Abstract
Objective
To identify the commonalities and discrepancies between national health policies to combat stroke in France and Brazil.
Justification
Both healthcare systems were structured as universal access and comprehensive care attention, hierarchized by the level of care, politically and administratively decentralized. France is an industrialized, high-income country, with health care involving copayment and reimbursement of expenses, and spontaneous demand for services. Brazil is a member of the BRICs, of upper middle income with totally free health care, with an active search for hypertension and diabetes in the general population.
Methods
Data regarding policies, risk factors, and health indicators about stroke care, from 2010 to 2017, were obtained from both countries (publicly accessible information or on request) from the respective Ministries of Health or international agencies.
Results
About acute stroke hospitalizations, on average, Brazil has 0.75 per 1000 annual population hospitalizations versus 1.54 per 1000 in France. Brazil has 0.21 per 1000 population deaths per year versus 0.40 per 1000 in France. The in-hospital mortality rate in Brazil has 139 per 1000 hospitalized people versus 263 in France. The average length of stay of acute hospitalizations was 7.6 days in Brazil versus 12.6 in France. The prevalence of strokes by age group shows from 0 to 39 years old (this rate is stable); 40–59 years (it is increasing in both countries); and 60–79 and 80+ years (this rate has been increasing in France and decreasing in Brazil).
Conclusion
No major differences were found about the health policies and the National Health Plans related to stroke. However, the data directly linked to the period of hospitalization differed substantially between countries. Subsequent studies can be implemented to identify the explanatory factors, notably among the risk factors and actions in primary care, and the moments after hospital care, such as secondary prevention and palliative care.
Keywords: stroke, risk factors, health policies, health care, Brazil, France
Introduction
Stroke is a non-communicable disease that results from an interruption of blood circulation in the brain, usually when a blood vessel ruptures, or a clot blocks it. The most common symptoms of a stroke are a sudden weakness or a loss of sensation in the face or limb, most often on one side of the body. A stroke’s consequences depend on the part of the brain affected and the delay in care.1 In Brazil, stroke is the leading cause of death – 40,019 deaths and 149,333 acute hospitalizations in the Unified Health System (SUS) in 2016.2 In France, stroke is the second leading cause of death; approximately 30,000 people die each year, about 110,000 people are hospitalized each year.3
According to WHO, the Global Noncommunicable Diseases Action Plan to the period 2013–2020 expected a 25% reduction in premature mortality and reduced the risk factors associated with stroke and other NCDs:
laws, policies, and regulations have important roles in the prevention and control of diseases. Only governments can legislate for health warnings, introduce mandatory standards and labeling and health policies. Often governments are the main providers of health care – prevention, treatment, research, and training.4
This paper’s goal was to compare the commonalities and discrepancies of the health policies in the process of stroke control and management, and some endpoint health indicators in France and Brazil, to better inform the policymaking in each country.
Methods
The method proposed was a comparison between Brazil and France about stroke care by collecting secondary data (already existing in the national databases or on request). The health policies concerning stroke care developed in both countries (care and prevention) and the health indicators related to care to better management were studied to achieve the objective. The populations under analysis comprise the entire population of metropolitan France and Brazil. The period analyzed was 2010 to 2017.
The data for the National healthcare policies from Brazil and France were searched in the Ministry of Health websites (National Health legislation – Circulaire DGOS/R4/R3/PF3 n°2012-106; Loi n°2004-806 du 9 août 2004 (France)); Portarias nº664 and 665/2012 (Brazil). From a careful reading, the main points related to stroke care were described in Table 1. It was sought to extract from only the text related to general stroke care, be it prehospital, hospitalization, and after discharge. The stroke care for certain more specific cases was not considered in this study because it is the exception, and because they were varied, what could change the focus of the subject. Those guidelines must be respected in both countries.
Table 1.
Health National Actions Plans – Brazil and France
| Country | Health Policies and Laws | Objective | Specific Objectives |
|---|---|---|---|
| Brazil | Cerebral Vascular Accident (CVA) Care Line in the Urgency and Emergency care network | Reduce stroke morbidity and mortality, through the Stroke Care Line in the Urgency and Emergency Care Network through the comprehensive care | - Disseminate the knowledge that stroke is a medical emergency; - Improve the population’s knowledge about stroke, its signs and symptoms, risk factors, and the need for adequate control of them; - Increase the control of risk factors for vascular diseases in primary healthcare network; - Qualify SAMU 192 for proper stroke care; - Enable Type I, Type II, and Type III Stroke Urgent Care Units, to perform general care and thrombolytic therapy; - Expand the supply of hospital beds for chronic care and rehabilitation; - Establish an adequate outpatient clinic care after hospital discharge - rehabilitation, specialized care, home care, and social and work reintegration of individuals |
