Abstract
Background:
There are many reasons to believe that surgeon personality traits and related leadership behaviors influence patient outcomes. For example, participation in continuing education, effective self-reflection, and openness to feedback are associated with certain personalities and may also lead to improvement in outcomes. In this context, we sought to determine if an individual surgeon’s thinking and behavior traits correlate with patient level outcomes after bariatric surgery.
Methods:
Practicing surgeons from the Michigan Bariatric Surgery Collaborative (MBSC) were administered the Life Styles Inventory (LSI) assessment. The results of this assessment were then collapsed into 3 major styles that corresponded with particular patterns of an individual’s thinking and behavior: Constructive (achievement, self-actualizing, humanistic-encouraging, affiliative), Passive/Defensive (approval, conventional, dependent, avoidance), and Aggressive/Defensive (perfectionistic, competitive, power, oppositional). We compared patients level outcomes for surgeons in the lowest, middle, and highest quintiles for each style. We then used patient level risk adjusted rates of complications after bariatric surgery to quantify the impact surgeon style on post-operative outcomes.
Results:
We found that patients undergoing bariatric surgery performed by surgeons with high levels of Constructive (achievement, self-actualizing, humanistic-encouraging, affiliative) and Passive/Defensive (approval, conventional, dependent, avoidance) styles had lower rates of adverse events compared with surgeons with low levels of the respective styles (High Constructive: 14.7% [13.8%-15.6%], Low Constructive: 17.7% [16.8%-18.6%]; High Passive: 14.8% [13.4%-16.1%], Low Passive: 18.7% [17.3%-19.9%]). Conversely, surgeons identified with high aggressive styles (perfectionistic, competitive, power, oppositional) had similar rates of postoperative adverse events compared with surgeons with low levels (High Aggressive: 15.2% [14.3%-16.1%], Low Aggressive: 14.9% [14.2%-15.6%]).
Conclusion:
Our analysis demonstrates that surgeons’ leadership styles are correlated with surgical outcomes for individual patients. This finding underscores the need for professional development for surgeons to cultivate strengths in the constructive domains including intentional self-improvement, development of interpersonal skills, and the receptiveness to feedback.
Keywords: Professional Development, Leadership Skills, Bariatric Surgery
Background
The definition of a “good” leader is changing. There is an increased appreciation of the importance of emotional intelligence—e.g., self-awareness, social awareness—among good leaders. The practice of medicine, however, has predominantly relied on traditional measures of intelligence as gateways to the profession, especially highly competitive specialties such as surgery [1]. Moreover, surgeons are often regarded as more likely to adopt an authoritative style of leadership making them less successful in team environments [2]. There has been a significant shift in surgery toward valuing collaboration and teamwork [3], which creates an environment where an authoritative style may be less effective than other styles that represent higher levels of emotional intelligence.
There are many reasons to believe that self-awareness and social-awareness are could impact patient outcomes. Namely, the practice of surgery demands that surgeons have flexibility in teamwork and high levels of emotional intelligence in order to guide highly functioning teams. Prior studies evaluate the relationship between surgeon technical skill and technique and patient outcomes [4], but there is very little evidence linking non-technical domains such as personality traits, leadership skills, and self-awareness with patient outcomes after surgery. Bariatric surgery is an excellent case study to evaluate the relationship between leadership style and outcomes. Bariatric procedures are highly routinized and uniquely dependent on efficient and highly functioning teams [5].
In this context, we sought to determine if an individual surgeon’s leadership style, as measured with the Life Skills Inventory (LSI), correlate with patient level outcomes after bariatric surgery.
Methods
The Michigan Bariatric Surgical Collaborative (MBSC) is a statewide quality improvement collaborative initiative supported by Blue Cross and Blue Shield of Michigan [6]. The MBSC emphasizes identification of best practices and quality improvement in the delivery of bariatric surgery care throughout the state of Michigan. At regular MBSC meetings, bariatric surgeons participate in continuing education including video review coaching, receive their patient level outcomes data, and participate in quality improvement efforts.
