Abstract
BACKGROUND AND PURPOSE:
When the femoral approach for mechanical thrombectomy (MT) in acute ischemic stroke (AIS) is limited, trans-brachial or-radial access is an alternative. However, transbrachial insertion of a 9Fr (outer diameter [OD]) balloon guide catheter (BGC) into the carotid artery is not feasible. Computed tomographic (CT) angiography (CTA) may provide vascular anatomical information for successful insertion. We investigated CTA anatomical features for successful transbrachial insertion of a 9Fr BGC into the carotid artery.
MATERIALS AND METHODS:
We analyzed AIS patients who underwent CTA and transbrachial MT using a 9Fr BGC between 2014 and 2016. We evaluated the successful insertion rate and CT angiographic anatomical features.
RESULTS:
Twenty-four patients met our inclusion criteria. We achieved successful insertion in 18 (75%) of 24 cases: 7 (58.3%) of 12 for left carotid arteries and 11 (91.7%) of 12 for right carotid arteries. Successful insertion was achieved in 4 of 4 bovine aortic arch for left carotid occlusion and in 3 of 8 nonbovine aortic arches for left carotid occlusion. We achieved successful insertion in 3 nonbovine cases with takeoff angles ≥23° and failed insertion in 5 cases with takeoff angles <23°. We achieved successful insertion in 10 of the 10 cases with takeoff angles ≥25° in the right common carotid artery. The BGC was broken in 1 of 2 cases with takeoff angles <25°.
CONCLUSIONS:
The CTA provided a high likelihood of successful 9Fr OD BGC insertion without an introducer sheath. Successful transbrachial insertion was achieved in bovine left carotid cases, in nonbovine left carotid cases with takeoff angles ≥23°, and in right carotid cases with takeoff angles ≥25°.
Keywords: Acute ischemic stroke, balloon guide catheter, computed tomographic angiography, trans-brachial approach
Introduction
Mechanical thrombectomy (MT) has become an essential treatment for acute ischemic stroke (AIS) due to large vessel occlusion.[1,2] The transfemoral approach is standard for introducing a guide catheter. However, aortic or peripheral arterial conditions, such as a tortuous aorta, “bovine” aortic arch, type III aortic arch, or peripheral arterial occlusive lesions, sometimes limit the transfemoral access.[3,4,5] Difficulties in navigating guide catheters extend procedure time and result in poor outcomes.[6,7,8] Trans-brachial or-radial access is an alternative.[9] Balloon guide catheters (BGCs) with a large internal diameter (ID) and a large outer diameter (OD) are used to prevent distal embolization of thrombus fragments during MT.[10,11,12,13,14,15,16] Trans-brachial or radial access using a BGC, however, is not standard[17] and BGCs were used in only 6 of 18 trans-radial cases.[9] To prevent procedure time extension due to difficulties in navigating guide catheters through the transfemoral route, we implemented computed tomographic angiography (CTA) to evaluate the anatomical conditions of the aortic arch before MT. There have been few reports about the anatomical features for successful transbrachial insertion of BCGs with a large ID into the target artery, and transbrachial insertion of BGCs with a large ID was not always successful. It is, therefore, vital to find anatomical features necessary for successful transradial or brachial insertion of BGCs with a large ID into the target carotid artery.
This retrospective study aimed to find the anatomical features on CTA for successful transbrachial insertion of a BGC with a large ID.[17]
Materials and Methods
In this retrospective, cross-sectional study, we included AIS patients who: (1) were admitted to our institution between January 2014 and June 2016 due to internal carotid artery (ICA) or middle cerebral artery (MCA) occlusion, (2) underwent a single-phase CTA from the aortic arch to the intracranial vessels, and (3) underwent transbrachial MT using a BGC with a 9 French size (Fr) OD and a 7Fr ID without an introducer sheath. We evaluated occlusion sites and successful insertion rate of the BGC into the target carotid artery and measured takeoff angles at the turning point of the BGC as aortic arch anatomical features on CTA.
