Abstract
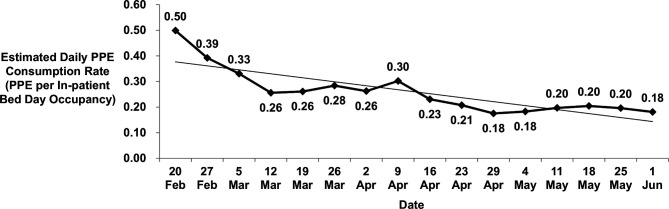
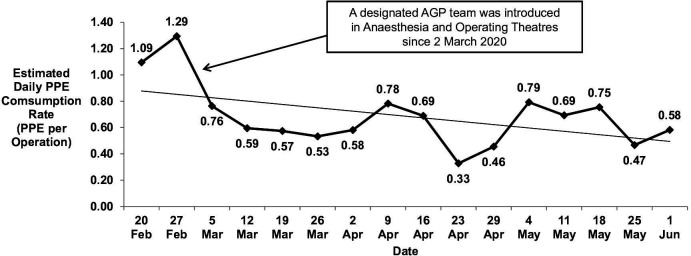
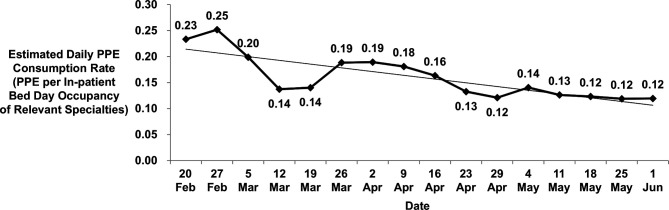
Since the outbreak of COVID-19 in December 2019, there had been global shortage of personal protective equipment (PPE) supply due to the breakage of supply chain and also the forbidding of PPE exported by various countries. This situation had greatly affected the healthcare services in local hospitals of Hong Kong. To maintain the availability of PPE for healthcare workers in high-risk clinical settings, the cluster management of New Territories West Cluster, Hospital Authority, had implemented a bundle of interventions in controlling and managing the PPE consumption and ensuring its proper use. A Taskforce on Management of PPE was set up in February 2020 with the aim to monitor and manage the use of PPE in five local hospitals and eight general outpatient clinics of New Territories West Cluster, which were governed in a cluster basis, under the COVID-19 epidemic. Interventions including cutting down non-essential services, implementing telecare, monitoring PPE consumption at unit level and PPE stock at the Cluster Central Distribution Centre and forming mobile infection teams were implemented. The updated PPE standards and usage guidelines to clinical staff were promulgated through forums, newsletters and unit visits. The PPE consumption rates of individual unit were reviewed. Significant decrease in PPE consumption rates was noted when comparing with the baseline data. Comparing the data between 20 February and 1 June 2020, the overall PPE consumption rates were reduced by 64% (r=−0.841; p<0.001) while the PPE consumption rates in anaesthesia and operating theatres, and isolation and surveillance wards were reduced by 47% (r=−0.506; p=0.023) and 49% (r=−0.810; p<0.001), respectively. A bundled approach, including both administrative measures and staff education, is effective in managing PPE consumption during major infection outbreaks especially when PPE supply is at risk.
Keywords: healthcare quality improvement, infection control, risk management
Problem
Personal protective equipment (PPE) is an important infection control measure to minimise the risk of infection and ensure staff’s safety in the healthcare system. Since the outbreak of COVID-19 in December 2019, there had been global shortage of PPE supply due to the breakage of supply chain and also the forbidding of PPE export by various countries.1 Healthcare management worldwide faced a crisis situation that was not thought of before.