The MBSC also incorporates professional development of bariatric surgeons in the state of Michigan as part of the collaborative’s quality improvement efforts. In October 2014, 35 practicing surgeons were administered the Life Styles Inventory (LSI) assessment under the guidance of an executive coach as a mechanism to assess leadership style and nontechnical skills [7,8]. The LSI assessment is intended to serve as a self-development guide by providing individualized representations of strengths and self-defeating behaviors. The LSI captures 12 styles that correlated with different ways of thinking about one’s self and behavior with individual scores ranging from 0 (lowest possible level) to 99 (highest possible level).
The results of this assessment for all participating surgeons were analyzed as 12 individual domains and also as the collapsed scores from 3 major clusters of styles: Constructive, Passive/Defensive, and Aggressive/Defensive. These major clusters that corresponded with particular patterns of an individual’s thinking and behavior by collapsing groups of 4 individual domains: Constructive (achievement, self-actualizing, humanistic-encouraging, affiliative), Passive/Defensive (approval, conventional, dependent, avoidance), and Aggressive/Defensive (perfectionistic, competitive, power, oppositional).
We then assessed patient level risk adjusted rates of complications after surgery for patients undergoing bariatric surgery in the state of Michigan using the prospectively collected patient data from the Michigan Bariatric Surgery Collaborative. Given the low rate of adverse events after bariatric surgery, we opted to use “any adverse” events occurring within 30 dys of the index operation as our measurement of postoperative outcomes in order to identify potential differences in surgeon performance driven by their leadership style. “Any adverse” event after bariatric surgery includes cardiopulmonary complication, renal failure, hemorrhage, surgical site infection, wound complication, venous thromboembolism, anastomotic leak, bowel obstruction or stricture, hospital related infection, and death. The rates of adverse events after bariatric surgery were adjusted for patient factors including age, comorbidity, and procedure. We then assessed each participating bariatric surgeon’s rate of risk adjusted rate of postoperative adverse events.
To quantify the impact surgeon leadership and non-technical styles on post-operative outcomes, we stratified surgeons into the lowest, middle, and highest quintiles for each of the three major clusters. We then assessed the correlation between risk adjusted patient level outcomes and major surgeon styles as determined by their LSI scores. In order to maximize variation in comparisons, we compared patient outcomes for surgeons the lowest and highest quintiles in each cluster.
No demographic data was analyzed given the small sample size. This study was approved by the University of Michigan Institutional Review Board (HUM00086502).
Results
Thirty-five surgeons completed the Life Styles Inventory tool at the October 2014 Meeting of the Michigan Bariatric Surgery Collaborative (Table 1).
Table 1.
Participating Surgeons
| Surgeons (#) | 35 |
| Gender (% Men) | 89% |
| Cases per Surgeon (Range) | 1,256 (43-4,302) |
| Procedures Performed (#) | |
| Roux-en-Y Gastric Bypass | 17,082 |
| Laparoscopic Band Placement | 4,503 |
| Sleeve Gastrectomy | 21,987 |
| Biliary-Pancreatic Diversion with Duodenal Switch | 417 |
| Rate of Adverse events (risk adjusted) | 14.5% |
From 2006-2017, the bariatric surgeons who completed the LSI assessment had prospective patient data recorded for 43,939 bariatric procedures recorded in the MBSC database. These cases included 17,082 Roux-en-Y Gastric Bypasses, 4,503 Laparoscopic Gastric Band Placements, 21,987 Sleeve Gastrectomies, and 417 Biliary-Pancreatic Diversion with Duodenal Switch procedures. Each surgeon who was included in this analysis performed between 43 and 4,302 procedures with an average of 1,247 procedures performed and a median of 947 procedures performed during the period of study. These procedures had an overall average risk adjusted rate of any adverse event of 14.5%.
There was substantial variation in the scores by individual domains across the 35 participating surgeons in this study. The average score of all individual domains was 48.1. When evaluated by individual style across the participating surgeons, the power style had the lowest average score of 36.1 and the avoidance style had the highest average score of 57.6. The major styles had similar average scores: Aggressive/Defensive Style 41.7, Constructive Style: 50.4, and Passive/Defensive Style: 52.4 (Figure 1, Table 2).