Computed tomographic angiography
We acquired images using an 80-row area detector computed tomographic scanner (Aquilion PRIME, Canon Medical Systems, Otawara, Tochigi, Japan). Acquisition started from the ascending aorta. After injecting 40 mL of a nonionic contrast medium (370 mg/mL iopamidol) at a rate of 3.8 mL/s, helical scans were acquired from the ascending aorta to the intracranial vessels.
Criteria for mechanical thrombectomy
Our criteria of MT for AIS were: (1) >6 on the National Institutes of Health Stroke Scale, (2) >6 on the diffusion-weighted image (DWI)-Alberta Stroke Program Early CT Score, (3) no signal in the ICA or the MCA on magnetic resonance angiography, and (4) DWI/perfusion-weighted images mismatch.[13]
Measurement of takeoff angles on computed tomographic angiography
We drew straight lines in the center of the orifices of two involved arteries in a direction parallel to the arterial directions. A turning point was defined as an intersection of the two lines while a takeoff angle was defined as an angle between two lines at the turning point [Figure 1]. We measured the takeoff angle between the right common carotid artery and the right subclavian artery in cases of right carotid insertion [Figure 1a and Figure 2], and the takeoff angle between the left common carotid artery and the brachiocephalic artery in cases of left carotid insertion [Figure 1b and Figure 3].
Figure 1.
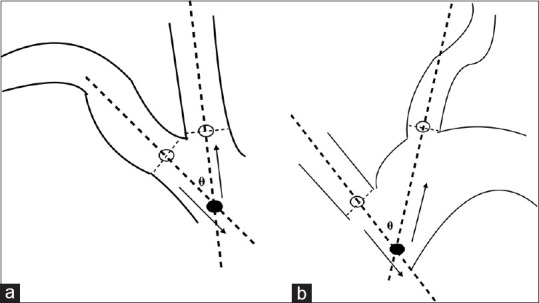
Measurement of the take-off angles. (a) In cases of right common carotid and subclavian arteries. (b) In cases of left common carotid and brachiocephalic arteries. Straight lines (broad dotted lines) are drawn at the center (white circles) of arterial orifices (thin dotted lines) in a direction parallel to the artery. The turning point (black circle) of a catheter (arrows) is the intersection of two lines. The take-off angle (θ) is the angle between the two lines
Figure 2.
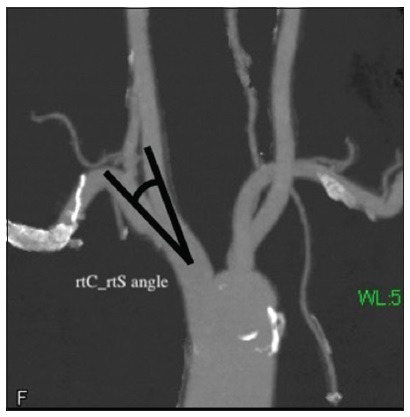
Computed tomography angiogram showing the take-off angle between the left common carotid artery and the brachiocephalic artery
Figure 3.
