor = 0.279, P = 9.87e−09), LAG3 (cor = 0.344, P = 8.32e−13), HAVCR2 (cor = 0.312, P = 1.18e−10), and TIGIT (cor = 0.255, P = 1.78e−07) (Fig. 5C).
Figure 5. Correlation of POLR3G expression with immune cell infiltration and immune checkpoint molecule expression by TIMER.
(A) Correlation of immune cell infiltration with prognoses of patients with TCC. (B) Correlation of POLR3G expression with immune cell infiltration. (C) Correlation of POLR3G expression with immune checkpoint molecule expression.
Discussion
Several studies have investigated prognostic biomarkers for TCC, such as FGF2 (Shariat et al., 2010), UHRF1 (Unoki et al., 2009), and GRIA1 (Tilley, Kim & Fry, 2017). However, there are still no ideal predictive molecule for clinical application. This study demonstrates that POLR3G is a potentially useful biomarker for predicting prognosis of TCC.
POLR3G is an RNA polymerase III peripheral subunit that synthesizes small RNAs, such as 5S rRNA, tRNAs, and some microRNAs (Haurie et al., 2010). POLR3G plays a role in sensing and limiting infection by intracellular bacteria and DNA viruses, acts as a nuclear and cytosolic DNA sensor involved in innate immune responses, and is also essential for the maintenance of stem cell state (Ablasser et al., 2009; Chiu, Macmillan & Chen, 2009; Lund et al., 2017; Wong et al., 2011). Several studies have described the links between POLR3G and cancer. For example, Durrieu-Gaillard et al. reported that POLR3G expression was strongly up-regulated during the process of tumoral transformation in the human lung fibroblast cell line IMR90 model system (Durrieu-Gaillard et al., 2018). Haurie et al. showed that overexpression of POLR3G in IMR90 increased the expression of genes associated with tumor growth and metastasis, including S100A4, RFC2, EZR, and RAC1, and reduced the expression of tumor-suppressing genes, such as PFDN5 and KLF6 (Haurie et al., 2010). Another study (Petrie et al., 2019) found that the expression of POLR3G was up to three-fold higher in prostate tumors compared to normal adjacent samples. Similar results were observed at the cellular level; POLR3G expression was elevated in the prostate cancer cell line PC-3 compared to the immortalized healthy prostate epithelium cell line PNT2C2. In addition, knockdown of POLR3G triggered the proliferative arrest of PC-3.
Results of this study revealed that POLR3G was highly expressed in multiple cancer types, including TCC, and qRT-PCR further confirmed that POLR3G was elevated in T24 cells compared to SV-HUC-1 cells. These findings are indicative of a cumulative alteration of POLR3G expression during TCC tumorigenesis. The traditional perspective of TCC tumorigenesis postulates that TCCs arise via two different but overlapping pathways: papillary pathway and non-papillary pathway (Dinney et al., 2004). We found that non-papillary TCCs exhibited higher POLR3G expression compared to papillary TCCs. Therefore, POLR3G might play different roles in these two pathways. We also found that high POLR3G expression was positively correlated with high T classification, advanced clinical stage, and tumor recurrence, which are strongly correlated with poor prognosis in patients with TCC. More importantly, further univariate and multivariate analysis identified POLR3G expression as an independent prognostic factor for overall survival.
We conducted GSEA analysis to investigate the relationship between POLR3G and gene signatures in TCCs. Our results showed that 41 gene sets were significantly enriched in the POLR3G high expression group, including mitotic spindle, Inflammatory response, TGF-β signaling, epithelial mesenchymal transition, PI3K-AKT-mTOR signaling, and IL-6-JAK-STATS3 signaling. Several of these pathways are associated with oncogenesis, progression, and metastasis of cancer, suggesting that POLR3G expression contributes to the development, progression, and prognosis of TCC. However, the regulatory mechanism needs to be further elucidated.