The Hong Kong Hospital Authority (HA) is a statutory body responsible for managing all public hospital services in the city. The New Territories West Cluster (NTWC) is one of the seven clusters of HA serving approximately 1 million people in the north-western parts of Hong Kong. NTWC consists of 3 acute hospitals with approximately 2800 inpatient beds, 2 psychiatric hospitals and 8 general outpatient clinics.2
Although planning for global pandemic was available and regularly reviewed by the Government of Hong Kong Special Administrative Region and HA3 following the past experience of severe acute respiratory syndrome in 2003 and swine flu H1N1 in 2009, the COVID-19 pandemic is a new challenge to Hong Kong. On 11 February 2020, HA announced that the PPE stock for healthcare workers (HCWs) could only last for not more than 1 month.4 There was no foresight in NTWC to prepare for the global shortage of PPE occurring during the pandemic which served as a double impact to the hospital services. How to maintain the availability of PPE for HCWs in high-risk clinical settings and address the concerns of staff in this pandemic became priority areas for the cluster management to handle. Given the possible stockpiling behaviour of PPE in clinical areas and NTWC did not have detailed day-to-day monitoring data on PPE consumption before, it was difficult for the cluster management to formulate effective plans to manage the appropriate use of PPE. Therefore, an NTWC Taskforce on Management of PPE (the Taskforce) was set up to manage the PPE consumption and to formulate strategic plans. This report outlined the interventions made by the Taskforce which aimed to reduce the overall PPE consumption rate by 50% of its peak during the early phase of the pandemic.
Background
Since December 2019, there had been an unexpected emergence of pneumonia cases in Wuhan City, Hubei province, China.5 This disease was later found to be caused by a novel type of coronavirus, which was later known as COVID-19.6 The WHO declared this COVID-19 epidemic a Public Health Emergency of International Concern on 30 January 2020 and a pandemic on 11 March 2020.7 8
With the first case of COVID-19 being confirmed in Hong Kong on 23 January 2020,9 the epidemic had led to a city-wide panic, triggering fear-related behavioural changes and altering consumption behaviour in both the public and healthcare sectors as described in previous major infection outbreaks.10 11 The WHO warned of ‘severe disruption’ in the PPE market and the worldwide stocks were ‘now insufficient’ to meet the demand.12 13 The situation had been further exacerbated by widespread and inappropriate use of PPE by HCWs and the break in the supply chain of PPE worldwide.14
To face the global shortage of PPE supply, the WHO announced its interim guidance on the use of PPE in this COVID-19 outbreak in healthcare settings on 27 February 2020. There were three key principles: (1) minimise the need for PPE, (2) ensure the use of PPE is rational and appropriate, and (3) coordinate PPE supply chain management mechanisms.1 Local hospitals in Hong Kong need to deal with the first two areas while HA head office had sped up her PPE sourcing, tendering and procurement processes.
Measurement
To effectively control and monitor the PPE consumption and ensure proper usage of PPE, all units in NTWC were asked to report their stock levels of PPE items including face shields, surgical masks, N95 respirators and isolation gowns (levels 1 and 3 of Association for the Advancement of Medical Instrumentation standards), twice weekly to the Taskforce. The trends of daily PPE consumption in each individual unit and all hospitals and clinics were calculated by averaging the weekly differences between the opening and closing stock levels of individual unit, and taking into account the supply of PPE from the NTWC Central Distribution Centre (warehouse in NTWC to store and distribute medical equipment and consumables) and the return of surplus items to the NTWC Central Distribution Centre within each measuring period. Ongoing PPE consumption charts were used to present the observed data over a specific period of time which helped to track the information and predict the trends.
The estimated daily PPE consumption data on 20 February 2020 were taken as the baseline measurement and it was about 112 000 pieces per day (0.50 per inpatient bed-day occupancy) for all units in NTWC. In particular, critical areas including anaesthesia and operating theatres, and isolation and surveillance wards, the PPE consumption rates were 402 pieces per day (1.09 per operation) and 1753 pieces per day (0.23 per inpatient bed-day occupancy of related specialties), respectively. Pearson correlation was used to evaluate whether there were any significant changes on the PPE consumption rates after the interventions. Statistical significance was considered when the p value was less than 0.05. The data were analysed using SPSS V.26.
