Abstract
Objective
This study aimed to evaluate the thickness of the remaining patellar bone stock following extra-articular knee resection (EKR) preserving the extensor mechanism in human cadaveric knee joints.
Methods
A total of 14 human cadaveric knee joints (8 men and 2 women) were dissected, and the patellar thickness from the joint capsule insertion to the anterior cortex of the patella was measured using an electronic caliper. The mean age of the cadavers was 37 years (range=28–50). Measurements were performed by an anatomist and an orthopedic surgeon. As the total number of the cadavers was not enough to show the patellar thickness with sampling (sex and age), we endeavored to supplement the content with magnetic resonance images (MRI). Accordingly, the patellar bone thickness was also measured on axial MRI scans of 100 adult and 25 pediatric knees of patients (71 women and 54 men; mean age=36 years; age range=7–67 years) admitted to our hospital in whom meniscal tears were suspected. The rate of specimens with remaining patellar thickness of less than 10 mm after presumed resection was evaluated. The macroscopic measurements in cadavers and MRI measurements in adult knees were compared statistically.
Results
The mean thickness of the residual patellar bone of the cadaver dissections following a presumed EKR preserving the extensor mechanism was 8.2 mm (range=3.4–15.8). Additionally, in 71.4% (10/14) of the cadaveric knees, the thickness of residual patellar bone was less than 10 mm. In MRI scans, the average thickness of residual patella after presumed resection was 8.6 mm (range: 3.6–16) in adult knees and 6.9 mm (range: 3.4–10) in pediatric knees, and the residual patellar thickness less than 10 mm after presumed resection was determined in 72% of all MRI scans. Macroscopic measurements in cadaveric knees were statistically similar to MRI scan measurements in adult knees (p=0.765, Mann-Whitney U test).
Conclusion
Evidence from this study revealed that the thickness of the remaining patellar bone stock after EKR preserving the extensor mechanism may be low. A preoperative assessment with MRI can guide the surgeon to select the appropriate method for knee resection in order to prevent from the complications of resected patella.
Keywords: Extra-articular, Extensor mechanism, Patellar bone stock, Extensor weakness, Patella fracture, Knee malignant
Introduction
Intra-articular malignant lesions, extension of malignant extra-articular tumors that contaminate the knee joint along the intra-articular cruciate ligaments, intra-articular pathological fractures due to malignant tumors and an inappropriate biopsy are the most common factors contaminating the knee joint and necessitate an extra-articular knee resection (EKR) (1, 2).
As a common site for malignant lesions, the knee is a special case for extra-articular resection because of the extensor mechanism. In case of intra-articular malignant contamination, options are above-knee amputation, primary arthrodesis, rotationplasty or endoprosthetic reconstruction following EKR. Extensor mechanism reconstruction with extensor mechanism allografts, artificial ligaments, or tendon transfers is only needed when EKR is performed without preserving patella and when such resection is reconstructed with a standard tumor endoprostheses. The availability of extensor mechanism allograft, infection, longevity of the material, and the incorporation of the allograft are the major drawbacks of this technique (2–10).
Extra-articular resection sparing the extensor mechanism has been defined as a variation of classical resection, which includes preservation of the extensor mechanism by releasing the Hoffa fat pad and synovial pouch, cutting the patella anterior to the joint capsule, and resection without any view of articular cartilage and synovium (11). Because of capsular penetration, contamination risk and the risk of fracture when excessive bone is removed are two main drawbacks of this procedure (12). Patellar resection leaving less than 10 mm bone stock is accepted as a risk factor for fracture in resurfaced patellas (13–17). Non-resurfacing the patella is another option for avoiding fracture with a moderate amount of extension loss.
As there is a potential for patellar complications or extension power loss after a certain amount of resection in EKR preserving the extensor mechanism, we sought to determine the thickness of the remaining patellar bone stock. This may be used for selecting the resection method or informing the patient preoperatively about the option of non-resurfaced patella.