Immunotherapy is a key treatment approach for TCC. Intravesical BCG immunotherapy has been used to treat superficial TCC for over 40 years and still represents the first-line adjuvant treatment for superficial TCC after TURBT to prevent tumor recurrence (Babjuk et al., 2019; Morales, Eidinger & Bruce, 1976). Over the past decade, immune checkpoint inhibitor (ICI) immunotherapy breakthroughs have enriched the available treatment modalities for advanced TCCs. Atezolizumab and Pembrolizumab have been approved for first-line systemic therapy for cisplatin-ineligible patients with local advanced or metastatic TCC whose tumors express PD-L1 (Balar et al., 2017a; Balar et al., 2017b). However, the objective response rate (ORR) to ICIs in bladder cancer patients was only ∼20% (Balar et al., 2017a; Balar et al., 2017b). Thus, identifying reliable biomarkers to distinguish which patients are more likely to respond to ICI immunotherapy is crucial for the successful treatment. Previous studies have demonstrated that the level of the immune infiltration within tumors correlates with bladder cancer prognosis and is a positive prognostic indicator of response to immunotherapy (Fridman et al., 2012; Pfannstiel et al., 2019). Furthermore, the expression of immune checkpoint PD-L1 on tumors correlates with unfavorable prognosis, but can also predict the immunotherapy reactivity of patients (Thompson, Dong & Kwon, 2007; Topalian, Drake & Pardoll, 2015). Therefore, we explored the potential role of POLR3G in immune cell infiltration within TCCs using TIMER.
First, we used the survival module to explore the association between immune infiltrate abundance and clinical outcome. Previous studies have reported that CD8+ T cells infiltration might play a positive role in the prognosis of colorectal cancer (Naito et al., 1998), triple-negative breast cancer (Vihervuori et al., 2019), and pancreatic cancer (Masugi et al., 2019). However, our results suggest that CD8+ T cell infiltration was negatively correlated with cumulative survival in TCC. Second, we used the gene module to explore the correlation between POLR3G expression and immune infiltrate abundance. Results from this analysis showed that POLR3G expression was significantly correlated with the level of infiltrating immune cells in TCC. More specifically, POLR3G expression was negatively correlated with tumor purity, and positively correlated with the infiltrating levels of CD8+ T cells, neutrophil cells, and dendritic cells in TCC. We further explored the correlations between POLR3G and immune checkpoint molecules in TCC via the correlation module. Results revealed that POLR3G expression was significantly correlated with several immune checkpoint molecules, including PDCD1, CD274, PDCD1LG2, CTLA4, LAG3, HAVCR2, and TIGIT. Taken together, these findings suggest that POLR3G contributes to the regulation of immune cell infiltration and immune checkpoint molecule expression, resulting in the suppression of anti-tumor immunity. These results provide a possible mechanistic explanation for the worse prognosis observed in patients with higher POLR3G expression.
To the best of our knowledge, this is the first study investigating the role of POLR3G in TCC
We found that POLR3G expression was an independent prognostic factor for overall survival and can potentially be used as a prognostic biomarker in TCC. However, there were some limitations to this study. First, this study was conducted using data from the public database TCGA, and the clinical information was incomplete for some patients. Further investigation with a larger sample size is needed to validate our findings. Second, the relationships between POLR3G and immune cell infiltration were analyzed using online tools, which need to be further elucidated via molecular experiments.
Conclusions
In summary, POLR3G expression was up-regulated in TCC and can potentially be used as a prognostic marker. In addition, the expression of POLR3G was associated with levels of immune cell infiltration and the expression of immune checkpoint molecules in TCC, suggesting potential value for predicting patient response to ICI immunotherapy.
Supplemental Information
Acknowledgments
The results shown here are mostly based upon data generated by the TCGA Research Network: http://cancergenome.nih.gov/.
Funding Statement
This work was supported by the Research and Development Foundation of Peking University People’s Hospital (No. RDX2018-04) and Beijing Medical Award Foundation (No. 2119000380). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Contributor Information
Kexin Xu, Email: cavinx@yeah.net.