Design
The Taskforce, comprising members of senior management, was set up in NTWC with the aim to monitor and manage the usage of PPE. Since early February 2020, the following five interventions had been implemented by the Taskforce:
Cut down non-essential clinical services
In order to concentrate manpower and resources (including PPE) to face the COVID-19 challenge, many non-urgent clinical services including operations and endoscopy services were postponed or cancelled. Outpatient and day care services were cut substantially and appointments were rescheduled together with the drug refilling programme for patients with stable chronic illnesses.
Implementation of telecare
Telecare was not popular in HA before the COVID-19 outbreak. With the substantial clinical service cut, telecare was considered a workable substitute of service provision to affected patients to minimise patient visits to hospitals or clinics, especially in the rehabilitative and allied health settings, for example, physiotherapy, occupational therapy, dietetics, speech therapy and clinical psychology. This was also introduced in elderly care consultations to nursing home residents and psychiatric consultations to hospital inpatients in isolation settings. Without the need of direct patient contact, the requirement of PPE was much reduced. The service cut down also helped to reduce people’s traffic in hospital areas so as to reduce cross-infections in clinical settings.
Formation of mobile infection teams working in high-risk areas and handling high-risk procedures
High-level PPE, for example, N95 respirators, is essential for HCWs working in high-risk areas or performing high-risk procedures like aerosol-generating procedures (AGP). Changing PPE after each patient encounter was the usual practice. However, with the support from Centers for Disease Control and Prevention of the USA,15 and HA Central Committee on Infectious Disease and Emergency Responses, an extended use of PPE was allowed during PPE shortage period. Staff could take care of several high-risk patients continuously without changing their N95 respirators if they were not obviously soiled. Face shield could be used during the caring process to reduce the chance of contamination. This idea generated the formation of small mobile infection teams (iTeams) in various clinical settings, for example, physiotherapists performing chest physiotherapy and sputum suction, anaesthesia AGP team performing intubation and extubation for patients undergoing surgery, nursing care of several patients in isolation ward cubicles and portering service for high-risk patient transfers. The iTeams usually consisted of a small number of staff highly experienced for the job. The re-engineering of the workflow concentrated the experienced staff for high-risk duties with adequate protection and reduce the PPE consumption.
Monitoring of PPE consumption at unit level and stock at NTWC Central Distribution Centre
There was no automated monitoring of the consumption rates of PPE by individual unit in NTWC before. In order to closely monitor the situation, all clinical units were asked to report to the Taskforce their local PPE stock count twice per week. In areas where the PPE consumption rates were high, for example, accident and emergency departments, isolation wards, surveillance wards, intensive care units, anaesthesia and operating theatres, daily stock take was conducted. Also, the PPE stock level in the NTWC Central Distribution Centre was closely monitored to ensure there was a healthy supply and demand of PPE.
Communication with staff through forums, visits and newsletters
Communication is vital to address any prevailing misinformation and stigma and reduce the fear and anxiety of staff and public during the pandemic.3 Weekly staff forums were held in hospitals with videoconferencing to other satellite sites. The contents included updated information about the virus and the epidemic, guidelines from HA and Hong Kong government and administrative support to staff. Other communication channels like e-newsletters, smartphone messages, point of contact for staff’s enquiries and direct unit visits to answer queries were also conducted.
Strategy
All interventions were discussed and agreed by the Taskforce before implementation. The baseline PPE consumption rates of individual unit were taken as references for devising strategic plans in order to minimise PPE consumption in different areas.
The non-essential clinical services were reduced in early February 2020, so that PPE could be reserved for critical areas and essential services. Elective surgeries and diagnostic imaging services were reduced by 60% while non-urgent endoscopy services and day hospital activities were suspended. iTeams and telecare were subsequently implemented in late February 2020 since time was required to communicate with iTeams staff and prepare for the technical systems and equipment, for example, collecting mobile devices for the units conducting telecare and setting up the necessary network and software applications. The effectiveness of the interventions was then monitored through the PPE consumption rates.