Figure 1.
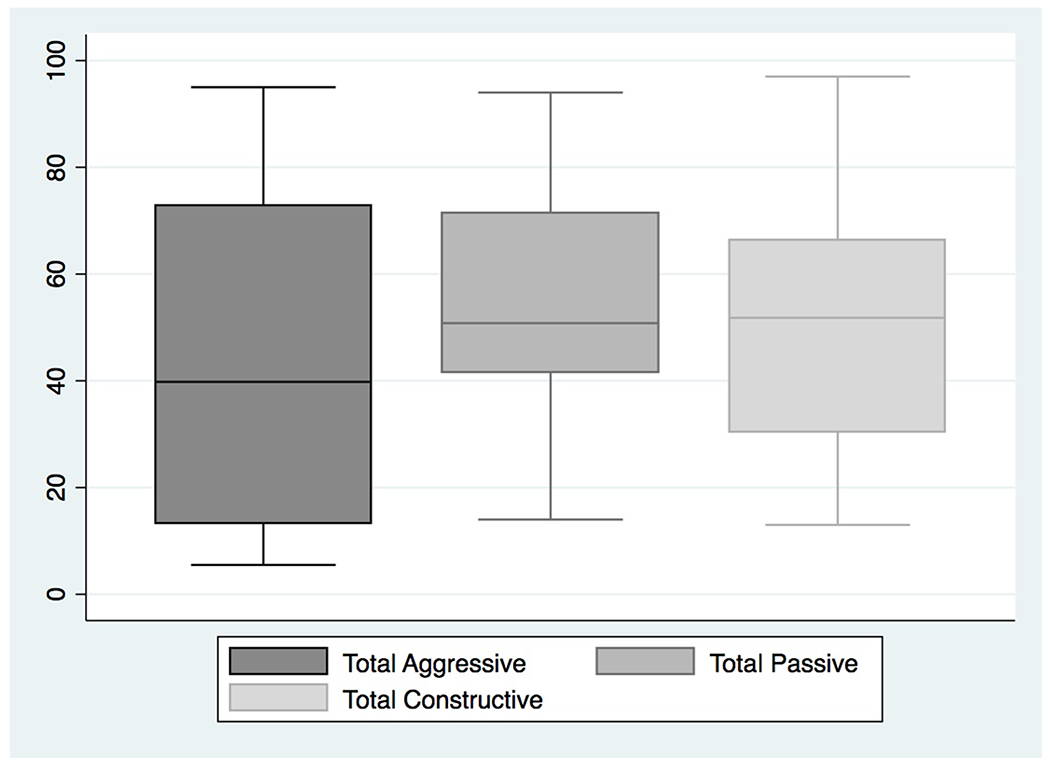
Life styles inventory scores across surgeons
Table 2.
Life Styles Inventory Scores by Surgeon
| Average (Median) | Range | |
|---|---|---|
| Individual Domain Scores | ||
| Humanistic | 47.9 (50) | [1-99] |
| Affiliative | 53.4 (55) | [12-99] |
| Approval | 52.1 (57) | [7-96] |
| Conventional | 50.3 (42) | [9-95] |
| Dependent | 49.5 (50) | [7-94] |
| Avoidance | 57.6 (55) | [25-99] |
| Oppositional | 46.7 (42) | [0-99] |
| Power | 36.1 (25) | [0-99] |
| Competitive | 41.5 (42) | [3-93] |
| Perfectionist | 42.4 (44) | [0-96] |
| Achievement | 52.9 (57) | [10-99] |
| Self-Actualize | 47.3 (42) | [8-91] |
| Cluster Scores | ||
| Aggressive | 41.7 (38.5) | [6-95] |
| Constructive | 50.4 (46.75) | [13-97] |
| Passive | 52.4 (49.5) | [14-94] |
The individual style scores varied significantly from 0 points in some style domains and as high as 99 in other domains. There was no single dominant style or consistent profile for the surgeons in this cohort, but rather wide variation in the scoring profiles was appreciated across participating surgeons.