| France | Action National Plan - Stroke 2010–2014 | Develop prevention and information to prevent strokes and limit their sequelae; Improve the organization of stroke care; Improve the offer of re-education, rehabilitation, and reintegration; Implement a research policy in the stroke field; Develop ethical thinking; Facilitate the accompaniment of patients and the action of patient associations; Contribute to changing the social outlook on disability. | - Take care of patient victim or suspect of stroke in an organized and territorially defined sector; - Reduce the time between the first symptoms and care, based on a positive diagnosis; - Increase the rate of thrombolysis in eligible patients; - Better coordinate the intervention of professionals at the interfaces between healthcare establishments and city, home, or medical-social sector; - Define a specific organization for the management of children’s stroke; - Improve professional practices; - Improve information and training for professionals and carers people; - Increase research efforts on stroke due to its social burden; |
| Brazil | Ordinance No. 664, April 12, 2012 | Approves the Clinical Protocol and Therapeutic Guidelines - Thrombolysis in Acute Ischemic Stroke | - The general concept of Acute Ischemic Stroke, diagnostic criteria, inclusion and exclusion criteria, treatment and regulation, control, and evaluation mechanisms. This protocol must be used by the Health Departments of the States, Federal District, and Municipalities. - Compliance with the Clinical Protocol and Therapeutic Guidelines - Thrombolysis in Acute Ischemic Stroke is mandatory in eligible patients. - It is mandatory to inform the patient or his legal guardian about the potential risks and side effects related to the use of recommended medication for the treatment of acute ischemic stroke; - State, district, and municipal managers of the Unified Health System (SUS) should structure the healthcare network, define referential services and establish flows for the care of patients described in the Annex to this Ordinance |
| Brazil | Ordinance No. 665, April 12, 2012 | Provides the criteria for the qualification of hospital establishments such as the Urgent Care Center for Patients with Stroke, institutes the respective financial incentive, and approves the Stroke Care Line. | - The Stroke Care Line is approved, to be observed by all health services enabled, - The Urgent Care Centers for stroke patients are part of the Stroke Care Line and are components of the Urgency and Emergency Care Network (RUE). - Treatment stroke patients, Urgent Care Centers, will be classified as Type I, Type II, or Type III. |
| France | Circular N ° DHOS/SDO/01/DGS/SD5D/DGAS/PHAN/3B/200 4/280; June 18, 2004 | Establishes the organizational principles of health care, medical-social and social, traumatic brain, and spinal cord injuries. Emphasizes these injuries’ characteristics and the need to provide speed, fluidity, relevance, and durability in their care also, physically, mentally, and socially. Recommends an organization in a network of experienced and identified actors for the reception, listening, information, and support for relatives of traumatized people. | - Give to the Regional Hospitalization Agencies (ARH), to regional directorates of health and social affairs (DRASS), to the departmental directorates of health business and social services (DDASS), and the organization of the care sector for traumatic brain injury and spinal cord injury which is a basis for the development of Regional Health Organization Schemes, in close collaboration with medical-social actors. - Specifies in its appendices the care of all traumatized craniocerebral types and spinal cord injury. |
| France | Circular DGOS/R4/R3/PF3 n 2012–106. March 6, 2012 | Relating to the organization of supply chains services for patients suffering from cerebrovascular accident (stroke) | Presents the guide intended to provide methodological support to ARS in the organization of care for stroke victims. The purpose is to present the three major objectives of the plan: structuring the sectors, ensuring individualized and optimal care for all stroke victims, and developing telemedicine and information systems. It is supplemented by a methodological guide to help the regions in the implementation of these objectives. |
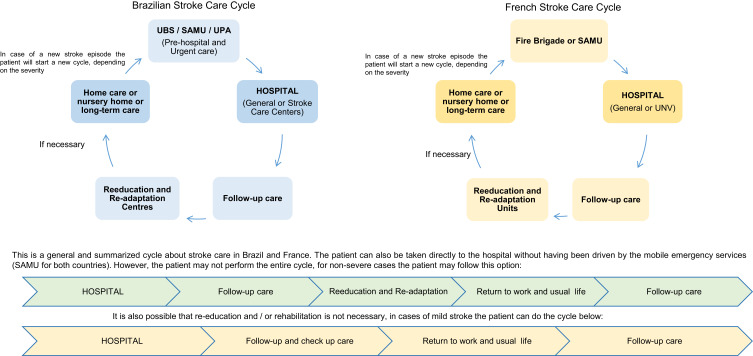
The figures were composed of information from both national health plans for stroke care in both countries, and the general steps to be followed for the stroke care were shown.
About the healthcare indicators, the following were chosen: number of acute hospitalizations, average length of stay, and in-hospital mortality rate, the reason for this choice were due to these data were available for both countries and are part of the effectiveness indicators related to the management. Data about stroke’s prevalence by age group (total cases in a year) were collected from the Hospitalization System of the Unified Health System, obtained in monthly files, according to the principal diagnosis of the discharge note. These files were consolidated in annual periods. For France, data were obtained by request to the Programme de Médicalisation des Systèmes d’Information PMSI.
The data for the acute hospitalizations and the hospital mortality rate per 1000 inhabitants, the following formulas were applied:
 |
and;
 |
and;
 |
For healthcare prevention, the data about risk factors indicators were collected from the WHO website.
The data referring to the estimated population were collected from the United Nations website. The lack of adjustment of differences in the case-mix and the absence of comparable indicators on post-stroke functional disability can be pointed out.