The PPE consumption data also helped the Taskforce to identify areas of deviant of PPE consumption and remedial actions would be taken immediately. For example, unit managers were asked to be aware of any malpractice and site visits were conducted to the units for promulgation of updated PPE standard guidelines. The information helped the Taskforce to quantify and visualise the trend of PPE depletion (down to individual item model) and to forecast the critical level of PPE stock when further service adjustment or suspension would be required. For example, N95 respirator was always the focus of concern as its supply source was limited but its role was critical for HCWs working in isolation settings. It was noted from the data analysis that there was relatively more availability of some rare models of N95 respirators in the NTWC Central Distribution Centre for which only a small number of HCWs had passed the fit test. As such, these HCWs were encouraged to use these rare models first and spare the stock of common models to the general pool of HCWs. N95 respirator fit tests were also slowed down for staff not working in high-risk areas to preserve and prioritise the supply of N95 respirators for critical areas handling suspected or confirmed patients with COVID-19.16
The PPE guidelines and their subsequent revisions according to the updated knowledge of the disease had generated concerns and uncertainties among HCWs. An open attitude to communicate with staff and a transparent culture were important to solicit understanding and support from them.
Results
When comparing data between 20 February and 1 June 2020, significant decreasing trends were found in the overall PPE consumption per inpatient bed-day occupancy (decrease in 64%; r=−0.841; p<0.001) (figure 1), PPE consumption in anaesthesia and operating theatres per operation performed (decrease in 47%; r=−0.506; p=0.023) (figure 2) and PPE consumption in isolation and surveillance wards per inpatient bed-day occupancy of relevant specialties (decrease in 49%; r=−0.810; p<0.001) (figure 3). Since the implementation of the bundle of interventions, there was no incident of cross-infection for both HCWs and patients occurring in clinical settings, which demonstrated the safety aspect of the interventions.
Figure 1.
Estimated daily consumption rates of personal protective equipment (PPE) from 20 February to 1 June 2020 in all units in New Territories West Cluster.
Figure 2.
Estimated daily consumption rates of personal protective equipment (PPE) from 20 February to 1 June 2020 in anaesthesia and operating theatres after the implementation of iTeams responsible for performing aerosol-generating procedures (AGP).
Figure 3.
Estimated daily consumption rates of personal protective equipment (PPE) from 20 February to 1 June 2020 in isolation and surveillance wards for confirmed and suspected patients with COVID-19.
Lessons and limitations
The success of the bundled interventions depends both on the efforts of the local hospitals and the corporate direction. The guidance from HA was also an important success factor. The adjustment of clinical services under the HA Emergency Response Level and revising the guidance on the proper use of PPE for different duties in hospitals were facilitating factors for the interventions.17
Under the stress of supply and stock shortage of PPE in all public hospitals, the proper and rational use of PPE is a critical step in combating the pandemic. Using PPE of higher standard in low-risk procedures is irrational, as it does not provide extra protection but rather gives staff a false sense of security and such malpractice would deplete the stock of high-level PPE for staff working in high-risk areas. Staff may also be unfamiliar with the donning and doffing procedures when using high-standard PPE, which would paradoxically increase their risk of infection.18 19
Apart from communication and education to staff, close monitoring and managing of PPE consumption is important for hospital management to handle this crisis of PPE shortage. However, this is a complex exercise for NTWC because there are hundreds of clinical units. The setting up of the PPE Taskforce and the assignment of dedicated staff (both clinical and administrative) to focus on the issue were instrumental. The temporary drastic cut down of non-essential services at the beginning was a major step to take. This facilitated the infection control by reducing people’s entry to hospitals and significantly reduced the PPE consumption. For those critical areas like isolation or surveillance wards, operating theatres, intensive care units, and so on, their essential services could not be reduced but were actually increased. With the recommendations to support the extended use of PPE and the staff’s agreement to form small iTeams, the PPE consumption was also significantly reduced in these critical areas. This could only be possible when staff were convinced of the rationale and had a good team spirit to work with the cluster management to face the double challenges of the pandemic and PPE shortage.