Materials and methods
A total of 14 knees from 10 formaldehyde-fixed human cadavers (8 men and 2 women) were collected and dissected without cutting the bone to determine the thickness of the patella and the distance between the anterior surface and the insertion of the anterior capsule to the patella (Figure 1). Measurements were performed by an anatomist and an orthopedic surgeon together in order to avoid any measurement error. The mean age of the cadavers was 37 years (range: 28–50). Microscopic magnification (×12) was used for precise dissection. After removal of skin, subcutaneous fat, and superficial fascia, complete arthrotomy was performed and the insertion of the capsule was exposed circumferentially and marked for measurement (Figure 2. a, b). Measurements were completed with electronic calipers to find the thickness of the patella anterior to the joint capsule (Figure 1). A real patellar resection was performed on only one cadaver to see if there is a difference between the measurements of residual patellar thickness following a presumed resection and after a real resection.
Figure 1.
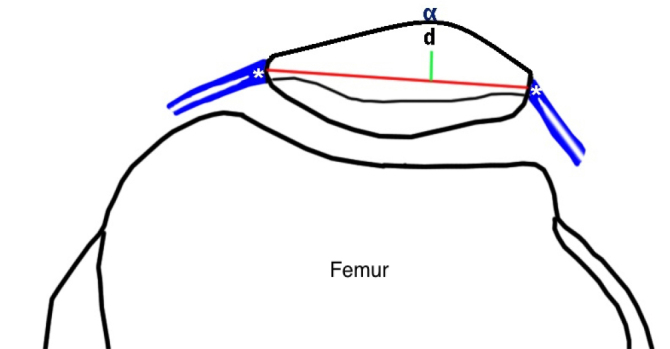
Diagram showing the line between the capsular insertion points. The measured distance is between this line and the anterior cortex. (*: capsular insertion, α: patellar anterior cortex, d: distance between the line and the anterior patellar cortex)
Figure 2. a, b.
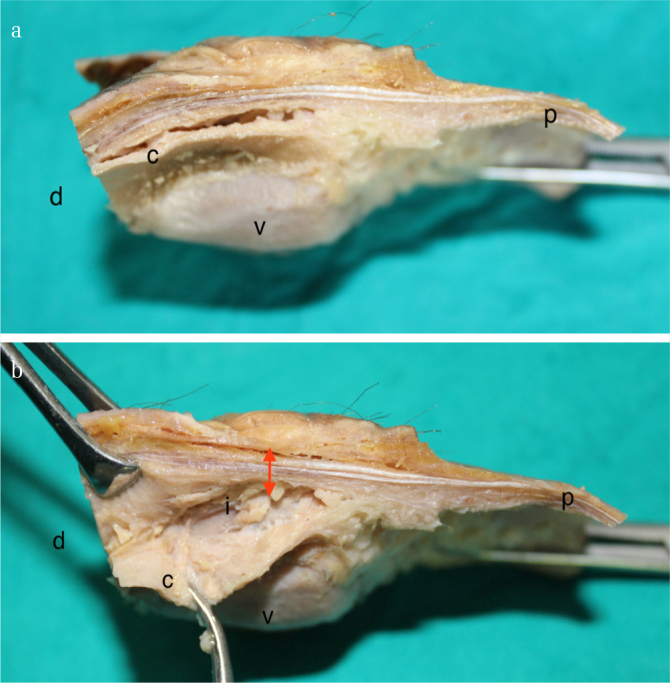
a) A photograph demonstrating the dissected patella in medial view b) dissected capsule. (i) Capsular insertion, (c) capsule, (v) articular side of patella, (p) proximal, (d) distal, red arrow representing anterior cortex
As the total number of the cadavers was not enough to show the patellar thickness with sampling (sex and age), we endeavored to supplement the content with MRI evaluation. The patellar bone thickness from the anterior cortex to the capsular insertion was also measured on axial MRI (1.5 Tesla, General Electric, Optima MR360, USA) scans of 100 adult and 25 pediatric knees of patients (71 women and 54 men; mean age: 36 years; range: 7–67 years) admitted to the hospital between August and December 2015 in whom meniscal tears were suspected. The study was performed on the axial proton density (PD) fat saturated images in the 5 mm slice thickness. A standardized protocol was used in positioning the subject’s knee and capturing the image. The cartilage bone interface was accepted as the closest point where extra-articular resection could safely be performed without violating the knee joint in radiological measurements (Figure 3). Centricity PACS-IW (General Electric Company, Barrington, IL, USA) software was used to access and to evaluate MRI scans of the patients. The measurement technique of the patellar thickness was taken from a study by Yoo et al. (18). The medial and lateral points for bone cartilage transition were marked in the radiological examination and a line was drawn connecting these two points. The distance between the line and the most anterior point of the patella was measured. In total, 1 mm was deducted from the measurement for the calculation of the remaining bone stock compensating for saw thickness and possible over resection.