Results
Stroke Policies and Guidelines
In 2011, Brazil published the Strategic Action Plan for Fight Against Chronic Noncommunicable Diseases in Brazil 2011–2022, which aims to promote the development and implementation of effective, integrated, sustainable, and evidence-based public policies for the prevention and control of NCDs and their risk factors.5,6,26 The Plan addresses four key modifiable risk factors: tobacco use, unhealthy diet, physical inactivity, harmful use of alcohol, which generate a significant portion of the burden of NCDs in Brazil. The National Plan has three pillars: health surveillance, monitoring, and evaluation; health prevention and promotion; and comprehensive care.7 Exclusive for stroke there is the Cerebral vascular accident (CVA) care line in the emergency care network.8 In Brazil, Ordinance nº664/2012 approves the Clinical Protocols and Therapeutic Guidelines for Stroke – thrombolysis in acute ischemic stroke and, the Ordinance nº665/2012 provides the criteria for qualifying hospital establishments as an Emergency Care Center for stroke patients in the Unified Health System (SUS). The compliance with this Clinical Protocol is mandatory.9,10
In France, the 2010–2014 National Stroke Action Plan was developed to the stroke prevention and care strategy. Its objectives are a program of operational and regional actions on a National and Regional scale and a toolbox including methods (regulations, good practice standards, guidelines). This Plan is centered on four main axes – improving the health prevention and public information before, during, and after the stroke; enforcing the healthcare channels and adapting information systems, providing information, training for professionals, promoting research, and ensuring demographic balances.11,12,25 The law n°2004-806 Public Health Policy (August 9, 2004) sets five objectives relating to cardiovascular diseases, including one specific to stroke – reducing the frequency and severity of the functional sequelae associated and; the Circular of March 6/2012 organizes the regional networks and standard care for stroke patients from the emergency wards to the medico-social relay and the patient return to home.13,14
The national clinical and therapeutic protocols were established by the Ministry of Health from both countries and were implemented by law or by ministerial ordinance. Table 1 summarizes the main items of the Health Action Plans of both countries, and it seeks to emphasize the points believed to strengthen health prevention, promotion, and recovery.25,26
Stroke Care in Brazil
In Brazil, the Stroke Care Line aims to provide integrated and continuous care within a hierarchical and regulated system and has the following components shown in Figure 18 The stroke prevention and promotion are made by Primary care through the Basic Health Units (UBS) facilities (pediatrics, gynecology, general practice, nursing, and dentistry). To promotion, prevention, and treatment-related to women’s and children’s health, mental health, family planning, cancer prevention, prenatal care, vaccines, laboratory tests, essential medication, and care for chronic diseases such as obesity, diabetes, and hypertension (follow-up care) that covers diagnosis, treatment, rehabilitation, harm reduction, in comprehensive care that positively impacts the population’s health at all health prevention levels – primary, secondary, tertiary, and quaternary.15–17
Figure 1.
Stroke Flow in a Comprehensive Health Care in Brazil.
In the case emergencies, such as strokes, the patient might be referred to a 24-hour Emergency Care Unit (UPA 24h) as a prehospital care, that includes ambulances and emergency mobile care service (SAMU), which transport the patient to a reference center or hospital as soon as possible, prioritizing potential patients for thrombolytic therapy. Telemedicine is expanding to qualified specialized assistance access, regardless of the physical distance. Thrombolytic therapy supported by telemedicine has successful experiences in Brazil, and it is a support for the diagnosis and treatment of acute stroke.8,9 In the acute stroke event, the team often performs the first care, evaluates vital signs and blood glucose, does a brief neurological examination, and contacts the referral’s central urgency regulation.8,17
The treatment is carried out in hospitals and specialized hospitals called Emergency Stroke Care Centers for Patients. These centers are classified as Type I; Type II or Type III with a qualified staff, coordinated by a clinical neurologist and the following resources should be available 24h/7d: continuous cardiovascular and respiratory monitoring; Intensive Care Unit; Clinical pathology laboratory; CT scanner; Neurosurgical; hemotherapy service or transfusion agency, including cryoprecipitate. The number of Emergency Stroke Care Centers increased from 35 (2008) to 149 in 2017.7,9,10
After the stroke care, the treatment should be prescribed by a specialist, and the patient returns to primary attention to regular visits at the general practitioner and specialists. Secondary prevention is done through the control of hypertension, diabetes, and lipids, and anticoagulation therapy may be indicated for some and the control and treatment for platelet anti-aggregation, atrial fibrillation, cardiomyopathy, and other more specific procedures, depending on each case.16,18
The rehabilitation is carried out in the Specialized Rehabilitation Centers (CERS) for diagnoses and treatments and have the following care: physiotherapy, speech therapy, ergotherapy, psychomotricity, neuropsychology, psychology, and physicians considering the impact of the disability on their functionality, as well as the clinical, emotional, environmental and social factors involved that provide a better quality of life.18
The long-term care and end-of-life care are done, in large part, at the patient’s residence, through a caregiver who can be a family member or a health professional according to the severity and complexity of the disability. The Palliative Care program includes different levels of patient care: home care, outpatient care, procedures in bed-day. In both cases, depending on the patient’s health status, he/she goes to control consultations at a UBS, or a team of health professionals goes to his/her home for medical monitoring. If the patient cannot return home due to insufficient autonomy or a disadvantaged social, it is usual to be housed in nursing homes. Usually, the patient is carried to the hospital for the end-of-life last care.19
Stroke Care in France
In France, the Stroke Care Line has the following components shown in Figure 2.12 The treatment of stroke is carried out in acute care hospitals (either public or private for-profit or private not for profit) and in more specialized services called Neuro-Vascular Units (UNV). These units are reference centers that are labeled by the Ministry of Health. The number of Neurovascular Units increased from 33 in 2007 to 135 in 2014,20 and the care is offered by medical and paramedical staff.12,21,22
Figure 2.
Stroke Flow in a Comprehensive Health Care in France.
The Care organization is based on coordination between the UNV and the various emergency services: SAMU, fire brigade, emergency reception, radiologists, neurologists, cardiologists, neurosurgery teams, resuscitators, Etc.12,23,24 Telemedicine is an emergency service that aims to benefit patients with treatment in a shorter period until they arrive at the emergency ward or the UNV.11
After the care, the patient undergoes an evaluation to start his/her personalized program for health recovery and day-to-day activities, and secondary prevention is done by preventing cardiovascular risk factors controlling blood pressure and blood sugar. These measures include taking anti-thrombotic treatment, statins, applying hygienic and dietary rules (stopping smoking, maintaining physical activity, controlling alcohol consumption), regular visits at the cardiologist, and general practitioner.12,23
The rehabilitation is carried out in the Reeducation and Re-adaptation Units, which are neurological or geriatric, and have the following care: physiotherapy, speech therapy, ergotherapy, psychomotricity, neuropsychology, psychology, and physicians.12
The long-term care and end-of-life care are done at the patient’s residence, or home equivalent (home hospitalization – HAD) or in an institution, according to the severity and complexity of the disability. Also, in accommodation establishment for dependent elderly (EHPAD), specialized reception homes (MAS), nursing homes. If the patient cannot return home due to insufficient autonomy or a disadvantaged social, he/she can be referred to the healthcare structures. According to the needs they express, palliative care is based on support for the person and those around them to help them as best as possible. Hospital professionals, referring general practitioners, family, and relatives of the patient, participate in the patient’s overall care.12
Results
Healthcare Indicators
Table 2 shows a comparison of the risk factor indicators tracked by WHO, they are essential for stroke control. Both countries are similar regarding salt consumption, diabetes, and obesity. France has higher alcohol consumption, tobacco smoking, and hypertensive adults. Brazil has a higher percentage of people who do not do physical activity.1,4,33,34
Table 2.