Hao Hu, Email: huhao@bjmu.edu.cn.
Additional Information and Declarations
Competing Interests
The authors declare there are no competing interests.
Author Contributions
Xianhui Liu conceived and designed the experiments, performed the experiments, analyzed the data, prepared figures and/or tables, authored or reviewed drafts of the paper, and approved the final draft.
Weiyu Zhang performed the experiments, analyzed the data, prepared figures and/or tables, authored or reviewed drafts of the paper, and approved the final draft.
Huanrui Wang and Chin-Hui Lai analyzed the data, authored or reviewed drafts of the paper, and approved the final draft.
Kexin Xu and Hao Hu conceived and designed the experiments, authored or reviewed drafts of the paper, and approved the final draft.
Data Availability
The following information was supplied regarding data availability:
Data analyzed in this study are available at TCGA:
References
- Ablasser et al. (2009).Ablasser A, Bauernfeind F, Hartmann G, Latz E, Fitzgerald KA, Hornung V. RIG-I-dependent sensing of poly(dA:dT) through the induction of an RNA polymerase III-transcribed RNA intermediate. Nature Immunology. 2009;10:1065–1072. doi: 10.1038/ni.1779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Babjuk et al. (2019).Babjuk M, Burger M, Compérat EM, Gontero P, Mostafid AH, Palou J, vanRhijn BWG, Rouprêt M, Shariat SF, Sylvester R, Zigeuner R, Capoun O, Cohen D, Escrig JLD, Hernández V, Peyronnet B, Seisen T, Soukup V. European association of urology guidelines on non-muscle-invasive bladder cancer (TaT1 and Carcinoma In Situ) - 2019 Update. European Urology. 2019;76:639–657. doi: 10.1016/j.eururo.2019.08.016. [DOI] [PubMed] [Google Scholar]
- Balar et al. (2017a).Balar AV, Castellano D, O’Donnell PH, Grivas P, Vuky J, Powles T, Plimack ER, Hahn NM, deWit R, Pang L, Savage MJ, Perini RF, Keefe SM, Bajorin D, Bellmunt J. First-line pembrolizumab in cisplatin-ineligible patients with locally advanced and unresectable or metastatic urothelial cancer (KEYNOTE-052): a multicentre, single-arm, phase 2 study. The Lancet Oncology. 2017a;18:1483–1492. doi: 10.1016/S1470-2045(17)30616-2. [DOI] [PubMed] [Google Scholar]
- Balar et al. (2017b).Balar AV, Galsky MD, Rosenberg JE, Powles T, Petrylak DP, Bellmunt J, Loriot Y, Necchi A, Hoffman-Censits J, Perez-Gracia JL, Dawson NA, vanderHeijden MS, Dreicer R, Srinivas S, Retz MM, Joseph RW, Drakaki A, Vaishampayan UN, Sridhar SS, Quinn DI, Durán I, Shaffer DR, Eigl BJ, Grivas PD, Yu EY, Li S, Kadel EE, Boyd Z, Bourgon R, Hegde PS, Mariathasan S, Thåström A, Abidoye OO, Fine GD, Bajorin DF. Atezolizumab as first-line treatment in cisplatin-ineligible patients with locally advanced and metastatic urothelial carcinoma: a single-arm, multicentre, phase 2 trial. Lancet. 2017b;389:67–76. doi: 10.1016/S0140-6736(16)32455-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chiu, Macmillan & Chen (2009).Chiu Y-H, Macmillan JB, Chen ZJ. RNA polymerase III detects cytosolic DNA and induces type I interferons through the RIG-I pathway. Cell. 2009;138:576–591. doi: 10.1016/j.cell.2009.06.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dinney et al. (2004).Dinney CPN, McConkey DJ, Millikan RE, Wu X, Bar-Eli M, Adam L, Kamat AM, Siefker-Radtke AO, Tuziak T, Sabichi AL, Grossman HB, Benedict WF, Czerniak B. Focus on bladder cancer. Cancer Cell. 2004;6:111–116. doi: 10.1016/j.ccr.2004.08.002. [DOI] [PubMed] [Google Scholar]