Figure 3.
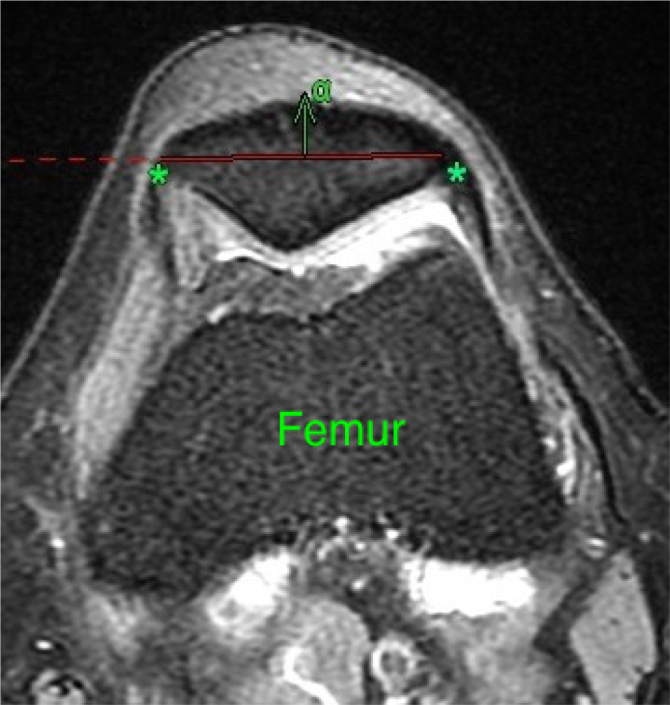
A magnetic resonance image showing the line between medial and lateral bone cartilage transition points; distance between the line and the anterior cortex of patella. (*) Capsular insertion, (α) anterior cortex
Statistical analysis
All data were combined using descriptive statistics. Continuous variables were calculated as a mean and range. For non-parametric data, Mann-Whitney U test was used.
Results
The residual patellar bone of the cadaver in which real patellar resection was planned is measured to be 8.4 mm right before the patellar resection. After the patellar resection, the residual patellar bone was measured as 8.4 mm as well. As both measurements were found to be the same, a real patellar resection was not carried out to the rest of the cadavers. The mean thickness of the residual patellar bone of the cadaver dissections following a presumed resection was 8.2 mm (range: 3.4–15.8). The mean values in women and men were 7.3 mm (range: 3.4–15.8) and 8.9 mm (range: 5.6–14.7), respectively. The rate of specimens with less than 10 mm remaining patellar thickness after the presumed resection was 71.4% (10/14) in the cadaver group. The rate of specimens with less than 5 mm and 7 mm remaining bone was 7% (1/14; 0 men and 1 women) and 42% (6/14; 2 men and 4 women), respectively.
The mean thickness of residual patella after presumed resection in adult patients on the MRI was 8.6 mm (range: 3.6–16.0). The mean values in women and men were 8.2 mm (range: 3.6–4.0) and 9.2 mm (range: 4.1–16.0), respectively. The pediatric patients had an average remaining bone thickness of 6.9 mm (range: 3.4–10.0).
