We read with great interest the article by Lerner and colleagues (Lerner et al. 2019) reporting transcranial magnetic stimulation (TMS)-induced seizure events observed between 2012 and 2016. In their study, based on a survey of active laboratories and clinics (n=174 respondents) a total of 24 seizure cases were reported in approximately 318,560 TMS sessions (less than 0.08/1000 sessions). If TMS was delivered within published guidelines (Wassermann 1998; Rossi et al. 2009) to individuals without recognized risk factors, 4 TMS-induced seizure events were observed across 242,067 sessions (less than 0.02/1000 sessions). We would like to congratulate the authors for their successful project and contributions to this field. To extend on their work, we conducted a thorough literature search with PubMed and Web of Science to document the number of published TMS-induced seizure cases from the inception of TMS through the present date to stratify the cases by population, stimulation site, and stimulation protocol.
Our search strategy involved identifying studies through PubMed and Web of Science by using the key terms: “transcranial magnetic stimulation (or TMS)” and “seizure”. The databases were searched through February of 2020. In addition, we searched through the reference lists from previous reviews on relevant TMS articles pertaining to seizures (Wassermann 1998; Rossi et al. 2009). Studies were included based on the following criteria: 1) a seizure event due to TMS was reported; 2) the seizure was regarded as an unintentional adverse event; 3) the onset of seizure was within 24 hours of TMS application. Studies were first identified through the database searches based on their title and abstract, and any study clearly not relevant was excluded. Then the full text of all studies from this initial selection was retrieved and read. Extracted data included stimulation site, TMS type (e.g., single-pulse, paired-pulse, repetitive, or deep TMS), parameters of the stimulation, seizure type, and patient condition upon entering the study prior to the reported seizure event. Any disagreement was resolved by discussion among authors.
Our search identified 312 potentially relevant studies for assessment. Of these, 276 articles were excluded upon further examination of title, abstract, and full text. The remaining 36 studies (https://docs.google.com/spreadsheets/d/1-61EvbdttugGkpmQ9D_0_vh0qGNFswuPs2FygK3LYK8/edit?usp=sharing) that met the inclusion criteria were included in this report. In total, 41 seizure cases from the 36 studies were reported (15 males, 22 females, 4 unknown). Four cases were individuals under age of 20 (10%; 16 ± 1 years old); and 28 cases were individuals between age of 21 and 65 (68%; 36 ± 13 years old). The age of the remaining 9 cases (22%) was not reported.
Among the 41 cases, 13 were healthy individuals (32%) and 28 were patients with clinical conditions (68%). Of the 28 patients with clinical conditions (Figure 1), the majority were psychiatric disorders (16/28 = 57%) and stroke (6/28 = 21%). The remaining clinical conditions included migraine, brain tumor, pain, hydrocephalus, tinnitus, and multiple sclerosis (1 seizure event for each clinical condition). For TMS types, the majority of studies used conventional repetitive TMS (21/41 = 51% -- high frequency = 19, low frequency = 1, and unknown frequency = 1), deep TMS (9/41 = 22% -- high frequency rTMS = 6, continuous TBS = 2, single-pulse TMS = 1), single-pulse TMS (8/41 = 20%). Seizures induced by TBS protocols were also reported (2/41 = 5% -- intermittent TBS = 1; continuous TBS = 1). For the stimulation sites, most of the identified seizure events resulted from TMS applied over the primary motor cortex (21/41 = 51%) and the prefrontal cortex (14/41 = 34%). The remaining observations comprised TMS at the parietal region (2/41 = 5%), opercular-insular area (2/41 = 5%), auditory cortex (1/41 = 2%), and one unreported location. Given the unknown denominator problem and the disproportionate regularity with which TMS is applied across these regions, these results should be interpreted with care. Most of the seizures could be classified as generalized seizures (22/41 = 54%) or focal to bilateral tonic-clonic seizures (11/41 = 27%). Six cases were focal seizures (6/41 = 15%) and in the remaining 2 cases, type of seizures was not reported.
Figure 1.