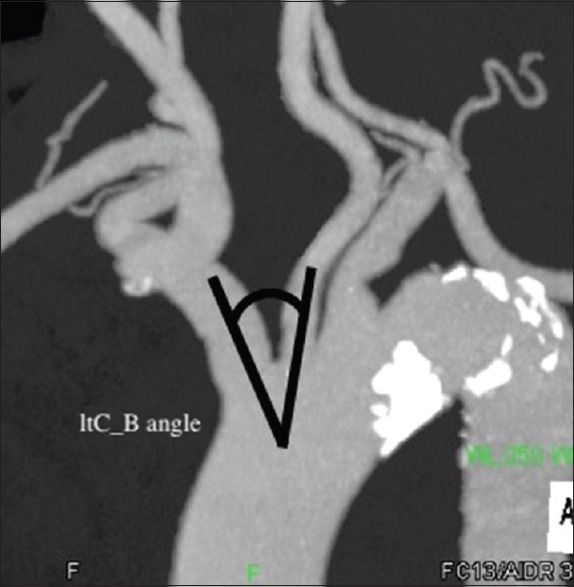
Computed tomography angiogram showing the take-off angle between the right common carotid artery and the right subclavian artery
Direct transbrachial insertion of a balloon guide catheter with a 9Fr outer diameter
The catheter with a 9Fr OD and a 7Fr ID was compatible with a 7Fr ID introducer sheath. The 9Fr OD is approximately 3 mm, and the ID of the brachial artery is about 5 mm. Therefore, we used the right brachial artery for direct insertion without an introducer sheath. We used a 22G needle for the right brachial artery puncture, subsequently inserting a 3F introducing sheath for dilatation of the puncture, inserted a 0.035-inch standard guidewire (Radifocus, Terumo, Tokyo, Japan) into the brachial artery, and replaced the 3F sheath with a 9Fr OD BGC (Optimo, 90 cm in length, 0.090-inch ID, Tokai Medical Products, Aichi, Japan). We inserted the 9Fr OD BGC directly into the brachial artery without a 9Fr ID introducing sheath. We advanced a 130-cm long 5Fr OD Simmons-type catheter through the BGC and a 0.035-inch guidewire into the target carotid artery [Figures 4a, b and 5a, b]. Then, we coaxially advanced the BGC [Figure 4c and 5c]. Once the BGC has been positioned, we inflated the balloon and started MT [Figures 4d and 5d].
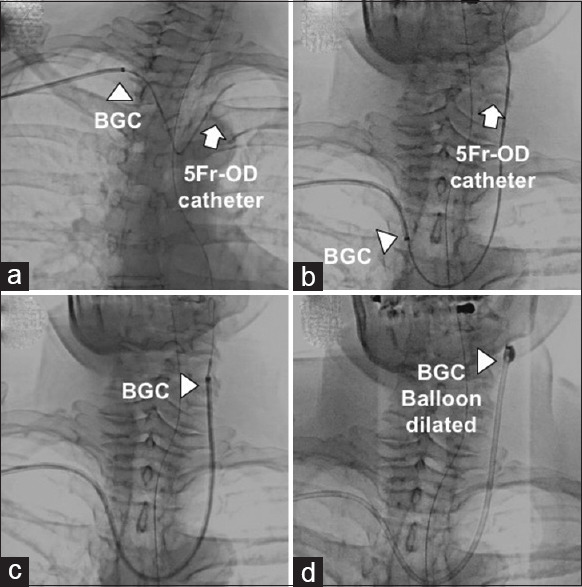
Figure 4.
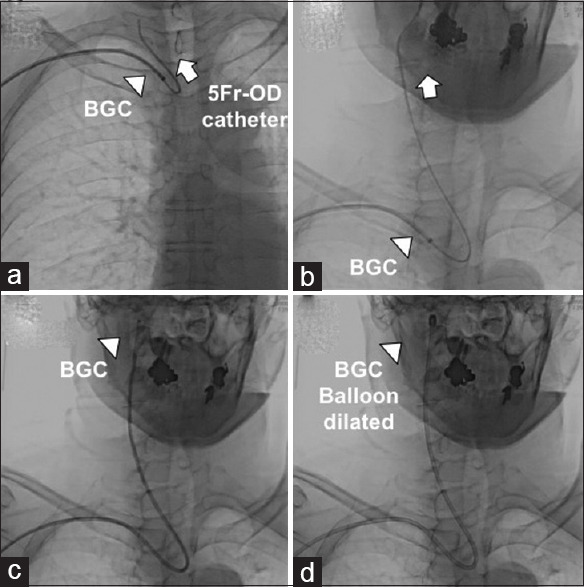
Sequential radiolucent images showing how to insert a balloon guide catheter into the right carotid artery with a take-off angle >to 25° between the right common carotid artery and the right subclavian artery. (a) Both the 5F catheter and the 0.035-inch guidewire were introduced into the right common carotid artery. (b) The 5F catheter was advanced into the right internal carotid artery. (c) A 9F balloon guide catheter was advanced coaxially into the right internal carotid artery. (d) The 5F catheter was withdrawn and the balloon was dilated
Figure 5.