Risk Factors Indicators Related to Stroke in Brazil and France, 2010 and 2016
| Risk Factors | 2010 | 2016 | ||
|---|---|---|---|---|
| Brazil | France | Brazil | France | |
| Total alcohol per capita consumption, adults aged 15+ (liters of pure alcohol) (world average is 6.4 liters) | 8.7 | 12.2 | 8 | 13 |
| Physical inactivity - adults aged 18+ (%) (recommended 150 minutes of moderate-intensity physical activity per week) | 48.6 | 33 | 47 | 32 |
| Salt/Sodium intake - (g/day) (recommendation - 5 g/day salt or 2g/day sodium) | x | x | 10g | 10g |
| Tobacco use - Current tobacco smoking, adults aged 15+ (%) (worldwide prevalence 20%) | 14.1 | 23.6 | 14 | 28 |
| Raised blood pressure - adults aged 18+ (%) | 40.0 | 42.7 | 23 | 29 |
| Diabetes - adults aged 18+ (%) | 9.7 | 6.8 | 8 | 8 |
| Obesity - adolescents aged 10–19 (%) | x | x | 9 | 7 |
| Obesity - adults aged 18+ (%) | 18.8 | 18.2 | 22 | 23 |
Table 3 shows the result of a historic series between the years 2010 to 2016 about Acute Stroke Hospitalizations, Average stay, and In-hospital mortality rate from Brazil and France. About Acute Stroke Hospitalizations, on average, Brazil has 0.75 per 1000 annual population hospitalizations versus 1.54 per 1000 in France. In-hospital mortality rate, Brazil has an average of 139 per 1000 hospitalized people versus 263 in France. The average length of stay of acute hospitalizations was about 7.6 days in Brazil versus 12.6 in France.
Table 3.
Acute Stroke Hospitalizations, Average Stay, Hospital Deaths and Hospital Mortality Rate from Brazil and France, 2010–2017
| Year | Acute Hospitalizations (Total Amount = Prevalence) | Average Stay (Days) | Hospital Deaths | Acute Hospitalizations Rate per 1.000 Inhabitants | Hospital Mortality Rate of 1.000 Inhabitants | Estimated Population (in Thousands) |
||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Brazil | France | Brazil | France | Brazil | France | Brazil | France | Brazil | France | Brazil | France | |
| 2010 | 116,633 | 101,982 | 7,5 | 12,74 | 20,018 | 28,559 | 0.59 | 1.62 | 0.102 | 0.454 | 195,714 | 62,880 |
| 2011 | 124,143 | 101,359 | 7,5 | 16,36 | 20,944 | 28,529 | 0.62 | 1.60 | 0.106 | 0.451 | 197,515 | 63,222 |
| 2012 | 127,512 | 105,269 | 7,6 | 10,71 | 21,082 | 28,141 | 0.63 | 1.65 | 0.105 | 0.442 | 199,287 | 63,564 |
| 2013 | 133,930 | 108,514 | 7,6 | 11,34 | 21,406 | 28,495 | 0.66 | 1.69 | 0.106 | 0.445 | 201,036 | 63,894 |
| 2014 | 142,403 | 110,439 | 7,7 | 13,35 | 22,134 | 28,550 | 0.70 | 1.72 | 0.109 | 0.444 | 202,764 | 64,194 |
| 2015 | 145,276 | 112,188 | 7,7 | 13,34 | 23,388 | 28,391 | 0.71 | 1.74 | 0.114 | 0.440 | 204,472 | 64,453 |
| 2016 | 149,333 | 115,460 | 7,7 | 10,63 | 24,154 | 28,301 | 0.72 | 1.78 | 0.117 | 0.437 | 206,163 | 64,668 |
| Total | 1,095,721 | 755,211 | – | – | 153,126 | 198,966 | – | – | – | – | – | – |
Table 4 shows the Stroke prevalence by age group in Brazil and France, 2010–2016. The prevalence of strokes by age group (Table 3) shows that this rate has remained practically stable from 0 to 39 years old, even with population growth. This rate for the age group 40–59 years has been increasing in both countries, and the age groups 60–79 and 80+ years, the rate has been increasing in France and decreasing in Brazil.
Table 4.