The use of PPE in an ongoing epidemic is different from usual clinical practices, especially in the early stage when the knowledge of the infection is limited and the PPE requirement is uncertain.20 Extensive stockpiling behaviour has to be taken into account when estimating the rate of PPE consumption.21 After the first local case of COVID-19 being confirmed on 23 January 2020, a typical epidemic fear with an irrational PPE stockpiling behaviour would be expected in local hospitals. The coincidence of the epidemic occurrence during the 4 days of Chinese New Year holidays and the subsequent lockdown of cities in China to control the infection led to a complete breakdown of the PPE supply chain. Although HA kept a 3-month stock of PPE according to the Pandemic Preparatory Plan,22 the unexpected PPE consumption rose together with the PPE supply halt. A rapid depletion of PPE stock of HA to a critical level of only around 1 month occurred in early February 2020. As a lesson to learn, HA had aimed at keeping a 6-month PPE stock for pandemic preparation in the future.23
The designated PPE Taskforce was set up at the critical moment in NTWC to deal with the crisis. No single solution could solve the big and imminent problem of PPE shortage in a pandemic. Thus, a bundle of interventions was implemented. The key success factors are soliciting the support and understanding of staff and accurately estimating and monitoring the PPE consumption rates. It is important to understand the workflow and the usual practices of different units and their PPE consumption in relation to the nature of the job. The Taskforce emphasised to staff about the goal to strive for zero infection incident among HCWs in clinical settings and encouraged the rational use of PPE. Establishing a mutual trust between the hospital staff and the cluster management is of paramount importance. The cluster management had to convince the staff that actions were taken quickly and decisively. The ‘TRUE’ (Transparent, Rumour clarification, Updates and Education) principles for risk communication in crisis had been useful for disseminating clear, concise and up-to-date information to staff through staff forums, e-newsletters, direct unit visits, and so on.24
Together with the stabilisation of PPE stock, the results demonstrated that the bundle of interventions was successful to achieve the aim of reducing 50% of overall PPE consumption rate. This was the results of the improved understanding of the disease nature of COVID-19 and what PPE requirement standards could be adjusted and the increasingly rational behaviour of the staff in using PPE. This instilled a calm and controlled atmosphere in clinical areas which was very precious and critical when one was facing a pandemic infection of unprecedented proportions.
The experience in this programme could shed some light to future pandemic preparatory planning. PPE supply and demand would be a key area to look into. PPE is now considered as one of the strategic national stockpile items for the management of infectious disease outbreaks in many countries. Simulation exercises should be run to evaluate how PPE supply and demand could be accurately monitored during crisis.25 Expanding the supply source of PPE would be a global movement. The guarantee of a stable PPE supply chain is instrumental to allay the fears of HCWs in handling infection epidemics. While adopting the iTeams concept to clinical services was successful, research into its effectiveness and safety, and the possible expansion to other service areas should be conducted. Telecare showed its distinct role to offer healthcare during infection outbreaks. Its potential to further develop is huge and it should be further studied as an alternative to the usual patient care.26 27 Last but not least, education on infection control, including the proper use of PPE and other precautionary measures, remains to be fundamental to ensuring staff safety in infection outbreaks.