Sequential radiolucent images showing how to insert a balloon guide catheter into the nonbovine left carotid artery with a take-off angle >to 23° between the left common carotid artery and the brachiocephalic artery. (a) A 5F catheter and a 0.035-inch guidewire were introduced into the left common carotid artery. (b) The 5F catheter was advanced into the left internal carotid artery. (c) A 9F balloon guide catheter was advanced coaxially into the left internal carotid artery. (d) The 5F catheter was withdrawn and the balloon was dilated
Ethics approval
All procedures performed in the study were in accordance with the ethical standards of the institution and with the 1964 Helsinki Declaration. The Institutional Ethical Committee approved our retrospective analysis (TGE01009-024).
Patient consent for publication
Written informed consent was not required because the procedure was routine medical care, the medical records of elderly patients treated several years ago were accessed retrospectively, and anonymization was done.
Statistical analysis
Nonnormally distributed continuous variables are expressed as medians and interquartile ranges (IQRs). Differences between two groups were compared using Fisher's exact test for categorical variables. P < 0.05 was considered statistically significant. The JMP software (version 15.1; SAS, NC, USA) was used for all the statistical analysis.
Results
Twenty-four patients met our inclusion criteria [Tables 1 and 2]. The median age was 81 (77–86) (IQR). Four of the 12 patients with left carotid occlusion had bovine arch demonstrated by CTA while the others suffered peripheral artery diseases. Four of the 12 patients with right carotid occlusion had Type III arch demonstrated by CTA while the others suffered from peripheral artery diseases. Operators determined transbrachial access in cases of the bovine arch for left carotid occlusion and in cases of Type III arch for right carotid occlusion, except for peripheral artery diseases [Tables 1 and 2].
Table 1.
Patients characteristics in the right carotid artery
| Case | Occlusion site | rtC_rtS angle (°) | BGC insertion | Arch type | Reason of brachial access |
|---|---|---|---|---|---|
| 1 | Right MCA | 72 | Success | I | Severe ASO |
| 2 | Right ICA | 65 | Success | III | Type III arch |
| 3 | Right MCA | 63 | Success | II | A_aneurysm |
| 4 | Right MCA | 43 | Success | II | A_aneurysm |
| 5 | Right ICA | 35 | Success | I | A_aneurysm |
| 6 | Right ICA | 32 | Success | I | Severe ASO |
| 7 | Right ICA | 31 | Success | III | Type III arch |
| 8 | Right ICA | 31 | Success | III | Type III arch |
| 9 | Right ICA | 30 | Success | II | A_aneurysm |
| 10 | Right ICA | 25 | Success | II | Severe ASO |
| 11 | Right ICA | 12 | Success | II | Severe ASO |
| 12 | Right ICA | 22 | Failure | III | Type III arch |
ICA: Internal carotid artery, MCA: Middle cerebal artery, rtC_rtS angle: Angle between the right common carotid artery and the right subclavian artery, BGC: Balloon guide catheter, A_aneurysm: Abdomincal aneurysm, ASO: Arteriosclerosis obliterans
Table 2.