The remaining patellar thickness less than 10 mm, between 7 mm and 10 mm and less than 7 mm after the presumed resection was determined in 72%, 46.4%, and 25.6%, respectively of all MRI scans. The demographic data are shown in Table 1. Comparison of residual patellar thickness values revealed that the macroscopic measurements in cadaveric knees were statistically similar to MRI scan measurements in adult knees (p=0.765, Mann-Whitney U test).
Table 1.
The demographic data of MR group
| Patella* | Men | Women | Pediatric | Total, n (%) |
|---|---|---|---|---|
| ≤ 7 mm | 3 | 16 | 13 | 32 (25.6) |
| 7–10 mm | 18 | 29 | 11 | 58 (46.4) |
| > 10 mm | 18 | 16 | 1 | 35 (28) |
| Total | 39 | 61 | 25 | 125 (100) |
Remaining patellar thickness after presumed resection
Discussion
The knee joint is the most common location for many primary sarcomas of bone and soft tissue, such as osteosarcoma, Ewing’s sarcoma, and synovial sarcoma (19). These malignant lesions may contaminate the knee joint via direct intra-articular spread of the tumor mass, involvement of cruciate ligaments, by an inappropriate biopsy contaminating the joint or after an intra-articular pathological fracture (1, 2). Irrespective of the cause, a joint, including malignant cells, should be removed completely with en bloc resection (9).
EKR is one of the surgical options that can be performed when malignant lesions contaminates the knee joint in order to achieve negative surgical margins. Performing EKR without preserving patella has the advantage of providing a safer resection in means of tumor-free wide margins; however, reconstructing an extensor mechanism will be the major concern that an orthopedic oncology surgeon must face. Performing the resection by sparing the extensor mechanism with anterior extra-articular portion of patella is a variation of classical EKR and is much more challenging due to contamination risk in case of capsular penetration and patellar fracture risk if patellar resection gets too superficial in order not to cause any capsular breach. In such resections, the amount of residual patellar bone thickness has paramount importance; thinner the patella, higher the risk for a fracture and harder to place a patellar component (2–8). Zwolak et al. described the results of an alternative technique consisting of the preservation of the extensor apparatus by splitting the patella anterior to the joint capsule and detaching the suprapatellar synovial pouch and infrapatellar fat pad. In the original technique, a precise patella osteotomy was performed leaving approximately 15 mm of bone for the polyethylene patellar component. They reported good clinical results with no extensor lag and no complications associated with the extensor mechanism or patella, specifically no patellar fractures (12). In previous studies performed on adult patients and cadavers, many authors stated that a patella thickness of 11 mm is a fracture risk limit in terms of normal daily loading (13, 14, 16). Seo et al. reported patellar resection thickness as a contributor to anterior knee pain and extensor mechanism efficiency in addition to fracture risk (15). Clarke et al. stated that the female gender is a risk factor for a post-resection residual patellar thickness less than 13 mm (17).
In this study, we studied the thickness of the patella anterior to the minimal resection level, which is accepted to be 1 mm anterior to the capsular insertion (including the thickness of a fine sagittal saw). Cadavers were used to evaluate the relationship between the capsular insertion and the remaining patellar bone stock. There are no studies indicating the rate of patellar deterioration in patients after presumed extra-articular resection.
Our data indicated that joint capsule insertion on the patella can be very close to the anterior margin, down to 3.4 mm. We assumed that patellar bone stock would be below the critical level in 72% of all MRI scan measurements. This gets even more critical for pediatric patients as the remaining patellar thickness less than 10 mm after the presumed resection was determined in 24 out of 25 (96%) pediatric MRI scans. Measurements on cadaver specimens and MRI sections were similar with a mean of 8.2 and 8.6 mm, respectively. Pediatric patients have an average remaining bone thickness of 6.9 mm, and in 52% of the cases, this value is below 7 mm, which indicates a very high fracture risk especially in the attempt to resurface the patella.