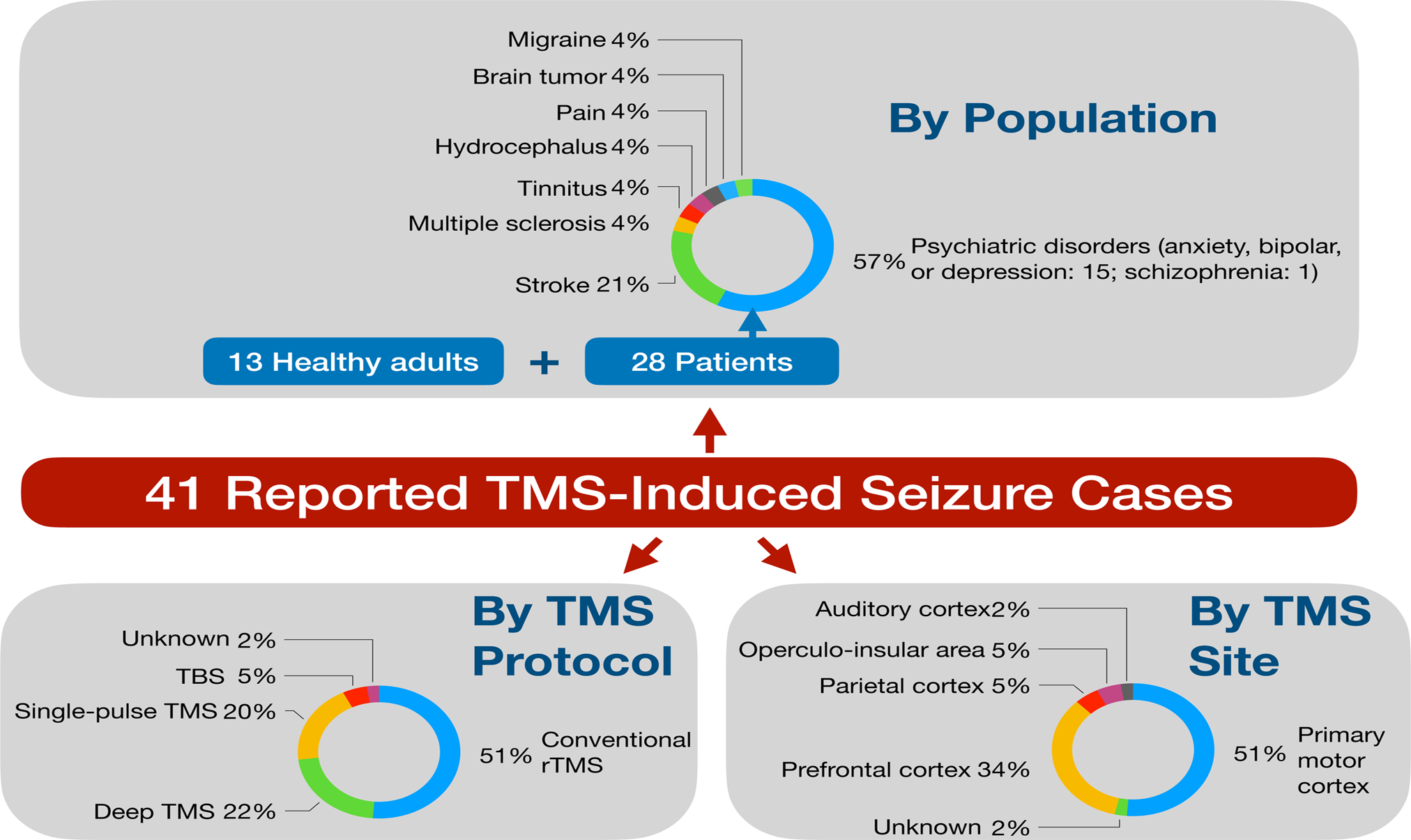
Reported TMS-induced seizure cases by population, stimulation protocol, and stimulation site.
Inadvertent induction of seizure remains one of the chief concerns when performing TMS procedures. As TMS-related research continues to expand, it is critical for researchers to understand, which participant characteristics and components of TMS protocols may increase the risk of seizure. This is best achieved with rigorous assessments of past adverse events that are frequently updated to reflect the current knowledgebase. We hope these findings can help to more accurately assess risk profiles and further reduce the incidence of TMS-induced seizures moving forward.
Acknowledgements
This work was supported by the NIH P30 AG019610 Arizona Alzheimer’s Consortium Pilot Study Program (Pilot Project PI: Y.-H. C.) and the University of Arizona BIO5 Team Scholars Award (PI: Y.-H. C.).
Footnotes
Conflict of interest
None of the authors have potential conflicts of interest to be disclosed.
References
- Lerner AJ, Wassermann EM and Tamir DI (2019). “Seizures from transcranial magnetic stimulation 2012–2016: Results of a survey of active laboratories and clinics.” Clin Neurophysiol 130(8): 1409–1416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rossi S, Hallett M, Rossini PM and Pascual-Leone A (2009). “Safety, ethical considerations, and application guidelines for the use of transcranial magnetic stimulation in clinical practice and research.” Clin Neurophysiol 120(12): 2008–2039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wassermann EM (1998). “Risk and safety of repetitive transcranial magnetic stimulation: report and suggested guidelines from the International Workshop on the Safety of Repetitive Transcranial Magnetic Stimulation, June 5–7, 1996” Electroencephalogr Clin Neurophysiol 108(1): 1–16. [DOI] [PubMed] [Google Scholar]


