Abstract
Introduction
The term “digital healthcare professional” alludes to a health professional with the additional digital capabilities such as information and technology. The assumption that attaining technical knowledge and skills to meet the available professional standards in digital healthcare, will engage and empower healthcare users, thus deliver person-centered digital healthcare (PCDHc), is flawed. Identifying where digital healthcare and technologies can genuinely support person-centered care may lead to future discourse and practical suggestions to build person-centered integrated digital healthcare environments. This review examines current digital health and informatics capability frameworks and identifies the opportunity to include additional or alternative principles.
Methods
A scoping review was conducted. Literature valuing person-centered digital healthcare requirements, digital health capabilities, and competencies were identified between 2000 and 2019 inclusive, then collated and considered. Using a PRISMA approach for eligibility screening, thirteen articles met the study inclusion criteria. Analysis used a thematic framework approach, which assisted in the data management, abstraction and description, and finally the explanations.
Results
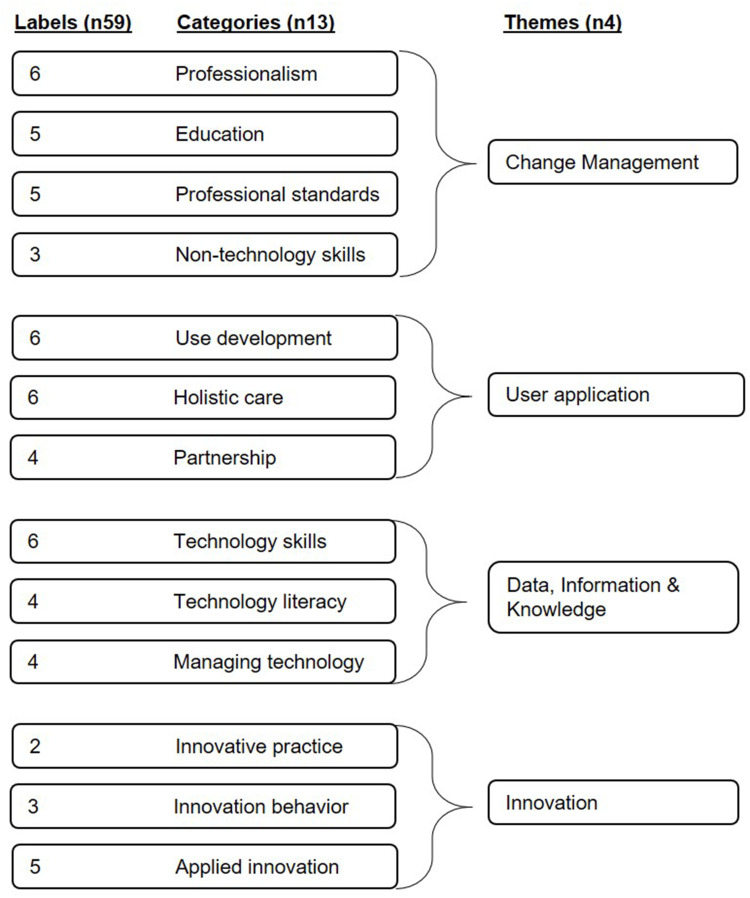
Analysis indexed fifty-nine (59) capabilities, charted thirteen (n13) categories, mapped four (n4) themes, which were then interpreted as findings.
Findings
The four themes identified were Change Management; User Application; Data, Information, and Knowledge; and Innovation. The themes recognize the opportunity to align the application of technical skills towards the capabilities required to deliver authentic PCDHc.
Discussion
Holistic mindsets are imperative in maintaining the objective of PCDHc. The authors propose that debates regarding professional digital capability persist in being “siloed” and “paternalistic” in nature. They also recommend that the transition to authentic PCDHc requires refocusing (rather than rewriting) current capabilities. The realignment of capabilities towards individual healthcare outcomes, rather than professional obligation, can steer the perspective towards a genuine PCDHc system.
Conclusion
This scoping review confirms the assumption that digital skills will empower all healthcare stakeholders is incorrect. This review also draws attention to the need for more research to enable digital healthcare systems and services to be designed to realize complex human behaviors and multiple person-centered care requirements. Now more than ever, it is imperative to align healthcare capabilities with technologies to ensure that the practice of PCDHc is the empowering journey for the healthcare user that theory implies.
Keywords: person-centered, digital healthcare, capability, professional practice
Introduction
The term “digital healthcare professional” alludes to a health professional with the additional digital capabilities in information and technology. The digital healthcare professional in this instance satisfies the role of a healthcare professional currently required to use informatics as part of their daily routine. There is growing consensus however that the expansion of healthcare into digital is humanistic and aligned with person-centered care, rather than merely a growth of technological capability.1,2 The assumption that attaining technical knowledge and skills to meet the available professional standards in digital healthcare, will engage and empower healthcare users (hereafter referred to as individuals) thus deliver person-centered digital healthcare (PCDHc), is flawed. This assumption exposes an oversight of the complexities of healthcare delivery, empowerment, engagement, and ultimately self-efficacy of the individual.3–5
Internationally, the focus is on the need for contemporary healthcare research, to revisit and embrace methods that facilitate genuine participation of all healthcare.1,2 Taking a holistic approach, which regards empowerment, engagement, and self-efficacy as fundamental to healthcare provision, aims to make use of contextual evidence, including the social determinants of health, which support individuals within their broader communities.6
Three decades ago, the underlying ideas behind person-centered care were borne from Bandura’s seminal work on Self-Efficacy4 and Wagner’s attempts to shift away from paternalistic care by introducing the Chronic Care Model (CCM).5 In both bodies of work, a fundamental improvement to healthcare outcomes for the individual was observed and discussed to be a fundamental benefit that should motivate their adoption in healthcare practices. The aspirations of person-centered care continue today in contemporary healthcare with models in which the individual ought to be considered the focal point of care: engaged, enabled, and empowered, actively involved in the decision-making of their healthcare journey.7 This is in contrast to the individual merely being invited to participate or considered equal to the healthcare professional in the management of their healthcare journey.8 However, person-centered care continues to be interpreted to “fit” the needs of the healthcare professional without consideration of these models.9 The continuing discourse regarding person-centered care delivery appears idealistic rather than established practice. This poses a question, has contemporary healthcare moved from traditional professional-centric healthcare towards delivering person-centered practices?
The umbrella term “digital health” incorporates, but is not limited to, technological areas such as eHealth, mHealth, telehealth, wearable devices, and personalized medical devices.10 This emphasis on technology suggests a priority in information technology knowledge and skills rather than personal digital health or care capability.11 Digital health research regarding the development and use of shared decision-making tools, for example, the electronic health record (EHR) or technologies for in-the-home interventions, continue to define the end-user of such systems as the healthcare professional, rather than embracing the role of the individual.12 In digital healthcare, there should be equal opportunities for all individuals of healthcare. In this case, the healthcare professional and the individual receiving the care, to be engaged, enabled, and empowered. To achieve this, healthcare professionals need to shift their healthcare delivery from traditional and paternalistic to that of an enabler and collaborator for the individual on their health journey.8,13 A PCDHc framework can provide a process, which increases self-efficacy and improved health outcomes.4,5
Technology is driving a shift toward empowering the individuals of healthcare services.1,2,14 Development and application of these services is leading to a demand and growth in research regarding professional competence and capability frameworks. In 2018, Brunner et al11 recognized the need to bridge existing and emerging digital health capabilities for health professionals by offering a framework, which aimed to better prepare incumbents to this evolving workforce. Likewise, other frameworks have suggested supporting skilled healthcare professionals by increasing their capability and practice in “digital skills” required for contemporary delivery.11,15 However, upon closer reading, there is a large variance in the rationale for developing these frameworks. The “why, how, and what”, which authors choose to place as broad concepts, can obscure the concept of delivering digital healthcare in a complex contemporary environment that is no longer able to exclude the role or input of the individual.1,16
New technologies in healthcare delivery have been credited as engaging, enabling, and empowering the individual by welcoming their involvement in their healthcare.14 For example, promoting a shared digital health record and shared decision-making between healthcare professionals and individuals assumes improved access, thus empowerment for the healthcare individual. This is an assumption of empowerment by the association of involvement. Healthcare demands on professionals are complex, inconsistent, and context-dependent.17 In the delivery of digital healthcare, generalizing principles for guiding communication behaviors has limitations.17 Evidence shows, when technology is used in the delivery of healthcare services, the satisfaction of the therapeutic relationship between the healthcare professional and the individual may decrease.18 Without professional capability in digital approachability, technology has the potential to negatively affect the individual, lessening social interaction, and increasing feelings of anxiety, loneliness, and disconnection.18 These negative impacts contradict the impression that any type of improved involvement with the individual automatically results in empowerment.
The authors suggest digital health and technology capabilities have been established with a continued focus on siloed traditional methods of healthcare delivery. Further, digital capability frameworks focus on the delivery of the digital healthcare technologies. These capabilities overlook required behavioral changes, goals, and outcomes skills required of professionals working in a digital healthcare environment.19 For example, the descriptions of Healthcare Digital Capabilities Framework of the United Kingdom’s National Health Services address confidence and competence using digital technologies independently of the purpose of the task at hand:15
I actively lead on and champion equitable access for all to digital teaching, learning and self-development, and I can create solutions to solve complex problems relating to individual and collaborative teaching and learning across a wide range of digital devices, tools, technologies, systems and learning environments15
The focus is the professional’s decisions and capabilities in using technologies, rather than considering the intended health outcome of having such technologies integrated into health or care delivery.11,15,20 The evidence fails to represent the required shift in communication behaviors and responsibilities required of PCDHc delivery. There is a continuing discourse around professional frameworks and capabilities for effective use of Digital Health,11,15 yet as recently as 2015, Gammon et al recognizes that the advancements in technology applied in health are still not being effectively bridged with effective development of models of care.20
Scoping the literature and mapping the capabilities currently identified for contemporary digital healthcare professionals delivering authentic PCDHc may offer insight into how the gap between theory and practice could be addressed. Identifying where digital healthcare and technologies can support person-centered care in a contemporary complex healthcare environment may lead to future discourse; practical suggestions to build person-centered integrated digital healthcare environments. This review examines current digital health and informatics capability frameworks, identifies the opportunity to include additional or alternative principles, which can underpin future development in this field of research and healthcare delivery.
This scoping review was conducted, by the two authors, over six months from September 2019 to February 2020. The objective, and method, was to scope and map available evidence of capabilities relevant and fundamental to the delivery of PCDHc, followed by identification of themes.
Method
After scoping and identifying relevant literature, a PRISMA approach21 was used to screen for eligibility. Finally, a thematic framework analysis approach22 assisted in a rigorous, iterative process required for the identification of PCDHc capabilities.
Scoping the Literature
This scoping review recognizes the “source” of information as any existing literature. For example, primary research studies, systematic reviews, meta-analyses, letters, guidelines, and websites (hereafter collectively referred to as articles). Unlike other reviews, scoping facilitated mapping of key concepts underpinning a research area, assisted in clarifying working definitions, and provided conceptual boundaries for a subject matter.23 Leaving the “source” of information open allowed the authors the inclusion of a diverse range of articles.24
The search included articles composed in English language, between 2000 and 2019 (inclusive). Databases and search engines included PubMed, Web of Science, and Google Scholar. The key search terms: digital health, health professional, allied health, digital, workforce, capability, competency, standards, and practice guidelines were used. The decision to scope the literature in this manner was made because digital healthcare professional capability frameworks are a relatively new concept and there is great variation in nomenclature and descriptions by authors which revealed difficulty in identifying the content being sought.11,25,26
This scoping review offers a preliminary assessment of available literature,27 to identify whether further attention is warranted.23 To fulfil this objective, iterative combinations of search terms were applied. Scereening the limited selection of the first hits per search in the interest of available resources for screening and relevance of articles continued in this manner.28 Where there was prior knowledge of articles these were also included for screening. An example search applied consisted of the terms “Digital health AND professional AND capability” applied in Google Scholar identified three articles of potential relevance according to their key words, title abstract, of which two succeeded the full screening process11,29 (Figure 1).
Figure 1.
Example of combination of search terms used in scoping literature to identify articles.
Eligibility Screening
Following PRISMA21 as a guide, the authors screened all identified articles for duplications, content eligibility, relevance, and finally full-text screening. Duplications were identified and removed. The remaining article titles, keywords, and abstracts were screened for content eligibility. Articles deemed irrelevant to digital healthcare practice, competencies, and capabilities were excluded. Full text of the remaining articles was screened. Those which met the inclusion criteria were agreed (Table 1).
Table 1.
Inclusion and Exclusion Criteria for Screening
| Inclusion | Exclusion |
|---|---|
| Articles published between January 1, 2000 - December 31, 2019 | Articles published before January 1, 2000 |
| English language | Absence of digital capabilities or competencies |
| Professional capability framework | Models for developing capability frameworks |
| Competencies applicable to delivering digital healthcare | Elements towards building frameworks |
| Capabilities for a digital healthcare workforce | Educational framework design |
Thematic Framework Analysis Approach
Data analysis was structured using a thematic framework analysis approach.22 Analysis was achieved in stages: Data management 1) thorough immersion in the identified literature constructing a framework by identifying descriptive characteristics then 2) indexing capabilities; Abstraction and Description 3) charting the capabilities to categories 4) mapping the categories to themes and finally Explanations 5) interpreting the findings. In summary, the approach aimed to clearly map themes, identify findings, and form a discussion. It should be noted, although the stages of analysis are depicted as linear, in practice data management, abstraction and description, and explanations were iterative.
Results
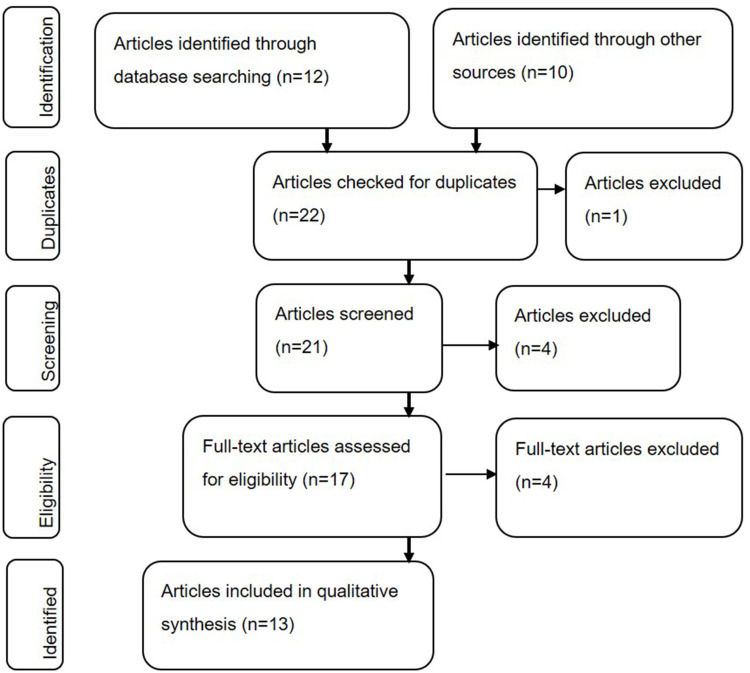
A PRISMA approach was used21 (Figure 2). After identifying relevant articles from database searches (n22), the duplicates were removed (n1). The authors then screened titles, abstracts, and keywords for eligibility by applying the inclusion/exclusion criteria (Table 1). Eight further articles were excluded; they lacked capabilities for delivering digital healthcare and were deemed to not represent appropriate capabilities or a professional competency framework. For example, there being a lack of direct focus on capabilities,7,30 description of educational elements or pedagogical approaches,31 recommendations,32–34 or discussion of intervention categories29 despite key words and titles that implied relevance. The full text articles of the remaining articles (n13) were retrieved. The authors independently reviewed these. Any differences in selection during screening and review were resolved by consensus.
Figure 2.
PRISMA approach Flow Diagram illustrating the scoping, and screening process.
Notes: Adapted with permission from Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. J BMJ. 2009;339:b2700.21
Thirteen articles were included in the final selection. These were considered to contain relevant, appropriate, and diverse contexts regarding digital healthcare capabilities required of a healthcare service or professional (Table 2).
Table 2.
Articles Eligible for Inclusion in the Review (N13)
| Reference | Comment |
|---|---|
| Adelaide University (2017)34 | Identified as a Capability - For graduates to progress into workforce supported by digital practices in health |
| Australian Digital Health Agency (2018)43 | Identified as a Capability - Areas of practice in digital health that reflect capabilities in professional practice |
| Brunner (2018)11 | Identified as a Capability - For graduates and health professionals to be e-ready and adaptable in the workforce |
| Di Donato (2019)44 | Identified as a Capability - Current and potential recognition of capabilities that underlie allied health professional role and activities in a digital health workforce |
| NHS (2018)15 | Identified as a Capability - Support the improvement of the digital capabilities of everyone working in healthcare |
| Eysenbach (2001)36 | Identified as a Characteristic – These are listed as outcomes however are described as activities reflecting competencies |
| van Houwelingen (2016)37 | Identified as a Competency - Used in professional practice of nurses operating Telehealth |
| Honey (2018)38 | Identified as a Competency - Principles for using informatics in nurses entering practice |
| Jisc (2018)39 | Identified as a Competency - Expertise for developing, delivering and educating digital health practice framework |
| Nagle (2014)40 | Identified as a Competency - Principles for using informatics in nurses entering practice |
| Martin-Sanchez (2017)41 | Identified as a Competency - A framework to define the discipline of Health informatics |
| Royal College of Nursing (2018)42 | Identified as a Competency - For digital practice in nursing |
| APS (2017)35 | Identified as a Competency - For design and delivery of a digital health service |
Scoping the literature found the terms capability, skill, characteristic, and competence were used interchangeably. Henceforth, the term capability is used to represent all terms; it is considered to encompass competency, extending beyond implied skills emphasizing adaptability, continued learning, and self-efficacy, addressing a wider view of professionalism.11,26,35 Capability is described as the aptitude to fulfill a task or type of work rather than focusing on the limitations applicable to specific roles.25 This is a point of view the authors agree with and have chosen to adopt this stance. The complex changing and adaptable nature of healthcare delivery is a reason why an open mind should be kept when considering what the role of PCDHc capabilities are.11,25,26
Analysis: Identification of Capability, Categories, and Themes
Following thorough immersion in the identified articles and constructing a framework by identifying descriptive characteristics the authors proceeded with their analysis.
Indexing Capability
The initial index contained 111 capabilities (both author’s capabilities merged). After repetitions were removed this reduced to 59 capabilities.11,36–46 Indexing the capabilities in this way made it possible to re-group the capabilities according to category if required.
Where multiple capabilities were identified as a group, these were individually labeled to reflect them as singular parts. For example, if “communication, collaboration, and participation” and “information, data, and media literacies” were cited as single capabilities in the source articles the authors separated them into individual capabilities of “Communication”, “Collaboration”, “Participation”, “Information literacy”, “Data literacy”, and “Media literacy”. Each capability was cross-checked and agreed between the authors.
Charting Categories
Charting the capabilities identified 13 categories. To assist in charting to categories, each category required a research-specific description. Category descriptions assisted in demonstrating a research-focused understanding of why each capability had been charted to a particular category, and later why the category was mapped to a theme.47
Mapping Themes
Once all the data had been labeled and categorized further refinement was required. The data in each category were reviewed together with the research objective (to scope and map available evidence of capabilities relevant and fundamental to the delivery of PCDHc). Finally, connections were made which created the themes. At this point, the author’s looked beyond the article context and toward the category descriptions and the developing themes.47 Finally, 59 capabilities charted to 13 categories, which were mapped as four themes: Change Management, User Application, Data Information & Knowledge, and Innovation (Figure 3). Validating the mapping towards generating the themes involved the author’s analysis of the key characteristics as laid out in the capabilities and categories (Table 3).
Figure 3.
Data synthesis figure of thematic analysis from labels to categories to themes.
Table 3.
Capabilities Charted into Categories
| Reference (n13) | Capabilities (n59) | Category (n13) |
|---|---|---|
| Adelaide University (2017);34 Jisc (2018);39 NHS (2018)15 | Digital creation | Applied Innovation: Activities that aim to close the gap between the theory and the practice of innovation. |
| Adelaide University (2017);34 Jisc (2018);39 NHS (2018)15 | Digital problem solving | |
| Jisc (2018)39 | Digital communication | |
| NHS (2018)15 | Safety and security (digital) | |
| NHS (2018)15 | Digital identity | |
| Eysenbach (2001);36 Di Donato (2019);44 Australian Digital Health Agency (2018);43 Royal College of Nursing (2018);42 NHS (2018)15 | Education | Education: Education is the process of facilitating learning, or the acquisition of knowledge, skills, values, beliefs, and habits. Educational methods include teaching, training, storytelling, discussion, and directed research. |
| Adelaide University (2017);34 Jisc (2018);39 Martin-Sanchez (2017)41 | Digital learning | |
| Adelaide University (2017)34 | Digital development | |
| Australian Digital Health Agency (2018)43 | Safety (medicine and therapy) | |
| van Houwelingen (2016)37 | Knowledge | |
| van Houwelingen (2016)37 | Attitudes | Holistic Care: The philosophy that the outcome or goal is greater than the sum of its parts; as such benefiting from consideration or inclusion of various elements that may not be strictly included in the definition of a given goal. |
| APS (2017)35 | Client suitability | |
| Eysenbach (2001)36 | Enabling | |
| Eysenbach (2001)36 | Engage | |
| Eysenbach (2001)36 | Equity | |
| Australian Digital Health Agency (2018)43 | My Health Record | |
| Adelaide University (2017);34 Royal College of Nursing (2018);42 NHS (2018);15 Jisc (2018)39 | Innovation | Innovation Behavior: The initiative to conceptualize, consider, attempt, or apply new ideas, products, processes, and procedures to a person’s work role, work unit, or organization. |
| Martin-Sanchez (2017);43 NHS (2018)15 | Digital wellbeing | |
| Australian Digital Health Agency (2018)43 | Champion | |
| Australian Digital Health Agency (2018)43 | Enhanced models of care | Innovative Practice: Practice with a new mindset or new way with value in it. |
| Eysenbach (2001)36 | Extending (scope of care) | |
| Adelaide University (2017);34 Martin-Sanchez (2017);41 Jisc (2018);39 Royal College of Nursing (2018);42 NHS (2018)15 | Data literacy | Technology Literacy: Ability to use technology appropriately and effectively to access, manage, integrate, evaluate, create and communicate information. |
| Adelaide University (2017);34 Martin-Sanchez (2017);41 NHS (2018);15 Jisc (2018)39 | Information literacy | |
| Brunner (2018);11 Martin-Sanchez (2017)41 | Analytics | |
| Jisc (2018);39 Adelaide University (2017)34 | Media literacy | |
| APS (2017);35 Australian Digital Health Agency (2018)43 | Privacy and security | Managing Technology: The integrated planning, design, optimization, operation, and control of technological products/tools, processes, and services. |
| Australian Digital Health Agency (2018)43 | Interoperability and data quality | |
| Nagle (2014)40 | Knowledge management | |
| Martin-Sanchez (2017)41 | Management sciences | |
| van Houwelingen (2016)37 | General skills | Non-technology Skills: Skills relevant to the role, task, or responsibilities of the person that is not defined by technology. |
| van Houwelingen (2016)37 | Implementation skills | |
| van Houwelingen (2016)37 | Clinical skills | |
| van Houwelingen (2016);37 Brunner (2018);11 Adelaide University (2017);34 NHS (2018);15 APS (2017)35 | Communication | Partnership: Cooperative skills, tasks or ethic to advance mutual interests of more than one party/role. |
| Adelaide University (2017);34 Royal College of Nursing (2018);42 NHS (2018);15 APS (2017)35 | Collaboration | |
| Adelaide University (2017);34 NHS (2018);15 APS (2017)35 | Participation | |
| Eysenbach (2001)36 | Encouragement | |
| APS (2017);35 Di Donato (2019)44 | Culture | Professionalism: The conduct, behavior, and attitude of someone in a work or business environment. These are better defined as beneficial characteristics than as requirements of a role. |
| APS (2017)35 | Policies and procedures | |
| APS (2017)35 | Organizational practice | |
| Honey (2018);38 Brunner (2018);11 Martin-Sanchez (2017);41 Royal College of Nursing (2018)42 | Professionalism | |
| Di Donato (2019);44 Royal College of Nursing (2018)42 | Leadership | |
| Eysenbach (2001)36 | Efficiency | |
| APS (2017)35 | Risk assessment and management | Professional Standards: A set of practices, ethics, and behaviors that members of a particular body (or professional role) must adhere to. |
| Nagle (2014)40 | Accountability | |
| Eysenbach (2001)36 | Enhancing quality | |
| Eysenbach (2001)36 | Ethics | |
| Eysenbach (2001)36 | Evidence based | |
| Honey (2018);38 Brunner (2018);11 Martin-Sanchez (2017);41 Nagle (2014);40 NHS (2018)15 | Information management | Technology Skills: Abilities and knowledge needed to perform specific tasks. They are practical and often relate to mechanical, information technology, mathematical, or scientific tasks. |
| Brunner (2018);11 Honey (2018);38 Martin-Sanchez (2017);41 Nagle (2014)40 | Information technology | |
| Martin-Sanchez (2017);41 Honey (2018);38 Nagle (2014)40 | Communication technology | |
| Adelaide University (2017);34 Honey (2018);38 Jisc (2018)39 | Information Communications Technology proficiency | |
| van Houwelingen (2016);37 NHS (2018);15 Royal College of Nursing (2018)42 | Technology Proficiency | |
| NHS (2018)15 | Data management | |
| Adelaide University (2017);34 Jisc (2018)39 | Digital identity | User Development: Aims to provide people without experience or pre-requisite skills with concepts, methods, and tools to allow them to create, manage, or use a given task or tool. |
| Adelaide University (2017);34 Jisc (2018)39 | Digital wellbeing | |
| Eysenbach (2001)36 | Empowerment | |
| Di Donato (2019)44 | Enable | |
| NHS (2018)15 | Self (user) development | |
| Brunner (2018)11 | Patient focus |
Findings
This section provides a description of the four themes: Change Management, User Application, Data, Information & Knowledge (DIK), and Innovation. They have been identified and validated through an iterative process of data analysis and consideration of the research objective. The four themes recognize the opportunity to align the application of technical skills towards healthcare professional capabilities required to deliver PCDHc.
Change Management
Change Management is described as the process, tools, and techniques used to manage the individual’s role in the change required to achieve an outcome.48 The theme Change Management is mapped from: professionalism, which recognizes the conduct, behavior, and attitude of an individual within a healthcare environment; education, which facilitates learning, the acquisition of knowledge, skills, values, beliefs, and habits; professional standards, which require ethical behaviors that the healthcare professional must adhere to; and the use of non-technology skills, which are relevant to the role, task, or responsibilities of the individual that are not defined by technology.
User Application
The theme, User Application, relates to tasks, processes, responsibilities, and objectives that are designed or designated for operation by the healthcare individual (specifically for the healthcare individual to apply). Despite a long-standing focus on the individual in person-centered healthcare, at times referred to as the “user”, the authors found no consistent language or terminology to reflect the focus on the supporting elements for the individual to be able to apply themselves or the technologies of person-centered healthcare. Therefore, the term “User Application” is considered a novel term for the purpose of this article. User Application differs from the theme Change Management in the person-centered focus of the healthcare individual as opposed to the focus on change itself. The theme is mapped from: User-development, suggesting the preparation of inexperienced individuals, those who require pre-requisite skills, methods, and tools to allow them to create, manage or use a given task or tool; and holistic care, described as greater than the sum of its parts. This theme benefits from consideration or inclusion of diverse elements; the third category in this theme is partnership, collaboration to advance mutual interests of more than one individual/profession.
Data, Information, Knowledge
The term Data, Information, Knowledge (DIK)49 represents the ability to identify data, interpret information, and create knowledge. The theme emphasizes insight, technical ability, knowledge, and understanding rather than “hands-on” healthcare application. DIK is mapped from: technology skills, which require the acquisition of ability and knowledge needed to perform specific mechanical, mathematical, or scientific tasks; technology literacy, which requires the ability to use technology appropriately and effectively to access, manage, integrate, evaluate, create, and communicate information; and managing technology, which requires the ability to integrate planning, design, optimization, operation, and control of technological products, processes, and services.
Innovation
Innovation is defined by the authors as fundamental to the creation, development, and adoption of contemporary models of care. This theme is mapped from: innovative practice, which requires valuing the opportunity of applying a new mindset; innovation behavior, requiring the ability to conceptualize, consider, attempt or apply new ideas, processes, and procedures; and applied innovation, which aims to close the gap between the theory and the practice. Technology is rapidly evolving. The development of new tools, applications, and opportunities provided by technology continually challenges current processes and technical proficiencies which in turn encourages innovation behavior.
Whilst evidence-based practice is a vital tenet of maintaining professional standards for high-quality healthcare, and represented in the capabilities of Change Management, these are directly impacted by the ability to conceptualize new forms of evidence, new mindsets for which evidence may be needed, and practices that may need review in light of new evidence and technology. Innovation practice is therefore a key factor in allowing the important function of continuing innovation to occur and in turn supporting and complimenting other themes identified.
Summary of Themes
The capabilities that mapped together forming each of the four themes shaped the priorities of each theme reflected in their definitions. The authors then considered whether the capability themes identified collectively and individually genuinely support PCDHc. Common focal points from each theme were found to provide complimentary as well as clashing interests in how they support PCDHc. The common points were technology focusing on its new possibilities and required literacy; contemporary models of care considering their objectives as well as the goal to develop and adopt such models; and finally the role of the individual in and for the given capability. The role of the individual is complimented between the theme of Change Management and User Application to achieve an outcome, whereby Change Management addresses the healthcare professional and User Application addresses the individual. These two themes however equally stand apart from each other in that Change Management prioritizes the change itself that needs managing whereas User Application prioritizes the person at the center above all else.
The objectives of contemporary models of care are reflected as priorities in the theme of Innovation and User Application by focusing on how these objectives are applied along with supporting the individual in achieving their appropriate outcomes of care, respectively. The theme of Innovation fundamentally focuses on innovations required to do so whereas User Application places the person as the priority instead. Innovation and Change Management converge regarding development and adoption of contemporary models of care. Innovation prioritizes the earlier stages of development whereas Change Management addresses the elements needed to see a successful adoption of such models of care and so represent related yet distinct parts of the same goal.
Technology brings together DIK, Innovation and User Application in using technology literacy to allow an individual to achieve an outcome that may be defined or created by innovations in technology and/or the model of care. These themes stand apart from each other in each prioritizing the technology itself over the purpose for its use, or the capacity to create new methods and outcomes of or prioritizing the support needed for the individual to achieve and outcome, respectively.
Discussion
Do the Current Capabilities Support PCDHc?
Four themes were identified from mapping the capabilities, with common focal points and points of difference among the scope and definitions in each theme. A clear understanding of the capabilities required to genuinely support PCDHc is dependent on a clear understanding of how to define PCDHc. The term PCDHc is comprised of: person-centered that can be considered as the individual with a role in the healthcare journey; digital that can be represented as the technology that is shaping contemporary healthcare and lastly healthcare itself can be thought to represent the contemporary model of care being used. The common points of interest across the four themes of capabilities thus support that the capabilities found in current literature do collectively support PCDHc. The NHS capability framework listed capabilities that mapped across all four themes; however, there was at least one category within each theme that did not contain any capabilities from this framework.15 The digital capability framework for health professional published by Brunner et al in 2018 did not provide any capabilities that mapped to the theme of Innovation.11 The available discourse around capabilities for PCDHc shows great variation in the recognition of required capabilities from across the four themes identified in this article to support PCDHc. Siloed discussion of the capabilities overlooks opportunities for alignment that could lead to more productive conversations and a better understanding of healthcare outcomes for contemporary models of care.
Realizing needed change in the adoption of PCDHc for the health professional and individual alike can be supported by the categories that were mapped to Change management. The theme of User Application recognizes what an individual’s healthcare journey should address how the use of healthcare technology and services should be applied to deliver benefit in health outcomes. The delivery of healthcare, especially with the use of technology should maintain a focus on the delivery of care (encouragement, collaboration, and attitude) along with individual digital user outcomes (digital wellbeing and My Health Record). The theme recognizes the healthcare individual together with the application of professional skills as necessary components of successful PCDHc.
While the focus of DIK is technical proficiency, required in the application of DIK, its value is fundamental in the enablement of successful Change Management and User Application. Diagnosis and delivery are essential components of any health process; DIK is an essential partner to all themes, allowing PCDHc to be holistic in design and delivery. The basic concept of informed decisions requires the ability to understand the information needed to be able to make a decision.
Effective change of tools, behaviors, and potential outcomes is benefited by a thorough understanding of how any change impacts any part of the healthcare journey. Holistic mindsets are imperative in maintaining healthcare practice and delivery and must align with the objective of PCDHc. Applied innovation thus supports the objective of achieving PCDHc by focusing on bringing theory and practice closer together. The four themes, together with the research aims and objectives, form the scaffold for the following discourse of PCDHc.
Future Directions and Considerations
The authors suggest, despite the urgent need for transitional models of healthcare, debates regarding professional digital capability persist in being “siloed” and “paternalistic”.13,20,47 The authors propose transitioning to PCDHc requires refocusing (rather than rewriting) current capabilities. Focusing on Change Management; User Application; Data, Information, and Knowledge; and Innovation.
Personal Cost in Change Management
Emphasis on Change Management11,37–46 implies high regard for capabilities that leverage technical skills and knowledge as effective performance in a professional role. A common occurrence in the workplace is the expectation of developing digital literacy and capability skills without appropriate investment in either time or support.50,51 There is a recognized expectation on healthcare professionals entering the workforce to be future-ready and proficient for PCDHc.11,36
The investment in time and effort, to transition to suitably proficient in new and evolving technical and procedural skills, results in hugely variable cognitive and professional load. The impact is represented in the literature as a professional burden.36,41,51 This burden effects an individual’s capacity to develop capability, thus creating simultaneous cause and effect of being overwhelmed and performance being compromised.51 Insufficient or ineffective change management is thus an important concern for individuals, healthcare professionals, and organizations. For all individuals, the potential consequence of digital illiteracy is disengagement.52 This multifaceted effect alienates individuals rather than valuing their interaction.18
Digital learning and development places a priority on the capability to achieve new and evolving technical proficiencies; for example, “digital learning and development”.36,41 Professional standards for accreditation, registrations, and other professional obligations dictate the change management needs and investments of the healthcare professional. If these standards are perceived as the motivation for a professional, who invests time and effort into gaining new capabilities, a reactive culture toward change management can be created rather than a pro-active one. The nuances of change management alone cannot truly reflect the intentions of PCDHc, which relies on a pro-active, innovative mindset.
Perspective and Priorities
The application of Bandura’s theory of self-efficacy in the context of health behavior remains in high regard when improving health outcomes.4 When considering User Application and development, the practice of self-efficacy should be prominent in creating and supporting elements of self-development and empowerment. However, the focus of capabilities identified in this review was aligned with the healthcare professional perspective of skills and objective goals, rather than the individual’s health outcome. The subtle but important difference in the underlying perspective implies that the practice of self-efficacy in healthcare, which should be the foundation of person-centered care, is not reflecting the theory and thus is not promoting a truly PCDHc. The authors suggest, this lack of alignment between theory and practice of person-centered care exemplifies the disconnect between digital capabilities in healthcare.
DIK is technical in its focus, of observation, description, and instruction.49 This focus misses the point, how to influence effective performance. The review identifies a strong consensus on the value of technology, rather than the capability of using technology to improve health outcomes. Further, the repeated emphasis on information management,11,15,40,42,43 rather than the importance of understanding the management of data,15 knowledge,42 and interoperability,45 suggests that information is deemed more valuable than knowing what to do with it. This restricted perspective of healthcare is considered to be limiting the ability for transformation toward PCDHc and envisioning a holistic perspective of the contemporary landscape. The inevitable growth of new technology-related knowledge constantly requires resources such as time and professional development support allocated accordingly. This iterative demand impacts the professional’s ability to remain open to the broader reaches of healthcare knowledge and needs.13 Specialist wisdom adds value to knowledge, and this requires judgment that is unique and personal to the individual.49 The appropriate application of wisdom should be regarded as innovation for the benefit of bridging knowledge and capabilities. Application of wisdom has the potential to benefit the holistic perspective of PCDHc seeks to attain.
The National Health Service, Health and Care Digital Capability Framework15 describes digital safety and security as the responsibility of championing safe and secure digital creation. The NHS framework requires the professional to reflect and evaluate unforeseen or unintended consequences their “digital methods and use of technology” may have on safety and security rather than vice versa.15 The fundamental priority of exploration into undefined knowledge, rather than conforming with current knowledge, is an innovative value that brings greater value than technical proficiency or professional merit alone can achieve.
In 2015, Gammon et al identified a fundamental disconnect between technology capabilities and healthcare service development and delivery.20 This review reawakens their concerns, which remain present and need greater attention in discourse regarding PCDHc capabilities and professional practice. Focusing on digital capabilities, such as the ability to use technology rather than understood to be integral to care, overlooks the fact that such capabilities impact professional functions required of healthcare delivery. These include clinical and ethical decision-making, empowerment, suitability for services, promotion of health and wellness, and new models of care.11,53
Chronic disease management is growing sector in healthcare,54 involving greater input from the healthcare individual over time than any other sector of healthcare. Complex chronic care therefore represents a good fit for discussing PCDHc as the future model of care. The authors refer Grover and Joshi’s55 review of Chronic Disease Models (CDM) models, including Chronic Care Model (CCM).5 The CCM demonstrates a robust model in supporting and improving chronic care. The integration of information systems is deemed the weakest attribute of the Chronic Care Model.5 However, the development in technical capability and related literature compensate for this. The CCM defines the outcomes of the healthcare journey rather than defining the role of a healthcare professional within that journey. This is in contrast to the Digital Capabilities articles identified in this scoping review that predominantly positioned the role of the healthcare professional within a paternalistic model of care. One which oversees the health outcome. This is a subtle distinction but the authors consider this to be a fundamental nuance in understanding the role of capabilities in PCDHc.
Digital tools and technologies can assist and support the delivery of person-centered healthcare. Understanding the purpose of using digital tools and technologies can assist in more productive conversations on how to define professional capabilities in PCDHc. This review affirms a previously held conviction that discourse on healthcare practices and professional capabilities do not reflect truly person-centered healthcare.13,20 The realignment of capabilities towards the person’s healthcare outcomes, rather than the professional’s immediate obligation can steer the perspective towards a real PCDHc system.
The consistent reference to data, information, and knowledge with an absence of wisdom reaffirms the gap between appreciation of digital capabilities and their place in PCDHc. Valuing holistic wisdom, across rather than towards skills in isolation, may be one way to address the technical focus rather than sought-after person-centered health outcomes. In PCDHc delivery, the unpredictable nature of the healthcare individual and professional will always impact the use and application of any task, tool, or technology. While healthcare tools and technology continue to evolve, professional capabilities must also evolve to address the complex behavior of the person at the center of their healthcare journey.
Limitations
Our study has several limitations, firstly that the scope of literature was not systematic. The risk of the current method is that appropriate articles may have been missed in the scoping exercise. Further exploration of this project or continuation would be advised to conduct a systematic review as the primary step. This project has also been completed over a relatively short six-month period, within the parameters of routine work and without any funding or additional time sought or received.
Given the relatively new field being investigated, and as such a new field of resources available, there were limited opportunities to develop frameworks/guidelines. This is, in turn, why a smaller project was conducted to gauge feasibility and scope for further potential investigation/research. Only two researchers conducted this research project however, it should be noted that the two researchers represent very different health disciplines, which itself is a benefit supporting a cross-discipline perspective of the subject matter. All data and findings were primarily validated by each author moderating the other’s work. Final validation was sought by requesting support from one further expert in the field of health, care, and education.
Conclusion
This scoping review confirms the assumption that digital skills will empower all healthcare stakeholders is incorrect. Bandura4 and Wagner5 have repeatedly discussed the need for appreciation of complex human behavior change. The need to enable and empower the healthcare individual in their digital healthcare journey is equally part of this conversation. Achieving these goals for the individual requires supporting self-efficacy4 and delivering PCDHc for safe, quality health outcomes for the healthcare individual and health service.
As recently as 2015, the authors identified, the continued disconnect between (or siloed delivery of) health, care, and the accepted innovations of technology available.20 However, articles continue to fail to acknowledge the impact of behavior4,11 on the delivery of PCDHc.11,20 The appropriate application of reflective practice, PCDHc delivery, and use of the capabilities discussed in Brunner et al and other articles40–44 remains open and important to achieve a truly PCDHc. This scoping review suggests healthcare models continue to be interpreted to fit the needs of the healthcare professional without the consideration of person-centered care. Healthcare professionals and researchers need to work together to address the intrinsic behaviors that could potentially allow for effective change in healthcare practice or health outcomes.
The root of this issue may be the gap that Gammon et al42 identified between models of care and digital technology evolutions. The authors propose it is time to stop generating ubiquitous silos and start bridging the gap between technology and the practice of healthcare. This review also draws attention to the need for more research to enable digital healthcare systems and services to be designed to realize complex human behaviors and multiple person-centered care requirements. Clarity and consistency of the objectives of PCDHc and the appropriate mindset for truly encompassing them may be beneficial in revising and/or further exploring the effective capabilities for PCDHc.
The authors acknowledge that people are complex, technology is constantly adapting, and care will always need to evolve to meet chronicity and changing behaviors. Any investment in resources such as time and effort into gaining new digital capabilities and professional development needs to be allocated appropriately. Now more than ever, it is imperative to align healthcare capabilities with technologies to ensure that the practice of PCDHc is the empowering journey for the healthcare user that theory implies.
Acknowledgments
The authors would like to acknowledge Dr Ian Almond, who contributed his expertise and time to reviewing and editing the paper.
Abbreviations
EHR, electronic health record; PCDHc, person-centered digital healthcare; DIK, data, information and knowledge; DIKW, data, information, knowledge, and wisdom; CCM, chronic care model; CDM, chronic disease model.
Disclosure
The authors report no conflicts of interest in this work. No funding or resources were sought or used in the preparation of this work.
References
- 1.Huckvale K, Wang CJ, Majeed A, Car J. Digital health at fifteen: more human (more needed). BMC Med. 2019;17(1):62. doi: 10.1186/s12916-019-1302-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ovretveit J. Digital technologies supporting person-centered integrated care - a perspective. Int J Integr Care. 2017;17(4):6. doi: 10.5334/ijic.3051 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sturmberg J. Person-centered medicine from a complex adaptive systems perspective. Eur J Person Centered Healthcare. 2014;2(1):85–97. doi: 10.5750/ejpch.v2i1.711 [DOI] [Google Scholar]
- 4.Bandura A. Self-efficacy and human functioning In: Schwarzer R, editor. Self-Efficacy: Thought Control of Action. Abingdon, Oxon: Routledge; 1992:3–38. [Google Scholar]
- 5.Wagner E, Austin B, Von Korff M. Improving outcomes in chronic illness. Managed Care Q. 1996;4(2):12–25. [PubMed] [Google Scholar]
- 6.Greenhalgh T, Snow R, Ryan S, Rees S, Salisbury H. Six ‘biases’ against patients and carers in evidence-based medicine. BMC Med. 2015;13:200. doi: 10.1186/s12916-015-043 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chute C, French T. Introducing care 4.0: an integrated care paradigm built on industry 4.0 capabilities. Int J Environ Res Public Health. 2019;16(12):2247. doi: 10.3390/ijerph16122247 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mesko B, Drobni Z, Benyei E, Gergely B, Gyorffy Z. Digital health is a cultural transformation of traditional healthcare. Mhealth. 2017;3:38. doi: 10.21037/mhealth.2017.08.07 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cronenwett L, Sherwood G, Barnsteiner J, et al. Quality and safety education for nurses. Nurs Outlook. 2007;55(3):122–131. doi: 10.1016/j.outlook.2007.02.006 [DOI] [PubMed] [Google Scholar]
- 10.Scholz N Focus on digital health events [Blog]. European Parliament Research Service. European Parliament Research Service;2016. Available from: https://epthinktank.eu/2016/06/07/focus-on-digital-health-events/. Accessed February10, 2019. [Google Scholar]
- 11.Brunner M, McGregor D, Keep M, et al. An eHealth capabilities framework for graduates and health professionals: mixed-methods study. J Med Internet Res. 2018;20(5):e10229. doi: 10.2196/10229 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Arsand E, Demiris G. User-centered methods for designing patient-centric self-help tools. Inform Health Soc Care. 2008;33(3):158–169. doi: 10.1080/17538150802457562 [DOI] [PubMed] [Google Scholar]
- 13.Maddocks I. Silo mentality bad for our patients. Med J Austr. 2016;41. [Google Scholar]
- 14.Topol E. The topol review: preparing the healthcare workforce to deliver the digital future [Report]. Health Education England, NHS; 2019. Available from: https://topol.hee.nhs.uk/. Accessed March5, 2019. [Google Scholar]
- 15.NHS. A health and care digital capabilities framework [Framework]. 2018. Available from: https://www.hee.nhs.uk/sites/default/files/documents/Digital%20Literacy%20Capability%20Framework%202018.pdf. Accessed September 2019.
- 16.Koshy K, Limb C, Gundogan B, Whitehurst K, Jafree D. Reflective practice in health care and how to reflect effectively. Int J Surg-Oncol. 2017;2:6. doi: 10.1097/IJ9.0000000000000020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Salmon P, Young B. Creativity in clinical communication: from communication skills to skilled communication. Med Educ. 2011;45(3):217–226. doi: 10.1111/j.1365-2923.2010.03801.x [DOI] [PubMed] [Google Scholar]
- 18.Lengacher L. Mobile technology: its effect on face-to-face communication and interpersonal interaction. URJHS. 2015;14:1. [Google Scholar]
- 19.Hadziomerovic A. Competencies, Capabilities and Skills. What’s the difference and how are they used?: Linkedin; October 2017. Available from: https://www.linkedin.com/pulse/competencies-capabilities-skills-whats-difference-how-aida/. Accessed November13, 2019.
- 20.Gammon D, Berntsen GK, Koricho AT, Sygna K, Ruland C. The chronic care model and technological research and innovation: a scoping review at the crossroads. J Med Internet Res. 2015;17(2):e25. doi: 10.2196/jmir.3547 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. J BMJ. 2009;339:b2700. doi: 10.1136/bmj.b2700 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ritchie J, Lewis J, Nicholls CM, Ormston R, editors. Qualitative Research Practice: A Guide for Social Science Students and Researchers. Sage; 2013. November; 1. [Google Scholar]
- 23.Arksey H, O’Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol. 2005;8(1):19–32. doi: 10.1080/1364557032000119616 [DOI] [Google Scholar]
- 24.Peters MDJ, Godfrey C, McInerney P, Munn Z, Tricco AC, Khalil H. Chapter 11: scoping Reviews (2020 version) In: Aromataris E, Munn Z, editors. JBI Manual for Evidence Synthesis. JBI; 2020. Available from: https://wiki.jbi.global/display/MANUAL/Chapter+11%3A+Scoping+reviews. Accessed December13, 2020. [Google Scholar]
- 25.Lester S. Professional standards, competence and capability. Higher Educ Skills Work-Based Learning. 2014;4(1):31–43. doi: 10.1108/heswbl-04-2013-0005 [DOI] [Google Scholar]
- 26.Phelps RHS, Ellis A. Competency, capability, complexity and computers: exploring a new model for conceptualising end-user computer education. Br J Educ Technol. 2005;36(1):67–84. doi: 10.1111/j.1467-8535.2005.00439.x [DOI] [Google Scholar]
- 27.Grant MJ, Booth A. A typology of reviews: an analysis of 14 review types and associated methodologies. Health Info Libr J. 2009;26(2):91–108. doi: 10.1111/j.1471-1842.2009.00848.x [DOI] [PubMed] [Google Scholar]
- 28.Pham M, Rajic A, Greig J, Sargent J, Papadopoulos A, McEwen S. A scoping review of scoping reviews: advancing the approach and enhancing consistency. Res Syn Meth. 2014;5:371–385. doi: 10.1002/jrsm.1123 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.World Health Organization. Report on the public consultation to inform development of the Framework on integrated people-centred health services [Report]. World Health Organization; 2016. Available from: https://apps.who.int/iris/bitstream/handle/10665/246252/WHO-HIS-SDS-2016.ng.pdf. Accessed September20, 2019. [Google Scholar]
- 30.Eysenbach G, Jadad A. Evidence-based patient choice and consumer health informatics in the Internet age. J Med Int Res. 2001;3(2):e19. doi: 10.2196/jmir.3.2.e19 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Herrington J, Oliver R. An instructional design framework for authentic learning environments. Etr&d-Educ Tech Res. 2000;48(3):23–48. doi: 10.1007/Bf02319856 [DOI] [Google Scholar]
- 32.Christopherson TA, Troseth MR, Clingerman EM. Informatics-enabled interprofessional education and collaborative practice: a framework-driven approach. J Interprof Ed Prac. 2015;1(1):10–15. doi: 10.1016/j.xjep.2015.03.002 [DOI] [Google Scholar]
- 33.Mantas J, Ammenwerth E, Demiris G, et al. Recommendations of the International Medical Informatics Association (IMIA) on education in biomedical and health informatics. Meth Inf Med. 2010;49(02):105–120. doi: 10.3414/ME5119 [DOI] [PubMed] [Google Scholar]
- 34.Beetham H, McGill L, Littlejohn A, Joint Information K Systems Committees (JISC). Thriving in the 21st century: learning literacies for the digital age (LLiDA project): executive Summary, Conclusions and recommendations [Study Report]. Open Research Online. June 2009. Available from: http://oro.open.ac.uk/52237/1/llidaexecsumjune2009.pdf. Accessed September20, 2019.