Patients characteristics in the left carotid artery
| Case | Occlusion site | ltC_B angle (°) | BGC insertion | Arch type | Reason of brachial access |
|---|---|---|---|---|---|
| 1 | Left ICA | 57 | Success | Bovine | Bovine arch |
| 2 | Left ICA | 111 | Success | Bovine | Bovine arch |
| 3 | Left ICA | 62 | Success | Bovine | Bovine arch |
| 4 | Left MCA | 59 | Success | Bovine | Bovine arch |
| 5 | Left ICA | 38 | Success | I | Severe ASO |
| 6 | Left MCA | 25 | Success | II | A_aneurysm |
| 7 | Left ICA | 23 | Success | II | A_aneurysm |
| 8 | Left ICA | 3 | Failure | II | A_aneurysm |
| 9 | Left ICA | 7 | Failure | II | Severe ASO |
| 10 | Left ICA | 18 | Failure | I | Severe ASO |
| 11 | Left MCA | −8 | Failure | II | Severe ASO |
| 12 | Left MCA | 8 | Failure | II | Severe ASO |
ICA: Internal carotid artery, MCA: Middle cerebal artery, ltC_B angle: Angle between the left common carotid artery and the brachiocephalic artery, BGC: Balloon guide catheter, A_aneurysm: Abdomincal aneurysm, ASO: Arteriosclerosis obliterans
The overall transbrachial insertion success rate was 75% (18/24). We successfully advanced the BGC in only 7 (58.3%) of the 12 left carotid cases. We achieved successful insertion in 4 (100%) of the 4 bovine aortic arch cases, but in only 3 (37.5%) of the 8 nonbovine aortic arch cases. In 3 nonbovine cases with takeoff angles ≥23°, we achieved successful insertion. In 5 cases with takeoff angles <23°, we failed to insert (sensitivity: 100%, specificity: 100%, positive predictive value: 100%) (P < 0.05) [Table 3]. We successfully advanced the BGC in 11 (91.7%) of the 12 right carotid cases. We achieved successful insertion in 10 (100%) of 10 cases with take-off angles ≥25° (sensitivity: 91%, specificity: 100%, positive predictive value: 100%). In 1 of 2 cases with takeoff angles <25°, the BGC was broken immediately after the withdrawal of the coaxial 3Fr catheter [Table 3]. No puncture-site complications occurred in the 24 patients.
Table 3.
Computed tomography angiographic features and successful insertion
| Insertion of a 9Fr BGC | P | ||
|---|---|---|---|
| Success | Failure | ||
| The left carotid artery | |||
| Bovine aortic arch cases | 4 | 0 | |
| In nonbovine cases | |||
| Take-off (ltC_B) angle (°) | |||
| ≥23 | 3 | 0 | <0.05 |
| <23 | 0 | 5 | |
| The right carotid artery | |||
| Take-off (rtC_rtS) angle (°) | |||
| ≥25 | 10 | 0 | NS |
| <25 | 1 | 1 | |
ltC_B angle: Take-off angle between the left common carotid artery and the brachiocephalic artery, rtC_rtS angle: Take-off angle between the right common carotid artery and the right subclavian artery, BGC: Balloon guide catheter
Discussion
Our results demonstrated that takeoff angles at the turning point of the BGC on the CTA are critical for successful BGC transbrachial insertion. The CTA, which covered the aorta to the distal carotid arteries before MT, provided useful information for successful BGC transbrachial insertion.
To prevent distal migration of clots during MT procedures, proximal blood flow blockade using a BGC is standard for MT.[11,12,13,14,15,16] When a trans-brachial or-radial approach is necessary because of vascular conditions that limit femoral access, CTA provides a high likelihood of successful 9Fr (OD) BGC insertion. If the take-off angle at the turning point is very sharp, the BGC is abandoned for a 6Fr guide sheath without proximal flow blockade.[18,19,20]
Fortunately, we experienced no complications in the artery puncture site, such as arm ischemia, arterial occlusion, nerve injury, pseudoaneurysm, or hematoma, requiring treatment. We used a 22G needle for the brachial artery puncture and subsequent dilatation technique. We did not use any vascular closure devices, such as the Angio-Seal STS Plus (St. Jude Medical, Minneapolis MN, USA).[21,22] These are probably why no brachial artery or median nerve injuries occurred. Indeed, there are potential risks of brachial artery puncture complications, but the brachial or radial artery approach rarely leads to fatal complications, such as retroperitoneal hematomas, which are occasionally caused by femoral artery puncture.[23,24] The trans-brachial or-radial approach seems to be safer because of few life-threatening complications.
Limitations
Our study had several limitations, including its small number of patients and the retrospective cross-sectional study design. Operators' decision on the transbrachial access was dependent on their experiences. A prospective study with a large sample size is required to confirm our results.
Conclusions
The CTA provided a high likelihood of successful 9Fr OD BGC insertion without an introducer sheath. Successful transbrachial insertion was achieved in bovine left carotid cases, in nonbovine left carotid cases with takeoff angles ≥23°, and in right carotid cases with takeoff angles ≥25°.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgements
The authors would like to thank Miss Nozomi Chiba, BA, for her secretarial support, and the specialized support of the radiographers and nurses at our comprehensive stroke center.
