Abstract
Purpose
Enrollment to antenatal care (ANC) is still not universal in Ethiopia. This study examines whether household food insecurity affects antenatal care attendance or not, as well as other factors associated with antenatal care. As optimal antenatal care is vital for the improvement of maternal and child health, the study will contribute to the efforts in improving maternal and child health.
Patients and Methods
A community-based cross-sectional study was conducted among 707 pregnant women at or above 3 months of self-reported pregnancy in Southern Ethiopia. Multi-stage sampling was employed to obtain the study units. Data were collected using an interviewer-administered structured questionnaire. Logistic regression analysis was conducted to identify the independent factors associated with study outcome.
Results
Out of a total of 707 study subjects, the majority (71%) of the study women visited a health facility for ANC service. The odds of ANC use was lower for women who were not in marital union (adjusted odds ratio (AOR)=0.39, 95% confidence interval (CI)=0.16–0.97), and those from food insecure households (AOR=0.50, 95% CI=0.32–0.79). ANC attendance was higher for women from high socio-economic status (AOR=2.62, 95% CI=1.29–5.29), with planned pregnancy (AOR=1.82, 95% CI=1.16–2.85) and a perceived risk from danger signs (AOR=4.32, 95% CI=1.60–11.67).
Conclusion
While the overall ANC use was high, women experiencing food insecurity and those with unplanned pregnancy were having lower odds of ANC attendance among others. Interventions targeting at enhancing women’s attendance to ANC service might be realized through commitment from the agriculture, economic, as well as health sectors by increasing productivity and providing special attention to women in the pre-pregnancy and pregnancy period. Moreover, educating women so that they can recognize that every pregnancy is risky and promotion of family planning to reduce unplanned pregnancy could improve attendance to the ANC service.
Keywords: antenatal care, food insecurity, Arba Minch Zuria Woreda, South Ethiopia
Introduction
Pregnancy is a crucial time to promote healthy behaviors and parenting skills. A prime care during this period is seen to be important in the improvement of maternal and child health.1 Antenatal care (ANC) is especial care given to pregnant women through public services with the aims of early detection of complications associated with pregnancy, taking prompt action in the presence of those complications, promotion of the wellbeing of the mother and the newborn, and prevention of diseases from the mother and newborn.2 ANC creates occasions for conveying health information and services that can enhance the health of women and their infants, though a significant reduction in maternal mortality is debatable.2–5 Yet there is sufficient evidence that ANC interventions (micronutrient supplementation, treatment of hypertension to prevent eclampsia, immunization against tetanus, HIV testing, and the use of prophylactic drugs to prevent mother-to-child transmission of HIV in cases of HIV-positive pregnant women, etc.) will improve maternal health, perinatal health, and at most perinatal survival.2,6
An optimal ANC links the woman and her family with the formal health system and contributes to good health through the life cycle. Being not able to receive or sub-optimal ANC breaks the link along the continuum of care, affecting the health of both women and their babies.1 Hence, ANC creates an opportunity to promote the use of skilled attendance at birth and health promoting behaviors such as breastfeeding, early postnatal care, and family planning. Health promoting behaviors can be particularly enhanced in areas where malaria is endemic through provision of medications and insecticide-treated mosquito nets to help prevent complications attributable to malaria.2,5,6 As Ethiopia is a country with a high burden of malaria and HIV,7–9 the importance of ANC is dual; increasing both maternal and newborn survival.5,6 Lowland areas of Arba Minch Zuria Woreda are recognized as one of the malaria endemic areas in the country.10
Globally, 86% of pregnant women receive ANC at least once from skilled health personnel and 62% receive at least four visits. The regions with the highest rates of maternal mortality, sub-Saharan Africa and South Asia, had a lesser attendance (52% and 46%, respectively) of at least four antenatal visits recently.6 In the years preceding 2016, only 32% of pregnant women in Ethiopia completed the four visits formerly recommended by WHO in the focused ANC,11,12 implying the need for further efforts in increasing the utilization of the service through identification of potential factors affecting it.
The Sustainable Development Goals (SDGs) now call for ensuring high quality sexual, reproductive, maternal, and newborn healthcare (pre- and post-natal care and others like emergency obstetric care) is available, accessible, and acceptable to all who need it as a guiding principle to end preventable maternal mortality.13 In 2016, the WHO launched a new model on ANC, which recommends pregnant women to have eight contacts with their healthcare provider (at 12, 20, 26, 30, 34, 36, 38, and 40 weeks’ gestation) for ANC in accordance with the SDGs. It is with the premise that increasing maternal and fetal assessments to detect complications increases the likelihood of positive pregnancy outcomes.14 In line with the global aspirations in the SDGs, Ethiopia in its current Health Sector Transformation Plan (HSTP) has given top priority to Reproductive, Maternal, Newborn, Child, Adolescent Health and Nutrition (RMNCAH). The proportion of women having at least four ANC visits is one of the core indicators to measure the universal health coverage index set for 20 years as of 2016.15
Existing evidence revealed that women’s age,16,17 income/wealth status,18–20 educational status,12,–15,–17–19,21,22 residence,15,17,18 birth order,15,23 religion,16 receiving advice from health extension workers or TV/radio,23 unplanned pregnancy,22,24 marital status,12 low knowledge of unhealthy pregnancy,24 number of pregnancy, number of live birth, place of delivery and the profession of birth attendants,25 illness experienced during past pregnancy,22 and perceived morbidity17 were factors associated with ANC service attendance.
Even though there are plenty of studies on ANC service use in Ethiopia,12,–17–19,22–25 to the best of the researchers’ knowledge, the potential factors assessed were limited to characteristics related to the individual woman and her partner. Recent evidence has shown that food insecurity predicted use of maternal healthcare services like ANC, skilled birth attendance,26,27 and family planning.28,29 Ethiopia is one of the world’s food insecure countries, with 10% of the population suffering from chronic food insecurity.30 Both urban and rural areas of the country are affected nearly alike. A study from a rural district in the Northern part of the country showed that nearly three quarters of the households (70.7%) had food insecurity and the situation was comparable in Addis Ababa, where 75% of households were food insecure.31,32 Documented in previous studies too, proximate socio-economic stressors, poverty and food vulnerability, had an impact on health service use behavior.33,34 This is supported by the concept of competing priorities of needs in life. The demand for food takes precedence over healthcare among women in food insecure conditions because of women’s dedication to fulfill their food needs before they decide to seek healthcare like antenatal care.35 Moreover, in developing countries like Ethiopia, women devote much more of their time and energy to household duties than seeking healthcare.36 Therefore, when women fail or get challenged to secure food, they will face the trade-off between fulfillment of food conditions and healthcare that will eventually end in non-use or under-use of healthcare in general and maternal healthcare in particular.