- Durrieu-Gaillard et al. (2018).Durrieu-Gaillard S, Dumay-Odelot H, Boldina G, Tourasse NJ, Allard D, André F, Macari F, Choquet A, Lagarde P, Drutel G, Leste-Lasserre T, Petitet M, Lesluyes T, Lartigue-Faustin L, Dupuy J-W, Chibon F, Roeder RG, Joubert D, Vagner S, Teichmann M. Regulation of RNA polymerase III transcription during transformation of human IMR90 fibroblasts with defined genetic elements. Cell Cycle. 2018;17:605–615. doi: 10.1080/15384101.2017.1405881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dutta et al. (2016).Dutta R, Abdelhalim A, Martin JW, Vernez SL, Faltas B, Lotan Y, Youssef RF. Effect of tumor location on survival in urinary bladder adenocarcinoma: a population-based analysis. Urologic Oncology. 2016;34:531.e531–531.e536. doi: 10.1016/j.urolonc.2016.06.009. [DOI] [PubMed] [Google Scholar]
- Ferlay et al. (2013).Ferlay J, Steliarova-Foucher E, Lortet-Tieulent J, Rosso S, Coebergh JWW, Comber H, Forman D, Bray F. Cancer incidence and mortality patterns in Europe: estimates for 40 countries in 2012. European Journal of Cancer. 2013;49:1374–1403. doi: 10.1016/j.ejca.2012.12.027. [DOI] [PubMed] [Google Scholar]
- Fridman et al. (2012).Fridman WH, Pagès F, Sautès-Fridman C, Galon J. The immune contexture in human tumours: impact on clinical outcome. Nature Reviews Cancer. 2012;12:298–306. doi: 10.1038/nrc3245. [DOI] [PubMed] [Google Scholar]
- Haurie et al. (2010).Haurie V, Durrieu-Gaillard S, Dumay-Odelot H, Da Silva D, Rey C, Prochazkova M, Roeder RG, Besser D, Teichmann M. Two isoforms of human RNA polymerase III with specific functions in cell growth and transformation. Proceedings of the National Academy of Sciences of the United States of America. 2010;107:4176–4181. doi: 10.1073/pnas.0914980107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kashif Khan, Ahmed & Raza (2014).Kashif Khan M, Ahmed I, Raza SJ. Factors effecting recurrence and progression of high grade non invasive bladder cancer treated by intravesical BCG. Pakistan Journal of Medical Sciences. 2014;30:326–330. doi: 10.12669/pjms.302.4117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khattar et al. (2016).Khattar E, Kumar P, Liu CY, Akıncılar SC, Raju A, Lakshmanan M, Maury JJP, Qiang Y, Li S, Tan EY, Hui KM, Shi M, Loh YH, Tergaonkar V. Telomerase reverse transcriptase promotes cancer cell proliferation by augmenting tRNA expression. The Journal of Clinical Investigation. 2016;126:4045–4060. doi: 10.1172/JCI86042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li et al. (2017).Li T, Fan J, Wang B, Traugh N, Chen Q, Liu JS, Li B, Liu XS. TIMER: a web server for comprehensive analysis of tumor-infiltrating immune cells. Cancer Research. 2017;77:e108–e110. doi: 10.1158/0008-5472.CAN-17-0307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li et al. (2016).Li B, Severson E, Pignon J-C, Zhao H, Li T, Novak J, Jiang P, Shen H, Aster JC, Rodig S, Signoretti S, Liu JS, Liu XS. Comprehensive analyses of tumor immunity: implications for cancer immunotherapy. Genome Biology. 