Stroke’s Prevalence by Age Group in Brazil and France, 2010–2016 (Total Cases in a Year and Prevalence per 10.000 Inhabitants, by Age Group)
| Year | Prevalence (Number of Cases) |
Prevalence per 10,000 Inhab. | Prevalence (Number of Cases) |
Prevalence per 10,000 Inhab. | Prevalence (Number of Cases) |
Prevalence per 10,000 Inhab. | Prevalence (Number of Cases) |
Prevalence per 10,000 Inhab. | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 0–39 Years Old | 40–59 Years Old | 60–79 Years Old | 80+ Years Old | |||||||||||||
| BR | FR | BR | FR | BR | FR | BR | FR | BR | FR | BR | FR | BR | FR | BR | FR | |
| 2010 | 6578 | 4919 | 0.05 | 0.15 | 35.147 | 19.522 | 0.78 | 1.14 | 75,184 | 46,658 | 6.07 | 4.18 | 34,337 | 48,495 | 13,89 | 14,44 |
| 2011 | 6801 | 4550 | 0.05 | 0.14 | 37.148 | 18.906 | 0.81 | 1.11 | 78,977 | 45,634 | 6.15 | 4.01 | 35,913 | 49,490 | 13,67 | 14,26 |
| 2012 | 7183 | 4798 | 0.05 | 0.15 | 37.706 | 19.855 | 0.79 | 1.16 | 79,877 | 47,450 | 6.00 | 4.10 | 36,731 | 51,848 | 13,28 | 14,51 |
| 2013 | 7357 | 4804 | 0.05 | 0.15 | 38.747 | 20.564 | 0.81 | 1.19 | 83,545 | 49,502 | 6.04 | 4.18 | 38,147 | 53,350 | 13,18 | 14,54 |
| 2014 | 7722 | 4676 | 0.05 | 0.14 | 40.665 | 20.872 | 0.84 | 1.21 | 87,870 | 50,723 | 6.11 | 4.20 | 39,198 | 54,492 | 12,96 | 14,51 |
| 2015 | 7752 | 4478 | 0.05 | 0.14 | 40.775 | 21.035 | 0.82 | 1.22 | 89,710 | 52,440 | 5.97 | 4.26 | 40,194 | 55,943 | 12,71 | 14,62 |
| 2016 | 7989 | 4778 | 0.06 | 0.15 | 41.697 | 21.926 | 0.83 | 1.27 | 92,391 | 55,983 | 5.91 | 4.47 | 41,386 | 59,154 | 12,25 | 15,16 |
Stroke Care Comparation
The care offered in the event of a stroke is not very different from one country to another, as illustrated in Figure 3. This care is since both countries follow the guidelines outlined by WHO, which reflect standardized care and have consolidated national health policies in stroke care.
Figure 3.
Stroke Care in Comparation.
Discussion
This research is essential because several countries have programs for evaluating their healthcare systems based on data and indicators to know the quality of hospital and primary care, the whole system’s performance or to evaluate specific parts, allocate resources, compare results, and promote policies. In Brazil, there is an effort to evaluate its healthcare system through indicators. The OECD evaluates the economic policies of its member countries intending to compare healthcare systems. Although Brazil is not a member, the OECD seeks to include it in calculating some indicators as it considers Brazil as one of the largest economies, and there is a good representation of indicators calculated for Brazil. Thus, Brazil has its healthcare system compared to other countries, pointing out areas that can be improved and its good results.35 This research is characterized as unprecedented and innovative because that compares the National health policies and the stroke care in two universal healthcare systems, and it had not been done before.
Laws and policies guide every public healthcare system, so the core policies developed follow the WHO recommendations based on each country’s experiences and health characteristics. The law refers to reducing the functional sequelae’s frequency and severity and organizing the networks and standard care. In both ministries of health websites, there is information about stroke – how it occurs, signs and symptoms, risk factors, prevention, and how to call for help, emphasizing the importance of the care as soon as possible to avoid sequels and premature death. There are no significant differences between policies and laws related to stroke prevention and treatment in both countries, but the health strategies are different.25,26
Concerning the indicators related to stroke care, a hypothesis for lower rates in Brazil, as a lower prevalence (Table 4) and Acute Stroke Hospitalizations (Table 3), could be associated with the intense work of UBSs, which mitigates risk factors.36 These services are also provided “on the move” in their territory in an attitude of “active search” in an asymptomatic population beyond spontaneous demand.37–40
Regarding the average length of stay due stroke, Brazil has 7.6 days, and France has 12.63 days. The French hospital length of stay average is about 61% higher than Brazilian. In Brazil, the stroke centers’ treatment was associated with a reduction of 2 to 10 days of hospitalization due to work carried out by the multidisciplinary team specialized within an average period of 7 days.41 Usually, the reasons for a longer ALS (average length of stay) are different in case mix, age, access to the healthcare system, and duration to the transfer to the rehabilitation structures. The age structure partly explains this difference: in Brazil, a stroke occurs at most in the age group between 60 and 79 years (5.91/10000 in Brazil against 4.47/10,000 in France) and, in France, the age group is people over 80 years old (15.16/10,000 in France against 12.25/10,000 in Brazil).
The in-hospital mortality due to stroke, Brazil, has an average of 1.08 per 10,000 inhabitants, and France has 4.44. Although patients stay longer in hospitals in France, the Brazilian in-hospital mortality rate is lower, and a hypothesis to explain this fact could be due to health prevention in the Brazilian primary care that improves the population’s health. Another hypothesis is even social inequalities in France are lower than in Brazil (Inequality-adjusted HDI is 0.574 in Brazil and France is 0.809 - closest one better the index),42,43 France has a healthcare system universal, but with copayment rates. That could repress the demand for health services.44,45 To alleviate these inequalities, SUS is free of charge, including consultations, medications, transportation, hospitalizations, surgeries.46 According to WHO, Brazil has one of the ten best health programs in the world for its effectiveness in controlling chronic diseases. The policies to reduce tobacco use and curb diet-related diseases like diabetes and hypertension made Brazil a country known for its progressive action to prevent non-communicable diseases.47–49 This effort in Brazil may be partly due to higher risk factors in France – a higher percentage of alcohol consumption, tobacco smoking, and hypertensive adults. The positive influence of SUS primary care has been proven to improve Brazilians’ health and the strengthening of primary health care for reducing inequalities and health-promoting and preventing.50–53
The care offered in the event of a stroke is not very different from one country to another, as illustrated in Figure 3. Both countries follow the guidelines outlined by WHO, reflecting standardized care, and consolidating national health policies in stroke care. Brazil aims the health prevention and control of NCDs in comprehensive care through the modifiable risk factors: tobacco use, unhealthy diet, physical inactivity, harmful use of alcohol. France aims the stroke prevention and care strategy through a program of operational and regional actions seeking to improve health promotion and prevention. Brazil shows promising results in care when compared to France – lower prevalence, acute hospitalization, and in-hospital mortality rates due to stroke. There is no pre-determined flow, as shown Figure 3, SAMU can assist the patient if the event occurs on the street as the patient can be taken directly to a hospital or an Urgent Care Center for Patients with Stroke. In France, the most common way is to call the fire brigade or SAMU, which will transport the patient to the emergency department of the nearest hospital or a UNV if there is one nearby. In both countries, it depends on the patient’s location and who will call for help. The care after stroke hospitalization is very similar for both countries. As an emerging country, Brazil shows promising results from its care in stroke and is comparable to the care in France. This research is essential to know if the Brazilian healthcare system is on the right track.