Cognizant to these evidences the present study hypothesized that women’s household food insecurity would be associated with their antenatal care attendance. Given the high magnitude of both problems in the country and a scarcity of such evidence in the Ethiopian setup, this study envisages that household food insecurity could be one of the barriers to attend ANC service and beheld its independent association controlling for the other factors stated above. Thus, the finding fills this gap by contributing to the scientific literature and it is expected to be of crucial importance for public health policy-making in the country. Specifically, mothers in the local set-ups will primarily benefit from the outputs of this study should the interventions for improvement of ANC attendance consider improving their household food security status in the community. This might suggest sectorial collaboration between the agriculture and health sectors so that pregnant women attending ANC should be targeted for food insecurity interventions.
Patients and Methods
Setting and Design of the Study
The study was conducted in Arba Minch Zuria woreda (woreda: an administrative unit corresponding to district in other parts of the world), Gamo Gofa Zone, South Ethiopia in March 2015. The woreda has 29 rural kebeles (smallest administrative units in the woredas in Ethiopia). Based on projection for the year 2014/2015 from the 2007 Ethiopian national census, the total population of the woreda was 205,204, with an estimated number of pregnant women equal to 7,101. At the time of the study, the woreda had six health centers and 37 health posts. Located at 505 km South of Addis Ababa, the capital city of Ethiopia, Arba Minch was the main town of both the Woreda and Gamo Gofa zone.37
The study employed a cross-sectional study design among pregnant women at or above 3 months of pregnancy in a community setting. Women reported their pregnancy status and months of gestation by themselves. The study participants were selected randomly from nine kebeles in the woreda. Those women who were not able to provide information either for serious acute illness or any other disability were excluded from the study for fear of not getting valid information. Likewise, those who did not live in the study area for at least 6 months were also excluded from participation in the study.
Sample Size and Sampling Procedure
This study is part of a previous study on 707 women38 from a thematic project on maternal and child healthcare utilization and food insecurity in Southern Ethiopia. The sample of women considered in the study was larger than sample sizes calculated using open epi software from ANC use estimates of two previous studies (86.3% and 28.5%) in the same region.17,22 The assumptions considered were 95% confidence, a pregnant population of 7,101, a design effect of 2, and a margin of error of 5%.
There are 29 rural kebeles in Arba Minch Zuria Woreda.37 The estimated number of pregnant women for each kebele was obtained by multiplying the total population of the kebeles by 3.46% (conversion factor for estimated number of pregnant women) in Southern Nations Nationalities and Peoples Region (SNNPR). The study subjects were selected using a multi-stage sampling technique. In the first stage, nine kebeles were selected from the 29 kebeles randomly. Proportional allocation of the sample was done to each kebele based on the number of pregnant women available in the kebele. A list of pregnant women was prepared using the current data from the monthly updated family folders in the health posts of each kebele. Secondly, the required numbers of pregnant women were selected randomly from the list in each kebele by using a SPSS generated random number of codes pre-assigned to each pregnant woman in the list. (Family folder: A service delivery tool or registration book at household level that contains members’ health and health related information and household characteristics, irrespective of their relationship in the household and marital status). Pregnancy identification was based on self-reported data from women themselves. Identification of pregnancy is made initially by leaders of the smallest 1–5 network of households at grass root level in their locale and continually reported to leaders of 30 households in the women development army (HDA) and then to the health extension workers (HEWs) in the health posts. While reports are collected in every contact of the HEWs with the HDA leaders, it is updated and compiled on a monthly basis.
Data Collection Method, Tools, and Procedure
After receiving a day long intensive training on the data collection process and instruments, seven public health nurses and two health officers collected the data and supervised the data collection, respectively. The questionnaire used for data collection was structured and administered by interviewers after being pre-tested in a kebele not selected for the study. ANC use was assessed using a questionnaire adapted from literature on ANC service attendance,16–25 and the Household Food Insecurity Access Scale (HFIAS) questionnaire by the Food and Nutrition Technical Assistance (FANTA III) was used to assess the household food insecurity status of women [39]. Health Development Army (HDA) leaders guided the data collectors and supervisors to the respective kebeles as well as households’ of the selected women. The list of pregnant women selected for the study with their respective kebeles was provided in advance to the data collectors.
Data Quality Management
The questionnaire initially prepared in English was translated to the local language Gamotho by an expert in the language and back translation was done to check its consistency with the original meaning by another expert having a very good skill in both languages. Data was collected using a structured Gammotho version questionnaire. Before commencing data collection, a pre-test was conducted in Chano Dorga kebele (one of the kebeles in the woreda that was not selected for the study) on 5% of the samples or 36 respondents. Based on the pretest, difficult or confusing items were revised. Each woman was interviewed in a separate private place to avoid social desirability bias. A completeness and update check was made on 30% of randomly picked samples of folders in each kebele, and the data collection period was set in line with the recent update.
Definitions and Measurement
Attended ANC service: when a woman had at least one visit to a health institution for checkup purpose during the current pregnancy.
Knowledgeable on danger signs: women who spontaneously mentioned two of the three key pregnancy danger signs (vaginal bleeding, swollen hands/face, and blurred vision) or three of the four key labor and delivery danger signs (severe vaginal bleeding, prolonged labor (>12 hours), convulsions, and retained placenta), or two of the three key postpartum danger signs (foul-smelling vaginal discharge, severe vaginal bleeding, and high fever).
Perceived risk from danger signs: Women who knew at least one of the key danger signs during pregnancy, labor, and delivery and the postpartum period and perceive that any of them could threaten their life (kill them or cause illness to them).