2016;17:174. doi: 10.1186/s13059-016-1028-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liberzon et al. (2015).Liberzon A, Birger C, Thorvaldsdóttir H, Ghandi M, Mesirov JP, Tamayo P. The Molecular Signatures Database (MSigDB) hallmark gene set collection. Cell Systems. 2015;1:417–425. doi: 10.1016/j.cels.2015.12.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lund et al. (2017).Lund RJ, Rahkonen N, Malonzo M, Kauko L, Emani MR, Kivinen V, Närvä E, Kemppainen E, Laiho A, Skottman H, Hovatta O, Rasool O, Nykter M, Lähdesmäki H, Lahesmaa R. RNA polymerase III subunit POLR3G regulates specific subsets of PolyA and SmallRNA transcriptomes and splicing in human pluripotent stem cells. Stem Cell Reports. 2017;8:1442–1454. doi: 10.1016/j.stemcr.2017.04.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Masugi et al. (2019).Masugi Y, Abe T, Ueno A, Fujii-Nishimura Y, Ojima H, Endo Y, Fujita Y, Kitago M, Shinoda M, Kitagawa Y, Sakamoto M. Characterization of spatial distribution of tumor-infiltrating CD8 T cells refines their prognostic utility for pancreatic cancer survival. Modern Pathology. 2019;32:1495–1507. doi: 10.1038/s41379-019-0291-z. [DOI] [PubMed] [Google Scholar]
- Morales, Eidinger & Bruce (1976).Morales A, Eidinger D, Bruce AW. Intracavitary Bacillus Calmette-Guerin in the treatment of superficial bladder tumors. The Journal of Urology. 1976;116:180–183. doi: 10.1016/s0022-5347(17)58737-6. [DOI] [PubMed] [Google Scholar]
- Naito et al. (1998).Naito Y, Saito K, Shiiba K, Ohuchi A, Saigenji K, Nagura H, Ohtani H. CD8+ T cells infiltrated within cancer cell nests as a prognostic factor in human colorectal cancer. Cancer Research. 1998;58:3491–3494. [PubMed] [Google Scholar]
- Petrie et al. (2019).Petrie JL, Swan C, Ingram RM, Frame FM, Collins AT, Dumay-Odelot H, Teichmann M, Maitland NJ, White RJ. Effects on prostate cancer cells of targeting RNA polymerase III. Nucleic Acids Research. 2019;47:3937–3956. doi: 10.1093/nar/gkz128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pfannstiel et al. (2019).Pfannstiel C, Strissel PL, Chiappinelli KB, Sikic D, Wach S, Wirtz RM, Wullweber A, Taubert H, Breyer J, Otto W, Worst T, Burger M, Wullich B, Bolenz C, Fuhrich N, Geppert CI, Weyerer V, Stoehr R, Bertz S, Keck B, Erlmeier F, Erben P, Hartmann A, Strick R, Eckstein M. The tumor immune microenvironment drives a prognostic relevance that correlates with bladder cancer subtypes. Cancer Immunology Research. 2019;7:923–938. doi: 10.1158/2326-6066.CIR-18-0758. [DOI] [PubMed] [Google Scholar]
- Robinson, McCarthy & Smyth (2010).Robinson MD, McCarthy DJ, Smyth GK. edgeR: a Bioconductor package for differential expression analysis of digital gene expression data. Bioinformatics. 2010;26:139–140. doi: 10.1093/bioinformatics/btp616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shariat et al. (2010).Shariat SF, Youssef RF, Gupta A, Chade DC, Karakiewicz PI, Isbarn H, Jeldres C, Sagalowsky AI, Ashfaq R, Lotan Y. Association of angiogenesis related markers with bladder cancer outcomes and other molecular markers. The Journal of Urology. 2010;183:1744–1750. doi: 10.1016/j.juro.2010.01.018. [DOI] [PubMed] [Google Scholar]
- Siegel, Miller & Jemal (2020).Siegel RL, Miller KD, Jemal A. Cancer statistics, 2020. CA: a Cancer Journal for Clinicians. 2020;70:7–30. doi: 10.3322/caac.21590. [DOI] [PubMed] [Google Scholar]