Conclusion and Implications
No significant differences were found about the health policies and the National Health Plans related to stroke. However, the data directly linked to the period of hospitalization differed substantially between countries. Subsequent studies can be implemented to identify the explanatory factors, notably among the risk factors and actions in primary care, and the moments after hospital care, such as secondary prevention and palliative care. This research can collaborate to improve the healthcare systems and health policies of both countries in stroke care.
Funding Statement
This research did not receive any funding from agencies in the public, commercial, or not-for-profit sectors.
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.World Health Organization WHO. World Health Statistics. Geneva; 2018. Available from https://apps.who.int/iris/bitstream/handle/10665/272596/9789241565585-eng.pdf?ua=1. Accessed October 2019. [Google Scholar]
- 2.Brasil e Mais Onze Países Assinam Documento Para Prevenção e Enfretamento Do AVC. Brasil: Ministério da Saúde; 2018. Available from: http://www.saude.gov.br/noticias/agencia-saude/43985-ministerio-da-saude-e-signatario-da-carta-de-gramado-para-prevencao-e-enfrentamento-do-avcministerio-da-saude-e-signatario-da-carta-de-gramado-para-prevencao-e-enfrentamento-do-avc. Accessed October 2019. [Google Scholar]
- 3.FRAVC – Fondation pour la recherche sur les AVC. Fréquence. 2020? Available from: http://www.fondation-recherche-avc.org/fr%C3%A9quence. Accessed October 2019.
- 4.World Health Organization WHO. WHA66/2013/REC/1. Sixty-Sixth World Health Assembly: Resolutions and Decisions, Annexes. Annex 4 - Global Action Plan for the Prevention and Control of Noncommunicable Diseases 2013–2020. 2013. Geneva: Available from: http://apps.who.int/gb/ebwha/pdf_files/WHA66-REC1/A66_REC1-en.pdf?ua=1&ua=.1. Accessed October 2019. [Google Scholar]
- 5.Bensenor IM, Goulart AC, Szwarcwald CL, et al. Prevalence of stroke and associated disability in Brazil: national Health Survey – 2013. Arquivo Neuro Psiquiatria. 2015;73(9):746–750. doi: 10.1590/0004-282X20150115 [DOI] [PubMed] [Google Scholar]
- 6.Silva JB Update on the Action Plan to Tackle Noncommunicable Diseases in Brazil. Presentation. Report on the 3rd forum on the strategic action plan to tackle Noncommunicable diseases in Brazil. 2013 – 2018 Brasilia:Ministry of Health of Brazil; Available from: http://portalms.saude.gov.br/images/pdf/2018/junho/19/INGLES-REPORT-3RD-FORUM-DCNT-19jun18-cs-ISBN-web.pdf. Accessed October 2019. [Google Scholar]
- 7.Silva GS, Rocha ECA, Pontes-Neto OM, Martins SO. Stroke care services in Brazil. J Stroke Med. 2018;V1(1):51–54. doi: 10.1177/2516608518776162 [DOI] [Google Scholar]
- 8.CONITEC. Comissão Nacional de Incorporação de Tecnologias no Sistema Único de Saúde. Protocolos e Diretrizes. Linha de cuidados em Acidente Vascular Cerebral (AVC) na rede de atenção às urgências e emergências; 2020. Available from http://conitec.gov.br/protocolos-e-diretrizes. Accessed October 2019. [Google Scholar]
- 9.Brazil. Portaria nº 664, de 12 de abril de 2012. Aprova o protocolo clínico e diretrizes terapêuticas - trombólise no acidente vascular cerebral isquêmico agudo. Brasilia. 2012a. Available from: http://bvsms.saude.gov.br/bvs/saudelegis/gm/2012/PRT0664_12_04_2012.html. Accessed October 2019.
- 10.Brazil. Portaria nº. 665, de 12 de abril de 2012. Dispõe sobre os critérios de habilitação dos estabelecimentos hospitalares como Centro de Atendimento de Urgência aos Pacientes com Acidente Vascular Cerebral (AVC), no âmbito do Sistema Único de Saúde (SUS), institui o respectivo incentivo financeiro e aprova a Linha de Cuidados em AVC. Brasilia. 2012b. Available from: http://bvsms.saude.gov.br/bvs/saudelegis/gm/2012/PRT0665_12_04_2012.html. Accessed October 2019.
- 11.Ministère de la Santé et des Sports, Ministère du Travail, de la Solidarité et de la Fonction Publique, Ministère de L’enseignement Supérieur et de la Recherche. Plan d’actions national accidents vasculaires cérébraux 2010–2014. France: 2010. Available from: https://www.cnsa.fr/documentation/plan_actions_avc_-_17avr2010.pdf. Accessed October 2019. [Google Scholar]
- 12.Broussy-Boudeau S. Parcours Post-AVC, mesure des séquelles Post-AVC et lien entre parcours et séquelles à un an: enjeux conceptuels et méthodologiques résultats d’une cohorte rétrospective perspectives de recherche. Thèse de Doctorat De L’Université de Bordeaux. Ecole Doctorale de Sante Publique et Science Politique. Discipline: Epidémiologie. 2019. Available from:: http://www.theses.fr/2019BORD0414. Accessed January 2020.