A household was classified as mildly food insecure if members of the household sometimes or often worry about not having enough food, and/or are not able to eat preferred foods, and/or eat a more monotonous diet than desired and/or some foods considered undesirable, but only rarely in the last 4 weeks (30 days).39
A household was classified as moderately food insecure if members of the household have started to reduce the number of meals or the size of meals in order to cut back on quantity, and/or sometimes or often eat undesirable foods or a monotonous diet, rarely or sometimes in the last 4 weeks (30 days).39
A household was classified as severely food insecure if members of the household have experienced any of the three conditions (going a whole day and night without eating, going to bed hungry, or running out of food) even once in the last 4 weeks (30 days).39
A household was considered as food insecure when it has any of the food insecurity conditions mentioned above (mild, moderate, or severe food insecure), otherwise it was classified as food secure or when it just experiences worry, but rarely.39
Data Analysis
Epidata version 3.1 and IBM SPSS statistics 20 were used for data entry and analysis, respectively. Findings were described using frequencies, percentages, means, and standard deviations. Binary logistic regression analysis was done in steps to identify independent predictors of ANC attendance. Initially, bivariate analysis was done to select candidate variables for multivariable regression analysis. Independent variables having an association with the outcome variable at a P-value<0.2540 and with public health importance based on prior strong significance were selected as candidate variables to fit the final multivariable analysis model. Variance Inflation Factor >10 was used as a criterion to check the existence of multicollinearity between the candidate variables. Lastly, the final multivariable analyses model was fitted between the candidate independent variables and the outcome variable in order to control for possible confounding and determine the presence of statistically significant association. The fitness of the final model was checked using Hosmer and Lemeshow goodness of fitness test. A backward elimination method was used to select the variables in the regression model. Statistical significance was declared at a P-value of <0.05, and the degree of association between independent variables and the outcome variable was measured by AOR with its 95% CI. Seventeen explanatory variables (women’s age, educational status, marital status, occupation, habit of listening to the radio, household wealth and food insecurity status, gravidity, parity, plan of pregnancy, age at first pregnancy, place of previous birth, history of still birth, history of abortion/miscarriage, knowledge on danger signs and perceived risk from danger signs, partner’s educational status) were fitted to bivariate logistic regression model to select potential candidates for multivariable analysis. Women’s age, gravida, age at first pregnancy, and partner’s educational status did not fulfill the selection criteria and hence were not selected for multivariable analysis. A household wealth/economic status of the study women was set from 13 items on common permanent assets in the study area using a principal component analysis method of data reduction. The items were removed at various iteration steps after checking the fulfillment of assumptions for principal component analysis using Kaiser-Meyer-Olkin measure of sampling adequacy and Bartlett’s Test of Sphericity.
Results
ANC Service Attendance
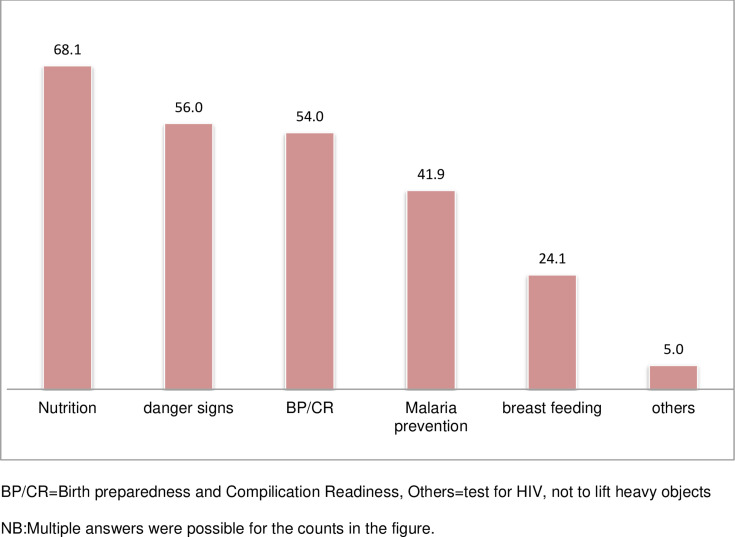
The majority of women in the study (87.2%) had heard about ANC service and few (12.8%) had never heard about the service. Out of those who had heard about the service, the majority (81.5%) received it during the current pregnancy. The overall ANC service attendance was 71% (95% CI=67.3–74.1%). Only 70 (13.9%) of them attended ANC at least four times, and this comprises 9.9% of the total eligible women of the study. With regard to women’s reasons for using ANC service, 304 (60.2%) used it to improve their general health condition, 254 (50.6%) used the service to know the condition of the current pregnancy, and 63 (12.6%) used the ANC service to gain information on appropriate nutrition (multiple answers were allowed). The majority of the study women (91.8%) on ANC follow-up received advices about their pregnancy, delivery, and postnatal care (Figure 1).
Figure 1.
Advice received during ANC among pregnant women in Arba Minch Zuria woreda, Gamo Gofa Zone, SNNPR, March 2015.
Notes: BP/CR, birth preparedness and complication readiness; Others, test for HIV, not to lift heavy objects. NB: Multiple answers were possible for the counts in the figure.
ANC Service Attendance by Women’s Socio-Demographic Characteristics
About two-thirds of the respondents (66.9%) were aged 20–34 years, with mean age being 27.2±5.5 years. The vast majority (676, 95.6%) were married, while nearly half (47.8%) of the study participants were housewives. Regarding their education, around a third (35.9%) of the respondents and more than a third (40.6%) were illiterate (not able to read and write) and attended primary education, respectively.
Among those women who received ANC service, 69.1% were in the age range of 20–34 years, and 96.8% were in marital union. Two hundred and twenty-four (44.7%) of the ANC users attended primary school level education and about 216 (59%) of them reported that they did not ever listen to the radio. With regard to their household food security status, 248 (49.4%) of ANC users were from food insecure households (Table 1).
Table 1.