We then analyzed the major style average scores by individual surgeon and the risk adjusted rates of any adverse events after bariatric surgery. We found that patients undergoing bariatric surgery performed by surgeons with high levels of Constructive (achievement, self-actualizing, humanistic-encouraging, affiliative) and Passive/Defensive (approval, conventional, dependent, avoidance) styles had lower rates of adverse events compared with surgeons with low levels of the respective styles (High Constructive: 14.7% [13.8%-15.6%], Low Constructive: 17.7% [16.8%-18.6%]; High Passive: 14.8% [13.4%-16.1%], Low Passive: 18.7% [17.3%-19.9%]). Conversely, surgeons identified with high aggressive styles (perfectionistic, competitive, power, oppositional) had similar rates of postoperative adverse events compared with surgeons with low levels (High Aggressive: 15.2% [14.3%-16.1%], Low Aggressive: 14.9% [14.2%-15.6%]) (Table 3).
Table 3.
Major Styles and Risk Adjusted Rates of Any Adverse Events
| Major Style | Quintile | Rate of Adverse Event | 95% CI |
|---|---|---|---|
| Aggressive | High | 15.2% | [14.3%-16.1%] |
| Low | 14.9% | [14.2%-15.6%] | |
| Constructive | High | 14.7% | [13.8%-15.6%] |
| Low | 17.7% | [16.8%-18.6%] | |
| Passive | High | 14.8% | [13.4%-16.1%] |
| Low | 18.7% | [17.3%-19.9%] |
Conclusions
Our analysis demonstrates that surgeons’ leadership styles as represented by this assessment of twelve thinking and behavior styles vary widely and can be correlated with post-operative outcomes for bariatric surgery patients. Surgeons with high scores for the constructive and passive clusters had lower rates of adverse events for their patients undergoing bariatric procedures, while the surgeons’ aggressive cluster scores were not correlated with postoperative outcomes.
Significant research has focused on the technical performance of bariatric surgery and the potential impact on patient outcomes [4]. Beyond variation in technical skill, there is significant variation in an individual surgeon’s nontechnical skills and leadership style that has not yet been linked to patient outcome [9]. Leadership skills, emotional intelligence, and situational awareness are crucial in the practice of surgery, but the full extent of impact of these nontechnical skills on patient outcomes is unknown. In this study, we demonstrate that nontechnical skills and styles among surgeon vary widely and can be correlated with patient outcomes.
This analysis also demonstrates that the composite “style” or “personality of a surgeon” varies widely. The power style, defined as “a high need for power, status, prestige, influence, and control,” had lowest average score for the thirty-five bariatric surgeons in this exercise [7]. This finding demonstrates stands in direct contrast to the often held stereotypical view of a surgeon. The diverse personalities and nontechnical skill sets of surgeons support the need for ongoing professional development, leadership curricula, and study of the relationship between surgeon leadership and personality styles and patient outcomes.
This is the first work aimed at defining the potential impact of surgeon leadership style and on patient outcomes. In each environment, a surgeon is responsible for employing nontechnical skills for successful performance. For example, a surgeon’s bedside manner and ability to engage with patients can impact patient satistfaction, while the ability to lead teams in is critical for a well functioning operating room [10, 11]. Additionally, openness to feedback and performance improvement are fundamental in the rapidly progressing field of surgery.
The results of this analysis should be interpreted in the context of several limitations. This study was limited to 35 bariatric surgeons in the Michigan Bariatric Surgery Collaborative. This small sample size limits our ability to extrapolate our findings to surgeons outside of the bariatric surgery and to evaluate demographic information of participants. Further, we were not able to capture whether the participants had previously received leadership training which could impact their performance on this tool.