References
- 1.Campbell BC, Mitchell PJ, Kleinig TJ, Dewey HM, Churilov L, Yassi N, et al. Endovascular therapy for ischemic stroke with perfusion-imaging selection. N Engl J Med. 2015;372:1009–18. doi: 10.1056/NEJMoa1414792. [DOI] [PubMed] [Google Scholar]
- 2.Goyal M, Demchuk AM, Menon BK, Eesa M, Rempel JL, Thornton J, et al. Randomized assessment of rapid endovascular treatment of ischemic stroke. N Engl J Med. 2015;372:1019–30. doi: 10.1056/NEJMoa1414905. [DOI] [PubMed] [Google Scholar]
- 3.Chang FC, Tummala RP, Jahromi BS, Samuelson RM, Siddiqui AH, Levy EI, et al. Use of the 8 French Simmons-2 guide catheter for carotid artery stent placement in patients with difficult aortic arch anatomy. J Neurosurg. 2009;110:437–41. doi: 10.3171/2008.7.17627. [DOI] [PubMed] [Google Scholar]
- 4.Iwata T, Mori T, Miyazaki Y, Nakazaki M, Takahashi Y, Mizokami K. Initial experience of a novel sheath guide for transbrachial carotid artery stenting: Technical note. J Neurointerv Surg. 2013;5(Suppl 1):i77–80. doi: 10.1136/neurintsurg-2012-010506. [DOI] [PubMed] [Google Scholar]
- 5.Mori T, Iwata T, Miyazaki Y, Tanno Y, Kasakura S, Yoshioka K, et al. Transbrachial approach as a first access route for neurointervention. Eur Radiol. 2014;ECR2014:C–1619. [Google Scholar]
- 6.Snelling BM, Sur S, Shah SS, Chen S, Menaker SA, McCarthy DJ, et al. Unfavorable vascular anatomy is associated with increased revascularization time and worse outcome in anterior circulation thrombectomy. World Neurosurg. 2018;120:e976–83. doi: 10.1016/j.wneu.2018.08.207. [DOI] [PubMed] [Google Scholar]
- 7.Spiotta AM, Vargas J, Turner R, Chaudry MI, Battenhouse H, Turk AS. The golden hour of stroke intervention: Effect of thrombectomy procedural time in acute ischemic stroke on outcome. J Neurointerv Surg. 2014;6:511–6. doi: 10.1136/neurintsurg-2013-010726. [DOI] [PubMed] [Google Scholar]
- 8.Prothmann S, Schwaiger BJ, Gersing AS, Reith W, Niederstadt T, Felber A, et al. Acute Recanalization of Thrombo-Embolic Ischemic Stroke with pREset (ARTESp): The impact of occlusion time on clinical outcome of directly admitted and transferred patients. J Neurointerv Surg. 2017;9:817–22. doi: 10.1136/neurintsurg-2016-012556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chen SH, Snelling BM, Sur S, Shah SS, McCarthy DJ, Luther E, et al. Transradial versus transfemoral access for anterior circulation mechanical thrombectomy: Comparison of technical and clinical outcomes. J Neurointerv Surg. 2019;11:874–8. doi: 10.1136/neurintsurg-2018-014485. [DOI] [PubMed] [Google Scholar]
- 10.Todo A, Minaeian A, Sahni R, Chao KH. Incidence and outcome of procedural distal emboli using the Penumbra thrombectomy for acute stroke. J Neurointerv Surg. 2013;5:135–8. doi: 10.1136/neurintsurg-2011-010216. [DOI] [PubMed] [Google Scholar]
- 11.Chueh JY, Kühn AL, Puri AS, Wilson SD, Wakhloo AK, Gounis MJ. Reduction in distal emboli with proximal flow control during mechanical thrombectomy: A quantitative in vitro study. Stroke. 2013;44:1396–401. doi: 10.1161/STROKEAHA.111.670463. [DOI] [PubMed] [Google Scholar]