- 13.Circulaire DGOS/R4/R3/PF3 n°2012-106 du 6 mars 2012 relative à l’organisation des filières régionales de la prise en charge des patients victimes d’accident vasculaire cérébral AVC. BO Sante, protection sociale, solidarité n°2012/4 du 15 mai 2012. Available from: https://solidarites-.gouv.fr/fichiers/bo/2012/12-04/ste_20120004_0100_0081.pdf. Accessed January 2020.
- 14.Loi n°2004–806 du 9 aout 2004 relative à la politique de sante publique (version consolide du 8 décembre 2011) JO. 2004. Available from: https://www.legifrance.gouv.fr/affichTexte.do?cidTexte=JORFTEXT000000787078&categorieLien=id. Accessed January 2020.
- 15.Sobre a Vigilância de DCNT. Brazil: Ministry of Health; 2019. Available from: http://www.saude.gov.br/noticias/43036-sobre-a-vigilancia-de-dcnt. Accessed January 2020. [Google Scholar]
- 16.Nugem RC, Bordin R, Schott-Pethelaz AM, Michel P, Piriou V. National Health Systems of Brazil and France: a comparative analysis. World J Advan Healthcare Res. 2019;3:50–61. [Google Scholar]
- 17.Ministry of Health of Brazil. Report on the 3rd forum on the strategic action plan to tackle Noncommunicable diseases in Brazil. 2013 – 2018. Brasilia. 2018. Available from: https://wwwsaude.gov.br/images/pdf/2018/junho/19/INGLES-REPORT-3RD-FORUM-DCNT-19jun18-cs-ISBN-web.pdf. Accessed January 2020.
- 18.Ministry of Health of Brazil. The health of People with Disabilities: guidelines, policies, and actions. 2020. Available from: https://saude.gov.br/saude-de-a-z/saude-da-pessoa-com-deficiencia. Accessed January 2020.
- 19.Borba SRC, Lamy M. Internação a longo prazo de portadores de sequelas neurológicas após acidentes vasculares cerebrais no Rio Grande do Sul: um problema de saúde pública. Long-term admission of neurological sequelae patients after stroke in Rio Grande do Sul: a public health problem. Unisanta Law Soc Sci. 7(3):97–119. [Google Scholar]
- 20.Com-Ruelle L, Nestrigue C, Le Guen N, et al. Parcours de soins des personnes hospitalisées pour un accident vasculaire cerebral. Premiers résultats. Questions d’économie de la santé. N. 234. 2018. Available from: https://www.irdes.fr/recherche/questions-d-economie-de-la-sante/234-parcours-de-soins-des-personnes-hospitalisees-pour-un-accident-vasculaire-cerebral.pdf. Accessed January 2020.
- 21.Ministère de la santé. La prise en charge des AVC. 2019. Available from: https://solidarites-sante.gouv.fr/soins-et-maladies/maladies/maladies-cardiovasculaires/accident-vasculaire-cerebral-avc/article/la-prise-en-charge-des-avc. Accessed January 2020. [Google Scholar]
- 22.Haute Autorité de Santé. Service communication. Accident vasculaire cérébral: prise en charge précoce (alerte, phase préhospitalière, phase hospitalière initiale, indications de la thrombolyse). 2009. Available from: www.has-sante.fr. Accessed January 2020.
- 23.Agence Nationale d’Accréditation et d’Évaluation en Santé (ANAES). Recommandations pour la pratique clinique. Prise en charge initiale des patients adultes atteints d’accident vasculaire cérébral - aspects paramédicaux – argumentaire. 2002a. Available from: https://www.has-sante.fr/jcms/c_451113/fr/avc-aspects-paramedicaux-recommandations. Accessed January 2020.
- 24.Agence Nationale d’Accréditation et d’Évaluation en Santé (ANAES). Prise en charge initiale des patients adultes atteints d’accident vasculaire cérébral - Aspects médicaux - Recommandations. 2002b. Available from: https://www.has-sante.fr/jcms/c_272249/fr/prise-en-charge-initiale-des-patients-adultes-atteints-d-accident-vasculaire-cerebral-aspects-medicaux. Accessed February 2020.
- 25.Ministère de la Sante et des Sports - Ministère du Travail, de la Solidarité et de la Fonction Publique - Ministère de L’enseignement Supérieur et de la Recherche. Plan d’actions national “accidents vasculaires cérébraux” 2010–2014. 2010. Available from: https://www.cnsa.fr/documentation/plan_actions_avc_-_17avr2010.pdf. Accessed February 2020.
- 26.Ministry of Health of Brazil. Strategic action plan to confront Non-communicable Chronic Diseases (NCDs). 2013–2019. Available from: http://www.saude.gov.br/vigilancia-em-saude/vigilancia-de-doencas-cronicas-nao-transmissiveis-dcnt/plano-de-acoes-estrategicas-para-o-enfrentamento-das-doencas-cronicas-nao-transmissiveis-dcnt. Accessed February 2020.
- 27.World Health Organization WHO. Global Report. Noncommunicable diseases country profiles. 2011. Available from: https://www.who.int/nmh/publications/ncd_profiles2011/en/. Accessed February 2020.
- 28.World Health Organization - Noncommunicable Diseases (NCD) Country Profiles. 2018. Available from: https://apps.who.int/iris/handle/10665/274512. Accessed February 2020.
- 29.DATASUS. Produção Hospitalar. 2019. Available from: http://www2.datasus.gov.br/DATASUS/index.php?area=0202. Accessed February 2020.
- 30.ATIH. SCANSANTÉ. MCO par diagnostic ou acte. 2019. Available from: https://www.scansante.fr/applications/statistiques-activite-MCO-par-diagnostique-et-actes?secteur=MCO. Accessed February 2020.