We recognize the limitations of cadaver models and radiological measurements, which have obvious differences from surgery itself. Additionally, the study is lacking pediatric cadavers and we did not perform any MRI evaluation in none of the cadaveric knees. Another important limitation is that real patellar resection was performed only on one cadaveric knee. As there was no difference between the measurements of residual patellar thickness following a presumed resection and after a real resection, a real patellar resection was not carried out to the rest of the cadavers. We also had the opportunity to perform a much more precise measurement from the connection of the cartilage and the bone in the study. However, this might have led to an under-estimation of the residual patellar thickness due to excessive resection in order to include the joint capsule itself. Despite the limitations, these measurements show the patellar stock following EKR is below the critical level in 72% of the cases.
Patellar resurfacing can be considered as safe in only 34% of adult and 4% in pediatric patient groups. These results highlight the importance of patient selection before the preoperative decision of extensor mechanism preservation. Therefore, preoperatively all options, such as EKR with entire patella, EKR with preserving the anterior portion of patellar bone without resurfacing, possible need for the use of extensor mechanism allografts, and endoprosthetic reconstruction types should be discussed with the patient.
In conclusion, our results clearly indicate that the amount of residual patellar bone after EKR is low. A preoperative risk evaluation can guide the surgeon to select the appropriate method for knee resection. Further clinical and anatomical research should be conducted to evaluate the results of EKR from the perspective of patellar resurfacing, non-resurfacing, and other methods as well as the risk of patellar fracture.
HIGHLIGHTS.
The knee joint is the most common location for many primary sarcomas of bone.
Extra-articular knee resection preserving extensor mechanism is one of the surgical options that can be performed when malignant lesions contaminates the knee joint in order to achieve negative surgical margins.
The amount of residual patellar bone thickness has paramount importance; thinner the patella, higher the risk for a fracture and harder to place a patellar component.
Footnotes
Ethics Committe Approval: N/A.
Informed Consent: N/A.
Author Contributions: Concept - K.B.; Design - K.B., M.O.K.; Supervision - M.A., Y.Y.; Materials - M.O.K., T.E., A.F.E., K.B., M.A., Y.Y.; Data Collection and/or Processing - M.O.K., A.F.E., T.E., M.A., K.B.; Analysis and/or Interpretation - Y.Y., M.O.K.; Literature Search - Y.Y., K.B., M.O.K., M.A., A.F.E., T.E.; Writing Manuscript - M.O.K.; Critical Review - Y.Y., K.B.,M.A.
Conflict of Interest: The authors have no conflicts of interest to declare.
Financial Disclosure: The authors declared that this study has received no financial support.
References
- 1.Eckardt J, Springfield D, Peabody T. Distal Femur. In: Simon MA, Springfield D, editors. Surgery for Bone and Soft Tissue Tumors. Philadelphia: Lippincott-Raven; 1997. pp. 357–73. [Google Scholar]
- 2.Malawer M. Musculoskeletal Cancer Surgery. Dordrecht: Kluwer Academic Publishers; 2001. Distal femoral resection with endoprosthetic reconstruction; pp. 459–83. [DOI] [Google Scholar]
- 3.Anract P, Missenard G, Jeanrot C, Dubois V, Tomeno B. Knee reconstruction with prosthesis and muscle flap after total arthrectomy. Clin Orthop Relat Res. 2001;384:208–16. doi: 10.1097/00003086-200103000-00024. [DOI] [PubMed] [Google Scholar]