This study had several limitations. First, the regular stock-taking exercise only provided a calculated estimation of daily PPE consumption of units which might be slightly different from the exact figures. However, the estimation appeared to be a good one and the actual stock on hand could be confidently monitored. Second, the sustainability of the interventions has to be evaluated to ensure they are effective in the ever-changing environment and pandemic situation. It would be expected that these bundled measures may not be applicable during the resumption of normal hospital services. The cluster management should study the practicality and feasibility of modifying and adopting those interventions under the ‘new normal’ of healthcare after COVID-19. Third, since the management of PPE consumption requires a prompt response, thorough planning by the plan-do-study-act cycle was considered difficult under this circumstance as it usually requires careful planning and more evaluation in the process.28 Therefore, ongoing PPE consumption charts were used for outcome measuring such that the cluster management could make effective decisions according to the latest trends.
Conclusion
Facing the COVID-19 pandemic together with the global PPE supply shortage, this programme demonstrated a successful approach to monitor and control the consumption of PPE in clinical areas and the interventions were proved to be effective. It is believed that other healthcare organisations can take reference to this approach to combat the global health challenge of COVID-19.
Acknowledgments
The authors would like to thank all members of the Taskforce for their support in monitoring the PPE consumption in different units.
Footnotes
Contributors: WMK, CKM, PML, MYM, TLQ and YHT designed the programme. WMK, CKM, YTK, HWL, KHC, THSL, PML, MYM, TLQ and YHT implemented the programme. YTK, KHC and THSL collected and interpreted the data. WMK, CKM and YTK drafted the manuscript. CKM and YHT made the final approval of the version submitted. YTK submitted the manuscript.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Patient consent for publication: Not required.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement: All data relevant to the study are included in the article.
References
- 1.World Health Organization Rational use of personal protective equipment for coronavirus disease 2019 (COVID-19) - Interim Guidance. Geneva: World Health Organization, 2020. [Google Scholar]
- 2.Hospital Authority Hospital authority annual report 2018-19. Hong Kong: Hospital Authority, 2019. [Google Scholar]
- 3.Centre for Health Protection Preparedness plan for influenza pandemic. Hong Kong: The Government of the Hong Kong Special Administrative Region, 2014. [Google Scholar]
- 4.The Standard Hospital authority says protective gear can last month. [Internet], 2020. Available: https://www.thestandard.com.hk/breaking-news/section/4/141650/Hospital-Authority-says-protective-gear-can-last-month
- 5.Lu H, Stratton CW, Tang Y-W. Outbreak of pneumonia of unknown etiology in Wuhan, China: the mystery and the miracle. J Med Virol 2020;92:401–2. 10.1002/jmv.25678 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.World Health Organization Naming the coronavirus disease (COVID-19) and the virus that causes it [Internet]. Geneva: World Health Organization, 2020. https://www.who.int/emergencies/diseases/novel-coronavirus-2019/technical-guidance/naming-the-coronavirus-disease-(covid-2019)-and-the-virus-that-causes-it [Google Scholar]
- 7.World Health Organization WHO Director-General’s statement on IHR Emergency Committee on Novel Coronavirus (2019-nCoV) [Internet]. Geneva: World Health Organization, 2020. https://www.who.int/dg/speeches/detail/who-director-general-s-statement-on-ihr-emergency-committee-on-novel-coronavirus-(2019-ncov) [Google Scholar]
- 8.World Health Organization WHO Director-General’s opening remarks at the media briefing on COVID-19 - 11 March 2020 [Internet]. Geneva: World Health Organization, 2020. https://www.who.int/dg/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---11-march-2020 [Google Scholar]