ANC Service Attendance Among Pregnant Women in Arba Minch Zuria Woreda by Their Socio-Demographic and Economic Characteristics, March 2015
| Variables (N=707) | Category | Attended ANC Service | |
|---|---|---|---|
| Yes | No | ||
| Age | Less than 20 | 60 (12%) | 29 (14.1%) |
| 20–34 | 347 (69.1%) | 126 (61.5%) | |
| 35 and above | 95 (18.9%) | 50 (24.4%) | |
| Educational status | Illiterate | 160 (31.9%) | 94 (45.9%) |
| Read and write | 44 (8.8%) | 27 (13.2%) | |
| Primary education | 224 (44.7%) | 63 (30.7%) | |
| Secondary education | 73 (14.6%) | 21 (10.2%) | |
| Marital status | In marital union | 486 (96.8%) | 190 (92.7%) |
| Not in marital union | 16 (3.2%) | 15 (7.3%) | |
| Occupation | Farmer | 231 (46%) | 107 (52.2%) |
| Housewives | 185 (36.9%) | 64 (31.2%) | |
| Others | 86 (17.1%) | 34 (16.6%) | |
| Wealth index | Low | 116 (23.2) | 87 (42.4%) |
| Low–medium | 104 (20.8%) | 45 (22%) | |
| Medium–high | 84 (16.8%) | 39 (19%) | |
| High | 196 (39.2%) | 34 (16.6%) | |
| Ever listened radio | Yes | 286 (41%) | 84 (57%) |
| No | 216 (59%) | 121 (43%) | |
ANC Service Attendance by Respondents’ Obstetric Characteristics
Four hundred and thirty (85.7%) of the ANC users were having a pregnancy of 2 or more (multigravida) and 238 (55.6%) were having parity of 2–4. Two-thirds (66.7%) of the ANC users planned their current pregnancy and the remaining one-third did not want to get pregnant. With regard to women’s age at first pregnancy, 292 (58.2%) of ANC users reported that they got pregnant at 18 years of age and above. In this study, more than half of women using ANC services (51.7%) gave their last birth at their home and 11.1% and 19.1% of ANC users had a history of stillbirth and abortion, respectively. Those women who did not use ANC service had a slightly higher rate of history of abortion and stillbirth (13.9% and 20.1%, respectively) (Table 2).
Table 2.
ANC Service Attendance Among Pregnant Women in Arba Minch Zuria Woreda by Their Obstetric Characteristics, March 2015
| Variables | Category | Attended ANC Service | |
|---|---|---|---|
| Yes | No | ||
| Gravida (N=707) | 2 and above | 430 (85.7%) | 158 (77.1%) |
| 1 | 72 (14.3%) | 47 (22.9%) | |
| Planned pregnancy (N=707) | Yes | 335 (66.7%) | 85 (41.5%) |
| No | 167 (33.3%) | 120 (58.5%) | |
| Age at first pregnancy (N=707) | Less than 18 | 210 (41.8%) | 72 (35.1%) |
| 18 and above | 292 (58.2%) | 133 (64.9%) | |
| Parity (N=583) | One | 158 (36.9%) | 45 (29%) |
| Two to four | 238 (55.6%) | 94 (60.6%) | |
| Five and above | 32 (7.5%) | 16 (10.3%) | |
| Place of last birth (N=589) | At home | 223 (51.7%) | 116 (73.4%) |
| At health institution | 208 (48.3%) | 42 (26.6%) | |
| History of still birth (N=589) | Yes | 48 (11.1%) | 22 (13.9%) |
| No | 383 (88.9%) | 136 (86.1%) | |
| History of abortion/miscarriage (N=588) | Yes | 82 (19.1%) | 32 (20.1%) |
| No | 347 (80.9%) | 127 (79.9%) | |
| Perception of future risk in pregnancy (N=707) | Yes | 377 (75.1%) | 84 (41%) |
| No | 125 (24.9%) | 121 (59%) | |
| Knowledgeable on danger signs (N=707) | Yes | 393 (78.3%) | 92 (44.9%) |
| No | 109 (21.7%) | 113 (55.1%) | |
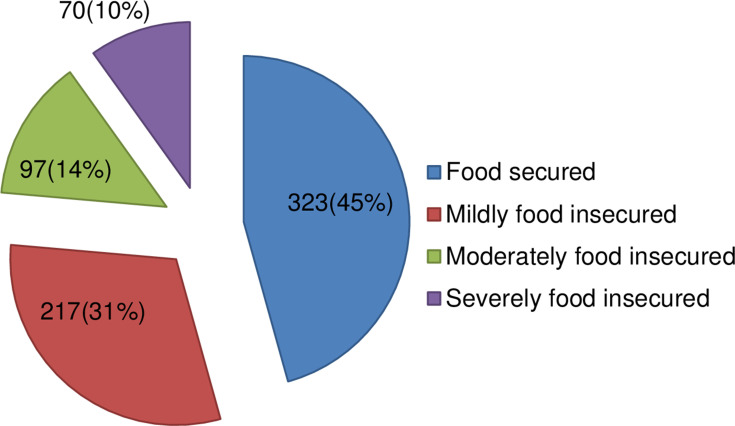
ANC Service Attendance by Women’s Household Food Security Status
More than half (54.3%) of the study women were from food insecure households and the rest (45.7%) were living in food secured households. The different degrees of household food insecurity among the study women are shown in Figure 2.
Figure 2.
Different degrees of food insecurity among pregnant women in Arba Minch Zuria woreda, Gamo Gofa Zone, SNNPR, March 2015.
One hundred and forty, 67 and 41 (27.9%, 13.4%, and 8.2%) of ANC users were from mildly, moderately, and severely food insecure households, respectively, and a total of 248 (49.4%) of ANC users were from food insecure households (Table 3).
Table 3.