- 12.Chueh JY, Puri AS, Wakhloo AK, Gounis MJ. Risk of distal embolization with stent retriever thrombectomy and ADAPT. J Neurointerv Surg. 2016;8:197–202. doi: 10.1136/neurintsurg-2014-011491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Imai K, Mori T, Izumoto H, Takabatake N, Kunieda T, Shimizu H, et al. Clot removal therapy by aspiration and extraction for acute embolic carotid occlusion. AJNR Am J Neuroradiol. 2006;27:1521–7. [PMC free article] [PubMed] [Google Scholar]
- 14.Imai K, Mori T, Izumoto H, Watanabe M. Successful thrombectomy in acute terminal internal carotid occlusion using a basket type microsnare in conjunction with temporary proximal occlusion: A case report. AJNR Am J Neuroradiol. 2005;26:1395–8. [PMC free article] [PubMed] [Google Scholar]
- 15.Iwata T, Mori T, Tajiri H, Miyazaki Y, Nakazaki M. Safety and effectiveness of emergency carotid artery stenting for a high-grade carotid stenosis with intraluminal thrombus under proximal flow control in hyperacute and acute stroke. J Neurointerv Surg. 2013;5:40–4. doi: 10.1136/neurintsurg-2011-010147. [DOI] [PubMed] [Google Scholar]
- 16.Velasco A, Buerke B, Stracke CP, Berkemeyer S, Mosimann PJ, Schwindt W, et al. Comparison of a balloon guide catheter and a non-balloon guide catheter for mechanical thrombectomy. Radiology. 2016;280:169–76. doi: 10.1148/radiol.2015150575. [DOI] [PubMed] [Google Scholar]
- 17.Mori T, Kasakura S, Tanno Y, Yoshioka K, Nakai N. Angiographic anatomical features for transbrachial carotid cannulation of a balloon-guide catheter. J Neurointerv Surg. 2016;8:A83. [Google Scholar]
- 18.Okawa M, Tateshima S, Liebeskind D, Ali LK, Thompson ML, Saver J, et al. Successful recanalization for acute ischemic stroke via the transbrachial approach. J Neurointerv Surg. 2016;8:122–5. doi: 10.1136/neurintsurg-2014-011451. [DOI] [PubMed] [Google Scholar]
- 19.Jadhav AP, Ribo M, Grandhi R, Linares G, Aghaebrahim A, Jovin TG, et al. Transcervical access in acute ischemic stroke. J Neurointerv Surg. 2014;6:652–7. doi: 10.1136/neurintsurg-2013-010971. [DOI] [PubMed] [Google Scholar]
- 20.Mokin M, Snyder KV, Levy EI, Hopkins LN, Siddiqui AH. Direct carotid artery puncture access for endovascular treatment of acute ischemic stroke: Technical aspects, advantages, and limitations. J Neurointerv Surg. 2015;7:108–13. doi: 10.1136/neurintsurg-2013-011007. [DOI] [PubMed] [Google Scholar]
- 21.Bangalore S, Arora N, Resnic FS. Vascular closure device failure: Frequency and implications: A propensity-matched analysis. Circ Cardiovasc Interv. 2009;2:549–56. doi: 10.1161/CIRCINTERVENTIONS.109.877407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Dregelid E, Jensen G, Daryapeyma A. Complications associated with the Angio-Seal arterial puncture closing device: Intra-arterial deployment and occlusion by dissected plaque. J Vasc Surg. 2006;44:1357–9. doi: 10.1016/j.jvs.2006.07.034. [DOI] [PubMed] [Google Scholar]
- 23.Trerotola SO, Kuhlman JE, Fishman EK. CT and anatomic study of postcatheterization hematomas. Radiographics. 1991;11:247–58. doi: 10.1148/radiographics.11.2.1827528. [DOI] [PubMed] [Google Scholar]
- 24.Sajnani N, Bogart DB. Retroperitoneal hemorrhage as a complication of percutaneous intervention: Report of 2 cases and review of the literature. Open Cardiovasc Med J. 2013;7:16–22. doi: 10.2174/1874192401307010016. [DOI] [PMC free article] [PubMed] [Google Scholar]