- 9.Centre for Health Protection Latest Situation of Novel Coronavirus Infection in Hong Kong [Internet]. Hong Kong: Centre for Health Protection, 2020. https://chp-dashboard.geodata.gov.hk/covid-19/en.html [Google Scholar]
- 10.Person B, Sy F, Holton K, et al. . Fear and stigma: the epidemic within the SARS outbreak. Emerg Infect Dis 2004;10:358–63. 10.3201/eid1002.030750 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bali S, Stewart KA, Pate MA. Long shadow of fear in an epidemic: fearonomic effects of Ebola on the private sector in Nigeria. BMJ Glob Health 2016;1:e000111. 10.1136/bmjgh-2016-000111 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mahase E. Coronavirus: global stocks of protective gear are depleted, with demand at "100 times" normal level, WHO warns. BMJ 2020;368:m543. 10.1136/bmj.m543 [DOI] [PubMed] [Google Scholar]
- 13.The Japan Times Face masks and hand sanitizers in short supply across Asia amid deadly virus panic [Internet], 2020. Available: https://www.japantimes.co.jp/news/2020/01/24/business/face-masks-hand-sanitizers-asia-coronavirus/#.XlyT6xEUnmg
- 14.World Health Organization WHO Director-General’s opening remarks at the media briefing on 2019 novel coronavirus - 7 February 2020 [Internet]. Available: https://www.who.int/dg/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-2019-novel-coronavirus-7-february-2020
- 15.The National Institute for Occupational Safety and Health Recommended guidance for extended use and limited reuse of N95 filtering Facepiece respirators in healthcare settings. Washington: Centre for Disease Control and Prevention, 2018. [Google Scholar]
- 16.Division of Occupational Safety and Health Temporary Enforcement Guidance - Healthcare Respiratory Protection Annual Fit-Testing for N95 Filtering Facepieces During the COVID-19 Outbreak. Washington: Occupational Safety and Health Administration, 2020. [Google Scholar]
- 17.Bhadelia N. Coronavirus: hospitals must learn from past pandemics. Nature 2020;578:193. 10.1038/d41586-020-00354-4 [DOI] [PubMed] [Google Scholar]
- 18.Reddy SC, Valderrama AL, Kuhar DT. Improving the use of personal protective equipment: applying lessons learned. Clin Infect Dis 2019;69:S165–70. 10.1093/cid/ciz619 [DOI] [PubMed] [Google Scholar]
- 19.Centre for Health Protection Preparedness and response plan for novel infectious disease of public health significance. Hong Kong: Centre for Health Protection, 2020. [Google Scholar]
- 20.Seale H, Leem JS, Gallard J, et al. . The cookie monster muffler: perceptions and behaviours of hospital healthcare workers around the use of masks and respirators in the hospital setting. Int J Infect Control 2015;11. [Google Scholar]
- 21.Swaminathan A, Martin R, Gamon S, et al. . Personal protective equipment and antiviral drug use during hospitalization for suspected avian or pandemic influenza. Emerg Infect Dis 2007;13:1541–7. 10.3201/eid1310.070033 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wong ATY, Chen H, Liu S-H, et al. . From SARS to avian influenza preparedness in Hong Kong. Clin Infect Dis 2017;64:S98–104. 10.1093/cid/cix123 [DOI] [PubMed] [Google Scholar]
- 23.RTHK Crippled hospitals to tap private sector for help [Internet], 2020. Available: https://news.rthk.hk/rthk/en/component/k2/1506626-20200204.htm?archive_date=2020-02-04
- 24.Department of Health and Human Services Crisis and emergency risk communication. Washington: Centre for Disease Control and Prevention, 2014. [Google Scholar]
- 25.Phin NF, Rylands AJ, Allan J, et al. . Personal protective equipment in an influenza pandemic: a UK simulation exercise. J Hosp Infect 2009;71:15–21. 10.1016/j.jhin.2008.09.005 [DOI] [PubMed] [Google Scholar]
- 26.Hollander JE, Carr BG. Virtually perfect? Telemedicine for Covid-19. N Engl J Med 2020;382:1679–81. 10.1056/NEJMp2003539 [DOI] [PubMed] [Google Scholar]
- 27.Pham C, Badowski MW. The role of telemedicine in infectious diseases. EMJ Innov 2019. [Google Scholar]
- 28.Reed JE, Card AJ. The problem with Plan-Do-Study-Act cycles. BMJ Qual Saf 2015;25:202–6. [DOI] [PMC free article] [PubMed] [Google Scholar]