ANC Service Attendance Among Pregnant Women in Arba Minch Zuria Woreda by Their Food Security Status, March 2015
| Variables (N=707) | Category | Attended ANC service | |
|---|---|---|---|
| Yes | No | ||
| Mildly food insecure | Yes | 140 (27.9%) | 77 (37.6%) |
| No | 361 (72.1%) | 128 (62.4%) | |
| Moderately food insecure | Yes | 67 (13.4%) | 30 (14.7%) |
| No | 434 (86.6%) | 174 (85.3%) | |
| Severely food insecure | Yes | 41 (8.2%) | 29 (14.2%) |
| No | 459 (91.8%) | 175 (85.8%) | |
| Food insecure | Yes | 248 (49.4%) | 136 (66.3%) |
| No | 254 (50.6%) | 69 (33.7%) | |
Factors Affecting Attendance to ANC Service Among Pregnant Women in Arba Minch Zuria Woreda
The odds of attending ANC were lower among women not in a marital union than those who were in a marital union (AOR=0.39, 95% CI=0.16–0.97). Similarly, women from food insecure households had lower odds of using ANC services than those from food secure households (AOR=0.50, 95% CI=0.32–0.79). However, the odds of attendance to ANC services was 2.62-times higher in women from high socio-economic status than those from a ow socio-economic group (AOR=2.62, 95% CI=1.29–5.29). Similarly, the odds of attendance to ANC service was 1.82-times higher in women whose current pregnancy was planned than those whose current pregnancy was unwanted (AOR=1.82, 95% CI=1.16–2.85). Perception of a future risk to health has also shown a positive association with women’s attendance to ANC services. Women who perceive that risks will happen to their future pregnancy career had 4.32-times higher odds of using ANC service than those who do not have such concern (AOR=4.32, 95% CI=1.60–11.67) (Table 4).
Table 4.
Factors Affecting ANC Service Attendance Among Pregnant Women in Arba Minch Zuria Woreda, Gamo Gofa Zone, South Ethiopia, March 2015
| Variables | Category | Attendance to ANC Service | Crude OR (95% CI) | Adjusted OR (95% CI) | |
|---|---|---|---|---|---|
| Yes | No | ||||
| Educational status | Illiterate | 160 (31.9%) | 94 (45.9%) | 1 | 1 |
| Read and write | 44 (8.8%) | 27 (13.2%) | 0.96 (0.56–1.65) | 0.61 (0.28–1.33) | |
| Primary education | 224 (44.7%) | 63 (30.7%) | 2.09 (1.43–3.05)b | 1.37 (0.75–2.51) | |
| Secondary education | 73 (14.6%) | 21 (10.2%) | 2.04 (1.18–3.53)b | 0.65 (0.25–1.66) | |
| Marital status | In marital union | 486 (96.8%) | 190 (92.7%) | 1 | 1 |
| Not in marital union | 16 (3.2%) | 15 (7.3%) | 0.42 (0.21–0.86)b | 0.39 (0.16–0.97)c | |
| Occupation | Farmer | 231 (46%) | 107 (52.2%) | 1 | 1 |
| Housewives | 185 (36.9%) | 64 (31.2%) | 1.34 (0.93–1.93) | 1.55 (0.93–2.58) | |
| Othersa | 86 (17.1%) | 34 (16.6%) | 1.17 (0.74–1.85) | 1.44 (0.73–2.85) | |
| Quintiles of wealth/SES | Low | 116 (23.%) | 87 (42.4%) | 1 | 1 |
| Low–medium | 104 (20.8%) | 45 (22%) | 1.73 (1.12–2.71)b | 1.54 (0.81–2.92) | |
| Medium–high | 84 (16.8%) | 39 (19%) | 1.62 (1.01–2.58)b | 1.30 (0.63–2.69) | |
| High | 196 (39.2%) | 34 (16.6%) | 4.33 (2.74–6.84)b | 2.62 (1.29–5.29)c | |
| Ever listened to radio | Yes | 286 (41%) | 84 (57%) | 1.91 (1.37–2.65)b | 1.03 (0.61–1.75) |
| No | 216 (59%) | 121 (43%) | 1 | 1 | |
| Food insecure | Yes | 248 (49.4%) | 136 (66.3%) | 0.49 (0.35–0.69)b | 0.50 (0.32–0.79)c |
| No | 254 (50.6%) | 69 (33.7%) | 1 | 1 | |
| Planned pregnancy | Yes | 335 (66.7%) | 85 (41.5%) | 2.83 (2.03–3.96)b | 1.82 (1.16–2.85)c |
| No | 167 (33.3%) | 120 (58.5%) | 1 | 1 | |
| Parity | One | 158 (36.9%) | 45 (29%) | 1 | 1 |
| Two to four | 238 (55.6%) | 94 (60.6%) | 0.72 (0.48–1.08) | 0.76 (0.47–1.24) | |
| Five and above | 32 (7.5%) | 16 (10.3%) | 0.57 (0.28–1.13) | 1.15 (0.49–2.69) | |
| Place of last birth | At home | 223 (51.7%) | 116 (73.4%) | 1 | 1 |
| At health institution | 208 (48.3%) | 42 (26.6%) | 2.57 (1.73–3.84)b | 1.47 (0.92–2.35) | |
| History of still birth | Yes | 48 (11.1%) | 22 (13.9%) | 0.77 (0.45–1.33) | 0.68 (0.34–1.37) |
| No | 383 (88.9%) | 136 (86.1%) | 1 | 1 | |
| History of abortion/miscarriage | Yes | 82 (19.1%) | 32 (20.1%) | 0.94 (0.59–1.48) | 0.85 (0.46–1.55) |
| No | 347 (80.9%) | 127 (79.9%) | 1 | 1 | |
| Knowledgeable on danger signs | Yes | 393 (78.3%) | 92 (44.9%) | 4.43 (3.13–6.27)b | 1.12 (0.41–3.04) |
| No | 109 (21.7%) | 113 (55.1%) | 1 | 1 | |
| Perceived risk from danger signs | Yes | 377 (75.1%) | 84 (41%) | 4.34 (3.08–6.13)b | 4.32 (1.60–11.67)c |
| No | 125 (24.9%) | 121 (59%) | 1 | 1 | |
Notes: aCarpenter, daily laborer, etc. bSignificant at bivariate analysis at P-value of <0.25, cSignificant at multivariable analysis at P-value of <0.05. Adjusted for women’s educational status, marital status, occupation, habit of listening radio, household wealth and food insecurity status, parity, plan of pregnancy, place of previous birth, history of still birth, history of abortion/miscarriage, knowledge on danger signs and perceived risk from danger signs.