This analysis of surgeon leadership styles and post-operative outcomes underscores the potential impact of nontechnical professional development of surgeons on the quality of patient care. These findings emphasize the critical need cultivate key constructive domains in practicing surgeons, emphasizing intentional self-improvement, development of interpersonal skills, and the receptiveness to feedback.
Acknowledgements of Research Support:
S.S. is supported by the National Clinician Scholars Program at the Institute for Healthcare Policy and Research at the University of Michigan.
A.K. is supported by the NIH grant T32 HS000053-24.
J.D. is supported for this work through R01 grants from the National Institute of Diabetes and Digestive and Kidney Diseases and Agency for Healthcare Research and Quality (Grant #: R01DK101423 and R01HS023597).
Footnotes
Conflicts of Interest: Dr. Dimick is a Cofounder of ArborMetrix, a company that makes software for profiling hospital quality and efficiency. For the remaining authors none were declared.
Presentation of work: This work will be presented at SAGES on April 13, 2018 as Oral Presentation S106 - Surgeon Leadership Style and Risk-Adjusted Patient Outcomes (SS26: Diversity and Innovation Session).
Disclosures
Sarah Shubeck, MD, MS: Nothing to disclose.
Arielle Kanters, MD, MS: Nothing to disclose.
Justin Dimick, MD, MPH: Dr. Dimick is a Cofounder of ArborMetrix, a company that makes software for profiling hospital quality and efficiency.
References
- 1.Emanuel E, Gudbranson E (2018) Does Medicine Overemphasize IQ? Jama 319:651–652. [DOI] [PubMed] [Google Scholar]
- 2.Drosdeck J, Osayi S, Peterson L, Yu L, Ellison E, Muscarella P (2015) Surgeon and nonsurgeon personalities at different career points. J Surg Res 196(1):60–66. [DOI] [PubMed] [Google Scholar]
- 3.Leach L, Myrtle R, Weaver F (2011) Surgical teams: role perspectives and role dynamics in the operating room. Health Serv Manage Res 24(2): 81–90. [DOI] [PubMed] [Google Scholar]
- 4.Birkmeyer J, Finks J, O’Reilly A, Oerline M, Carlin A, Nunn A, Dimick J, Banerjee M, Birkmeyer N (2013) Surgical skill and complication rates after bariatric surgery. N Engl J Med 369(15):1434–1442. [DOI] [PubMed] [Google Scholar]
- 5.Telem D, Jones D, Schauer P, Brethauer S, Rosenthal R, Provost D, Jones S (2018) Updated panel report: best practices for the surgical treatment of obesity. Surg Endosc, DOI: 10.1007/s00464-018-6160-x, March 30, 2018. [DOI] [PubMed] [Google Scholar]
- 6.Michigan Bariatric Surgery Collaborative (2018) Available at: http://michiganbsc.org/. Accessed April 2, 2018.
- 7.Life Styles Inventory (2018) Available at: https://www.humansynergistics.com/change-solutions/change-solutions-for-individuals/assessments-for-individuals/life-styles-inventory. Accessed April 2, 2018.
- 8.Ware M, Leak G, and Perry N (1985) Life Styles Inventory: Evidence for its Factorial Validity . Psychological Reports, 56(3): 963–968. [Google Scholar]
- 9.Hu Y, Parker S, Lipsitz S, Arriaga A, Peyre S, Corso K, Roth E, Yule S, Greenberg C (2016) Surgeons’ Leadership Styles and Team Behavior in the Operating Room. J Am Coll Surg 222(1):41–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Makary M, Sexton J, Freischlag J, Holzmueller C, Milliman E, Rowen L, Pronovost P. (2006) Operating room teamwork among physicians and nurses: teamwork in the eye of the beholder. J Am Coll Surg, 202 (5): 746–52. [DOI] [PubMed] [Google Scholar]
- 11.Frasier L, Quamme S, Becker A, Booth S, Gutt A, Wiegmann D, Greenberg C (2017) Investigating Teamwork in the Operating Room: Engaging Stakeholders and Setting the Agenda. JAMA Surgery 152(1): 109–111. [DOI] [PubMed] [Google Scholar]