- 31.PMSI. Fédération Hospitalière de France. 2020. Available from: https://www.fhf.fr/gestion-hospitaliere/pmsi.html. Accessed February 2020.
- 32.United Nations. World Population Prospects 2019. Available from: https://population.un.org/wpp/. Accessed February 2020.
- 33.World Health Organization WHO. Global status report on noncommunicable diseases. 2014. Available from: https://www.who.int/nmh/publications/ncd-status-report-2014/en/. Accessed February 2020.
- 34.World Health Organization WHO. Noncommunicable diseases progress monitor 2020. Geneva: 2020. Available from: https://www.who.int/publications-detail-redirect/ncd-progress-monitor-2020. Accessed 1March 2020. [Google Scholar]
- 35.Lima CP Comparando a saúde no Brasil com os países da OCDE: explorando dados de saúde pública. Dissertação (mestrado) - Fundação Getulio Vargas. Escola de Matemática Aplicada. 140 f. 2016. Available from: https://bibliotecadigital.fgv.br/dspace/handle/10438/16503. Accessed March 2020.
- 36.Ministério da Saúde. Estratégia de Saúde da Família. 2013. Available from: https://www.saude.gov.br/acoes-e-programas/saude-da-familia. Accessed March 2020.
- 37.Schnitzler A, Erbault M, Solomiac A, et al. Impact of the stroke plan on the management of acute ischemic stroke in France: trends of assessment indicators of the French national authority for health from 2011 to 2016. BEH. 2018;5:78–84. [Google Scholar]
- 38.Ministério da Saúde. Estratégia de Saúde da Família. 2013Available from: https://www.saude.gov.br/acoes-e-programas/saude-da-familia. Accessed March 2020.
- 39.Lemke RA, Silva RAN The active search as political principle of practices of care in the territory. Estudos e Pesquisas em Psicologia, UERJ; 1, P. 281–295. 2010. Available from: http://www.revispsi.uerj.br/v10n1/artigos/pdf/v10n1a18.pdf. [Google Scholar]
- 40.Mattos RA. Os sentidos da integralidade: algumas reflexões acerca de valores que merecem ser defendidos In: Pinheiro R, Mattos RA, editors. Os Sentidos da integralidade na atenção e no cuidado à Saúde. Rio de Janeiro: UERJ;2001:39–63. Available from: https://www.cepesc.org.br/wp-content/uploads/2013/08/Livro-completo.pdf. Accessed March 2020. [Google Scholar]
- 41.Moura MC, Casulari LA. Impacto da adoção de medidas inespecíficas no tratamento do acidente vascular cerebral isquêmico agudo em idosos: a experiência do Distrito Federal, Brasil. Rev Panam Salud Publica. 2015;38(1):57–63. [PubMed] [Google Scholar]
- 42.Schnitzler A, Erbault M, Solomiac A, et al. Impact of the stroke plan on the management of acute ischemic stroke in France: trends of assessment indicators of the French national authority for health from 2011 to 2016. BEH 5. 78–84. 2018. Available from: http://beh.santepubliquefrance.fr/beh/2018/5/pdf/2018_5.pdf. Accessed March 2020.
- 43.United Nations. Human development reports. Brazil: 2020. Available from: http//hdr.undp.org/en/countries/profiles/BRA. Accessed April 2020. [Google Scholar]
- 44.Human Development Reports. France: United Nations; 2020. Available from: http//hdr.undp.org/en/countries/profiles/FRA. Accessed April 2020. [Google Scholar]
- 45.Bayle-Iniguez A. Un français sur trois renonce à des soins pour des raisons financières. Le Quotidien du Médecin.fr. 2018. Available from: https://www.lequotidiendumedecin.fr/actus-medicales/politique-de-sante/un-francais-sur-trois-renonce-des-soins-pour-des-raisons-financieres. Accessed May 2020.
- 46.Revil H. Le ”non-recours” à la Couverture maladie universelle: émergence d’une catégorie d’action et changement organisationnel. Science politique. Université de Grenoble, 2014. Available from: https://www.theses.fr/2014GRENH033.pdf.
- 47.World Health Organization WHO. Handbook on Health Inequality Monitoring: With a Special Focus on Low- and Middle-Income Countries. Geneva; 2013. Available from: https://www.who.int/docs/default-source/gho-documents/health-equity/handbook-on-health-inequality-monitoring/handbook-on-health-inequality-monitoring.pdf?sfvrsn=d27f8211_2. Accessed April 2020. [Google Scholar]
- 48.Baroni LL. 6 Programas De Saúde Pública No Brasil Considerados Referência No Mundo. São Paulo: UOL; 2018. Available from:: https://noticias.uol.com.br/saude/ultimas-noticias/redacao/2018/06/05/6-programas-de-saude-publica-do-brasil-considerados-referencia-no-mundo.htm. Accessed April 2020. [Google Scholar]
- 49.Henning K. Global health checkup: seven steps to tackle NCDs in Brazil. Bloomberg Philanthropies Public Health. 2018. Available from: https//www.bloomberg.org/blog/global-health-checkup-seven-steps-tackle-ncds-brazil/. Accessed April 2020. [Google Scholar]
- 50.World Health Organization WHO. Tobacco control in Brazil. 2015. Available from: https://www.who.int/tobacco/about/partners/bloomberg/bra/en/. Accessed April 2020.
- 51.Paim JS. Equity and reform in the health services system: the case of the Unified Health System of Brazil. Saude Sociedade. 2006;15(2). [Google Scholar]
- 52.Ministério da Saúde. Painel De Indicadores Do SUS. Temático Saúde Da Família. Vol. 2 Brasília; 2007. [Google Scholar]
- 53.Lopes SMSC. O reflexo das desigualdades sociais no atendimento básico do serviço de saúde do SUS. Âmbito Jurídico. 2016. [Google Scholar]