Abbreviations: SES, socio-economic status; COR, crude odds ratio; AOR, adjusted odds ratio.
Discussion
In 2016, WHO launched a new model on ANC that recommends an increase in the number of ANC visits from the former four focused ANC to eight contacts with a skilled healthcare worker with the premise that an increase in the number of quality ANC contacts would result in a healthy pregnancy outcome.14 However, in this study, 71% of women visited for ANC at least once and only 9.9% had four and above visits to a skilled healthcare worker implying increased efforts in the promotion of the service in the area. ANC attendance was relatively lower than findings from other African countries16,41,42 and Ethiopia,17,19,23,24 but it was higher than some other studies in the country.12,18,22 This implies that ANC service use in Ethiopia is at varying magnitudes across different regions and settings of the same region. Although the target women in this study have the potential to have some more visits, 29% of them did not start to use the service in the appropriate time14 implying an increased effort in meeting timely attendance to the ANC.
Marital status was found to affect ANC service use in this study; where being not in a marital union was associated with lower odds of utilizing ANC as compared to being in marital union. This is in agreement with a study from Tigray, Northern Ethiopia.12 This can be explained by the fact that married women might have the chance getting support from their husbands in initiation of the service as male involvement increases utilization of maternal healthcare services.43,44 On the other hand, the unmarried groups are more likely to be household heads having responsibilities that deter them from receiving such services. Moreover, being in wedlock increases women’s confidence in utilizing public health services owing to reduced stigma and discrimination from the community around them.45 The finding suggests a tailored approach to unmarried women with special promotion of the benefits of ANC attendance and thorough follow-up by healthcare professionals in the ANC clinic.
In recently published studies, food insecurity was found to be an independent factor of maternal healthcare utilization.26–29 This study also has a consistent finding where the odds of ANC use was lower for women from food insecure households than those from food secure households. This may be explained by the fact that in developing countries like Ethiopia, women spend much of their time on household duties than on their health.36 Hence, women in food insecure households might be averted from seeking for ANC as demand for food takes precedence over demand for healthcare.35 Though getting rid of food insecurity is a challenging situation in Ethiopia, with 10% of the population having chronic food insecurity,30 the country has made considerable advancement towards food security as evidenced by an increase in crop yields and availability.15 Therefore, in the long run, efforts to culminate its effect should at least target pregnant women so that they might have better access to maternal health services and subsequently a favorable pregnancy outcome.14 Likewise, socio-economic status has been independently associated with ANC attendance in which being from a high socio-economic status increased the odds of ANC attendance. This is in line with previous studies.18–20 Even though maternal healthcare services are free of charge these days in Ethiopia,46 women from higher economic classes would tend to be in a better position in decision-making on household matters including their choice of healthcare services.47,48 The findings might denote that women’s ANC attendance stems from meeting their most basic needs like boosting household wealth in general and access to food in particular.
Planning on pregnancy has shown an association with ANC attendance in previous studies.22,24,49 Our study showed a similar finding. Women whose current pregnancy was planned had 1.82-times higher odds of using ANC than those whose current pregnancy was unplanned. This could be explained by the fact that women with unplanned pregnancies may not easily accept their pregnancies by themselves and neglect caring to themselves and the growing fetus. In Ethiopia, women with unplanned pregnancies are more likely to be not in a marital union and the stigma associated with out-of-wedlock pregnancies might demotivate them from utilizing public health services like ANC.45 This suggests the existence of an unmet need for family planning in this rural community and its bad consequence on the reproductive healthcare seeking behavior of women and calls for fostering the integration between reproductive health services.
Knowledge on danger signs did not show a significant association with ANC attendance in the present study, though women with a low knowledge on unhealthy pregnancy were less likely to use ANC service from a study in Northern Ethiopia, Tigray region and from a review on cultural barriers of maternal healthcare utilization in Ethiopia.24,50 However, women’s perceived future risks of the danger signs was found to be an independent predictor for their ANC attendance where those having such perception (as measured by perceived threats of danger signs) had 4.32-times higher odds of attending ANC services than those who do not have such a concern. The finding is in line with a study in Hadiya zone, South Ethiopia where women who consider pregnancy as a risky event had higher odds of ANC use.17 The possible explanation to this could be such women might be forced to use the service owing to their concern on possible threats to their health. This might suggest that improving knowledge on danger signs should be promoted with creation of positive and receptive attitudes.
The study has few limitations. The pregnancy status and months of gestation was not confirmed by an ultrasound or any laboratory investigation; it was based on self-reports from the women. This might result in an inability to identify the state of pregnancy particularly among primiparous women and alter the months of gestation. Consideration of pregnant women for this study could pose exclusion of those women having the potential to attend ANC service or have some more visits. The general sampling of women without any consideration to pregnancies among vulnerable and stigmatized populations like servants and unmarried women in a household could lead to under-reporting of the actual number of pregnancies. Hence, the findings of this study need to be interpreted within these limitations.
Conclusion
The study revealed a relatively higher ANC service attendance in the study area. The odds of ANC attendance was lower for women from food insecure households and those who were not in a marital union. Women from high household wealth, with perceived future risk from danger signs and with a planned pregnancy, had a higher likelihood of ANC service attendance.
Efforts in increasing ANC service attendance should consider improving women’s household food security and socio-economic/wealth status. Moreover, promotions of planned pregnancy through improvement of access to family planning service are needed in the efforts to improve antenatal care attendance. Particular attention is needed among unmarried and poorer women. Health workers at various levels have to strengthen their efforts in developing positive attitude among women through realization of the perception that every pregnancy carries a risk. Future research could explore the relationship between food insecurity and ANC attendance in more depth through qualitative or intervention-based approaches.
Acknowledgments
Our sincere appreciation and warmest thanks goes to the supervisors, data collectors, and the study participants for their willingness and cooperation in the data collection process. Our gratitude should also be extended to health extension workers for their assistance in community mobilization and information provision from the family folder.
Funding Statement
The study was funded by Jimma University, College of health sciences. The university had no role in the design, analysis, and interpretation of data and in writing of the manuscript. The study was conducted by the full responsibility of the authors.