- Stein et al. (2001).Stein JP, Lieskovsky G, Cote R, Groshen S, Feng AC, Boyd S, Skinner E, Bochner B, Thangathurai D, Mikhail M, Raghavan D, Skinner DG. Radical cystectomy in the treatment of invasive bladder cancer: long-term results in 1, 054 patients. Journal of Clinical Oncology. 2001;19:666–675. doi: 10.1200/JCO.2001.19.3.666. [DOI] [PubMed] [Google Scholar]
- Subramanian et al. (2005).Subramanian A, Tamayo P, Mootha VK, Mukherjee S, Ebert BL, Gillette MA, Paulovich A, Pomeroy SL, Golub TR, Lander ES, Mesirov JP. Gene set enrichment analysis: a knowledge-based approach for interpreting genome-wide expression profiles. Proceedings of the National Academy of Sciences of the United States of America. 2005;102:15545–15550. doi: 10.1073/pnas.0506580102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thompson, Dong & Kwon (2007).Thompson RH, Dong H, Kwon ED. Implications of B7-H1 expression in clear cell carcinoma of the kidney for prognostication and therapy. Clinical Cancer Research. 2007;13:709s–715s. doi: 10.1158/1078-0432.CCR-06-1868. [DOI] [PubMed] [Google Scholar]
- Tilley, Kim & Fry (2017).Tilley SK, Kim WY, Fry RC. Analysis of bladder cancer tumor CpG methylation and gene expression within The Cancer Genome Atlas identifies as a prognostic biomarker for basal-like bladder cancer. American Journal of Cancer Research. 2017;7:1850–1862. [PMC free article] [PubMed] [Google Scholar]
- Topalian, Drake & Pardoll (2015).Topalian SL, Drake CG, Pardoll DM. Immune checkpoint blockade: a common denominator approach to cancer therapy. Cancer Cell. 2015;27:450–461. doi: 10.1016/j.ccell.2015.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Unoki et al. (2009).Unoki M, Kelly JD, Neal DE, Ponder BAJ, Nakamura Y, Hamamoto R. UHRF1 is a novel molecular marker for diagnosis and the prognosis of bladder cancer. British Journal of Cancer. 2009;101:98–105. doi: 10.1038/sj.bjc.6605123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vihervuori et al. (2019).Vihervuori H, Autere TA, Repo H, Kurki S, Kallio L, Lintunen MM, Talvinen K, Kronqvist P. Tumor-infiltrating lymphocytes and CD8 T cells predict survival of triple-negative breast cancer. Journal of Cancer Research and Clinical Oncology. 2019;145:3105–3114. doi: 10.1007/s00432-019-03036-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Witjes et al. (2020).Witjes JA, Bruins HM, Cathomas R, Compérat EM, Cowan NC, Gakis G, Hernández V, LinaresEspinós E, Lorch A, Neuzillet Y, Rouanne M, Thalmann GN, Veskimäe E, Ribal MJ, vanderHeijden AG. European association of urology guidelines on muscle-invasive and metastatic bladder cancer: summary of the 2020 guidelines. European Urology. 2020 doi: 10.1016/j.eururo.2020.03.055. Epub ahead of print Apr 29 2020. [DOI] [PubMed] [Google Scholar]
- Wong et al. (2011).Wong RC-B, Pollan S, Fong H, Ibrahim A, Smith EL, Ho M, Laslett AL, Donovan PJ. A novel role for an RNA polymerase III subunit POLR3G in regulating pluripotency in human embryonic stem cells. Stem Cells. 2011;29:1517–1527. doi: 10.1002/stem.714. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The following information was supplied regarding data availability:
Data analyzed in this study are available at TCGA: