Abstract
The Plasma Bio-Filler Facelift is an exciting aesthetic process being introduced in dermatology. The dermal filler gel is autologous and easy to obtain. It works well for fine rhytides reduction as well as to volumize, contour and rejuvenate the face, neck and hands. The consistency and autologous nature of plasma bio-filler are better accepted by patients than the high density hyaluronic acid fillers.
Keywords: Bio-filler, plasma filler, plasma gel
Sir,
The Plasma Bio-Filler Facelift is an exciting aesthetic process being introduced in dermatology. The dermal filler gel is autologous and easy to obtain. It works well for fine rhytides reduction as well as to volumize, contour, and rejuvenate the face, neck, and hands. The consistency and autologous nature of plasma bio-filler are better accepted by patients than the high-density hyaluronic acid fillers.
A 52-year-old woman presented to us with facial aging changes such as loss of volume on zygomatic bones, nasolabial lines, and fine lines around eyes and forehead. She was counseled regarding hyaluronic acid fillers, botulinum toxin treatments, and radio-frequency or CO2 laser skin tightening. But she was unwilling for any of these procedures. We advised regarding platelet-rich plasma (PRP) injections for fine lines and plasma gel filler for adding volume to zygomatic prominence points and nasolabial lines. She agreed to this considering low cost and plasma gel being autologous product so no immunogenic potential. She was counseled regarding lasting of effects of this procedure up to 3–6 months with a touch-up procedure at 2–3 months.
Topical 2.5% lidocaine plus 2.5% prilocaine anesthetic cream was applied over the patient’s face on the areas to be treated for 45 min. Ten milliliters of patient’s blood was drawn and mixed with 1 mL anticoagulant acid citrate dextrose. It was rotated at 3200 rotations per minute (RPM) for 8 min in a centrifuge machine. The plasma solution was withdrawn and centrifuged again at 1000 RPM for 5 min. The upper part that is platelet-poor plasma (PPP) was withdrawn in a 5 mL syringe, approximately 4.5 mL, and the lower part that is PRP was withdrawn in 3 insulin (1 mL) syringes, approximately 2.5 mL [Figure 1].
Figure 1.

PRP and PPP formation
Calcium gluconate was added in the PPP in the proportion of 0.01 mL/1 mL of PPP. It was incubated in hot water (heated in a metal container) at 100°C (gradually reducing to 98°C) for 5 min and then in cold water bath in a metal container with initial temperature 7°C and gradually increasing to 10°C for 5 min. The temperatures were measured by infrared thermometer. The viscous gel, approximately 3 mL in volume, was ready for use [Figure 2]. After cleaning of the topical anesthetic cream, approximately 2.5 mL of PRP was injected at multiple points over forehead, around eyes, and around lips over fine lines and wrinkles through insulin syringes. Then PPP gel filler was injected below the dermis just above the bone with 24G needle on both zygomatic prominences with three points triangle technique, 1 mL on each side. It was injected linearly along the nasolabial lines depositing the bio-filler while withdrawing the needle, 0.5 mL on each side (linear threading technique). Injections were placed away from visible blood vessels. The sites were gently massaged to allow uniform distribution of the injected plasma gel to maintain the contour of the surrounding tissues. Other than mild pain due to injections, patient did not have any adverse effects. The patient was advised to avoid massage or extended pressure within the treated area for a week. As a result of some resorption of the gel after 2 weeks, a touch‐up session of plasma gel injection was given to provide optimal correction [Figure 3].
Figure 2.
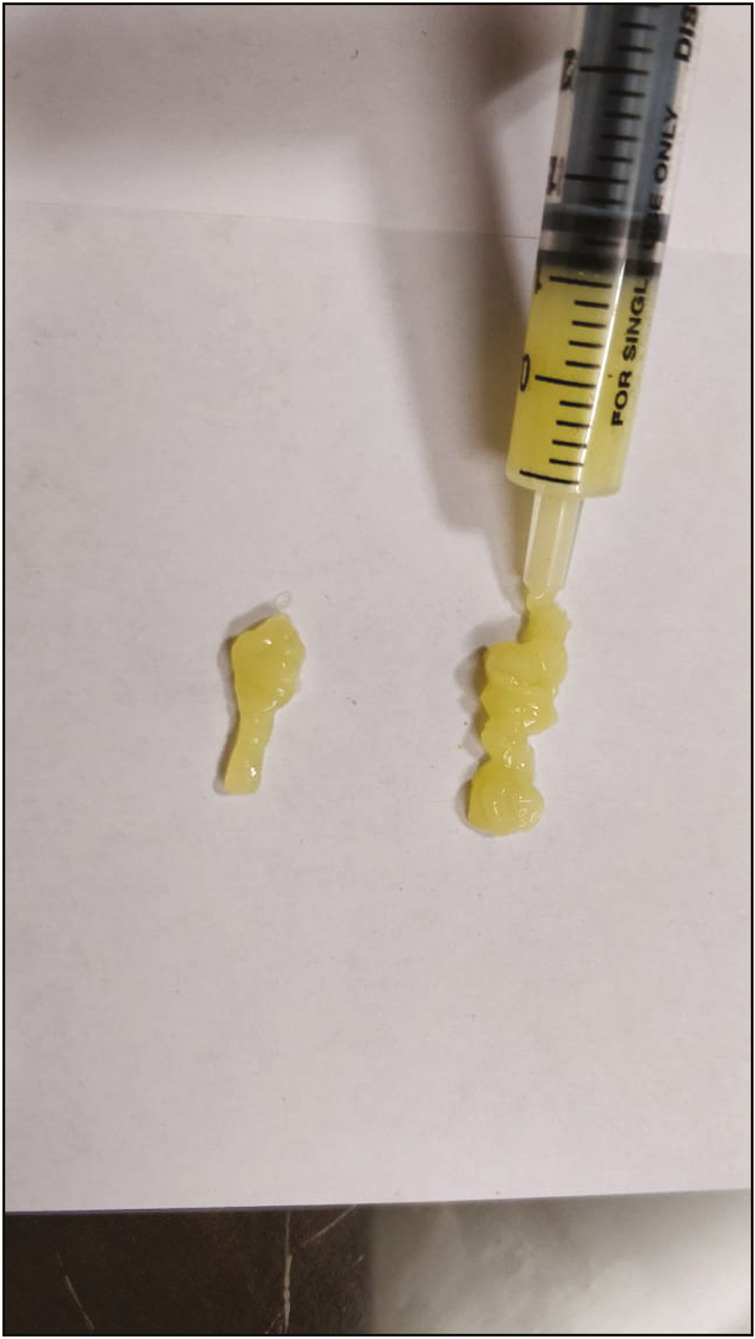
Plasma gel after incubation of platelet-poor plasma
Figure 3.

Before and after image of patient after injecting bio-filler
The hollowness over zygomatics and nasolabial lines immediately showed more volume and filled effect. Patient was counseled regarding improvement of fine lines over 3–4 weeks due to new collagen production by PRP. On the follow-up of 1 month and later at 3 months, patient showed considerable improvement in overall skin texture, laxity, and dullness, and the filling effect of bio-filler was maintained up to 60%–70% of the original volume.
Anti-aging or facial rejuvenation by soft-tissue augmentation to eliminate facial wrinkles, tear trough deformity, smile lines, and sunken cheek bones has been successfully treated by surgery,[1] botulinum toxin, injectable fillers such as hyaluronic acid, and bovine collagen. In spite of several advantages with these materials, the high cost and possibility of allergic reaction, inflammation, foreign body granuloma formation, and skin necrosis due to incorrect injection techniques resulting in blockage of blood vessels are still considerable adverse effects.[2] Therefore, autologous bio-implants including fat and collagen have been introduced for augmentative purpose. However, they require general or tumescent anesthesia and may cause donor-site morbidity and difficulty with volume control of acquired tissue.[3] Thus, more convenient, safe, and inexpensive autologous materials are required.
Activation of PPP by adding a clotting cascade activator, such as calcium gluconate, calcium chloride or thrombin, and/or thermal treatment, gives rise to the formation of plasma gel.[4] It contains fibrin, which provides the gel greater consistency and resistance, and gelled proteins provide constant stability and volume.[5] In the recent years, plasma gel has gained popularity in other fields such as plastic surgery, orthopedic surgery, and oral surgery.[6] Hatakeyama et al.[7] evaluated the ultrastructural morphology and components of both PRP and PPP, and found that although the concentration of platelets and their growth factors in the PRP was much higher than in the PPP, fibrinogen concentration in PPP was much higher than in PRP. The fibrin fibers are usually formed in bundles in PPP rather than in PRP. This fibrous network of insoluble fibrin provides a scaffold for platelets that serve as a source for the sustained release of growth factors.[7] This scaffolding helps to localize the growth factors and increase their concentration at the desired location to facilitate tissue regeneration.[8] The direct volumetric filling effect of the gel is due to the denaturized gelled proteins and fibrin bundles providing constant stability and volume.[8] In addition, platelets work through the degranulation of α‐granules that contain presynthesized growth factors.[9]
The gel serves to localize both activated platelets and their presynthesized growth factors in the treated area. The platelets trapped in the gel continue to synthesize and release bioactive growth factors after injection.[10] These growth factors interact with the undifferentiated adipose-derived stem cells and dermal fibroblasts by binding to their specific cellular receptors promoting neovascularization and neocollagenesis, resulting in soft-tissue augmentation and reduction of wrinkles.[11] It is suggested that the continual release of growth factors from trapped platelets at the injection site may be responsible for the sustained therapeutic effects of plasma gel for several months after the treatment session.[12] These growth factors also enhance synthesis of extracellular matrix components such as hyaluronic acid. The contraction of myofibroblasts around wrinkles causes skin tightening and strengthening.[13]
The study conducted by Doghaim et al.[14] on 52 female patients with facial wrinkles (group A) and tear trough deformities (group B) reported a few side effects of plasma gel injection such as transient minor pain, burning sensation, erythema, and edema at the site of injection, which disappeared spontaneously within few hours. No patient reported any fibrosis, irregularity, hardness, or lumpiness at the injection site at any time. They showed immediate significant clinical improvement after plasma gel injection that was maintained till the end of follow‐up period of 3 months. This finding was confirmed by significant reduction in the mean values of Wrinkle Severity Rating Scale in group A and Tear Trough Rating Scale in group B, and significant improvement of skin homogeneity and texture in both groups.[14]
PPP gel injection as a dermal filler is a cost‐effective, well‐tolerated, very simple nonsurgical clinic procedure. It is an autologous material easily obtained from the patient’s own blood, and therefore, any risks of immunogenic reactions or disease transmission are eliminated. The viscous plasma gel gives immediate significant volumetric filling effect maintained for 3–6 months. It does not depend on high concentrations of platelets and gradual release of growth factors as compared to PRP but rather on its fibrin bundles that provide a scaffold for platelets trapping them in the treatment area to serve as a source for sustained release of growth factors. Although this method needs further validations, initial results are encouraging and promising. Further studies on bigger study population and longer duration of follow‐up, in addition to comparative studies with other types of popular dermal fillers, are required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Carruthers J, Cohen SR, Joseph JH, Narins RS, Rubin M. The science and art of dermal fillers for soft tissue augmentation. J Drugs Dermatol. 2009;8:335–50. [PubMed] [Google Scholar]
- 2.Requena L, Requena C, Christensen L, Zimmermann US, Kutzner H, Cerroni L. Adverse reactions to injectable soft tissue fillers. J Am Acad Dermatol. 2011;64:1–34; quiz 35-6. doi: 10.1016/j.jaad.2010.02.064. [DOI] [PubMed] [Google Scholar]
- 3.Woo SH, Kim JP, Park JJ, Chung PS, Lee SH, Jeong HS. Autologous platelet-poor plasma gel for injection laryngoplasty. Yonsei Med J. 2013;54:1516–23. doi: 10.3349/ymj.2013.54.6.1516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Yang L, Ma J, Gan S, Chu S, Maldonado M, Zhou J, et al. Platelet poor plasma gel combined with amnion improves the therapeutic effects of human umbilical cord‑derived mesenchymal stem cells on wound healing in rats. Mol Med Rep. 2017;16:3494–502. doi: 10.3892/mmr.2017.6961. [DOI] [PubMed] [Google Scholar]
- 5.Moreno PG, Ortiz GA, Martinez LT, Barbero J, O’Valle F, Wang HL. Composition of platelet‐rich plasma gel: Western blot analysis. J Oral Sci Rehabilit. 2016;17:42–8. [Google Scholar]
- 6.Janmey PA, Winer JP, Weisel JW. Fibrin gels and their clinical and bioengineering applications. J R Soc Interface. 2009;6:1–10. doi: 10.1098/rsif.2008.0327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hatakeyama I, Marukawa E, Takahashi Y, Omura K. Effects of platelet‐poor plasma, platelet‐rich plasma, and platelet‐rich fibrin on healing of extraction sockets with buccal dehiscence in dogs. Tissue Eng Part A. 2014;3:874–82. doi: 10.1089/ten.tea.2013.0058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sclafani AP. Safety, efficacy, and utility of platelet-rich fibrin matrix in facial plastic surgery. Arch Facial Plast Surg. 2011;13:247–51. doi: 10.1001/archfacial.2011.3. [DOI] [PubMed] [Google Scholar]
- 9.Galindo‐Moreno P, Fernández‐Barbero JE, Avila‐Ortiz G, Caba O, Sánchez‐Fernández E, Wang HL. Flow cytometric and morphological characterization of platelet‐rich plasma gel. Clin Oral Implants Res. 2006;17:687–93. doi: 10.1111/j.1600-0501.2006.01179.x. [DOI] [PubMed] [Google Scholar]
- 10.Wasterlain AS, Braun HJ, Harris AH, Kim HJ. The systemic effects of platelet‐rich plasma injection. Am J Sports Med. 2013;41:186–193. doi: 10.1177/0363546512466383. [DOI] [PubMed] [Google Scholar]
- 11.Amini F, Abiri F, Ramasamy TS, Tan ES. Efficacy of platelet rich plasma (PRP) on skin rejuvenation: a systematic review. Iran J Dermatol. 2015;18:119–127. [Google Scholar]
- 12.Man D, Plosker H, Winland‐Brown JE. The use of autologous platelet‐rich plasma (platelet gel) and autologous platelet‐poor plasma (fibrin glue) in cosmetic surgery. Plast Reconstruct Surg. 2001;107:229–37. doi: 10.1097/00006534-200101000-00037. [DOI] [PubMed] [Google Scholar]
- 13.Papakonstantinou E, Roth M, Karakiulakis G. Hyaluronic acid: a key molecule in skin aging. Dermatoendocrinol. 2012;4:253–8. doi: 10.4161/derm.21923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Doghaim NN, El-Tatawy RA, Neinaa YM. Assessment of the efficacy and safety of platelet poor plasma gel as autologous dermal filler for facial rejuvenation. J Cosmet Dermatol. 2019;18:1271–9. doi: 10.1111/jocd.12876. [DOI] [PubMed] [Google Scholar]