- 4.Kendall SJ, Singer GC, Briggs TW, Cannon SR. A functional analysis of massive knee replacement after extra-articular resections of primary bone tumors. J Arthroplasty. 2000;15:754–60. doi: 10.1054/arth.2000.8104. [DOI] [PubMed] [Google Scholar]
- 5.Ayerza MA, Aponte-Tinao LA, Abalo E, Muscolo DL. Continuity and function of patellar tendon host-donor suture in tibial allograft. Clin Orthop Relat Res. 2006;450:33–8. doi: 10.1097/01.blo.0000229291.21722.b5. [DOI] [PubMed] [Google Scholar]
- 6.Dominkus M, Sabeti M, Toma C, Abdolvahab F, Trieb K, Kotz RI. Reconstructing the extensor apparatus with a new polyester ligament. Clin Orthop Relat Res. 2006;453:328–34. doi: 10.1097/01.blo.0000229368.42738.b6. [DOI] [PubMed] [Google Scholar]
- 7.Bickels J, Wittig JC, Kollender Y, et al. Reconstruction of the extensor mechanism after proximal tibia endoprosthetic replacement. J Arthroplasty. 2001;16:856–62. doi: 10.1054/arth.2001.25502. [DOI] [PubMed] [Google Scholar]
- 8.Dominkus M, Sabeti M, Kotz R. [Functional tendon repair in orthopedic tumor surgery]. Orthopade. 2005;34:556–9. doi: 10.1007/s00132-005-0802-0. [DOI] [PubMed] [Google Scholar]
- 9.Enneking WF, Shirley PD. Resection-arthrodesis for malignant and potentially malignant lesions about the knee using an intramedullary rod and local bone grafts. J Bone Joint Surg Am. 1977;59:223–36. doi: 10.2106/00004623-197759020-00016. [DOI] [PubMed] [Google Scholar]
- 10.Kotz R, Salzer M. Rotation-plasty for childhood osteosarcoma of the distal part of the femur. J Bone Joint Surg Am. 1982;64:959–69. doi: 10.2106/00004623-198264070-00001. [DOI] [PubMed] [Google Scholar]
- 11.Nakamura S, Kusuzaki K, Murata H, et al. Extra-articular wide tumor resection and limb reconstruction in malignant bone tumors invading the knee joint. Oncol Rep. 8:365–8. doi: 10.3892/or.8.2.365. [DOI] [PubMed] [Google Scholar]
- 12.Zwolak P, Kühnel SP, Fuchs B. Extraarticular knee resection for sarcomas with preservation of the extensor mechanism: Surgical technique and review of cases. Clin Orthop Relat Res. 2011;469:251–6. doi: 10.1007/s11999-010-1359-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lie DTT, Gloria N, Amis AA, Lee BPH, Yeo SJ, Chou SM. Patellar resection during total knee arthroplasty: effect on bone strain and fracture risk. Knee Surg Sports Traumatol Arthrosc. 2005;13:203–8. doi: 10.1007/s00167-004-0508-6. [DOI] [PubMed] [Google Scholar]
- 14.Jujo Y, Yasui T, Nagase Y, Kadono Y, Oka H, Tanaka S. Patellar fracture after total knee arthroplasty for rheumatoid arthritis. J Arthroplasty. 2013;28:40–3. doi: 10.1016/j.arth.2012.04.022. [DOI] [PubMed] [Google Scholar]
- 15.Seo JG, Moon YW, Park SH, Lee JH, Kang HM, Kim SM. A case-control study of spontaneous patellar fractures following primary total knee replacement. J Bone Joint Surg Br. 2012;94:908–13. doi: 10.1302/0301-620X.94B7.28552. [DOI] [PubMed] [Google Scholar]
- 16.Fitzpatrick CK, Kim RH, Ali AA, Smoger LM, Rullkoetter PJ. Effects of resection thickness on mechanics of resurfaced patellae. J Biomech. 2013;46:1568–75. doi: 10.1016/j.jbiomech.2013.03.016. [DOI] [PubMed] [Google Scholar]
- 17.Clarke HD, Spangehl MJ. Gender optimized patellar component designs are needed to better match female patellar anatomy. Knee. 2014;21:1250–3. doi: 10.1016/j.knee.2014.08.009. [DOI] [PubMed] [Google Scholar]
- 18.Yoo JH, Yi SR, Kim JH. The geometry of patella and patellar tendon measured on knee MRI. Surg Radiol Anat. 2007;29:623–8. doi: 10.1007/s00276-007-0261-x. [DOI] [PubMed] [Google Scholar]
- 19.Eck JC, Aboulafia AJ. Endoprosthetic reconstruction for treatment of tumors about the knee. Curr Opin Orthop. 2004;15:41–4. doi: 10.1097/00001433-200402000-00011. [DOI] [Google Scholar]