Data Sharing Statement
The dataset supporting the conclusions of this article can be obtained from the corresponding author upon reasonable request.
Ethics Approval and Informed Consent
Ethical clearance was obtained from Jimma University Ethical Review Committee and the study was conducted in accordance with the Declaration of Helsinki. By the approval of the IRB, verbal informed consent was obtained from the study subjects as some of them were not able to read and write and they were assured that the information will not be disclosed to any one out of the research team. A formal letter of permission to conduct the study was obtained from Gamo Gofa zone health desk and subsequently from Arba Minch Zuria Woreda Health office. The participants were informed about the purpose and objectives of the study.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising, or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure
The authors declared that they have no competing interests.
References
- 1.Lincetto O, Mothebesoane-Anoh S, Gomez P, Munjanja S. Antenatal care. Opportunities for Africa’s newborn; 2006:55–62.
- 2.WHO. Antenatal Care in Developing Countries: Promises, Achievements and Missed Opportunities. An Analysis of Trends, Levels and Differentials. 1990–2001. Geneva, Switzerland: WHO; 2003. [Google Scholar]
- 3.Mcdonagh M. Is antenatal care effective in reducing maternal morbidity and mortality? Health Policy Plan. 1996;11(1):1–15. doi: 10.1093/heapol/11.1.1 [DOI] [PubMed] [Google Scholar]
- 4.WHO. Maternal Health and Safe Motherhood Programme .Division of Family Health. Antenatal Care and Maternal Health. How Effective is It? Geneva. Switzerland: 1992. WHO/MSM/92.4 [Google Scholar]
- 5.Oyerinde K. Can antenatal care result in significant maternal mortality reduction in developing countries? J Community Med Health Educ. 2013;3:2. doi: 10.4172/2161-0711.1000e116 [DOI] [Google Scholar]
- 6.UNICEF data: monitoring the situation of children and women. Maternal health/antenatal care; 2017. Available from: http://s20036.p584.sites.pressdns.com/maternal-health/antenatal-care#sthash.W01W4q5P.dpuf. Accessed October16, 2020.
- 7.Alelign A, Dejene T. Current status of malaria in Ethiopia: evaluation of the burden, factors for transmission and prevention methods. Acta Parasitol Glob. 2016;7(1):01–06. [Google Scholar]
- 8.Deribew A, Dejene T, Kebede B, et al. Incidence, prevalence and mortality rates of malaria in Ethiopia from 1990 to 2015: analysis of the global burden of diseases 2015. Malar J. 2017;16:271. doi: 10.1186/s12936-017-1919-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.WHO. CDC, Ethiopia. HIV/AIDS progress report. WHO country office, Addis Abeba, Ethiopia; 2014. Available from: http://www.afro.who/int/en/Ethiopia/who-country-office-ethiopia.html. Accessed October16, 2020.
- 10.Gammo Goffa Zone, Culture and Tourism Department. Woga Gammo Goffa; 2014. [Google Scholar]
- 11.Central Statistical Agency (CSA) [Ethiopia] and ICF. Ethiopia Demographic and Health Survey 2016. Addis Ababa, Ethiopia, and Rockville, Maryland, USA: CSA and ICF; 2016. [Google Scholar]
- 12.Tsegay Y, Gebrehiwot T, Goicolea I, et al. Determinants of antenatal and delivery care utilization in Tigray region, Ethiopia: across-sectional study. Int J Equity Health. 2013;12:30. doi: 10.1186/1475-9276-12-30 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.UNDP. UNFPA. UNICEF. WHO. WORLD BANK. Human Reproduction Programme. Strategies Toward Ending Preventable Maternal Mortality (EPMM). Geneva, Switzerland: World Health Organization; 2015. [Google Scholar]
- 14.Tuncalp Ӧ, Pena-Rosas JP, Lawrie T, et al. WHO recommendations on antenatal care for a positive pregnancy experience—going beyond survival. BJOG. 2017;124:860–862. doi: 10.1111/1471-0528.14599 [DOI] [PubMed] [Google Scholar]
- 15.The Federal Democratic Republic of Ethiopia, Ministry of Health. Health Sector Transformation Plan; 2015.
- 16.Nketiah-Amponsah E, Senadza B, Arthur E. Determinants of utilization of antenatal care services in developing countries: recent evidence from Ghana. Afr J Econ Manag Stud. 2013;4(1):58–73. doi: 10.1108/20400701311303159 [DOI] [Google Scholar]
- 17.Abosse Z, Woldie M, Ololo S. Factors influencing antenatal care service utilization in Hadiya Zone. Ethiop J Health Sci. 2010;20(2). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Gurmesa T. Antenatal care service utilization and associated factors in Metekel Zone, Northwest Ethiopia. Ethiop J Health Sci. 2009;19(2). [Google Scholar]
- 19.Alemayehu T, Haidar J, Habte D. Utilization of antenatal care services among teenagers in Ethiopia: a cross sectional study. Ethiop J Health Dev. 2010;24(3):221–225. [Google Scholar]
- 20.Nisar N, White F. Factors affecting utilization of antenatal care among reproductive age group women (15–49 years) in an urban squatter settlement of Karachi. J Pak Med Assoc. 2003;53(2). [PubMed] [Google Scholar]
- 21.Yesuf EA, Calderon-Margalit R. Disparities in the use of antenatal care service in Ethiopia over a period of fifteen years. BMC Pregnancy Childbirth. 2013;13:131. doi: 10.1186/1471-2393-13-131 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Tewodros B, Dibaba Y. Factors affecting antenatal care utilization in Yem Special Woreda, Southwestern Ethiopia. Ethiop J Health Sci. 2009;19(1). [Google Scholar]
- 23.Regassa N. Antenatal and postnatal care service utilization in southern Ethiopia: a population-based study. Afr Health Sci. 2011;11(3):390–397. [PMC free article] [PubMed] [Google Scholar]
- 24.Berhe KK, Welearegay HG, Abera GB, Kahsay HB, Kahsay AB. Assessment of antenatal care utilization and its associated factors among 15 to 49 years of age women in Ayder Kebelle, Mekelle City 2012/2013; a cross sectional study. Am J Adv Drug Deliv. 2014;62:75. [Google Scholar]