- 35.O’Connell JGG, Coyer F. Beyond competencies: using a capability framework in developing practice standards for advanced practice nursing. J Adv Nurs. 2014;70(12):2728–2735. doi: 10.1111/jan.12475 [DOI] [PubMed] [Google Scholar]
- 36.Adelaide University. Developing Digitally Capable Graduates [Framework]. Digital Capabilities @ Adelaide. 2017. Available from: https://universityofadelaide.app.box.com/s/d65cpexld49xbhxp0u7lws48v0ghtxis. Accessed September20, 2019.
- 37.APS Ltd. Telehealth measure to improve access to psychological services for rural and remote patients under the Better Access initiative [Considerations for Providers]. Australian Psychological Society; 2017. Available from: https://www.psychology.org.au/getmedia/4dd9dd91-1617-421b-928c-531d019f05c2/17APS-Telehealth-Web.pdf. Accessed September20, 2019. [Google Scholar]
- 38.Eysenbach G. What is e-health? J Med Internet Res. 2001;3(2):E20. doi: 10.2196/jmir.3.2.e20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.van Houwelingen CT, Moerman AH, Ettema RG, Kort HS, Ten Cate O. Competencies required for nursing telehealth activities: a Delphi-study. Nurse Educ Today. 2016;39:50–62. doi: 10.1016/j.nedt.2015.12.025 [DOI] [PubMed] [Google Scholar]
- 40.Honey M, Collins E, Britnell S. Guidelines: Informatics for Nurses Entering Practice [Guidelines]. Aukland, New Zealand: Univesity of Auckland; 2018. Available from: https://auckland.figshare.com/articles/Guidelines_Informatics_for_nurses_entering_practice/7273037. Accessed September20, 2019. [Google Scholar]
- 41.Jisc. Building digital capability: the six elements defined [Framework]. Jisc. September 2018. Available from: http://repository.jisc.ac.uk/6611/1/JFL0066F_DIGIGAP_MOD_IND_FRAME.PDF. Accessed September20, 2019..
- 42.Nagle LM, Crosby K, Frisch N, et al. Developing entry-to-practice nursing informatics competencies for registered nurses. Stud Health Technol Inform. 2014;201:356–363. [PubMed] [Google Scholar]
- 43.Martin-Sanchez F, Rowlands D, Schaper L, Hansen D. The Australian Health Informatics Competencies Framework and Its Role in the Certified Health Informatician Australasia (CHIA) program. Stud Health Technol Inform. 2017;245:783–787. [PubMed] [Google Scholar]
- 44.Royal College of Nursing. Every Nurse an E-Nurse: Insights from a Consultation on the Digital Future of Nursing [Report]. London: Royal College of Nursing; 2018. Available fromhttps://www.rcn.org.uk/professional-development/publications/pdf-007013#detailTab. Accessed September20, 2020. [Google Scholar]
- 45.Australian Digital Health Agency. Framework for action: how Australia will deliver the benefits of digitally enabled health and care [Framework]. ADHA. 2018. Available from: https://conversation.digitalhealth.gov.au/sites/default/files/framework_for_action_-_july_2018.pdf. Accessed September20, 2020.
- 46.Donato D. The untapped potential in digital health. J Allied Health Professionals. 2019. Available from https://www.hisa.org.au/wp-content/uploads/2019/08/Allied-HI-PositionStatement.pdf?x30583. [Google Scholar]
- 47.Almond H Exploring the experiences of and engagement with Australia’s shared digital health record by people living with complex chronic conditions in a rural community. [Thesis]. University of Tasmania; 2018. [Google Scholar]
- 48.Prosci. An Introduction to Change Management [Article] Thought Leadership Articles. Prosci; Available from https://www.prosci.com/resources/articles/change-management-definition#:~:text=Change%20management%20is%20the%20process,adoption%20and%20realization%20of%20change. Accessed February14, 2020. [Google Scholar]
- 49.Rowley J. The wisdom hierarchy: representations of the DIKW hierarchy. J Info Com Sci. 2007;33:2. doi: 10.1177/0165551506070706 [DOI] [Google Scholar]
- 50.S BP L, Konstantinidis ST, Traver V, Car J, Zary N. Setting priorities for EU healthcare workforce IT skills competence improvement. Health Informatics J. 2019;25(1):174–185. doi: 10.1177/1460458217704257 [DOI] [PubMed] [Google Scholar]
- 51.Morrison JaL P. When no one has time: measuring the impact of computerization on health care workers. Workplace Health Saf. 2008;56(9):373–378. doi: 10.1177/216507990805600902 [DOI] [PubMed] [Google Scholar]
- 52.van der Vaart R, Drossaert CH, Taal E, Drossaers-Bakker KW, Vonkeman HE, MA van de Laar. Impact of patient-accessible electronic medical records in rheumatology: use, satisfaction and effects on empowerment among patients. BMC Musculoskelet Disord. 2014;15(1):102–110. doi: 10.1186/1471-2474-15-102 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Gray K. Public health platforms: an emerging informatics approach to health professional learning and development. J Public Health Res. 2016;5(1):665. doi: 10.4081/jphr.2016.665 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.AIHW. Chronic Disease [Homepage]. AIHW, Australian Government; 2019. Available from: https://www.aihw.gov.au/reports-data/health-conditions-disability-deaths/chronic-disease/overview. Accessed February14, 2020. [Google Scholar]
- 55.Grover A, Joshi A. An overview of chronic disease models: a systematic literature review. Glob J Health Sci. 2015;7(2):210. doi: 10.5539/gjhs.v7n2p210 [DOI] [PMC free article] [PubMed] [Google Scholar]