- 25.Dulla D, Daka D, Wakgari N. Antenatal care utilization and its associated factors among pregnant women in Boricha District, Southern Ethiopia. Divers Equal Health Care. 2017;14(2):76–84. doi: 10.21767/2049-5471.100096 [DOI] [Google Scholar]
- 26.McCoy S, Buzdugan R, Mushavi A, Mahomva A, Cowan F, Padian N. Food insecurity is a barrier to service uptake in the prevention of mother to child HIV transmission (PMTCT) cascade in Zimbabwe. BMC Public Health. 2015. doi: 10.1186/s12889-015-1764-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Bishwajit G, Yaya S. Household food insecurity is independently associated with poor utilization of maternal healthcare services in Bangladesh. FACETS. 2017;2:969–983. doi: 10.1139/facets-2017-0018 [DOI] [Google Scholar]
- 28.Feyisso M, Belachew T, Tesfay A, Addisu Y. Differentials of modern contraceptive methods use by food security status among married women of reproductive age in Wolaita Zone, South Ethiopia. Arch Public Health. 2015;73:38. doi: 10.1186/s13690-015-0089-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Diamond-Smith N, Raj A, Prata N, Weiser SD. Associations of women’s position in the household and food insecurity with family planning use in Nepal. PLoS One. 2017;12(4):e0176127. doi: 10.1371/journal.pone.0176127 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Endalew B, Muche M, Tadesse S. Assessment of food security situation in Ethiopia: a review. Asian J Agric Res. 2015;9(2):55–68. doi: 10.3923/ajar.2015.55.68 [DOI] [Google Scholar]
- 31.Endale W, Birhanu Z, Atinafu A, Awoke A. Food Insecurity in Farta District, Northwest Ethiopia: a community based cross–sectional study. BMC Res Notes. 2014;7:130. doi: 10.1186/1756-0500-7-130 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Gezimu G. Determinants of food insecurity among households in Addis Ababa city, Ethiopia. INDECS. 2012;10(2):159–173. doi: 10.7906/indecs.10.2.9 [DOI] [Google Scholar]
- 33.Sundari Ravindran TK. Poverty, food security and universal access to sexual and reproductive health services: a call for cross-movement advocacy against neoliberal globalisation. Reprod Health Matters. 2014;22(43):14–27. doi: 10.1016/S0968-8080(14)43751-0. [DOI] [PubMed] [Google Scholar]
- 34.Young S, Wheeler AC, McCoy SI, Weiser SD. A review of the role of food insecurity in adherence to care and treatment among adult and pediatric populations living with HIV and AIDS. AIDS Behav. 2014;18(Suppl.5):505–515. doi: 10.1007/s10461-013-0547-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kushel M, Gupta R, Gee L, Haas J. Housing instability and food insecurity as barriers to health care among low-income Americans. J Gen Intern Med. 2012;21(1):71–77. doi: 10.1111/j.1525-1497.2005.00278.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.World Bank. World Development Report: Infrastructure for Development. New York: Oxford University Press; 1994. [Google Scholar]
- 37.Arba Minch Zuria Woreda Health Office. Annual Report of the Year 2013/2014. Arba Minch, Ethiopia; 2014. [Google Scholar]
- 38.Andarge E, Nigussie A, Wondafrash M. Factors associated with birth preparedness and complication readiness in Southern Ethiopia: a community based cross-sectional study. BMC Pregnancy Childbirth. 2017;17:412. doi: 10.1186/s12884-017-1582-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Coates J, Swindale A, Bilinsky P Household food insecurity access scale (HFIAS) for measurement of food access: indicator guide questionnaire by food and nutrition technical assistance (FANTA) III: USAID; 2007:3.
- 40.Zoran Bursac C, Heath Gauss D, Williams K, Hosmer D. A purposeful selection of variables macro for logistic regression. SAS global forum. Statistics and data analysis. Source Code Biol Med. 2008;3:17. doi: 10.1186/1751-0473-3-17 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Dairo MD, Owoyokun KE. Factors affecting the utilization of antenatal care services in Ibadan, Nigeria. Benin J Postgrad Med. 2010;12(1). [Google Scholar]
- 42.Gupta S, Yamada G, Mpembeni R, et al. Factors associated with four or more antenatal care visits and its decline among pregnant women in Tanzania between 1999 and 2010. PLoS One. 2014;9(7):e101893. doi: 10.1371/journal.pone.0101893 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Joshua CP, KRobert O, Derek TA. Male involvement in maternal health care at Anomabo,Central Region, Ghana. Int J Reprod Med. 2017. doi: 10.1155/2017/2929013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Singh D, Lample M, Earnes J. The involvement of men in maternal health care: cross-sectional, pilot case studies from Maligita and Kibibi, Uganda. Reprod Health. 2014;11:68. doi: 10.1186/1742-4755-11-68 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Mekonnen Y, Mekonnen A. Utilization of Maternal Health Care Services in Ethiopia. Calverton, Maryland, USA: ORC Macro; 2002. [Google Scholar]
- 46.Federal Democratic Republic of Ethiopia, Ministry of Health. Policy and practice information for action. Q Health Bull. 2014;6(1). [Google Scholar]
- 47.Pambè MW, Gnoumou B, Kaboré I. Relationship between women’s socioeconomic status and empowerment in Burkina Faso: a focus on participation in decision-making and experience of domestic violence. Afr PopulStud. 2014;28(2):1146. doi: 10.11564/28-0-563 [DOI] [Google Scholar]
- 48.Samari G, Anne PR. Individual and Household Determinants of Women’s Autonomy: Recent Evidence from Egypt. Los Angeles: California center for population research, university of California; PWP-CCPR-2015-004; 2015. [Google Scholar]
- 49.Yohannes WD, Mesganaw AF, Michelle HJ. Unintended pregnancies and the use of maternal health services in southwestern Ethiopia. BMC Int Health Hum Rights. 2013;13(36). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.USAID. Cultural Barriers to Seeking Maternal Health Care in Ethiopia: A Review of the Literature. Maternal and Child Health Integrated Programme (MCHIP); 2012